Expectations Versus Reality in Inhalation Technique—A Case–Control Study of Inhalation Technique in Patients with Asthma or COPD
Abstract
1. Introduction
2. Materials and Methods
2.1. General Study Design
2.2. Patients
2.3. Methods
- -
- General demographic and education data;
- -
- Clinical data on asthma or COPD, as well as comorbidities;
- -
- Data on the duration of the disease, its previous course;
- -
- -
- -
- -
- Number of former IT training sessions and/or sources of information on proper IT via prescribed device;
- -
- Motivation for treatment was evaluated with the use of a dedicated 8-item questionnaire created for the purpose of the study (Supplementary Table S2);
- -
- -
- Potential visual or hearing impairment was evaluated in an indicative assessment using both questionnaires and ophthalmological Snellen charts.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MDI | Metered Dose Inhaler |
| DPI | Dry Powder Inhaler |
| COPD | Chronic Obstructive Pulmonary Disease |
| IT | Inhalation Technique |
| PIF | Peak Inspiratory Flow |
References
- Skolnik, N.; Yawn, B.P.; de Sousa, J.C.; Vázquez, M.M.M.; Barnard, A.; Wright, W.L.; Ulrich, A.; Winders, T.; Brunton, S. Best practice advice for asthma exacerbation prevention and management in primary care: An international expert consensus. npj Prim. Care Respir. Med. 2024, 34, 39. [Google Scholar] [CrossRef]
- Sanchis, J.; Gich, I.; Pedersen, S. Systematic Review of Errors in Inhaler Use: Has Patient Technique Improved Over Time? Chest 2016, 150, 394–406. [Google Scholar] [CrossRef]
- Molimard, M.; Raherison, C.; Lignot, S.; Balestra, A.; Lamarque, S.; Chartier, A.; Droz-Perroteau, C.; Lassalle, R.; Moore, N.; Girodet, P.-O. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: Real-life assessment of 2935 patients. Eur. Respir. J. 2017, 49, 1601794. [Google Scholar] [CrossRef] [PubMed]
- Usmani, O.S.; Lavorini, F.; Marshall, J.; Dunlop, W.C.N.; Heron, L.; Farrington, E.; Dekhuijzen, R. Critical inhaler errors in asthma and COPD: A systematic review of impact on health outcomes. Respir. Res. 2018, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Melani, A.S.; Bonavia, M.; Cilenti, V.; Cinti, C.; Lodi, M.; Martucci, P.; Serra, M.; Scichilone, N.; Sestini, P.; Aliani, M.; et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir. Med. 2011, 105, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Grandmaison, G.; Grobéty, T.; Vaucher, J.; Hayoz, D.; Suter, P. Prevalence of Critical Errors and Insufficient Peak Inspiratory Flow in Patients Hospitalized with COPD in a Department of General Internal Medicine: A Cross-Sectional Study. Chronic Obstr. Pulm. Dis. 2024, 11, 406–415. [Google Scholar] [CrossRef]
- Halpin, D.M.G.; Mahler, D.A. Systematic review of the effects of patient errors using inhaled delivery systems on clinical outcomes in COPD. BMJ Open Respir. Res. 2024, 11, e002211. [Google Scholar] [CrossRef]
- Leving, M.T.; van Boven, J.F.M.; Bosnic-Anticevich, S.Z.; van Cooten, J.; de Sousa, J.C.; Cvetkovski, B.; Dekhuijzen, R.; Dijk, L.; Pardo, M.G.; Gardev, A.; et al. Suboptimal Peak Inspiratory Flow and Critical Inhalation Errors are Associated with Higher COPD-Related Healthcare Costs. Int. J. Chronic Obstruct. Pulmon. Dis. 2022, 17, 2401–2415. [Google Scholar] [CrossRef]
- Kocks, J.; Bosnic-Anticevich, S.; van Cooten, J.; de Sousa, J.C.; Cvetkovski, B.; Dekhuijzen, R.; Dijk, L.; Pardo, M.G.; Gardev, A.; Gawlik, R.; et al. Identifying critical inhalation technique errors in Dry Powder Inhaler use in patients with COPD based on the association with health status and exacerbations: Findings from the multi-country cross-sectional observational PIFotal study. BMC Pulm. Med. 2023, 23, 302. [Google Scholar] [CrossRef]
- Calle Rubio, M.; Adami Teppa, P.J.; Rodríguez Hermosa, J.L.; García Carro, M.; Tallón Martínez, J.C.; Riesco Rubio, C.; Fernández Cortés, L.; Morales Dueñas, M.; Chamorro del Barrio, V.; Sánchez-del Hoyo, R.; et al. Insights from Real-World Evidence on the Use of Inhalers in Clinical Practice. J. Clin. Med. 2025, 14, 1217. [Google Scholar] [CrossRef]
- Marko, M.; Pawliczak, R. Inhalation technique-related errors after education among asthma and COPD patients using different types of inhalers—Systematic review and meta-analysis. npj Prim. Care Respir. Med. 2025, 35, 15. [Google Scholar] [CrossRef] [PubMed]
- Marko, M.; Klimczak, M.; Sobczak, M.; Wojakiewicz, M.; Dębowski, T.; Emeryk, A.; Pawliczak, R. Effective inhaler technique education is achievable—Assessment and comparison of five inhaler devices errors. Front. Pharmacol. 2025, 16, 1538283. [Google Scholar] [CrossRef] [PubMed]
- Pankovitch, S.; Frohlich, M.; AlOthman, B.; Marciniuk, J.; Bernier, J.; Paul-Emile, D.; Bourbeau, J.; Ross, B.A. Peak Inspiratory Flow and Inhaler Prescription Strategies in a Specialized COPD Clinical Program: A Real-World Observational Study. Chest 2025, 167, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. 2024 Report. Available online: https://ginasthma.org/2024-report/ (accessed on 14 August 2025).
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for Prevention, Diagnosis and Management of COPD. 2025 Report. Available online: https://goldcopd.org/2025-gold-report/ (accessed on 14 August 2025).
- Kocks, J.W.H.; Chrystyn, H.; van der Palen, J.; Thomas, M.; Yates, L.; Landis, S.H.; Driessen, M.T.; Gokhale, M.; Sharma, R.; Molimard, M. Systematic review of association between critical errors in inhalation and health outcomes in asthma and COPD. npj Prim. Care Respir. Med. 2018, 28, 43. [Google Scholar] [CrossRef]
- Bohadana, A.; Jarjoui, A.; Lujan, R.; Jaffal, S.; Rokach, A.; Izbicki, G. Inhaler Technique, Critical Errors, and Effective Inspiratory Flow in COPD Patients: A Prospective Study Comparing Patients Over and Under 65 Years of Age. J. Aerosol Med. Pulm. Drug Deliv. 2025; ahead of print. [Google Scholar] [CrossRef]
- Allen, S.C.; Ragab, S. Ability to learn inhaler technique in relation to cognitive scores and tests of praxis in old age. Postgrad. Med. J. 2002, 78, 37–39. [Google Scholar] [CrossRef]
- Song, M.J.; Kim, S.Y.; Kang, Y.A.; Kim, Y.S.; Park, M.S.; Ye, B.S.; Jung, J.Y. The relationship between cognitive function and competence in inhaler technique in older adults with airway disease. Geriatr. Nurs. 2022, 43, 15–20. [Google Scholar] [CrossRef]
- Elander, A.; Gustafsson, M. Inhaler Technique and Self-reported Adherence to Medications Among Hospitalised People with Asthma and COPD. Drugs Real World Outcomes 2020, 7, 317–323. [Google Scholar] [CrossRef]
- Usmani, O.S. Choosing the right inhaler for your asthma or COPD patient. Ther. Clin. Risk Manag. 2019, 15, 461–472. [Google Scholar] [CrossRef]
- Matsuyama, T.; Machida, K.; Hamu, A.; Takagi, K.; Momi, H.; Higashimoto, I.; Inoue, H. Effects of instructional materials on the proper techniques of inhaler device use. Respir. Investig. 2022, 60, 633–639. [Google Scholar] [CrossRef]
- Marando, M.; Tamburello, A.; Diedrich, J.P.; Valenti, A.; Gianella, P. Effectiveness of an Educational Intervention on Inhaler Technique Proficiency in Chronic Obstructive Pulmonary Disease: A Single-Center Quality Improvement Study. J. Respir. 2022, 2, 139–146. [Google Scholar] [CrossRef]
- Basheti, I.A.; Obeidat, N.M.; Reddel, H.K. Effect of novel inhaler technique reminder labels on the retention of inhaler technique skills in asthma: A single-blind randomized controlled trial. npj Prim. Care Respir. Med. 2017, 27, 9. [Google Scholar] [CrossRef]
- Dabrowska, M.; Luczak-Wozniak, K.; Miszczuk, M.; Domagala, I.; Lubanski, W.; Leszczynski, A.; Maskey-Warzechowska, M.; Rubinsztajn, R.; Hermanowicz-Salamon, J.; Krenke, R. Impact of a Single Session of Inhalation Technique Training on Inhalation Skills and the Course of Asthma and COPD. Respir. Care 2019, 64, 1250–1260. [Google Scholar] [CrossRef] [PubMed]
- Bosnic-Anticevich, S.; Bender, B.G.; Shuler, M.T.; Hess, M.; Kocks, J.W. Recognizing and Tackling Inhaler Technique Decay in Asthma and Chronic Obstructive Pulmonary Disesase (COPD) Clinical Practice. J. Allergy Clin. Immunol. Pract. 2023, 11, 2355–2364.e5. [Google Scholar] [CrossRef] [PubMed]
- Price, D.B.; Román-Rodríguez, M.; McQueen, R.B.; Bosnic-Anticevich, S.; Carter, V.; Gruffydd-Jones, K.; Haughney, J.; Henrichsen, S.; Hutton, C.; Infantino, A.; et al. Inhaler Errors in the CRITIKAL Study: Type, Frequency, and Association with Asthma Outcomes. J. Allergy Clin. Immunol. Pract. 2017, 5, 1071–1081.e9. [Google Scholar] [CrossRef] [PubMed]
- Chrystyn, H.; Price, D. Not all asthma inhalers are the same: Factors to consider when prescribing an inhaler. Prim. Care Respir. J. 2009, 18, 243–249. [Google Scholar] [CrossRef]
- Laube, B.L.; Janssens, H.M.; de Jongh, F.H.; Devadason, S.G.; Dhand, R.; Diot, P.; Everard, M.L.; Horvath, I.; Navalesi, P.; Voshaar, T.; et al. What the pulmonary specialist should know about the new inhalation therapies. Eur. Respir. J. 2011, 37, 1308–1331. [Google Scholar] [CrossRef]
- Gupta, N.; Pinto, L.M.; Morogan, A.; Bourbeau, J. The COPD assessment test: A systematic review. Eur. Respir. J. 2014, 44, 873–884. [Google Scholar] [CrossRef]
- Nathan, R.A.; Sorkness, C.A.; Kosinski, M.; Schatz, M.; Li, J.T.; Marcus, P.; Murray, J.J.; Pendergraft, T.B. Development of the asthma control test: A survey for assessing asthma control. J. Allergy Clin. Immunol. 2004, 113, 59–65. [Google Scholar] [CrossRef]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.M.; Zheng, J.; et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef]
- Stanojevic, S.; Kaminsky, D.A.; Miller, M.R.; Thompson, B.; Aliverti, A.; Barjaktarevic, I.; Cooper, B.G.; Culver, B.; Derom, E.; Hall, G.L.; et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur. Respir. J. 2022, 60, 2101499. [Google Scholar] [CrossRef]
- Juniper, E.F.; Buist, A.S.; Cox, F.M.; Ferrie, P.J.; King, D.R. Validation of a standardized version of the Asthma Quality of Life Questionnaire. Chest 1999, 115, 1265–1270. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M.; Littlejohns, P. A self-complete measure of health status for chronic airflow limitation: The St. George’s Respiratory Questionnaire. Am. Rev. Respir. Dis. 1992, 145, 1321–1327. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Pracownia Testów Psychologicznych PTP. MMSE—Mini Mental State Examination: Polska Adaptacja i Normalizacja Testu. Podręcznik Użytkownika; Pracownia Testów Psychologicznych PTP: Warsaw, Poland, 2025. [Google Scholar]
- Mossakowska, M.; Więcek, A.; Błędowski, P. Aspekty Medyczne, Psychologiczne, Socjologiczne i Ekonomiczne Starzenia się Ludzi w Polsce; Termedia Wydawnictwa Medyczne: Poznań, Poland, 2020; pp. 293–327. [Google Scholar]
- Bao, L.K.; Khoa, N.D.; Chi, L.T.K.; Anh, N.T. Prevalence and Factors Affecting Appropriate Inhaler Use in Elderly Patients with Chronic Obstructive Pulmonary Disease: A Prospective Study. J. Clin. Med. 2023, 12, 4420. [Google Scholar] [CrossRef]
- Melzer, A.C.; Ghassemieh, B.J.; Gillespie, S.E.; Lindenauer, P.K.; McBurnie, M.A.; Mularski, R.A.; Naureckas, E.T.; Vollmer, W.M.; Au, D.H. Patient characteristics associated with poor inhaler technique among a cohort of patients with COPD. Respir. Med. 2017, 123, 124–130. [Google Scholar] [CrossRef]
- Mahler, D.A. The role of inspiratory flow in selection and use of inhaled therapy for patients with chronic obstructive pulmonary disease. Respir. Med. 2020, 161, 105857. [Google Scholar] [CrossRef]
- Usmani, O.S.; Levy, M.L. Effective respiratory management of asthma and COPD and the environmental impacts of inhalers. npj Prim. Care Respir. Med. 2023, 33, 24. [Google Scholar] [CrossRef]
- Janson, C.; Henderson, R.; Löfdahl, M.; Hedberg, M.; Sharma, R.; Wilkinson, A.J.K. Carbon footprint impact of the choice of inhalers for asthma and COPD. Thorax 2020, 75, 82–84. [Google Scholar] [CrossRef]
- Vartiainen, V.; Woodcock, A.A.; Wilkinson, A.; Janson, C.; Björnsdóttir, U.; Haahtela, T.; Lehtimäki, L. Thoughtful prescription of inhaled medication has the potential to reduce inhaler-related greenhouse gas emissions by 85. BMJ Open Respir. Res. 2024, 11, e001782. [Google Scholar] [CrossRef]
- Molimard, M.; Raherison, C.; Lignot, S.; Depont, F.; Abouelfath, A.; Moore, N. Assessment of handling of inhaler devices in real life: An observational study in 3811 patients in primary care. J. Aerosol Med. 2003, 16, 249–254. [Google Scholar] [CrossRef]
- Alotaibi, M.M.; Hughes, L.; Ford, W.R. Assessing Inhaler Techniques of Asthma Patients Using Aerosol Inhalation Monitors (AIM): A Cross-Sectional Study. Healthcare 2023, 11, 1125. [Google Scholar] [CrossRef]
- Iamthanaporn, C.; Wisitsartkul, A.; Chuaychoo, B. Cognitive impairment according to Montreal Cognitive Assessment independently predicts the ability of chronic obstructive pulmonary disease patients to maintain proper inhaler technique. BMC Pulm. Med. 2023, 23, 144. [Google Scholar] [CrossRef]
- Zhou, L.-J.; Wen, X.-X.; Jiang, R.; Zhou, H.-Y.; Li, Y.; Mao, X.-R.; Lan, M. Inhaler use in chronic obstructive pulmonary disease patients: A meta-analysis. Front. Nurs. 2022, 9, 343–352. [Google Scholar] [CrossRef]
- Nicola, M.; Soliman, Y.M.A.; Hussein, R.; Saeed, H.; Abdelrahim, M. Comparison between traditional and nontraditional add-on devices used with pressurised metered-dose inhalers. ERJ Open Res. 2020, 6, 00073-2020. [Google Scholar] [CrossRef] [PubMed]
- Abdelfattah, A.M.; Sarhan, R.M.; Madney, Y.M.; Mady, A.F.; Abdelrahim, M.E.A.; Harb, H.S. User-Friendliness Evaluation of Handling pMDI with Various Add-on Devices in Asthmatic Patients. AAPS PharmSciTech 2024, 25, 274. [Google Scholar] [CrossRef] [PubMed]
- Göriş, S.; Taşci, S.; Elmali, F. The effects of training on inhaler technique and quality of life in patients with COPD. J. Aerosol Med. Pulm. Drug Deliv. 2013, 26, 336–344. [Google Scholar] [CrossRef]
- Cushen, B.; Sulaiman, I.; Greene, G.; MacHale, E.; Mokoka, M.; Reilly, R.B.; Bennett, K.; Doyle, F.; van Boven, J.F.M.; Costello, R.W. The Clinical Impact of Different Adherence Behaviors in Patients with Severe Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2018, 197, 1630–1633. [Google Scholar] [CrossRef]
- Maricoto, T.; Santos, D.; Carvalho, C.; Teles, I.; Correia-de-Sousa, J.; Taborda-Barata, L. Assessment of Poor Inhaler Technique in Older Patients with Asthma or COPD: A Predictive Tool for Clinical Risk and Inhaler Performance. Drugs Aging 2020, 37, 605–616. [Google Scholar] [CrossRef]
- Chorão, P.; Pereira, A.M.; Fonseca, J.A. Inhaler devices in asthma and COPD—An assessment of inhaler technique and patient preferences. Respir. Med. 2014, 108, 968–975. [Google Scholar] [CrossRef]
- Usami, O. Improved inhaler handling after repeated inhalation guidance for elderly patients with bronchial asthma and chronic obstructive pulmonary disease. Medicine 2022, 101, e30238. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, J.; Sonnenburg, T.; Luecke, E. Inhaler devices in asthma and COPD patients—A prospective cross-sectional study on inhaler preferences and error rates. BMC Pulm. Med. 2020, 20, 222. [Google Scholar] [CrossRef] [PubMed]
- Kamps, A.W.; van Ewijk, B.; Roorda, R.J.; Brand, P.L.P. Poor inhalation technique, even after inhalation instructions, in children with asthma. Pediatr. Pulmonol. 2000, 29, 39–42. [Google Scholar] [CrossRef]
- Almomani, B.A.; Al-Qawasmeh, B.S.; Al-Shatnawi, S.F.; Awad, S.; Alzoubi, S.A. Predictors of proper inhaler technique and asthma control in pediatric patients with asthma. Pediatr. Pulmonol. 2021, 56, 866–874. [Google Scholar] [CrossRef] [PubMed]
- Volerman, A.; Balachandran, U.; Zhu, M.; Akel, M.; Hull, A.; Siros, M.; Luna, V.; Xu, I.; Press, V.G. Evaluating inhaler education interventions for hospitalized children with asthma: A randomized controlled trial. Ann. Allergy Asthma Immunol. 2023, 131, 217–223.e1. [Google Scholar] [CrossRef]
- Capanoglu, M.; Dibek Misirlioglu, E.; Toyran, M.; Civelek, E.; Kocabas, C.N. Evaluation of inhaler technique, adherence to therapy and their effect on disease control among children with asthma using metered dose or dry powder inhalers. J. Asthma 2015, 52, 838–845. [Google Scholar] [CrossRef]
- Chrystyn, H.; van der Palen, J.; Sharma, R.; Barnes, N.; Delafont, B.; Mahajan, A.; Thomas, M. Device errors in asthma and COPD: Systematic literature review and meta-analysis. npj Prim. Care Respir. Med. 2017, 27, 22. [Google Scholar] [CrossRef]
- Calzetta, L.; Aiello, M.; Frizzelli, A.; Ritondo, B.L.; Pistocchini, E.; Rogliani, P.; Chetta, A. Impact of Sex on Proper Use of Inhaler Devices in Asthma and COPD: A Systematic Review and Meta-Analysis. Pharmaceutics 2022, 14, 1565. [Google Scholar] [CrossRef]
- Ocakli, B.; Ozmen, I.; Tuncay, E.A.; Gungor, S.; Ozalp, A.; Yasin, Y.; Adiguzel, N.; Gungor, G.; Karakurt, Z. Influence of Gender on Inhaler Technique. Respir. Care 2020, 65, 1470–1477. [Google Scholar] [CrossRef]
- Wieshammer, S.; Dreyhaupt, J. Dry powder inhalers: Which factors determine the frequency of handling errors? Respiration 2008, 75, 18–25. [Google Scholar] [CrossRef]
- Barnestein-Fonseca, P.; Cotta-Luque, V.M.; Aguiar-Leiva, V.P.; Leiva-Fernández, J.; Martos-Crespo, F.; Leiva-Fernández, F. The importance of reminders and patient preferences to improve inhaler technique in older adults with COPD. Front. Pharmacol. 2022, 13, 989362. [Google Scholar] [CrossRef]
- Press, V.G.; Arora, V.M.; Kelly, C.A.; Carey, K.A.; White, S.R.; Wan, W. Effectiveness of Virtual vs In-Person Inhaler Education for Hospitalized Patients with Obstructive Lung Disease: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e1918205. [Google Scholar] [CrossRef]
- Al-Kharouf, M.S.; Abdeljalil, M.H.; Obeidat, N.M.; Al Oweidat, K.; Awwad, O.; Rababa, M.J. Video-based teach-to-goal intervention on inhaler technique on adults with asthma and COPD: A randomized controlled trial. PLoS ONE 2023, 18, e0286870. [Google Scholar] [CrossRef] [PubMed]
- Imanipour, M.; Molazem, Z.; Rakhshan, M.; Fallahi, M.J. Evaluation of the Effectiveness of Teach-back Training on Asthma Control Indicators. Tanaffos 2022, 21, 230–238. [Google Scholar] [PubMed]
- Abbas, M.A.; Tariq, O.; Bin Zafar, S.; Jamil, M.I.; Hamid, K.; Iqbal, A.; Ahmed, A.; Naeem, I. Improvement in Inhaler Techniques After Training and Counseling in Patients with Chronic Obstructive Pulmonary Disease or Asthma. Cureus 2024, 16, e62255. [Google Scholar] [CrossRef] [PubMed]
- Sadowski, C.A.; Cor, K.; Cave, A.; Banh, H.L. Administration Technique and Acceptance of Inhaler Devices in Patients with Asthma or COPD. Ann. Pharmacother. 2015, 49, 639–648. [Google Scholar] [CrossRef]
- Lenney, J.; Innes, J.A.; Crompton, G.K. Inappropriate inhaler use: Assessment of use and patient preference of seven inhalation devices. Respir. Med. 2000, 94, 496–500. [Google Scholar] [CrossRef]
- Miszczuk, M.; Domagała, I.; Dąbrowska, M.; Maskey-Warzęchowska, M.; Krenke, R. How to assess inhalation technique in patients with asthma and COPD—Comparison of three different methods. Eur. Respir. J. 2020, 56 (Suppl. 64), 3180. [Google Scholar] [CrossRef]
| The Whole Group | Asthma | COPD | |
|---|---|---|---|
| Number of patients | 180 | 115 | 65 |
| Age (years) | 63.5 (52–71) | 60 (44–66.5) | 70 (64–76) |
| Sex F/M | 104/76 | 76 (66.1%)/39 (33.9%) | 28 (43.1%)/37 (56.9%) |
| Duration of the disease (years) | 10 (6–20) | 15 (7–26.5) | 10 (5–15) |
| Number of used inhalers | 2 (1–2) | 2 (1–2) | 2 (2–2) |
| Smoking history (NS/S/EX) | 61/15/104 | 58/7/50 | 3/8/54 |
| FEV1% N | 69% (45–88) | 81% (61–95.5) | 44.5% (37–65) |
| Education (primary/secondary/higher) | 13/95/72 | 6/59/50 | 7/36/22 |
| Number of comorbidities | 1 (1–3) | 1 (1–2) | 2 (0–3) |
| Asthma Control Test (points) | X | 20 (16–23.5) | X |
| Quality of Life—AQLQ (points) | X | 5.48 (4.29–6.23) | X |
| COPD Assessment Test (points) | X | X | 22 (16–26) |
| Quality of Life—SGRQ (points) | X | X | 56.9 (35.9–70) |
| MDI/SMI N = 140 | DPI N = 110 | |||||
|---|---|---|---|---|---|---|
| Proper Inhalation Technique N = 52 | Incorrect Inhalation Technique N = 88 | p Value | Proper Inhalation Technique N = 77 | Incorrect Inhalation Technique N = 33 | p Value | |
| Age (years) | 62.5 (51.8–70) | 65.5 (55.8–71) | 0.267 | 64 (55–71) | 63 (54–70) | 0.854 |
| Asthma/COPD | 35 (67.3%)/17 (32.7%) | 56 (63.6%)/ 32 (26.4%) | 0.797 | 45 (58.4%)/ 32 (41.6%) | 18 (54.5%)/ 15 (45.4%) | 0.866 |
| Disease duration (years) | 10 (6–22) | 11 (6,8–20) | 0.761 | 10 (7–20) | 10 (5–20) | 0.786 |
| Gender (F/M) | 32 (61.5%)/ 20 (38.5%) | 48 (54.5%)/ 40 (45.5%) | 0.528 | 40 (51.9%)/37 (48.1%) | 20 (60.6%)/13 (39.4%) | 0.531 |
| Smoking history (S/ExS, NS) | 3/38/11 | 10/47/31 | 0.103 | 7/43/27 | 4/18/11 | 0.887 |
| Education (primary/ secondary/ higher) | 5 (9.6%)/ 23 (46.2%)/ 24 (46.2%) | 6 (6.8%)/ 55 (62.5%)/ 27 (30.7%) | 0.109 | 4 (5.2%)/ 43 (55.8%)/ 30 (38.9%) | 4 (12.1%)/ 19 (57.6%)/ 10 (30.3%) | 0.366 |
| Motivation for therapy (points) | 10 (9–10) | 10 (9–10) | 0.484 | 10 (8–10) | 10 (9–10) | 0.640 |
| Number of inhalers | 2 (1–2) | 2 (2–2) | 0.063 | 2 (2–2) | 2 (1.8–2) | 0.753 |
| FEV1%N z-score | −1.6 (−2.4; −0.5) | −2.4 (−2.4; −1.2) | 0.109 | −1.9 (−2.4; −1.3) | −2.4 (−2.4; −1.1) | 0.534 |
| Side effects of the inhalers | 1 (1–3) | 1 (0–2) | 0.004 | 1 (0–2) | 1 (0–2) | 0.534 |
| Significant visual disorders | 12 (37.5%) | 33 (29.7%) | 0.897 | 24 (31.2%) | 11 (33.3%) | 0.823 |
| Significant hearing loss | 4 (7.7%) | 8 (9.1%) | 0.775 | 10 (13%) | 0 | 0.089 |
| Hand muscle/joint disorders | 0 | 4 (4.5%) | 0.408 | 3 (18.8%) | 1 (33.3%) | 0.597 |
| Any cognitive disorders (MMSE) | 6 (11.5%) | 20 (22.7%) | 0.099 | 14 (20.3%) | 10 (35.7%) | 0.158 |
| Regular use of inhalers in self-assessment 1 | 51 (98.1%) | 84 (95.4%) | 0.736 | 73 (94.8%) | 31 (93.9%) | 0.854 |
| Any deviations from regular use of inhalers during last 6 months 1 | 6 (11.5%) | 21 (23.9%) | 0.118 | 11 (14.3%) | 10 (30.3%) | 0.090 |
| Positive self-assessment of own inhalation technique 1 | 50 (96.2%) | 80 (90.9%) | 0.410 | 76 (98.7%) | 29 (87.9%) | 0.046 |
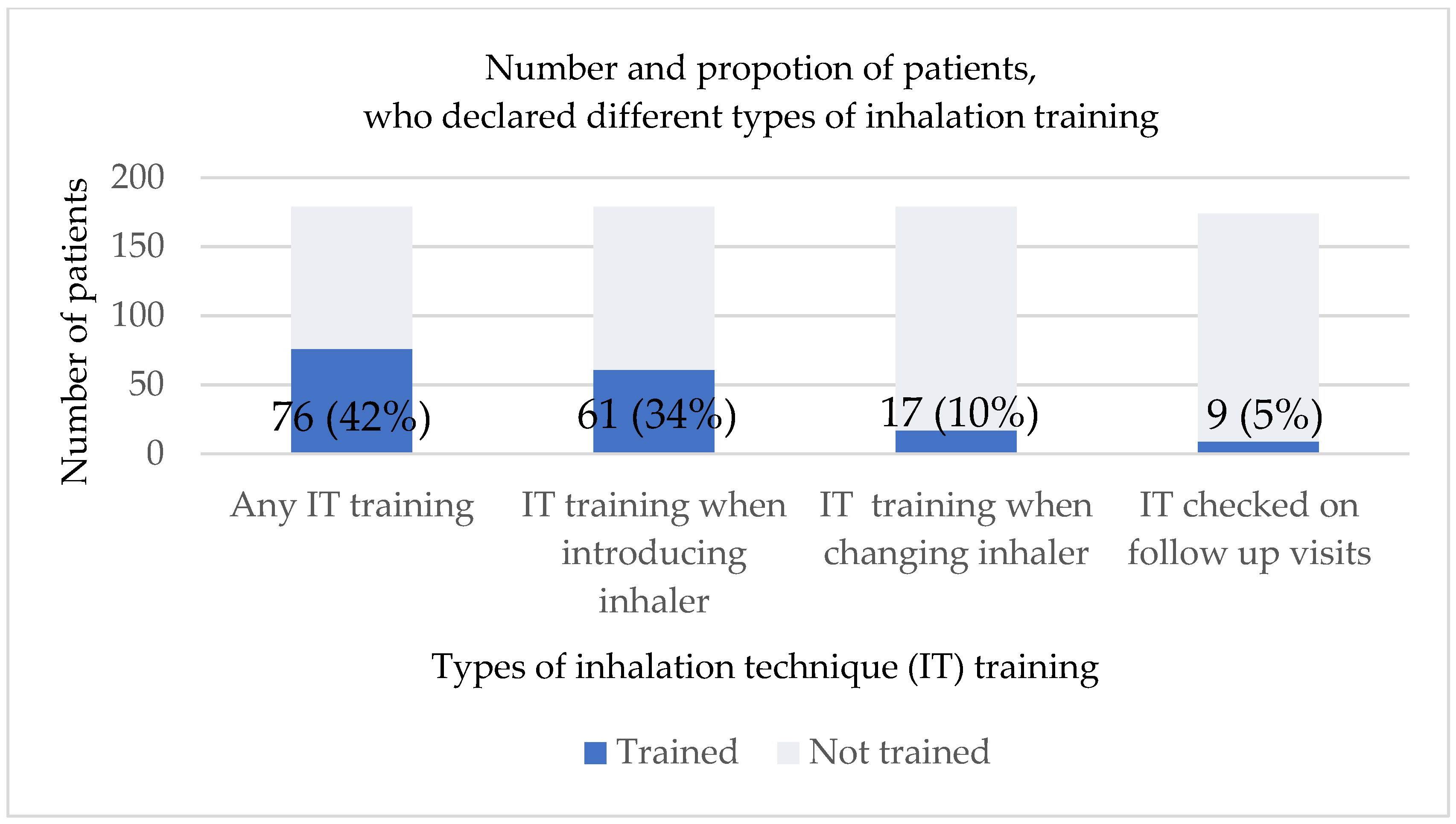
| Any IT before | 23 (45.1%) | 36 (40.9%) | 0.761 | 38 (49.4%) | 4 (12.1%) | 0.001 |
| IT when introducing treatment | 12 (23.5%) | 30 (34.1%) | 0.265 | 32 (41.6%) | 3 (9.1%) | 0.002 |
| IT when changing Inhaler | 4 (7.8%) | 8 (9.1%) | 0.775 | 11 (14.3%) | 0 | 0.052 |
| Reading the drug leaflet | 49 (96.1%) | 70 (79.6%) | 0.015 | 65 (84.4%) | 28 (84.9%) | 0.954 |
| Asthma N = 115 | COPD N = 65 | p Value | |
|---|---|---|---|
| Age | 60 (44–66.5) | 70 (64–76) | <0.001 |
| Disease duration | 15 (7–26.5) | 10 (5–15) | <0.001 |
| Motivation | 10 (8–10) | 10 (9–10) | 0.443 |
| Number of inhalers | 2 (1–2) | 2 (2–2) | 0.652 |
| Gender (F/M) | 76 (66.1%)/39 (33.9%) | 28 (43.1%)/37 (56.9%) | 0.004 |
| Number of comorbidities | 1 (1–2) | 2 (0–3) | 0.264 |
| Any inhalation training before | 61 (53.5%) | 15 (23.1%) | <0.001 |
| Any inhalation training when starting treatment | 47 (41.2%) | 14 (21.5%) | 0.012 |
| Any inhalation training when switching the inhaler | 17 (14.9%) | 0 | 0.003 |
| Reading the drug leaflet | 100 (87.7%) | 55 (84.6%) | 0.720 |
| Number of side effects related to inhalers | 1 (0–2) | 1 (0–2) | 0.228 |
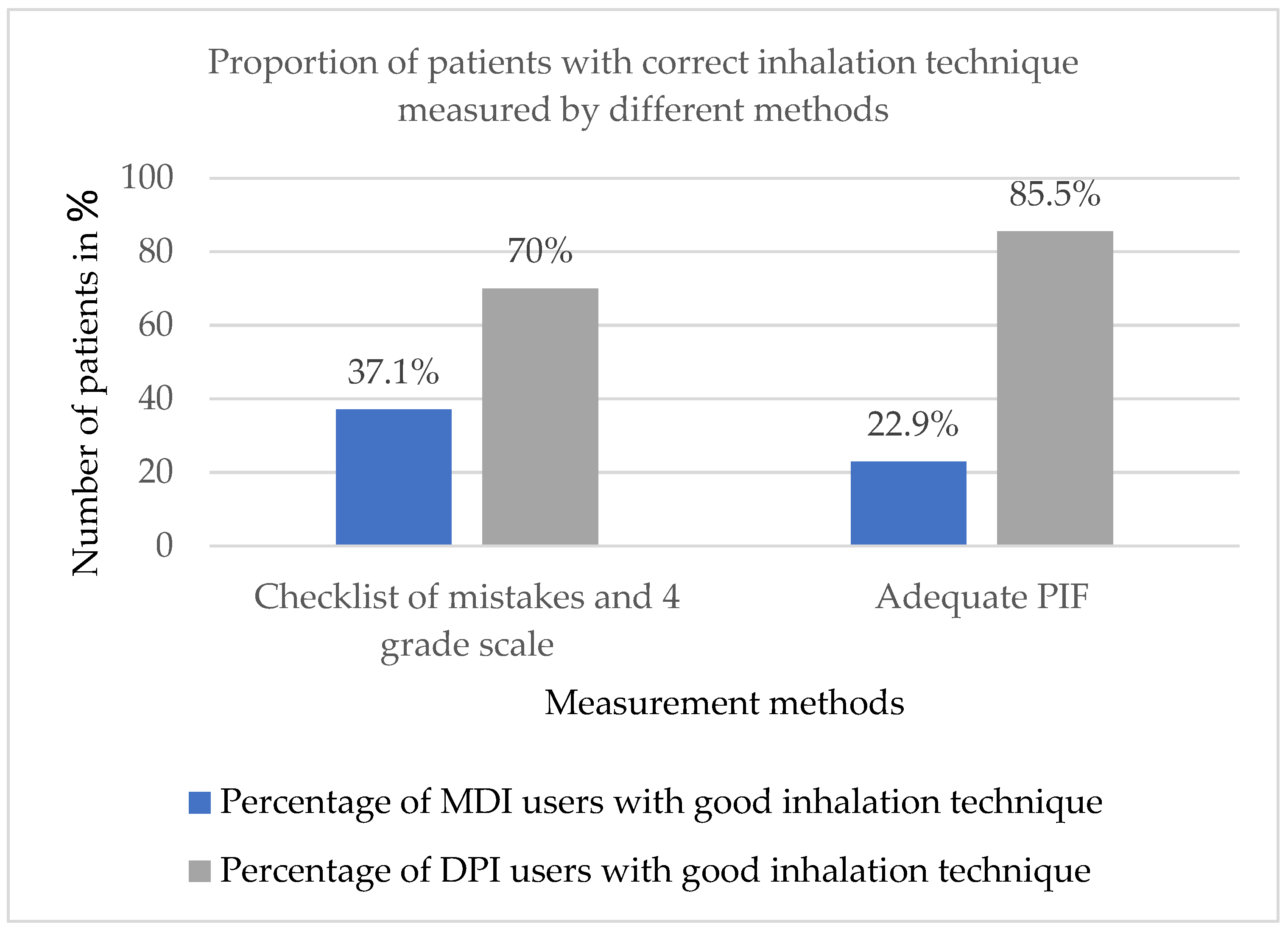
| Proper inhalation technique for DPI | 26 (41.3%) | 21 (44.7%) | 0.913 |
| Proper inhalation technique for MDI | 11 (12.1%) | 5 (10.2%) | 0.951 |
| Proper peak inspiratory flow by In-Check Dial in DPI users | 53 (86.9%) | 41 (89.1%) | 0.958 |
| Proper peak inspiratory flow by In-Check Dial in MDI users | 21 (22.6%) | 11 (22.0%) | 0.937 |
| Factor | OR | SE | p Value | 95%CI |
|---|---|---|---|---|
| Good self-assessment of inhalation technique | 1.50 | 0.15 | 0.08 | 1.12–2.02 |
| Deviations from regular use of inhaler during last 6 months | 0.83 | 0.09 | 0.03 | 0.70–0.98 |
| Use of MDI | 0.79 | 0.09 | 0.01 | 0.66–0.94 |
| Use of both types of inhalers | 1.00 | 0.01 | 0.99 | 0.84–1.20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domagała-Mańczyk, I.; Miszczuk-Cieśla, M.; Maskey-Warzęchowska, M.; Zielecki, M.; Szczudlik, P.; Dąbrowska, M. Expectations Versus Reality in Inhalation Technique—A Case–Control Study of Inhalation Technique in Patients with Asthma or COPD. J. Clin. Med. 2025, 14, 6848. https://doi.org/10.3390/jcm14196848
Domagała-Mańczyk I, Miszczuk-Cieśla M, Maskey-Warzęchowska M, Zielecki M, Szczudlik P, Dąbrowska M. Expectations Versus Reality in Inhalation Technique—A Case–Control Study of Inhalation Technique in Patients with Asthma or COPD. Journal of Clinical Medicine. 2025; 14(19):6848. https://doi.org/10.3390/jcm14196848
Chicago/Turabian StyleDomagała-Mańczyk, Izabela, Marta Miszczuk-Cieśla, Marta Maskey-Warzęchowska, Michał Zielecki, Piotr Szczudlik, and Marta Dąbrowska. 2025. "Expectations Versus Reality in Inhalation Technique—A Case–Control Study of Inhalation Technique in Patients with Asthma or COPD" Journal of Clinical Medicine 14, no. 19: 6848. https://doi.org/10.3390/jcm14196848
APA StyleDomagała-Mańczyk, I., Miszczuk-Cieśla, M., Maskey-Warzęchowska, M., Zielecki, M., Szczudlik, P., & Dąbrowska, M. (2025). Expectations Versus Reality in Inhalation Technique—A Case–Control Study of Inhalation Technique in Patients with Asthma or COPD. Journal of Clinical Medicine, 14(19), 6848. https://doi.org/10.3390/jcm14196848







