Correction of Anterior Open Bite Using Temporary Anchorage Devices: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Information Sources
- P (Patients): Patients with anterior open bite
- I (Intervention): Molar intrusion using temporary anchorage devices
- C (Comparison): Other treatment modalities for correcting open bite, such as orthognathic surgery
- O (Outcomes): Molar intrusion with TADs as an effective and less invasive technique, associated with lower risk and faster recovery.
2.3. Search Strategy
2.4. Eligibility Criteria
- Articles published within the last 10 years
- Articles written in English or Spanish
- Randomized controlled trials (RCTs), cohort studies, case-control studies, and case series
- Human studies
- Systematic reviews and meta-analyses
2.5. Data Extraction
2.6. Study Selection and Variables
2.7. Risk of Bias
- 1.
- Bias arising from the randomization process
- 2.
- Bias due to deviations from intended interventions
- 3.
- Bias due to missing outcome data
- 4.
- Bias in measurement of the outcome
- 5.
- Bias in selection of the reported result
- 1.
- Confounding
- 2.
- Selection of participants
- 3.
- Classification of interventions
- 4.
- Deviations from intended interventions
- 5.
- Missing data
- 6.
- Measurement of outcomes
- 7.
- Selection of the reported result
2.8. Data Synthesis and Statistical Analysis
3. Results
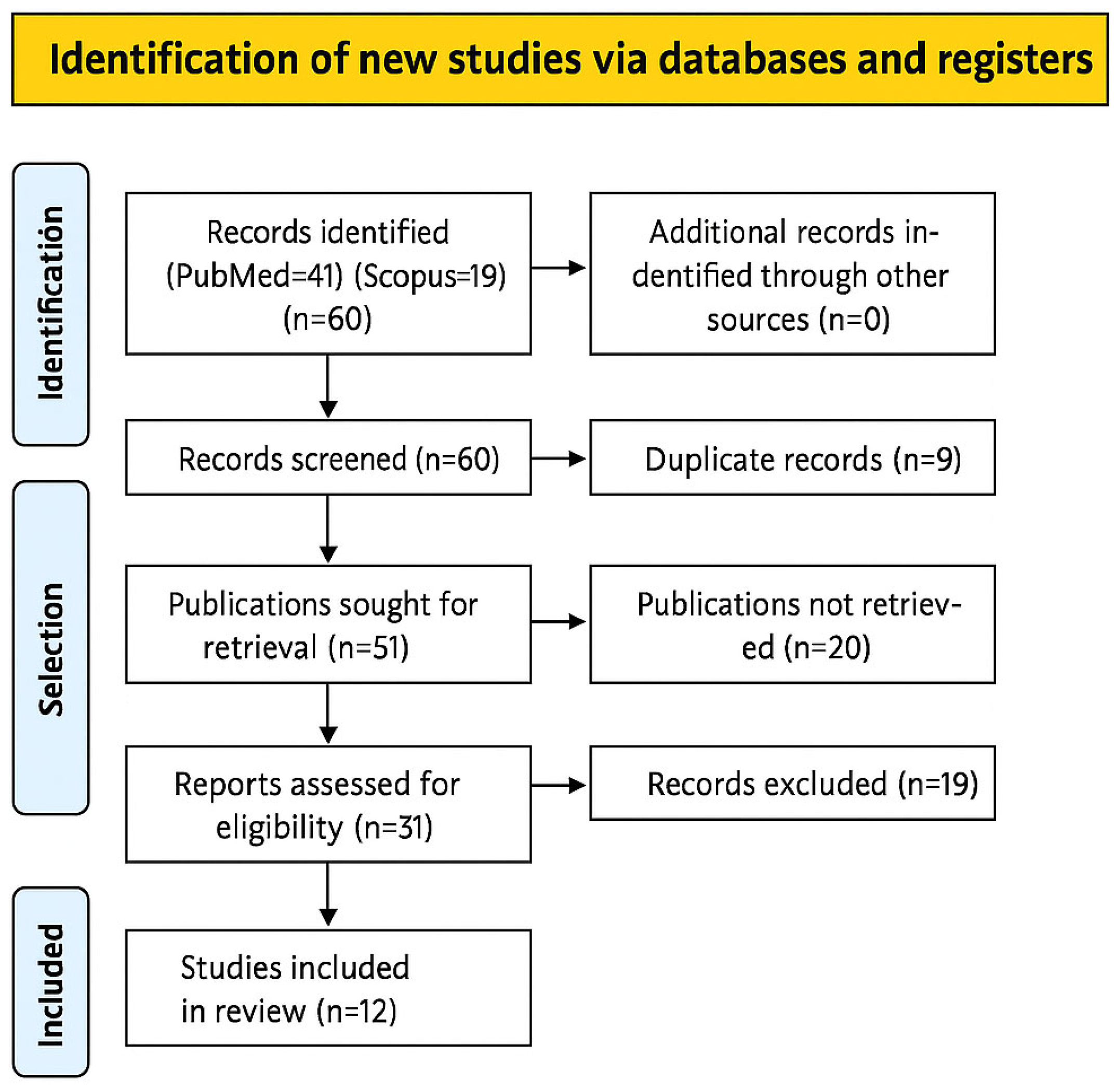
3.1. Study Selection Characteristics
3.2. Results of Individual Studies
3.3. Quality Assessment
- A predominance of observational studies with moderate risk of bias, as evaluated through ROBINS-I and JBI tools.
- Limited consistency in reported outcomes, with intrusion values ranging from 1.0 mm to 3.1 mm.
- Sample size variability and occasional absence of confidence intervals, affecting precision.
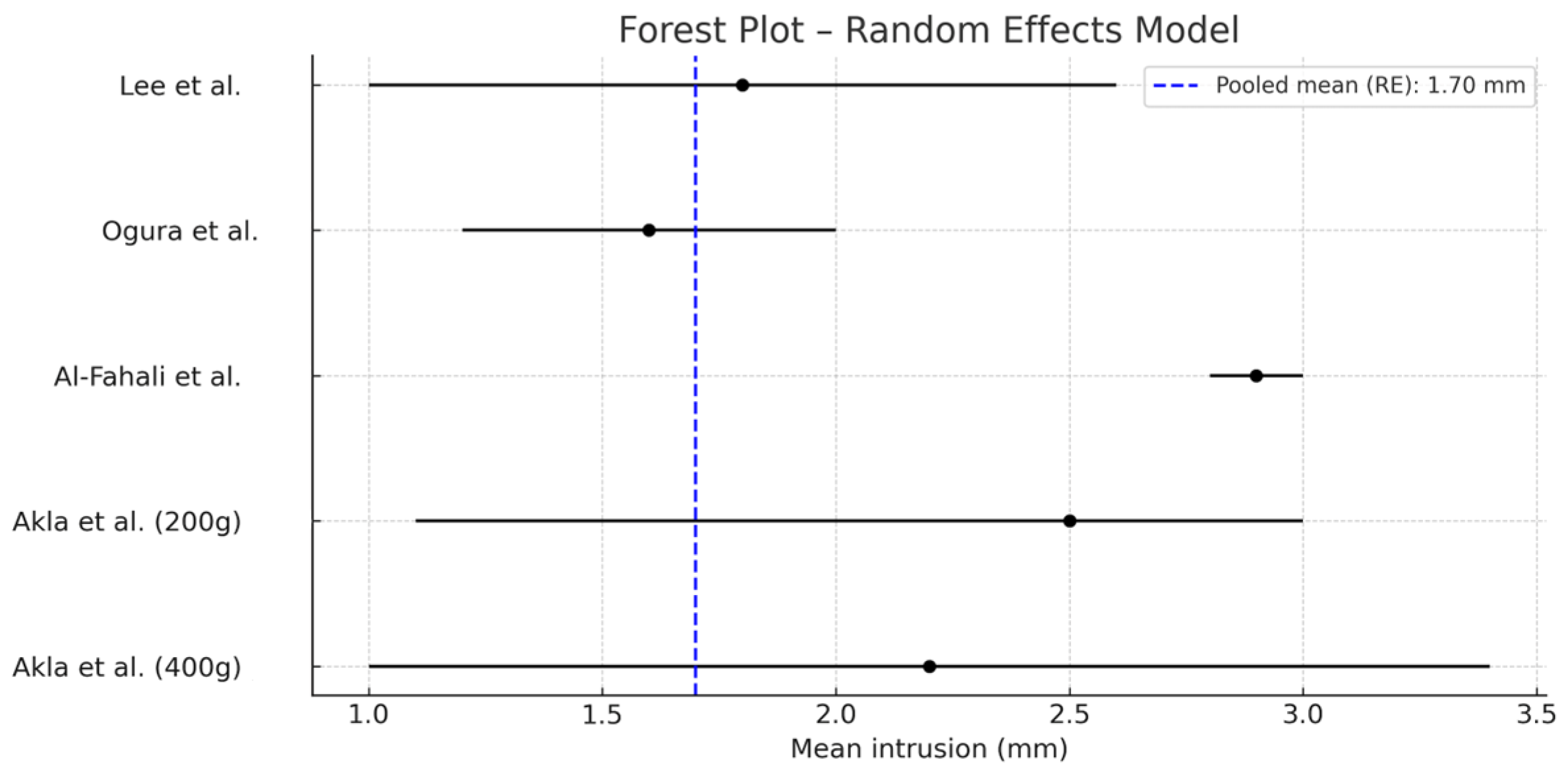
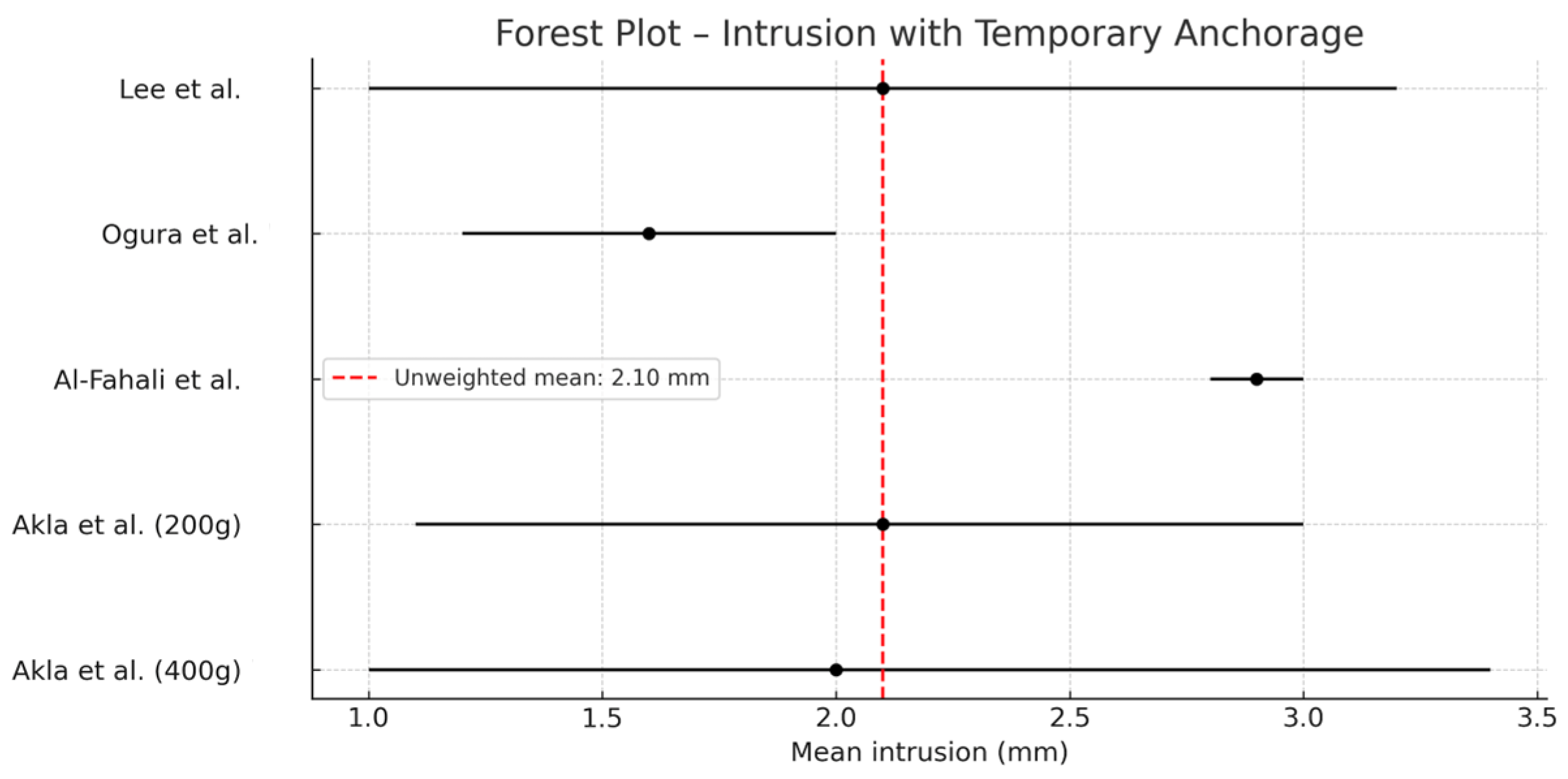
3.4. Quantitative Synthesis
- 1.
- Pooled mean calculation (Figure 4):
- 2.
- 95% confidence interval (CI) estimation (Figure 5):
- 3.
- Heterogeneity analysis:
- Cochran’s Q test: Quantified observed variability among studies.
- I2 statistic: Represented the percentage of variability attributable to true heterogeneity rather than chance. An I2 > 75% indicates high heterogeneity.
4. Discussion
5. Conclusions
- -
- Temporary anchorage devices (TADs) are an effective and safe tool for molar intrusion in the treatment of anterior open bite, particularly in adult patients.
- -
- Comparison between different placement techniques shows that both interradicular miniscrews and zygomatic miniplates can be effective, provided they are applied using well-controlled mechanical protocols.
- -
- Regarding clinical protocols, evidence supports individualized planning. Nevertheless, the most stable outcomes with fewer complications are associated with light forces, segmented arch mechanics, and TADs placed in biomechanically safe areas such as the palate or buccal interradicular region, following prior cephalometric evaluation.
- -
- The meta-analysis revealed a mean molar intrusion of 1.7 mm, which is clinically significant. However, the high heterogeneity among studies highlights the need for further research to determine the achievable degree of intrusion and to define optimal force protocols, as excessive forces do not proportionally increase intrusion and may compromise outcomes.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TADs | Dispositivos de anclaje temporal |
| MAA | Mordida Abierta Anterior |
References
- Omidkhoda, M.; Bardideh, E.; Jahanbin, A.; Zarei, M. Effects of posterior intrusion using skeletal anchorage on treating anterior open bite: A systematic review and meta-analysis. J. Dent. Res. Dent. Clin. Dent. Prospect. 2023, 17, 196–210. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Popov, M.; Marinkovic, N.; Arsic, I.; Janosevic, P.; Nedeljkovic, N. Treatment of Open Bite Based on Skeletal Anchorage Using Extrusion Lever Arms and Class III Elastics. Case Rep. Dent. 2024, 2024, 7768109. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alsafadi, A.S.; Alabdullah, M.M.; Saltaji, H.; Abdo, A.; Youssef, M. Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: A systematic review. Prog. Orthod. 2016, 17, 9. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaku, M.; Kawai, A.; Koseki, H.; Abedini, S.; Kawazoe, A.; Sasamoto, T.; Sunagawa, H.; Yamamoto, R.; Tsuka, N.; Motokawa, M.; et al. Correction of severe open bite using miniscrew anchorage. Aust. Dent. J. 2009, 54, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Foot, R.; Dalci, O.; Gonzales, C.; Tarraf, N.E.; Darendeliler, M.A. The short-term skeleto-dental effects of a new spring for the intrusion of maxillary posterior teeth in open bite patients. Prog. Orthod. 2014, 15, 56. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Malara, P.; Bierbaum, S.; Malara, B. Outcomes and Stability of Anterior Open Bite Treatment with Skeletal Anchorage in Non-Growing Patients and Adults Compared to the Results of Orthognathic Surgery Procedures: A Systematic Review. J. Clin. Med. 2021, 10, 5682. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Mesquita, E.V.; Meloti, F.; Silva, E.; de Almeida Cardoso, M.; An, T.L.; do Carmo Chagas Nascimento, M. Craniomandibular transverse tomographic evaluation after anterior open bite orthodontic treatment with miniplates anchorage. Prog. Orthod. 2024, 25, 19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ogura, H.; Numazaki, K.; Oyanagi, T.; Seiryu, M.; Ito, A.; Noguchi, T.; Ohori, F.; Yoshida, M.; Fukunaga, T.; Kitaura, H.; et al. Three-Dimensional Evaluation of Treatment Effects and Post-Treatment Stability of Maxillary Molar Intrusion Using Temporary Anchorage Devices in Open Bite Malocclusion. J. Clin. Med. 2024, 13, 2753. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Umalkar, S.S.; Jadhav, V.V.; Paul, P.; Reche, A. Modern Anchorage Systems in Orthodontics. Cureus 2022, 14, e31476. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iwasa, A.; Horiuchi, S.; Kinouchi, N.; Izawa, T.; Hiasa, M.; Kawai, N.; Yasue, A.; Hassan, A.H.; Tanaka, E. Skeletal anchorage for intrusion of bimaxillary molars in a patient with skeletal open bite and temporomandibular disorders. J. Orthod. Sci. 2017, 6, 152–158. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tavares, C.A.E.; Allgayer, S. Open bite in adult patients. Dent. Press J. Orthod. 2019, 24, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Al-Falahi, B.; Hafez, A.M.; Fouda, M. Three-dimensional assessment of external apical root resorption after maxillary posterior teeth intrusion with miniscrews in anterior open bite patients. Dent. Press J. Orthod. 2018, 23, 56–63. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akl, H.E.; Abouelezz, A.M.; El Sharaby, F.A.; El-Beialy, A.R.; El-Ghafour, M.A. Force magnitude as a variable in maxillary buccal segment intrusion in adult patients with skeletal open bite. Angle Orthod. 2020, 90, 507–515. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akl, H.E.; El-Beialy, A.R.; El-Ghafour, M.A.; Abouelezz, A.M.; El Sharaby, F.A. Root resorption associated with maxillary buccal segment intrusion using variable force magnitudes. Angle Orthod. 2021, 91, 733–742. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, J.; Choi, Y.J.; Park, J.H.; Chung, C.J.; Lee, J.H.; Kim, K.H. Surgical vs nonsurgical treatments in patients with anterior open-bite have similar effects in occlusal function: A 2-year follow-up study. Am. J. Orthod. Dentofac. Orthop. 2024, 165, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Marzouk, E.S.; Abdallah, E.M.; El-Kenany, W.A. Molar Intrusion in Open-bite Adults Using Zygomatic Miniplates. Int. J. Orthod. 2015, 26, 47–54. [Google Scholar] [PubMed]
- Marzouk, E.S.; Kassem, H.E. Evaluation of long-term stability of skeletal anterior open bite correction in adults treated with maxillary posterior segment intrusion using zygomatic miniplates. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Peres, L.R.; Rossouw, P.E.; Cousley, R.; Corsetti, M.A. Mini-implant assisted posterior intrusion: A quantification of anterior bite closure in nongrowing subjects. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Akan, B.; Ünal, B.K.; Şahan, A.O.; Kızıltekin, R. Evaluation of anterior open bite correction in patients treated with maxillary posterior segment intrusion using zygomatic anchorage. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Lo-Cao, D.; Pandis, N.; Darendeliler, M.A.; Papadopoulou, A.K. A 3-dimensional comparative assessment of the dentoskeletal effects of clear aligners vs temporary skeletal anchorage device-assisted posterior intrusion in adolescents with anterior open bite: A single-center, retrospective, cohort study. Am. J. Orthod. Dentofac. Orthop. 2025, 167, 345–361. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.N.; Cui, S.J.; Liu, Y.; Fu, Y.; Zhang, J.N.; Zhou, Y.H.; Wang, X.D. Quantitative evaluation of vertical control in orthodontic camouflage treatment for skeletal class II with hyperdivergent facial type. Head Face Med. 2024, 20, 31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaku, M.; Yamamoto, T.; Yashima, Y.; Izumino, J.; Kagawa, H.; Ikeda, K.; Tanimoto, K. Correction of skeletal class II severe open bite with temporomandibular joint disorder treated by miniscrew anchorage and molar extraction: A case report. J. Med. Case Rep. 2019, 13, 207. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Jun, H.; Yoon, S.H.; Roh, M.; Kim, S.H.; Lee, J.; Lee, J.; Kwon, M.; Leem, J. Quality assessment and implications for further study of acupotomy: Case reports using the case report guidelines and the Joanna Briggs Institute critical appraisal checklist. J. Acupunct. Res. 2021, 38, 122–133. [Google Scholar] [CrossRef]
- Molina Arias, M. Aspectos metodológicos del metaanálisis (2). Rev. Pediatr. Aten. Primaria 2018, 20, 401–405. [Google Scholar]

| Patients | Intervention | Comparison | Outcomes |
|---|---|---|---|
#1 Humans [MeSH] | #3 Orthodontic anchorage devices [MeSH] Skeletal anchorage Bone screws [MeSH] OR | #5 Efficiency Efectiveness Amount intrusion OR | |
#2 Open bite [MeSH] Dolichofacial Vertical malocclusion Vertical dysplasia OR | |||
| #4 Tooth intrusion [MeSH] | |||
| #1AND #2AND#3AND#4AND #5 = #6 | |||
| Author, Year (Journal) | Study Design | Sample Size | Technique | Treatment Duration | Molar Intrusion (mm) | Overbite Increase (mm) | Type of TAD | |
|---|---|---|---|---|---|---|---|---|
| 1 | Ogura et al., 2024 [8] | Retrospective non-randomized clinical study | 10 | Maxillary molar intrusion with micro-implants | 7.1 months (intrusion) + 3.1 years (total) | 1.6 | 4.1 | Mini-implants |
| 2 | Al-Falahi et al., 2018 [12] | Non-randomized clinical trial | 15 | Maxillary molar intrusion with mini-implants | 5.1 ± 1.3 months | 2.79 ± 0.46 | Not reported | Mini-implants |
| 3 | Akl et al., 2021 [13] | Randomized clinical trial | 20 | Maxillary molar intrusion with mini-implants and root resorption evaluation | 6 months | Not reported | Not reported | Mini-implants |
| 4 | Akl et al., 2020 [14] | Randomized clinical trial | 20 | Maxillary molar intrusion with mini-implants (200 g vs. 400 g force) | 6 months | 2.42 (200 g), 2.26 (400 g) | 2.24 (200 g), 3.15 (400 g) | Mini-implants |
| 5 | Lee et al., 2024 [15] | Cohort study | 56 | Maxillary molar intrusion with mini-implants vs. orthognathic surgery | 5.2 ± 1.3 months | 1.7 | 4.0 (−0.9 mm after 2 years) | Mini-implants |
| 6 | Marzouk et al., 2015 [16] | Non-randomized clinical trial | 13 | Maxillary molar intrusion with zygomatic miniplates | 9 ± 2.5 months | 3.1 ± 0.74 | 6.55 ± 1.83 | Zygomatic miniplates |
| 7 | Marzouk et al., 2016 [17] | Cohort study | 26 | Maxillary molar intrusion with zygomatic miniplates | 4 years | 3.04 | 6.93 | Zygomatic miniplates |
| 8 | Peres et al., 2023 [18] | Cohort study | 53 | Maxillary molar intrusion with mini-implants | Variable | 2.67 | 3.6 | Mini-implants |
| 9 | Akan et al., 2020 [19] | Cohort study | 19 | Maxillary molar intrusion with zygomatic miniplates and acrylic appliance | 9.4 ± 0.7 months | 2.32 | 2.48 | Zygomatic miniplates |
| 10 | Lo-Cao et al., 2025 [20] | Cohort study | 29 | Invisalign vs. intrusion with TADs (Sydney Intrusion Spring) | 28.7 ± 3.9 months | 2.09–2.98 | 2.03–2.87 | Mini-implants with SIS |
| 11 | Guo et al., 2024 [21] | Cohort study | 36 | Maxillary molar intrusion with TADs | Variable | 2.25 | Variable | Mini-implants |
| 12 | Kaku et al., 2019 [22] | Case report | 1 | Molar intrusion with mini-implants and molar extraction | 36 months | 1 | Improved from −6.0 to 1.5 mm | Palatal mini-implants |
| 1 | 3 | 4 | 5 | 6 | 8 | 9 | 10 | 12 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Confounding Bias | |||||||||
| a. Were the inclusion and exclusion criteria clearly described? | |||||||||
| b. Were the participants selected in an appropriate and unbiased manner? | |||||||||
| c. Were relevant confounding variables considered and adjusted for? | |||||||||
| 2. Intervention Classification Bias | |||||||||
| a. Was the classification of the intervention blinded for participants and outcome assessors? | |||||||||
| b. Are the methods used to classify the intervention clearly described? | |||||||||
| c. Were the classification methods applied consistently across all participants? | |||||||||
| 3. Bias Due to Deviations from Intended Interventions | |||||||||
| a. Is the intervention protocol clearly described? | |||||||||
| b. Was the intervention applied according to protocol? | |||||||||
| c. Were deviations from the intervention protocol reported appropriately? | |||||||||
| 4. Attrition Bias | |||||||||
| a. Was there a systematic loss of participants during follow-up? | |||||||||
| b. Was participant loss similar across comparison groups? | |||||||||
| c. Were sensitivity analyses conducted to assess the impact of participant loss? | |||||||||
| 5. Outcome Measurement Bias | |||||||||
| a. Were objective and valid measures used to assess outcomes? | |||||||||
| b. Were outcomes assessed in a blinded manner for participants and evaluators? | |||||||||
| c. Were outcome measurement results reported completely and appropriately? | |||||||||
| 6. Reporting Bias | |||||||||
| a. Were the reported outcomes selected appropriately? | |||||||||
| b. Were the results of all pre-specified analyses reported? | |||||||||
| 7. Inappropriate Outcome Reporting Bias | |||||||||
| a. Were all important consequences of the interventions considered? | |||||||||
| b. Were all relevant outcomes, including adverse events, reported? | |||||||||
| c. Were sensitivity analyses conducted to assess the impact of missing inappropriate outcome data? |
 Yes—Criterion fulfilled;
Yes—Criterion fulfilled;  No—Criterion not fulfilled;
No—Criterion not fulfilled;  Unclear—Insufficient information to determine;
Unclear—Insufficient information to determine;  Not applicable—Criterion not relevant to the study.
Not applicable—Criterion not relevant to the study.| 7 | 11 | |
|---|---|---|
| 1. Bias in the randomization process | ||
| a. Was the generation of the random sequence adequate? | ||
| b. Was the allocation adequately concealed until the intervention? | ||
| c. Were there any suspicious imbalances in baseline characteristics? | ||
| 2. Bias due to deviations from intended interventions | ||
| a. Were participants and personnel blinded to allocation? | ||
| b. Were there important deviations from the protocol? | ||
| c. Were the data analyzed according to the original allocation (intention to treat)? | ||
| 3. Bias due to missing outcome data | ||
| a. Were outcome data missing for some participants? | ||
| b. Were the missing data related to the outcome? | ||
| c. Were appropriate methods used to handle the missing data? | ||
| 4. Bias in outcome measurement | ||
| a. Was the method of measurement appropriate for the outcome? | ||
| b. Were outcome assessors blinded to the assigned group? | ||
| c. Is it likely that outcome measurement was influenced by knowledge of the intervention? | ||
| 5. Bias in selection of the reported result | ||
| a. Were all pre-specified outcomes reported? | ||
| b. Were the reported outcomes selected after knowing the results? |
 Yes—Criterion fulfilled.
Yes—Criterion fulfilled.| 2 | |
|---|---|
| Were the two groups similar and recruited from the same population? | |
| Were the exposures measured similarly to assign participants to exposed and unexposed groups? | |
| Was the exposure measured in a valid and reliable manner? | |
| Were the conditions that were present at the start of the study clearly identified? | |
| Were the outcomes of interest identified at the start of the study? | |
| Were confounding factors identified and adjusted for? | |
| Were the outcomes measured in a valid and reliable way? | |
| Was the follow-up period long enough for outcomes to occur? | |
| Was follow-up complete, and if not, were the reasons for loss to follow-up described? | |
| Were appropriate methods used for statistical analysis? | |
| Was the study approved by an ethics committee, and was informed consent obtained from participants? |
 Yes—Criterion fulfilled;
Yes—Criterion fulfilled;  No—Criterion not fulfilled;
No—Criterion not fulfilled;  Unclear—Insufficient information to determine;
Unclear—Insufficient information to determine;  Not applicable—Criterion not relevant to the study.
Not applicable—Criterion not relevant to the study.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burgos-Lancero, P.; Ibor-Miguel, M.; Marqués-Martínez, L.; Boo-Gordillo, P.; García-Miralles, E.; Guinot-Barona, C. Correction of Anterior Open Bite Using Temporary Anchorage Devices: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 4958. https://doi.org/10.3390/jcm14144958
Burgos-Lancero P, Ibor-Miguel M, Marqués-Martínez L, Boo-Gordillo P, García-Miralles E, Guinot-Barona C. Correction of Anterior Open Bite Using Temporary Anchorage Devices: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(14):4958. https://doi.org/10.3390/jcm14144958
Chicago/Turabian StyleBurgos-Lancero, Patricia, Marta Ibor-Miguel, Laura Marqués-Martínez, Paula Boo-Gordillo, Esther García-Miralles, and Clara Guinot-Barona. 2025. "Correction of Anterior Open Bite Using Temporary Anchorage Devices: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 14: 4958. https://doi.org/10.3390/jcm14144958
APA StyleBurgos-Lancero, P., Ibor-Miguel, M., Marqués-Martínez, L., Boo-Gordillo, P., García-Miralles, E., & Guinot-Barona, C. (2025). Correction of Anterior Open Bite Using Temporary Anchorage Devices: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(14), 4958. https://doi.org/10.3390/jcm14144958