Comparative Outcomes of 1-Level vs. 2-Level Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
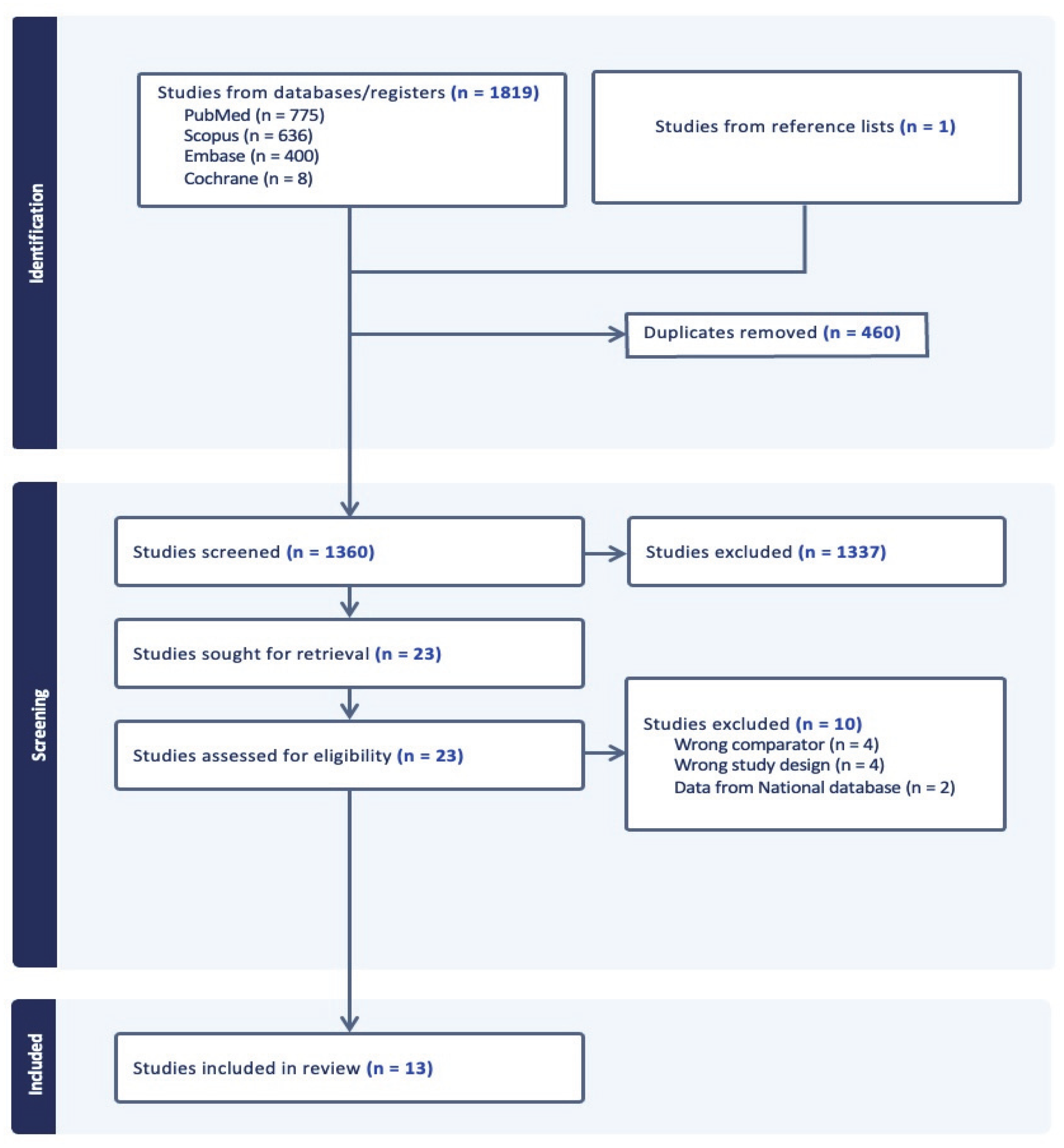
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Data and Statistical Analysis
2.5. Risk of Bias Assessment (RoB)
3. Results
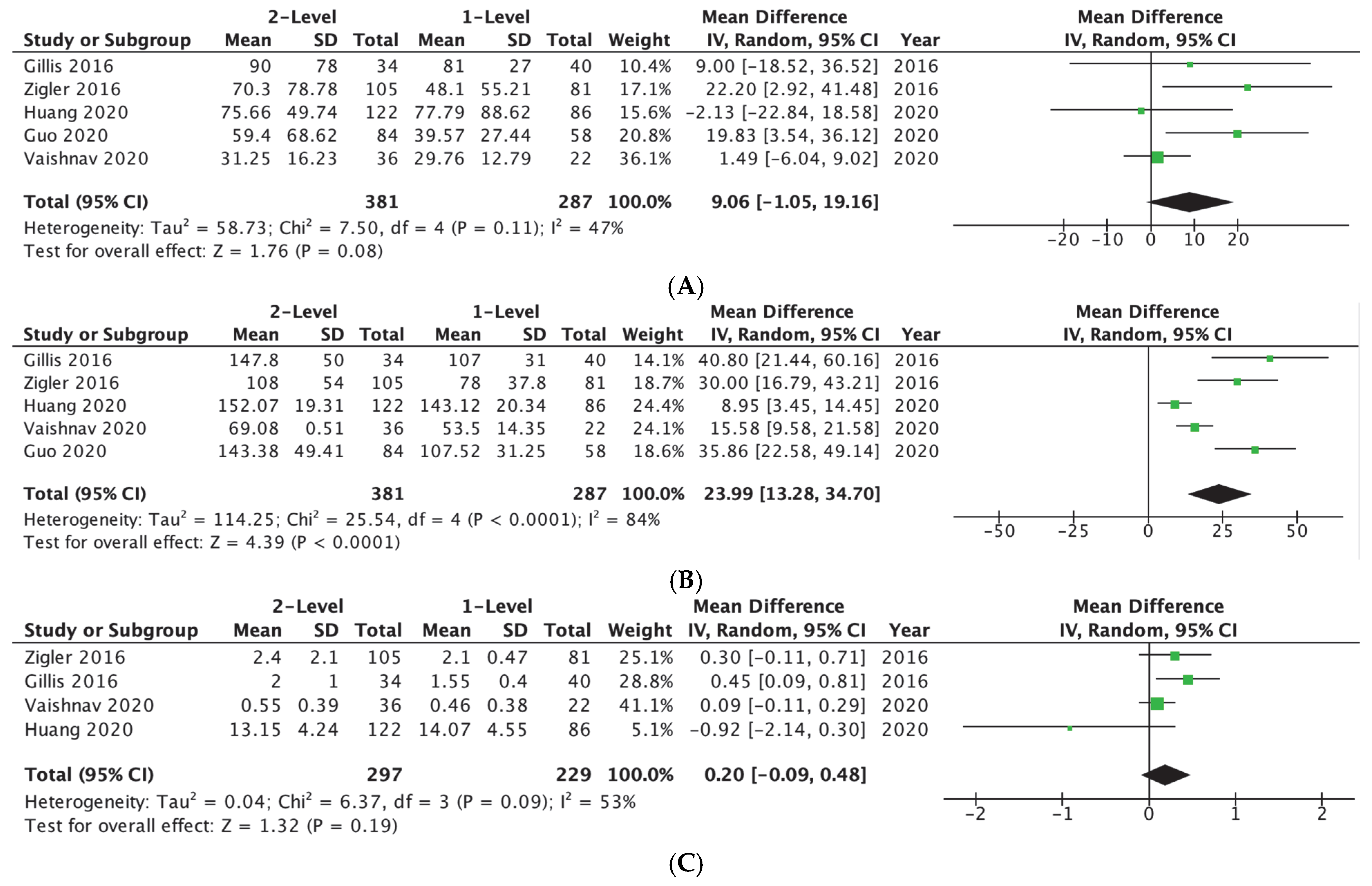
3.1. Surgery-Related Outcomes
3.2. Complications
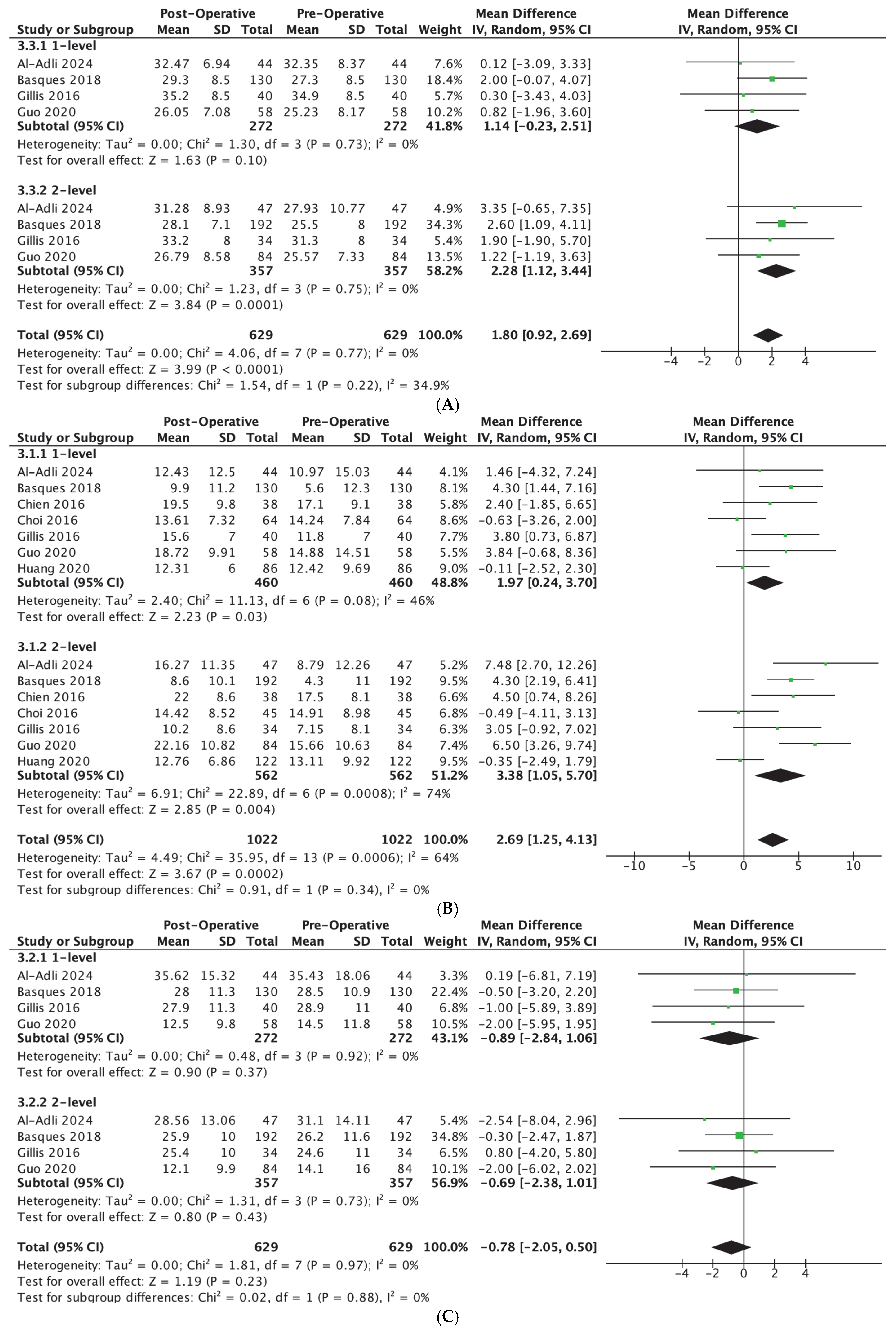
3.3. Radiographic Parameters
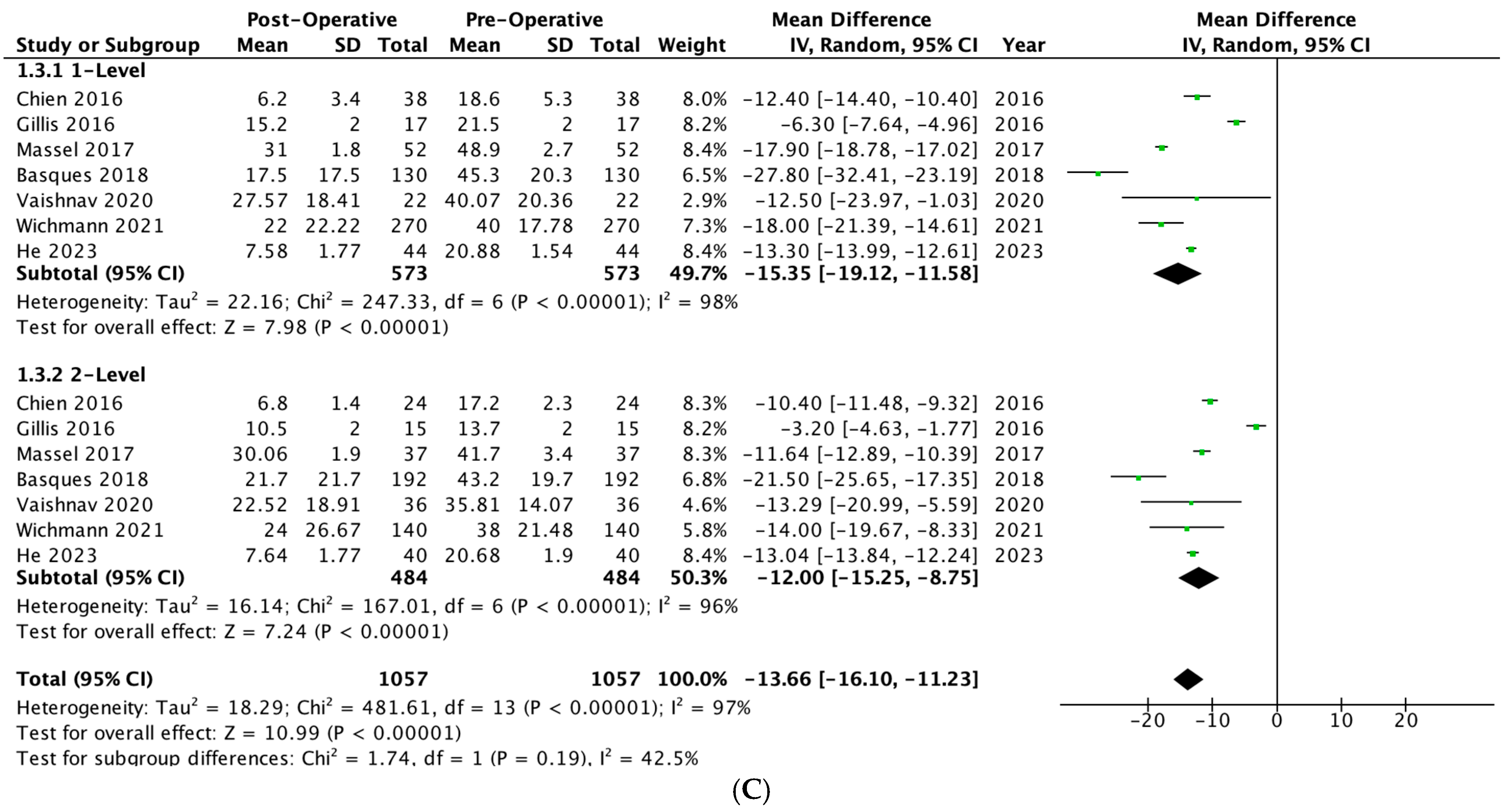
3.4. Patient-Reported Outcomes
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A


References
- Joo, P.Y.; Zhu, J.R.; Kammien, A.J.; Gouzoulis, M.J.; Arnold, P.M.; Grauer, J.N. Clinical outcomes following one-, two-, three-, and four-level anterior cervical discectomy and fusion: A national database study. Spine J. 2022, 22, 542–548. [Google Scholar] [CrossRef]
- Veeravagu, A.; Cole, T.; Jiang, B.; Ratliff, J.K. Revision rates and complication incidence in single- and multilevel anterior cervical discectomy and fusion procedures: An administrative database study. Spine J. 2014, 14, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Zigler, J.E.; Rogers, R.W.; Ohnmeiss, D.D. Comparison of 1-Level Versus 2-Level Anterior Cervical Discectomy and Fusion: Clinical and Radiographic Follow-Up at 60 Months. Spine 2016, 41, 463–469. [Google Scholar] [CrossRef]
- Matz, P.G.; Holly, L.T.; Groff, M.W.; Vresilovic, E.J.; Anderson, P.A.; Heary, R.F.; Kaiser, M.G.; Mummaneni, P.V.; Ryken, T.C.; Choudhri, T.F.; et al. Indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy. J. Neurosurg. Spine 2009, 11, 174–182. [Google Scholar] [CrossRef]
- Iyer, S.; Kim, H.J. Cervical radiculopathy. Curr. Rev. Musculoskelet. Med. 2016, 9, 272–280. [Google Scholar] [CrossRef]
- Basques, B.A.; Louie, P.K.; Mormol, J.; Khan, J.M.; Movassaghi, K.; Paul, J.C.; Varthi, A.; Goldberg, E.J.; An, H.S. Multi- versus single-level anterior cervical discectomy and fusion: Comparing sagittal alignment, early adjacent segment degeneration, and clinical outcomes. Eur. Spine J. 2018, 27, 2745–2753. [Google Scholar] [CrossRef]
- Chien, A.; Lai, D.M.; Wang, S.F.; Hsu, W.L.; Cheng, C.H.; Wang, J.L. Comparison of Cervical Kinematics, Pain, and Functional Disability Between Single- and Two-level Anterior Cervical Discectomy and Fusion. Spine 2016, 41, E915–E922. [Google Scholar] [CrossRef]
- Neifert, S.N.; Martini, M.L.; Yuk, F.; McNeill, I.T.; Caridi, J.M.; Steinberger, J.; Oermann, E.K. Predicting Trends in Cervical Spinal Surgery in the United States from 2020 to 2040. World Neurosurg. 2020, 141, e175–e181. [Google Scholar] [CrossRef]
- Ibrahim, M.T.; Kirven, J.C.; Kavuri, V.; Yu, E.; Singh, V.K. Trends in Cervical Spine Surgery in the United States: A National Database Analysis. World Neurosurg. 2025, 198, 123961. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Lu, S.; Kong, C.; Li, X.; Liu, C. Comparison of Clinical Outcomes and Sagittal Alignment After Different Levels of Anterior Cervical Discectomy and Fusion in Patients with Cervical Spondylotic Myelopathy: From One-level to Three-level. Spine 2021, 46, E153–E160. [Google Scholar] [CrossRef]
- He, P.; Wang, M.; Li, D.; Zheng, L.; Yuan, H.; Yang, Y.; Wang, J.; He, Q.; Feng, D.; Liu, X. Comparison of Flexion Relaxation Phenomenon After Single-Level and Multi-Level Anterior Cervical Discectomy and Fusion. World Neurosurg. 2023, 178, e265–e274. [Google Scholar] [CrossRef] [PubMed]
- Riley, L.H.; Skolasky, R.L.; Albert, T.J.; Vaccaro, A.R.; Heller, J.G. Dysphagia after anterior cervical decompression and fusion: Prevalence and risk factors from a longitudinal cohort study. Spine 2005, 30, 2564–2569. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.K.; Kim, S.B.; Park, C.K.; Kim, S.M. Comparison of the clinical and radiologic outcomes obtained with single- versus two-level anterior cervical decompression and fusion using stand-alone PEEK cages filled with allograft. Acta Neurochir. 2016, 158, 481–487. [Google Scholar] [CrossRef]
- Gillis, C.C.; Kaszuba, M.C.; Traynelis, V.C. Cervical radiographic parameters in 1- and 2-level anterior cervical discectomy and fusion. J. Neurosurg. Spine 2016, 25, 421–429. [Google Scholar] [CrossRef]
- Massel, D.H.; Mayo, B.C.; Bohl, D.D.; Narain, A.S.; Hijji, F.Y.; Fineberg, S.J.; Louie, P.K.; Basques, B.A.; Long, W.W.; Modi, K.D.; et al. Improvements in Neck and Arm Pain Following an Anterior Cervical Discectomy and Fusion. Spine 2017, 42, E825–E832. [Google Scholar] [CrossRef]
- Vaishnav, A.S.; Saville, P.; McAnany, S.; Haws, B.; Singh, K.; Iyer, S.; Albert, T.; Gang, C.H.; Qureshi, S.A. Is the likelihood of dysphagia different in patients undergoing one-level versus two-level anterior cervical discectomy and fusion? Spine J. 2020, 20, 737–744. [Google Scholar] [CrossRef]
- Huang, C.; Abudouaini, H.; Wang, B.; Ding, C.; Meng, Y.; Yang, Y.; Wu, T.; Liu, H. Comparison of Patient-Reported Postoperative Dysphagia in Patients Undergoing One-Level Versus Two-Level Anterior Cervical Discectomy and Fusion with the Zero-P Implant System. Dysphagia 2021, 36, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Wichmann, T.O.; Bech-Azeddine, R.; Norling, A.L.; Einarsson, H.B.; Rasmussen, M.M. Comparison of outcomes and complications between one- and two-level anterior cervical discectomy and fusion: A population-based study of 410 patients. Br. J. Neurosurg. 2024, 38, 928–933. [Google Scholar] [CrossRef]
- Al-Adli, N.N.; Tummala, S.; Oh, M.C. Early radiographic outcomes after anterior cervical discectomy and fusion with anatomic versus lordotic cages. N. Am. Spine Soc. J. 2024, 17, 100292. [Google Scholar] [CrossRef]
- Tani, S.; Okano, I.; Dodo, Y.; Camino-Willhuber, G.; Caffard, T.; Schönnagel, L.; Chiapparelli, E.; Amoroso, K.; Tripathi, V.B.; Arzani, A.B.; et al. Risk Factors for Unexpected Conversion From Ambulatory to Inpatient Admission Among One-level or Two-level ACDF Patients. Spine 2023, 48, 1427–1435. [Google Scholar] [CrossRef]
- Karcz, M.; Papadakos, P.J. Respiratory complications in the postanesthesia care unit: A review of pathophysiological mechanisms. Can. J. Respir. Ther. 2013, 49, 21–29. [Google Scholar]
- Phan, K.; Kim, J.S.; Kim, J.H.; Somani, S.; Di’cApua, J.; Dowdell, J.E.; Cho, S.K. Anesthesia Duration as an Independent Risk Factor for Early Postoperative Complications in Adults Undergoing Elective ACDF. Glob. Spine J. 2017, 7, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Childers, C.P.; Maggard-Gibbons, M. Understanding Costs of Care in the Operating Room. JAMA Surg. 2018, 153, e176233. [Google Scholar] [CrossRef] [PubMed]
- Xue, R.; Ji, Z.Y.; Cheng, X.D.; Zhang, Z.Q.; Zhang, F. Risk Factors for Dysphagia after Anterior Cervical Discectomy and Fusion with the Zero-P implant system: A Study with Minimum of 2 Years Follow-up. Orthop. Surg. 2022, 14, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Balmaceno-Criss, M.; Anderson, G.; Parhar, K.; Daher, M.; Gregorczyk, J.; Liu, J.; McDonald, C.L.; Diebo, B.G.; Daniels, A.H. Anterior cervical discectomy and fusion versus cervical disc arthroplasty: An epidemiological review of 433,660 surgical patients from 2011 to 2021. Spine J. 2024, 24, 1342–1351. [Google Scholar] [CrossRef]
- Joseph, J.R.; Smith, B.W.; Mummaneni, P.V.; La Marca, F.; Park, P. Postoperative dysphagia correlates with increased morbidity, mortality, and costs in anterior cervical fusion. J. Clin. Neurosci. 2016, 31, 172–175. [Google Scholar] [CrossRef]
- Yue, W.M.; Brodner, W.; Highland, T.R. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: A 5- to 11-year follow-up study. Eur. Spine J. 2005, 14, 677–682. [Google Scholar] [CrossRef]
- Logemann, J.A.; Larsen, K. Oropharyngeal dysphagia: Pathophysiology and diagnosis for the anniversary issue of Diseases of the Esophagus. Dis. Esophagus 2012, 25, 299–304. [Google Scholar] [CrossRef]
- Qi, M.; Chen, H.; Liu, Y.; Zhang, Y.; Liang, L.; Yuan, W. The use of a zero-profile device compared with an anterior plate and cage in the treatment of patients with symptomatic cervical spondylosis: A preliminary clinical investigation. Bone Jt. J. 2013, 95-B, 543–547. [Google Scholar] [CrossRef]
- Passias, P.G.; Horn, S.R.; Oh, C.; Ramchandran, S.; Burton, D.C.; Lafage, V.; Lafage, R.; Poorman, G.W.; Steinmetz, L.; International Spine Study Group (ISSG); et al. Evaluating cervical deformity corrective surgery outcomes at 1-year using current patient-derived and functional measures: Are they adequate? J. Spine Surg. 2018, 4, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, N.; Zhou, J.; Li, H.; Du, X.; He, H.; Rong, P.; Wang, W.; Liu, Y. Effect of cervical alignment change after anterior cervical fusion on radiological adjacent segment pathology. Quant. Imaging Med. Surg. 2022, 12, 2464–2473. [Google Scholar] [CrossRef] [PubMed]
- Łosiński, K.; Bryndal, A.; Grochulska, A.; Nawos-Wysocki, W.; Glowinski, S. Assessment of lumbosacral spinal curvatures before and after surgery using 3D posturography. Sci. Rep. 2025, 15, 16126. [Google Scholar] [CrossRef] [PubMed]
- Liu, E.; Persad, A.R.L.; Baron, N.; Fourney, D.R. Long-Term (>24 Months) Duration of Symptoms Negatively Impacts Patient-Reported Outcomes Following Anterior Cervical Discectomy and Fusion for Cervical Radiculopathy. Spine 2024, 49, 519–529. [Google Scholar] [CrossRef]
- De Simone, M.; Amoroso, E.; Iaconetta, G. Letter to the Editor Regarding “Does Bone Preservation at the Anterior Edge of the Vertebral Body Affect the Subsidence of Zero-Profile Cages After Anterior Cervical Discectomy and Fusion?”. World Neurosurg. 2025, 195, 123665. [Google Scholar] [CrossRef]
| Author Year | Study Design | Indication for Surgery | Number of Levels Fused | Number of Participants | Mean Age ± SD (Years) | Sex | Mean BMI ± SD (kg/m2) | Last Follow-Up Time Point (Months) |
|---|---|---|---|---|---|---|---|---|
| Riley 2005 [13] | Retrospective Study | Myelopathy or Radiculopathy | 1-level | 149 | 48.2 ± 10.74 | 134 M, 122 F | NR | 24 |
| 2-level | 107 | |||||||
| Chien 2016 [7] | Prospective Study | Myelopathy or Radiculopathy | 1-level | 38 | 53.4 ± 12.0 | 21 M, 17 F | NR | 12 |
| 2-level | 24 | 56.3 ± 10.4 | 15 M, 9 F | NR | ||||
| Zigler 2016 [3] | Randomized controlled trial | Myelopathy or Radiculopathy | 1-level | 81 | 44.0 ± 8.21 | 36 M, 45 F | 27.4 ± 4.18 | 24 |
| 2-level | 105 | 46.2 ± 7.99 | 45 M, 60 F | 28.1 ± 4.19 | ||||
| Choi 2016 [14] | Retrospective Study | Spondylotic Myelopathy | 1-level | 64 | 52.2 ± 14.0 | 44 M, 20 F | NR | 12 |
| 2-level | 45 | 54.2 ± 17.1 | 27 M, 18 F | NR | ||||
| Gillis 2016 [15] | Retrospective Study | Myelopathy or Radiculopathy or Spondylosis | 1-level | 40 | 52.0 ± 9.33 | 37 M, 37 F | 27.1 ± 1 | 12 |
| 2-level | 34 | |||||||
| Massel 2017 [16] | Retrospective Study | Spondylosis or Spondylolisthesis or Herniated Nucleus Pulposus | 1-level | 52 | 49.7 ± 8.8 | 50 M, 49 F | NR | 12 |
| 2-level | 37 | |||||||
| Basques 2018 [6] | Retrospective Study | Myelopathy or Radiculopathy | 1-level | 130 | 46.6 ± 11.9 | 61 M, 69 F | 28.4 ± 6.0 | 28 |
| 2-level | 192 | 50.2 ± 10.0 | 97 M, 95 F | 28.2 ± 6.1 | ||||
| Guo 2020 [11] | Prospective study | Myelopathy | 1-level | 58 | 51.93 ± 8.90 | 33 M, 25 F | 24.80 ± 3.06 | 12 |
| 2-level | 84 | 57.05 ± 9.89 | 47 M, 37 F | 24.54 ± 3.29 | ||||
| Vaishnav 2020 [17] | Retrospective Study | Myelopathy or Radiculopathy | 1-level | 22 | 48.06 ± 10.68 | 13 M, 9 F | 29.13 ± 5.18 | 3 |
| 2-level | 36 | 54.17 ± 8.67 | 14 M, 2 F | 28.65 ± 6.29 | ||||
| Huang 2020 [18] | Retrospective Study | Myelopathy or Radiculopathy | 1-level | 86 | 51.47 ± 11.46 | 52 M, 34 F | 24.16 ± 2.88 | 18 ± 3.46 |
| 2-level | 122 | 52.39 ± 8.68 | 70 M, 52 F | 23.82 ± 3.31 | ||||
| Wichmann 2021 [19] | Retrospective Study | Radiculopathy | 1-level | 270 | 52 ± 10 | 124 M, 146 F | NR | 12 |
| 2-level | 140 | 55 ± 9.8 | 67 M, 73 F | |||||
| He 2023 [12] | Prospective Study | Spondylosis | 1-level | 44 | 52.79 ± 5.55 | 26 M, 18 F | 23.19 ± 2.49 | 12 |
| 2-level | 40 | 54 ± 5.94 | 22 M, 18 F | 22.08 ± 2.70 | ||||
| Al-Adli 2024 [20] | Retrospective Study | Myelopathy or Radiculopathy | 1-level | 44 | 59.9 ± 9.1 | 18 M, 73 F | 30.5 ± 5.7 | 2.6 ± 0.96 |
| 2-level | 47 |
| Surgery-Related Outcomes | Mean Difference [95% CI] | p-Value |
| EBL | 9.06 [−1.05, 19.16] mL | 0.08 |
| OR time | 23.99 [13.28, 34.70] min | <0.001 |
| LOS | 0.20 [−0.09, 0.48] days | 0.19 |
| Complications | Odds Ratio [95% CI] | p-value |
| Dysphagia | 1.75 [1.00, 3.08] | 0.05 |
| Adjacent segment disease | 0.91 [0.34, 2.43] | 0.85 |
| Revision surgery | 1.72 [0.78, 3.79] | 0.18 |
| Mean Postoperative Scores (Mean ± SD) | |||
|---|---|---|---|
| Radiographic Parameters | 1-Level | 2-Level | p-value |
| cSVA | 25.91 ± 13.90 | 22.96 ± 12.04 | 0.005 |
| Cervical lordosis | 13.79 ± 10.63 | 13.64 ± 10.65 | 0.83 |
| Patient-reported outcomes | 1-Level | 2-Level | p-value |
| VAS arm | 1.54 ± 3.07 | 2.11 ± 3.3 | 0.005 |
| VAS neck | 2.07 ± 2.89 | 2.16 ± 3.22 | 0.59 |
| NDI | 19.65 ± 18.89 | 20.8 ± 21.33 | 0.35 |
| 1-Level | 2-Level | |||
| Radiographic Parameters | Mean Difference [95% CI] | p-Value | Mean Difference [95% CI] | p-Value |
| Cervical lordosis | 1.97 [0.24, 3.70] | 0.03 | 3.38 [1.05, 5.70] | <0.01 |
| cSVA | −0.89 [−2.84, 1.06] | 0.37 | −0.69 [−2.38, 1.01] | 0.43 |
| Patient-reported outcomes | Mean Difference [95% CI] | p-value | Mean Difference [95% CI] | p-value |
| VAS arm | −4.06 [−5.11, −3.01] | <0.01 | −3.40 [−4.55, −2.25] | <0.01 |
| VAS neck | −4.12 [−4.93, −3.32] | <0.01 | −3.57 [−4.53, −2.62] | <0.01 |
| NDI | −15.35 [−19.12, −11.58] | <0.01 | −12.00 [−16.10, −11.23] | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nassar, J.E.; Knebel, A.; Singh, M.; Farias, M.J.; Carayannopoulos, N.L.; Chisango, Z.M.; Fani, N.; Daher, M.; Kuris, E.O.; Diebo, B.G.; et al. Comparative Outcomes of 1-Level vs. 2-Level Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 6788. https://doi.org/10.3390/jcm14196788
Nassar JE, Knebel A, Singh M, Farias MJ, Carayannopoulos NL, Chisango ZM, Fani N, Daher M, Kuris EO, Diebo BG, et al. Comparative Outcomes of 1-Level vs. 2-Level Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(19):6788. https://doi.org/10.3390/jcm14196788
Chicago/Turabian StyleNassar, Joseph E., Ashley Knebel, Manjot Singh, Michael J. Farias, Nicolas L. Carayannopoulos, Zvipo M. Chisango, Negin Fani, Mohammad Daher, Eren O. Kuris, Bassel G. Diebo, and et al. 2025. "Comparative Outcomes of 1-Level vs. 2-Level Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 19: 6788. https://doi.org/10.3390/jcm14196788
APA StyleNassar, J. E., Knebel, A., Singh, M., Farias, M. J., Carayannopoulos, N. L., Chisango, Z. M., Fani, N., Daher, M., Kuris, E. O., Diebo, B. G., & Daniels, A. H. (2025). Comparative Outcomes of 1-Level vs. 2-Level Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(19), 6788. https://doi.org/10.3390/jcm14196788







