Deferred Lateral Margin Control in the Surgical Treatment of Genital Paget’s Disease and Lentiginous Vulvar Melanoma
Abstract
1. Introduction
2. Materials and Methods
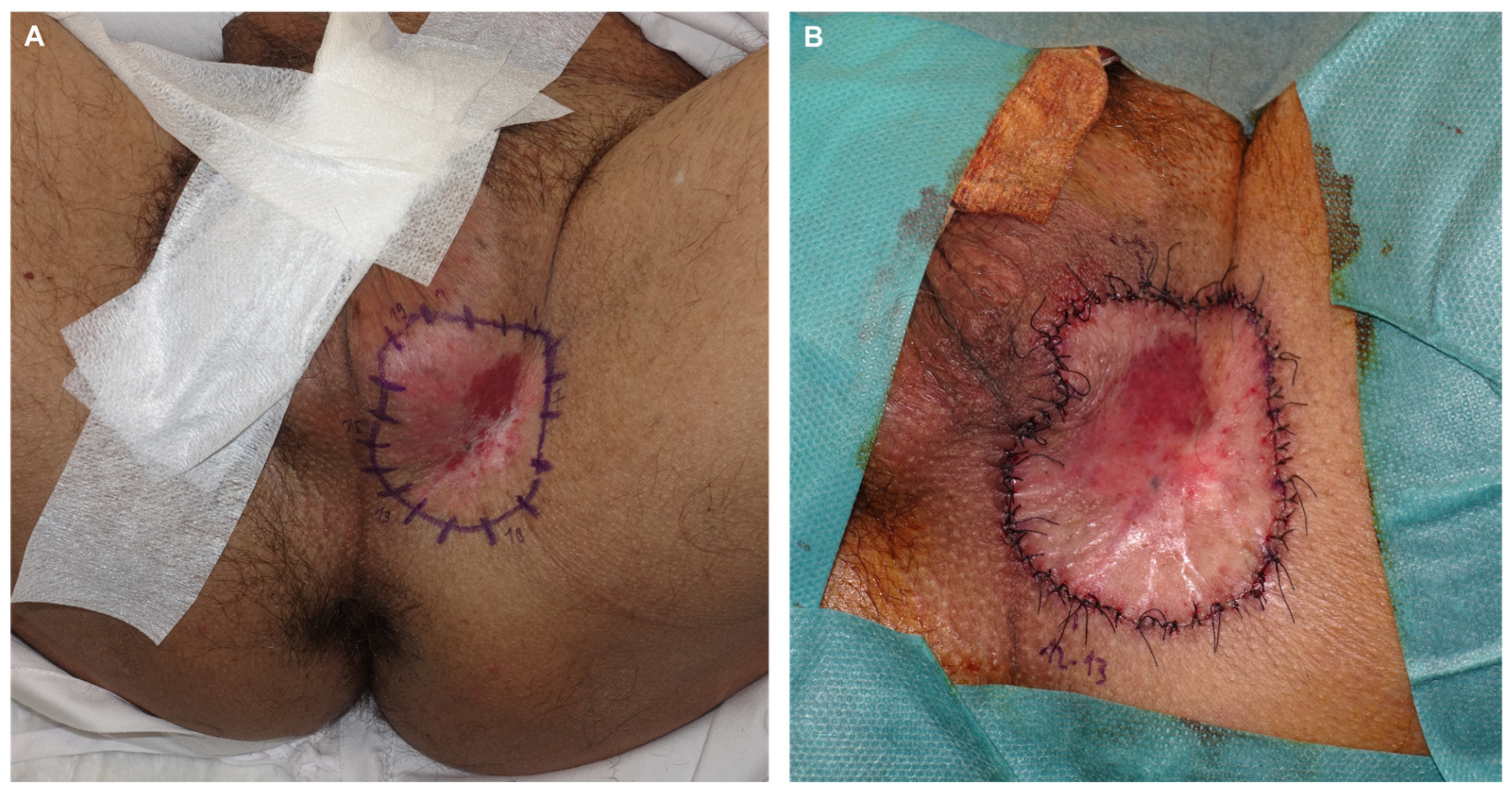
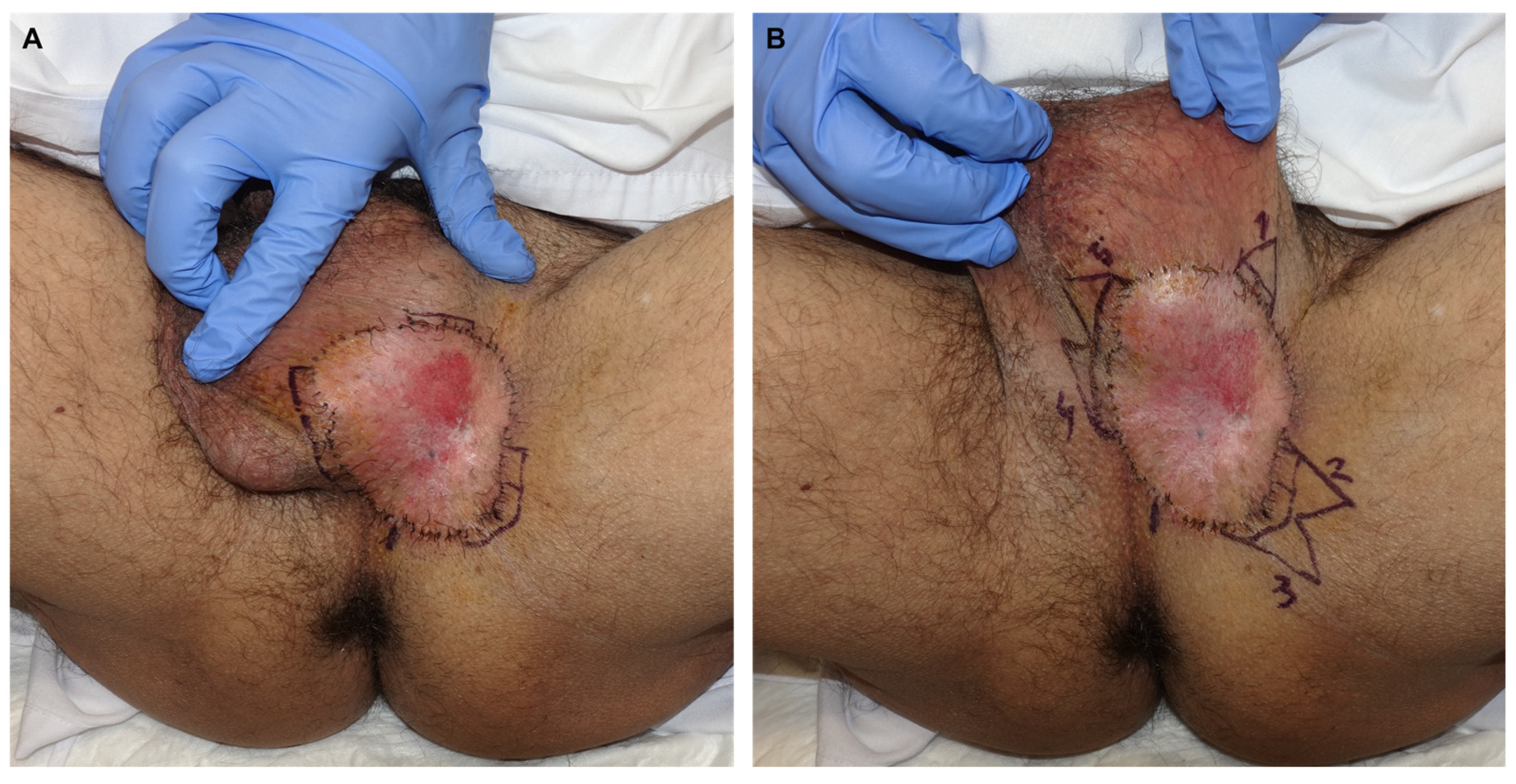
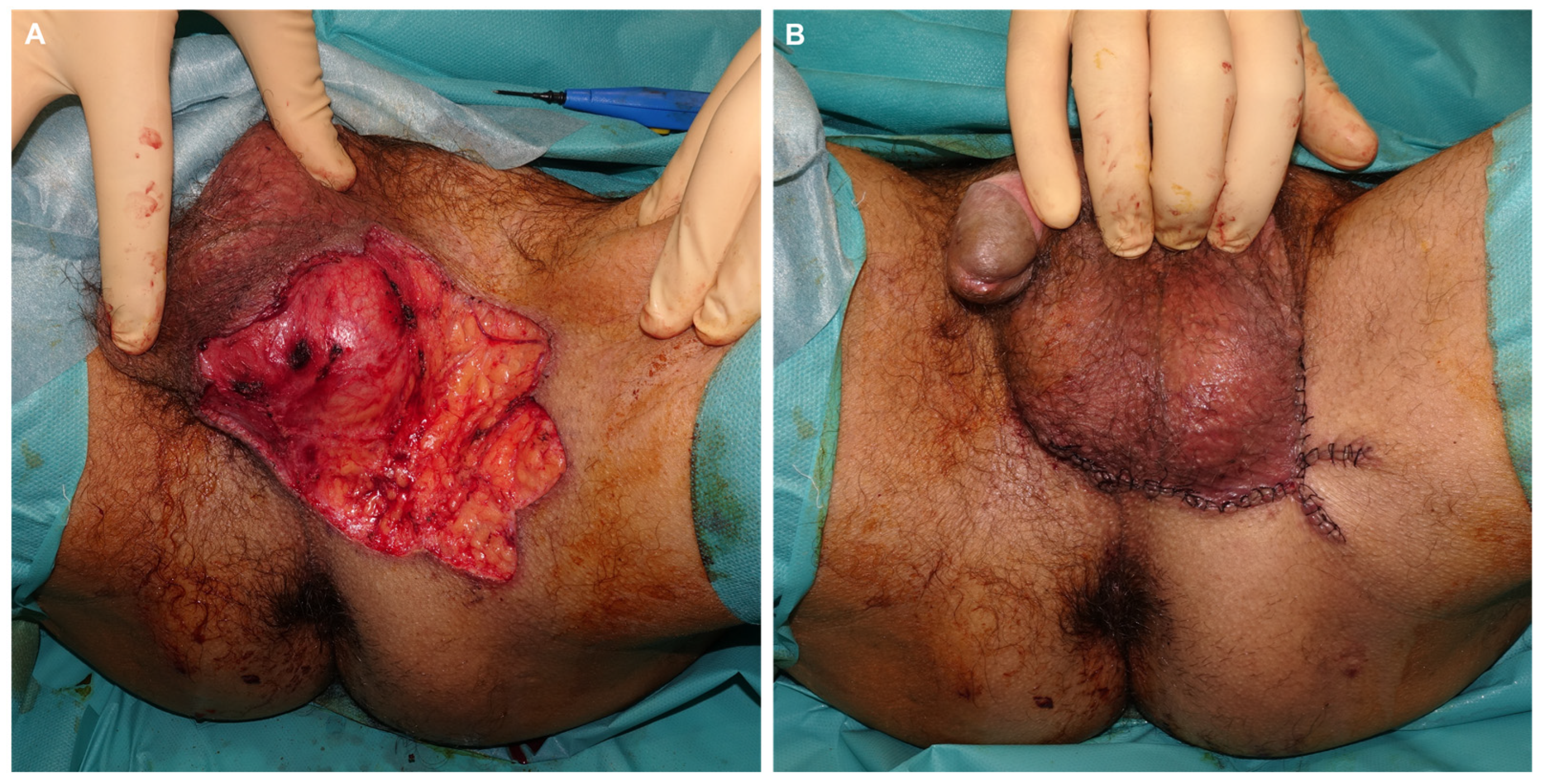
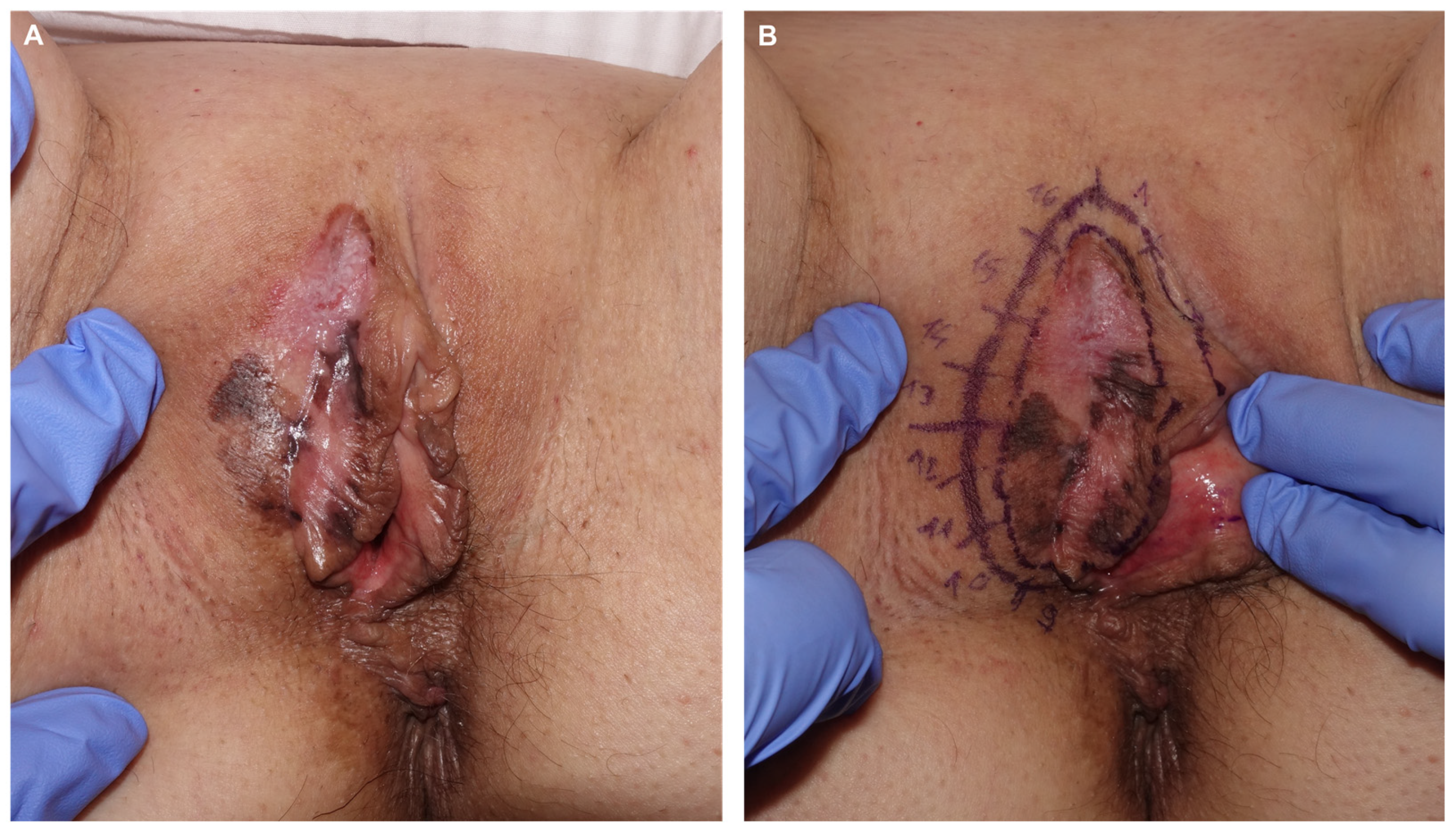
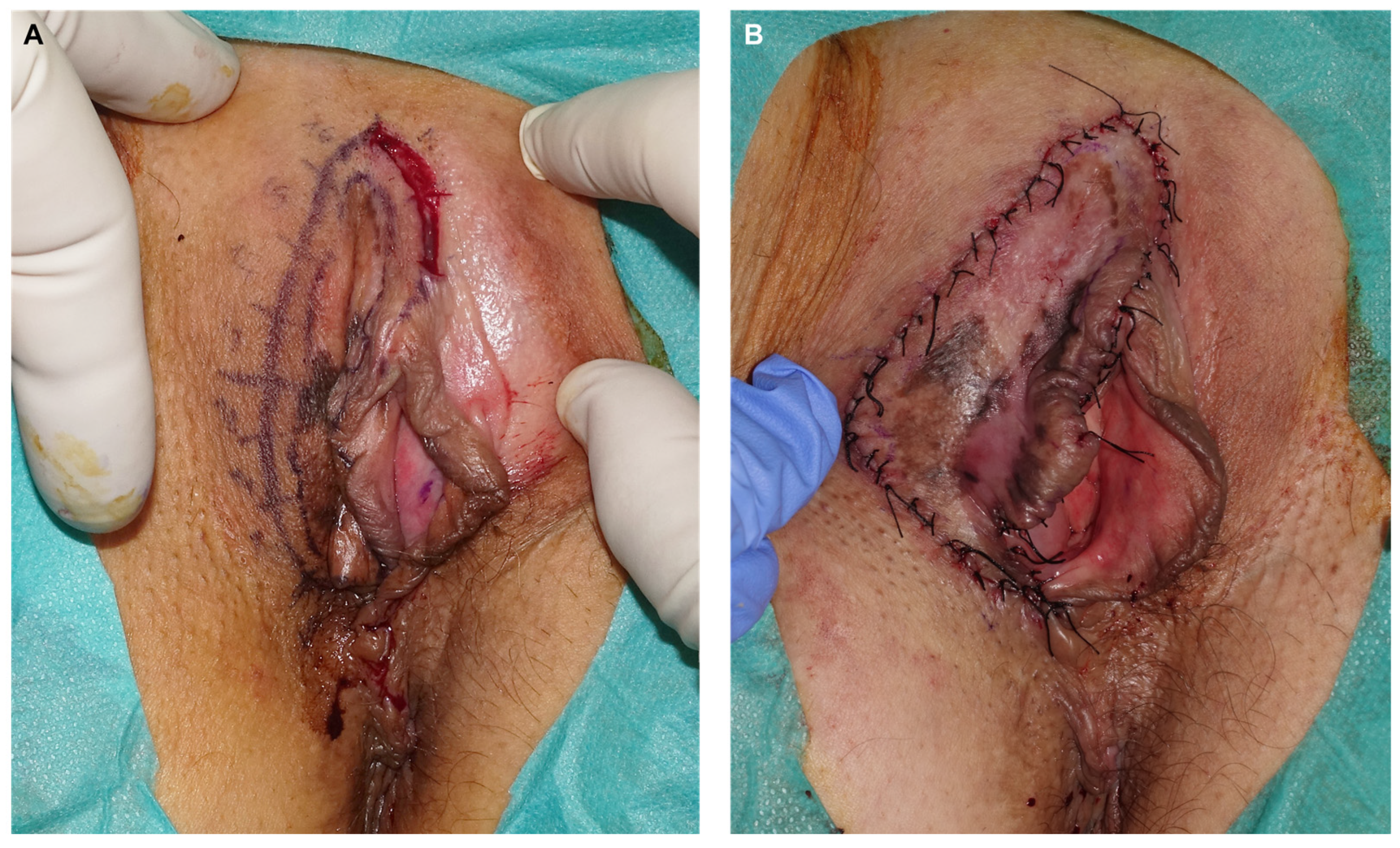
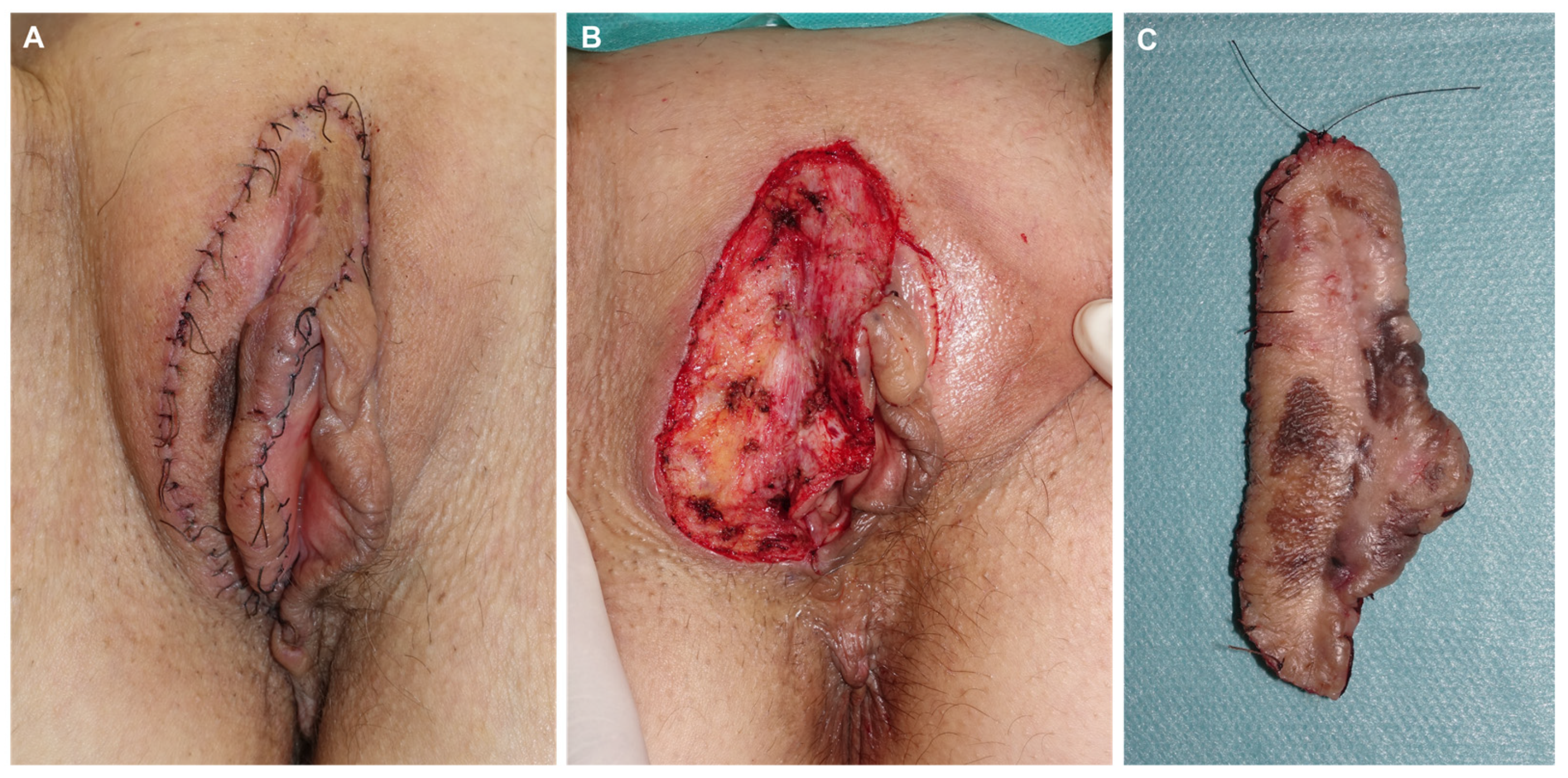
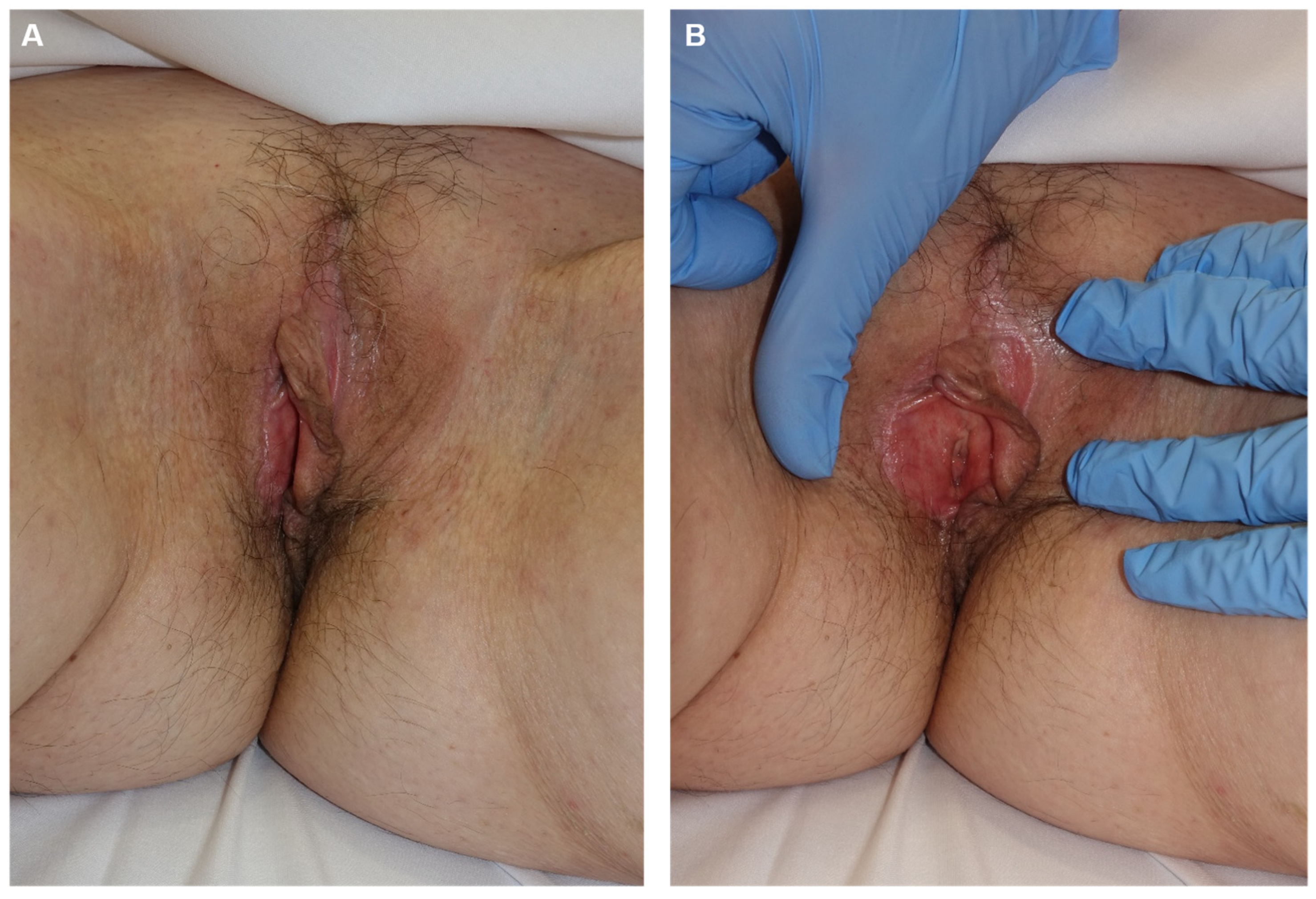
2.1. Case Reports
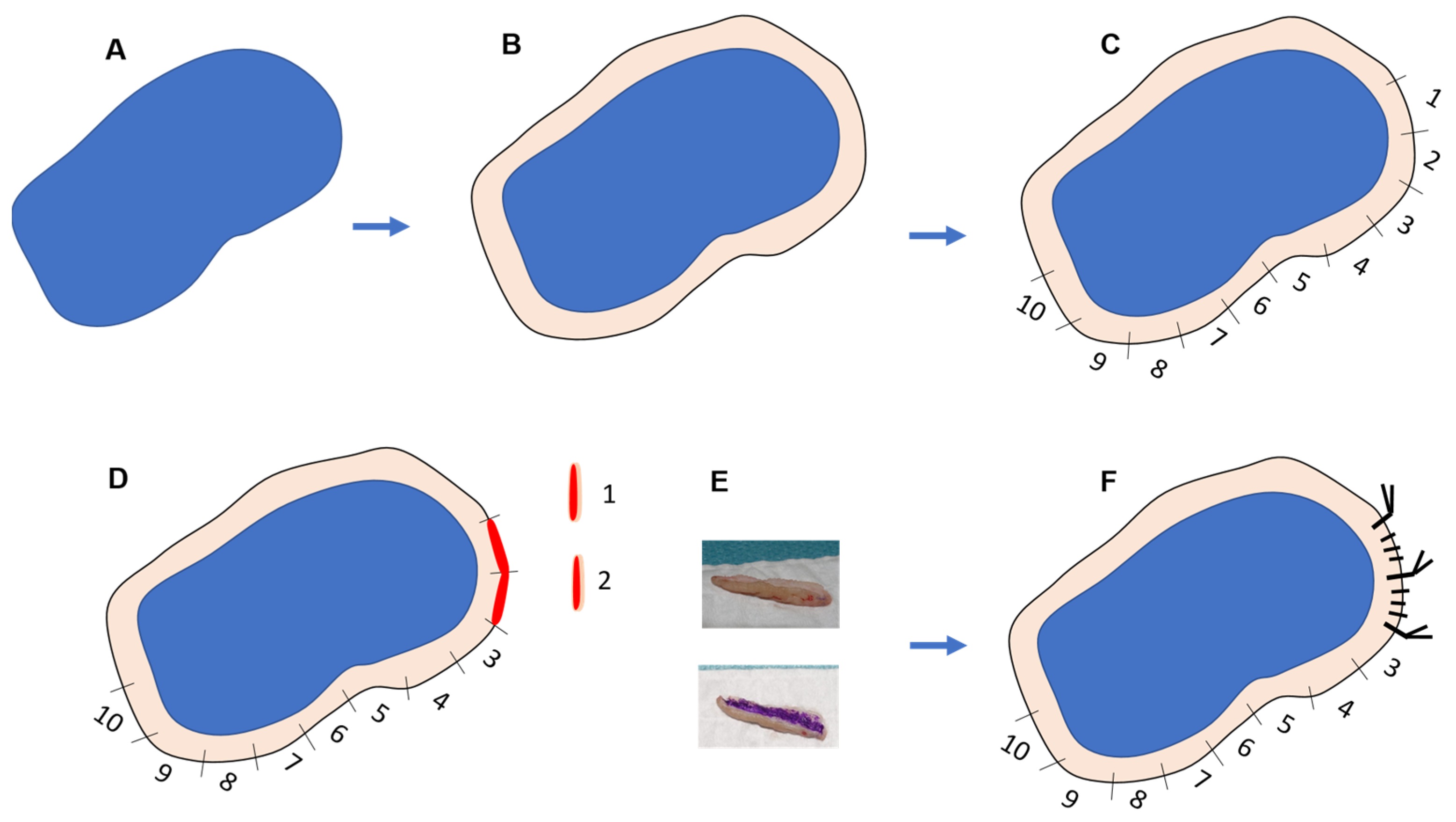
2.2. Surgical Technique
3. Discussion
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ragnarsson-Olding, B.K.; Kanter-Lewensohn, L.R.; Lagerlof, B.; Nilsson, B.R.; Ringborg, U.K. Malignant melanoma of the vulva in a nationwide, 25-year study of 219 Swedish females: Clinical observations and histopathologic features. Cancer 1999, 86, 1273–1284. [Google Scholar] [CrossRef]
- Nagarajan, P.; Curry, J.L.; Ning, J.; Piao, J.; Torres-Cabala, C.A.; Aung, P.P.; Ivan, D.; Ross, M.I.; Levenback, C.F.; Frumovitz, M.; et al. Tumor Thickness and Mitotic Rate Robustly Predict Melanoma-Specific Survival in Patients with Primary Vulvar Melanoma: A Retrospective Review of 100 Cases. Clin. Cancer Res. 2017, 23, 2093–2104. [Google Scholar] [CrossRef] [PubMed]
- Moxley, K.M.; Fader, A.N.; Rose, P.G.; Case, A.S.; Mutch, D.G.; Berry, E.; Schink, J.C.; Kim, C.H.; Chi, D.S.; Moore, K.N. Malignant melanoma of the vulva: An extension of cutaneous melanoma? Gynecol. Oncol. 2011, 122, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Seifried, S.; Haydu, L.E.; Quinn, M.J.; Scolyer, R.A.; Stretch, J.R.; Thompson, J.F. Melanoma of the vulva and vagina: Principles of staging and their relevance to management based on a clinicopathologic analysis of 85 cases. Ann. Surg. Oncol. 2015, 22, 1959–1966. [Google Scholar] [CrossRef] [PubMed]
- Grewal, S.K.; Leboit, P.E.; Saylor, D.K. Mohs for Vulvar Melanoma In Situ. Dermatol. Surg. 2021, 47, 695–696. [Google Scholar] [CrossRef]
- Swetter, S.M.; Tsao, H.; Bichakjian, C.K. Guidelines of care for the management of primary cutaneous melanoma. J. Am. Acad. Dermatol. 2019, 80, 208–250. [Google Scholar] [CrossRef] [PubMed]
- Kunishige, J.H.; Brodland, D.G.; Zitelli, J.A. Surgical margins for melanoma in situ. J. Am. Acad. Dermatol. 2012, 66, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Stigall, L.E.; Brodland, D.G.; Zitelli, J.A. The use of Mohs micrographic surgery (MMS) for melanoma in situ (MIS) of the trunk and proximal extremities. J. Am. Acad. Dermatol. 2016, 75, 1015–1021. [Google Scholar] [CrossRef]
- Young, J.N.; Nguyen, T.A.; Freeman, S.C. Permanent section margin concordance after Mohs micrographic surgery with immunohistochemistry for invasive melanoma and melanoma in situ: A retrospective dual-center analysis. J. Am. Acad. Dermatol. 2023, 88, 1060–1065. [Google Scholar] [CrossRef]
- O’Connor, E.A.; Hettinger, P.C.; Neuburg, M.; Dzwierzynski, W.W. ExtramammaryPaget’s disease: A novel approach to treatment using a modification of peripheral Mohs micrographic surgery. Ann. Plast. Surg. 2012, 68, 616–620. [Google Scholar] [CrossRef]
- Mohs, F.E.; Blanchard, L. Microscopically controlled surgery for extramammary Paget’s disease. Arch. Dermatol. 1979, 115, 706–708. [Google Scholar] [CrossRef] [PubMed]
- Fanning, J.; Lambert, H.L.; Hale, T.M.; Morris, P.C.; Schuerch, C. Paget’s disease of the vulva: Prevalence of associated vulvar adenocarcinoma, invasive Paget’s disease, and recurrence after surgical excision. Am. J. Obstet. Gynecol. 1999, 180, 24–27. [Google Scholar] [CrossRef]
- Hendi, A.; Brodland, D.G.; Zitelli, J.A. Extramammary Paget’s disease: Surgical treatment with Mohs micrographic surgery. J. Am. Acad. Dermatol. 2004, 51, 767–773. [Google Scholar] [CrossRef] [PubMed]
- Wagner, G.; Sachse, M.M. Extramammary Paget disease—Clinical appearance, pathogenesis, management. J. Dtsch. Dermatol. Ges. 2011, 9, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Gaudy-Marqueste, C.; Perchenet, A.S.; Taséi, A.M.; Madjlessi, N.; Magalon, G.; Richard, M.A.; Grob, J.J. The ‘‘spaghetti technique’’: An alternative to Mohs surgery or staged surgery for problematic lentiginous melanoma (lentigo maligna and acral lentiginous melanoma). J. Am. Acad. Dermatol. 2011, 64, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Verschraegen, C.F.; Benjapibal, M.; Supakarapongkul, W.; Levy, L.B.; Ross, M.; Atkinson, E.N.; Bodurka-Bevers, D.; Kavanagh, J.J.; Kudelka, A.P.; Legha, S.S. Vulvar melanoma at the, M.D. Anderson Cancer Center: 25 years later. Int. J. Gynecol. Cancer. 2001, 11, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Reid, G.C.; DeLancey, J.O.; Hopkins, M.P.; Roberts, J.A.; Morley, G.W. Urinary incontinence following radical vulvectomy. Obstet. Gynecol. 1990, 75, 852–858. [Google Scholar] [CrossRef] [PubMed]
- Lukowiak, T.M.; Perz, A.M.; Aizman, L.; Kovell, R.C.; Kovach, S.; Fischer, J.P.; Krausz, A.; Giordano, C.; Higgins, H.W., 2nd; Shin, T.M.; et al. Mohs micrographic surgery for male genital tumors: Local recurrence rates and patient-reported outcomes. J. Am. Acad. Dermatol. 2021, 84, 1030–1036. [Google Scholar] [CrossRef] [PubMed]
- Duque, M.L.; Porras, N.R.; Bulla, F.; Noreña, J.C. Melanoma In Situ on the Penis Treated Using Mohs Micrographic Surgery: Slow Mohs and Local Flap Reconstruction. Dermatol. Surg. 2022, 48, 1109–1111. [Google Scholar] [CrossRef] [PubMed]
- Veronese, F.; Boggio, P.; Tiberio, R.; Gattoni, M.; Fava, P.; Caliendo, V.; Colombo, E.; Savoia, P. Wide local excision vs. Mohs Tübingen technique in the treatment of dermatofibrosarcoma protuberans: A two-centre retrospective study and literature review. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 2069–2076. [Google Scholar] [CrossRef]
- Nieto-Benito, L.M.; Ciudad-Blanco, C.; Sanmartin-Jimenez, O.; Garces, J.R.; Rodríguez-Prieto, M.A.; Vilarrasa, E.; de Eusebio-Murillo, E.; Miñano-Medrano, R.; Escutia-Muñoz, B.; Gonzalez-Sixto, B.; et al. Mohs micro graphic surgery in dermatofibrosarcoma protuberans: Rate and risk factors for recurrence in a prospective cohort study from the Spanish Registry of Mohs Surgery (REGESMOHS) and review of the literature. Exp. Dermatol. 2021, 30, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Hanson, J.; Demer, A.; Liszewski, W.; Foman, N.; Maher, I. Improved overall survival of melanoma of the head and neck treated with Mohs micrographic surgery versus wide local excision. J. Am. Acad. Dermatol. 2020, 82, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Elshot, Y.S.; Tio, D.C.; van Haersma-de With, A.S.; Ouwerkerk, W.; Zupan-Kajcovski, B.; Crijns, M.B.; Limpens, C.E.; Klop, W.M.; Bekkenk, M.W.; Balm, A.J.; et al. Lentigo maligna (melanoma): A systematic review and meta-analysis on surgical techniques and presurgical mapping by reflectance confocal microscopy. J. Eur. Acad. Dermatol. Venereol. 2023, 37, 871–883. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.M.; Choi, Y.Y.; Kim, H.; Oh, B.H.; Roh, M.R.; Nam, K.; Chung, K.Y. Mohs micrographic surgery for extramammary Paget disease: A pooled analysis of individual patient data. J. Am. Acad. Dermatol. 2013, 68, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Warnig, C.; Wollina, U. Cutaneous squamous cell carcinoma of head and neck region: A single center analysis of 1296 tumors with clinical characteristics, comorbidities, treatment, and sun-protection behavior. Dermatol. Ther. 2021, 34, e14992. [Google Scholar] [CrossRef]
- Then, S.Y.; Malhotra, R.; Barlow, R.; Kurwa, H.; Huilgol, S.; Joshi, N.; Olver, J.; Collin, R.; Selva, D. Early cure rates with narrow-margin slow-Mohs surgery for periocular malignant melanoma. Dermatol. Surg. 2009, 35, 17–23. [Google Scholar] [PubMed]
- Carola Eberle, F.; Kanyildiz, M.; Maria Schnabl, S.; Schulz, C.; Häfner, H.M.; Adam, P.; Breuninger, H. Three dimensional (3D) histology in daily rou tine: Practical implementation and its evaluation. J. Dtsch. Dermatol. Ges. 2014, 12, 1028–1035. [Google Scholar] [CrossRef]
- Surmanowicz, P.; Sivanand, A.; Du, A.X.; Mahmood, M.N.; Gniadecki, R. Muffin technique micrographic surgery for non-melanoma skin cancer. Front. Med. 2020, 7, 637223. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.M.; Headington, J.T.; Baker, S.R.; Lowe, L. Usefulness of the staged excision for lentigo maligna and lentigo maligna melanoma: The ‘‘square’’ procedure. J. Am. Acad. Dermatol. 1997, 37, 758–764. [Google Scholar] [CrossRef] [PubMed]
- Breuninger, H.; Schaumburg-Lever, G. Control of excisional margins by conventional histopathological techniques in the treatment of skin tumours. An. Altern. Mohs’ Technique. J. Pathol. 1988, 154, 167–171. [Google Scholar]
- Mahoney, M.H.; Joseph, M.; Temple, C.L. The perimeter technique for lentigo maligna: An alternative to Mohs micrographic surgery. J. Surg. Oncol. 2005, 91, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Clayton, B.D.; Leshin, B.; Hitchcock, M.G.; Marks, M.; White, W.L. Utility of rush paraffin-embedded tangential sections in the management of cutaneous neoplasms. Dermatol. Surg. 2000, 26, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Möller, M.G.; Pappas-Politis, E.; Zager, J.S.; Santiago, L.A.; Yu, D.; Prakash, A.; Kinal, A.; Clark, G.S.; Zhu, W.; Puleo, C.A.; et al. Surgical management of melanoma-in-situ using a staged marginal and central excision technique. Ann. Surg. Oncol. 2009, 16, 1526–1536. [Google Scholar] [CrossRef] [PubMed]
- Moehrle, M.; Dietz, K.; Garbe, C.; Breuninger, H. Conventional histology vs. three-dimensional histology in lentigo maligna melanoma. Br. J. Dermatol. 2006, 154, 453–459. [Google Scholar] [CrossRef]
- Lichte, V.; Breuninger, H.; Metzler, G.; Haefner, H.M.; Moehrle, M. Acral lentiginous melanoma: Conventional histology vs. three dimensional histology. Br. J. Dermatol. 2009, 160, 591–599. [Google Scholar] [CrossRef]
- Abdelmalek, M.; Loosemore, M.P.; Hurt, M.A.; Hruza, G. Geometric staged excision for the treatment of lentigo maligna and lentigo maligna melanoma: A long-term experience with lite rature review. Arch. Dermatol. 2012, 148, 599–604. [Google Scholar] [CrossRef] [PubMed]
- de Vries, K.; Greveling, K.; Prens, L.M.; Munte, K.; Koljenović, S.; van Doorn, M.B.; Prens, E.P. Recurrence rate of lentigo maligna after micrographically controlled staged surgical excision. Br. J. Dermatol. 2016, 174, 588–593. [Google Scholar] [CrossRef]
- Kassi, K.; Vanwijck, R.; Kanga, J.-M. The ‘‘collerette’’ technique for skin excision and biopsy: An efficient method for managing lentigo maligna of the head and neck. Int. J. Dermatol. 2014, 53, 899–903. [Google Scholar] [CrossRef]
- Martinez-Molina, M.; Richarz, N.; Jaka, A.; Bassas-Vila, J.; Mora-Fernández, V.; Pi-Sunyer, A.Q.; Podlipnik, S.; Carrascosa, J.M.; Boada, A. Spaghetti Technique Versus Wide Local Excision for Lentigo Maligna Affecting the Head and Neck Regions: Surgical Outcome and Descriptive Analysis of 79 Cases from a Single Practice Cohort. Dermatol. Pract. Concept. 2023, 13, e2023193. [Google Scholar] [CrossRef] [PubMed]
- Hazan, C.; Dusza, S.W.; Delgado, R.; Busam, K.J.; Halpern, A.C.; Nehal, K.S. Staged excision for lentigo maligna and lentigo maligna melanoma: A retrospective analysis of 117 cases. J. Am. Acad. Dermatol. 2008, 58, 142–148. [Google Scholar] [CrossRef]
- Hu, J.; Cai, X.; Lv, J.J.; Wan, X.C.; Zeng, X.Y.; Feng, M.L.; Dai, B.; Kong, Y.Y. Preferentially expressed antigen in melanoma immunohistochemistry as an adjunct for differential diagnosis in acral lentiginous melanoma and acral nevi. Hum. Pathol. 2022, 120, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Damavandy, A.A.; Terushkin, V.; Zitelli, J.A.; Brodland, D.G.; Miller, C.J.; Etzkorn, J.R.; Shin, T.M.; Cappel, M.A.; Mitkov, M.; Hendi, A. Intraoperative Immunostaining for Cytokeratin-7 During Mohs Micrographic Surgery Demonstrates Low Local Recurrence Rates in Extramammary Paget’s Disease. Dermatol. Surg. 2018, 44, 354–364. [Google Scholar] [CrossRef]
- Geng, R.S.Q.; Sood, S.; Waked, J.; Towheed, S.; Devoy, C.; Lee, A.; Usman, S.; Mahmood, R.; Merchant, N.; Yeung, J.; et al. Treatment Outcomes in Extramammary Paget’s Disease: A Systematic Review. J. Cutan. Med. Surg. 2024, 12034754241293107. [Google Scholar] [CrossRef] [PubMed]
- Kofler, L.; Breuninger, H.; Schulz, C.; Häfner, H.-M.; Kofler, K. Local recurrence rates of skin tumors after resection with complete circumferential peripheral and deep margin assessment-identification of high-risk entities. Dermatol. Surg. 2021, 47, e31–e36. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.J.; Wood, G.C.; Marks, V.J. Mohs micrographic surgery in the treatment of rare aggressive cutaneous tumors: The Geisinger experience. Dermatol. Surg. 2007, 33, 333–339. [Google Scholar] [PubMed]
- Rodríguez-Jiménez, P.; Jimenez, Y.D.; Reolid, A.; Sanmartın-Jimenez, O.; Garces, J.R.; Rodríguez-Prieto, M.A.; Medrano, R.M.; Vilarrasa, E.; de Eusebio-Murillo, E.; Redondo, P.; et al. State of the art of Mohs surgery for rare cutaneous tumors in the Spanish Registry of Mohs Surgery (REGESMOHS). Int. J. Dermatol. 2020, 59, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Cabrioli, C.; Maione, V.; Arisi, M.; Perantoni, M.; Guasco Pisani, E.; Venturini, M.; Calzavara-Pinton, P.; Licata, G. Surgical margin mapping for lentigo maligna and lentigo maligna melanoma: Traditional technique (visual inspection with dermoscopy) versus combined paper tape and reflectance confocal microscopy technique. Int. J. Dermatol. 2023, 62, 805–811. [Google Scholar] [CrossRef]
- Couty, E.; Tognetti, L.; Labeille, B.; Douchet, C.; Habougit, C.; Couzan, C.; Biron-Schneider, A.C.; Cambazard, F.; Prade, V.; Rubegni, P.; et al. In vivo reflectance confocal microscopy combined with the ’spaghetti technique’ for the identification of surgical margins of lentigo maligna: Experience in 70 patients. J. Eur. Acad. Dermatol. Venereol. 2018, 32, e366–e368. [Google Scholar] [CrossRef] [PubMed]
- Champin, J.; Perrot, J.L.; Cinotti, E.; Labeille, B.; Douchet, C.; Parrau, G.; Cambazard, F.; Seguin, P.; Alix, T. In vivo reflectance confocal microscopy to optimize the spaghetti technique for defining surgical margins of lentigo maligna. Dermatol. Surg. 2014, 3, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Terrier, J.E.; Tiffet, O.; Raynaud, N.; Cinotti, E. In Vivo Reflectance Confocal Microscopy Combined With the “Spaghetti” Technique: A New Procedure for Defining Surgical Margins of Genital Paget Disease. Dermatol. Surg. 2015, 41, 862–864. [Google Scholar] [CrossRef] [PubMed]
- Paraskevas, L.-R.; Halpern, A.C.; Marghoob, A. Utility of the Wood’s light: Five cases from a pigmented lesion clinic. Br. J. Dermatol. 2005, 152, 1039–1044. [Google Scholar] [CrossRef]
- Sano, T.; Minagawa, A.; Suzuki, R.; Koga, H.; Okuyama, R. Dermoscopy with near-ultraviolet light highlights the demarcation of melanin distribution in cutaneous melanoma. J. Am. Acad. Dermatol. 2021, 84, e23–e24. [Google Scholar] [CrossRef]
- Wu, M.; Huang, L.; Lu, X.; Li, J.; Wang, Y.; Zang, J.; Mo, X.; Shao, X.; Wang, L.; Cheng, W.; et al. Utility of photodynamic diagnosis plus reflectance confocal microscopy in detecting the margins of extramammary Paget disease. Indian. J. Dermatol. Venereol. Leprol. 2021, 87, 207–213. [Google Scholar] [CrossRef]
- Guitera, P.; Moloney, F.J.; Menzies, S.W.; Stretch, J.R.; Quinn, M.J.; Hong, A.; Fogarty, G.; Scolyer, R.A. Improving management and patient care in lentigo maligna by mapping with in vivo confocal microscopy. JAMA Dermatol. 2013, 149, 692–698. [Google Scholar] [CrossRef] [PubMed]





| Mohs Surgery | Spaguetti Technique | |
|---|---|---|
| Patient satisfaction | Good | Good |
| Number of days the patient enters the operating room | Almost always one day | Variable |
| Total duration of treatment | Longer (one time only) * | Shorter (sum of several times) |
| Quality of the analyzed tissue | Good | Best |
| Possibility of artifacts in sample processing (false negatives) | Low | Very low |
| Possibility of studying larges pieces | Limited | Adequate |
| Immunohistochemistry techniques | Limited | Widely available |
| Possibility of planning a surgical closure | At the time | In a planned way |
| Need for specialized dermatological and patological equipment | Yes | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Redondo, P. Deferred Lateral Margin Control in the Surgical Treatment of Genital Paget’s Disease and Lentiginous Vulvar Melanoma. J. Clin. Med. 2025, 14, 69. https://doi.org/10.3390/jcm14010069
Redondo P. Deferred Lateral Margin Control in the Surgical Treatment of Genital Paget’s Disease and Lentiginous Vulvar Melanoma. Journal of Clinical Medicine. 2025; 14(1):69. https://doi.org/10.3390/jcm14010069
Chicago/Turabian StyleRedondo, Pedro. 2025. "Deferred Lateral Margin Control in the Surgical Treatment of Genital Paget’s Disease and Lentiginous Vulvar Melanoma" Journal of Clinical Medicine 14, no. 1: 69. https://doi.org/10.3390/jcm14010069
APA StyleRedondo, P. (2025). Deferred Lateral Margin Control in the Surgical Treatment of Genital Paget’s Disease and Lentiginous Vulvar Melanoma. Journal of Clinical Medicine, 14(1), 69. https://doi.org/10.3390/jcm14010069






