Preoperative Neutrophil-to-Lymphocyte Ratio as a Predictor of Clinical Outcomes in Patients Undergoing Femoral Endarterectomy
Abstract
1. Introduction
2. Materials and Methods
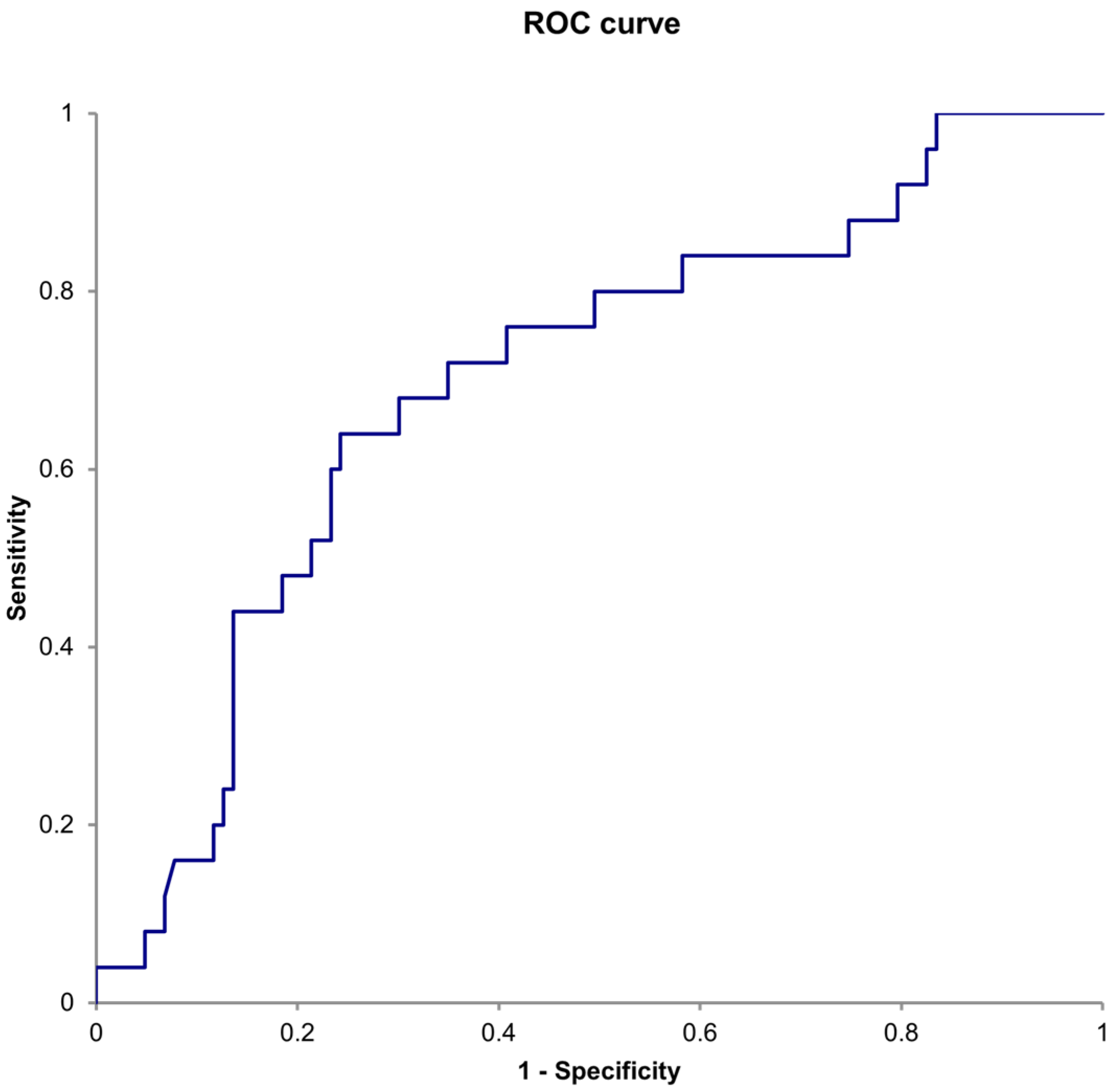
Statistical Analyses
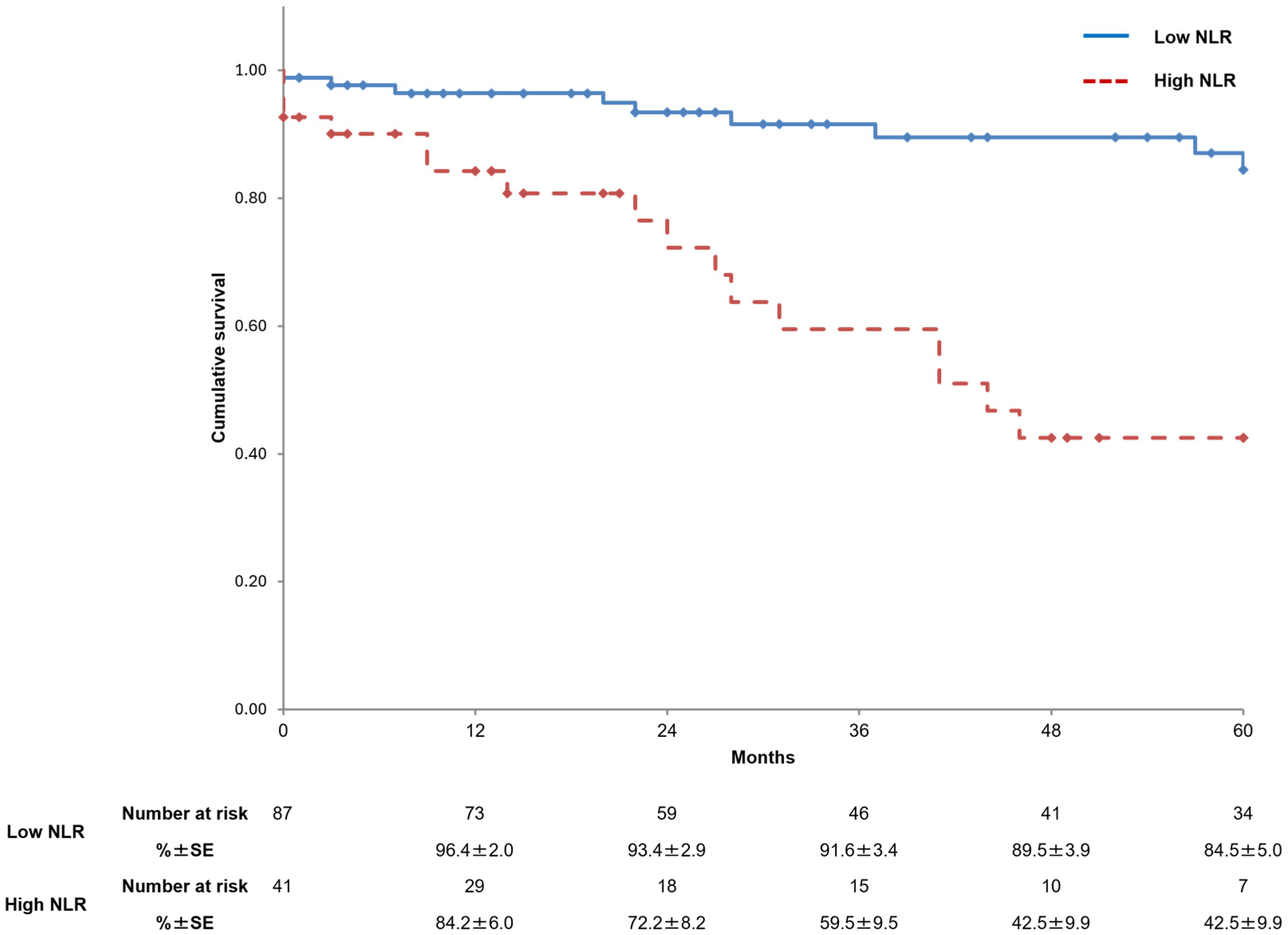
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aboyans, V.; Ricco, J.B.; Bartelink, M.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. Editor’s Choice—2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2018, 55, 305–368. [Google Scholar] [CrossRef] [PubMed]
- Gouëffic, Y.; Della Schiava, N.; Thaveau, F.; Rosset, E.; Favre, J.P.; Salomon du Mont, L.; Alsac, J.M.; Hassen-Khodja, R.; Reix, T.; Allaire, E.; et al. Stenting or surgery for de novo common femoral artery stenosis. JACC Cardiovasc. Interv. 2017, 10, 1344–1354. [Google Scholar] [CrossRef]
- Kaneta, G.; Husain, S.; Musto, L.; Hamakarim, T.; Elsharkawi, A.; Littlejohn, S.; Helm, J.; Saratzis, A.; Zayed, H. Editor’s choice—eligibility of common femoral artery atherosclerotic disease for endovascular treatment—the CONFESS Study. Eur. J. Vasc. Endovasc. Surg. 2022, 64, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Saenz-Pipaon, G.; Martinez-Aguilar, E.; Orbe, J.; González Miqueo, A.; Fernandez-Alonso, L.; Paramo, J.A.; Roncal, C. The role of circulating biomarkers in peripheral arterial disease. Int. J. Mol. Sci. 2021, 22, 3601. [Google Scholar] [CrossRef]
- Zahorec, R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy 2021, 122, 474–488. [Google Scholar] [CrossRef] [PubMed]
- Soeters, P.B.; Wolfe, R.R.; Shenkin, A. Hypoalbuminemia: Pathogenesis and clinical significance. J. Parenter. Enter. Nutr. 2019, 43, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Uchiyama, H.; Oonuki, M. Outcomes of femoral endarterectomy with superficial tributary vein patch angioplasty. Ann. Vasc. Surg. 2023, 90, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.N.; Amdur, R.L.; Abugideiri, M.; Rahbar, R.; Neville, R.F.; Sidawy, A.N. Postoperative complications after common femoral endarterectomy. J. Vasc. Surg. 2015, 61, 1489–1494.e1. [Google Scholar] [CrossRef] [PubMed]
- Kuma, S.; Tanaka, K.; Ohmine, T.; Morisaki, K.; Kodama, A.; Guntani, A.; Ishida, M.; Okazaki, J.; Mii, S. Clinical outcome of surgical endarterectomy for common femoral artery occlusive disease. Circ. J. 2016, 80, 964–969. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Yamamoto, S.; Kimura, M.; Sano, M.; Sato, O.; Deguchi, J. Long-term outcomes following common femoral endarterectomy. J. Clin. Med. 2022, 11, 6873. [Google Scholar] [CrossRef] [PubMed]
- Nakama, T.; Takahara, M.; Iwata, Y.; Fujimura, N.; Yamaoka, T.; Suzuki, K.; Obunai, K.; CAULIFLOWER Study Investigators. 1-year outcomes of thromboendarterectomy vs endovascular therapy for common femoral artery lesions: CAULIFLOWER study results. JACC Cardiovasc. Interv. 2022, 15, 1453–1463. [Google Scholar] [CrossRef]
- Zahorec, R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 2001, 102, 5–14. [Google Scholar]
- Huang, Z.; Fu, Z.; Huang, W.; Huang, K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am. J. Emerg Med. 2020, 38, 641–647. [Google Scholar] [CrossRef]
- Dilektasli, E.; Inaba, K.; Haltmeier, T.; Wong, M.D.; Clark, D.; Benjamin, E.R.; Lam, L.; Demetriades, D. The prognostic value of neutrophil-to-lymphocyte ratio on mortality in critically ill trauma patients. J. Trauma Acute Care Surg. 2016, 81, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: A systematic review and meta-analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef] [PubMed]
- Arbel, Y.; Finkelstein, A.; Halkin, A.; Birati, E.Y.; Revivo, M.; Zuzut, M.; Shevach, A.; Berliner, S.; Herz, I.; Keren, G.; et al. Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography. Atherosclerosis 2012, 225, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Ha, E.T.; Yee, A.; Peterson, S.J.; Kobayashi, Y.; Sacchi, T.; Parikh, M.; Brener, S.J. Neutrophil-to-lymphocyte ratio and prognosis in patients undergoing percutaneous coronary intervention for acute coronary syndrome. Cardiovasc. Revascularization Med. 2024, 60, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Hou, M.; Ding, Z.; Liu, X.; Shao, Y.; Li, X. Prognostic value of neutrophil-to-lymphocyte ratio in stroke: A systematic review and meta-analysis. Front. Neurol. 2021, 12, 686983. [Google Scholar] [CrossRef]
- Köklü, E.; Yüksel, İÖ.; Arslan, Ş.; Bayar, N.; Çağırcı, G.; Gencer, E.S.; Alparslan, A.Ş.; Çay, S.; Kuş, G. Is elevated neutrophil-to-lymphocyte ratio a predictor of stroke in patients with intermediate carotid artery stenosis? J. Stroke Cerebrovasc. Dis. 2016, 25, 578–584. [Google Scholar] [CrossRef]
- Buso, G.; Faggin, E.; Rosenblatt-Velin, N.; Pellegrin, M.; Galliazzo, S.; Calanca, L.; Rattazzi, M.; Mazzolai, L. The role of neutrophils in lower limb peripheral artery disease: State of the art and future perspectives. Int. J. Mol. Sci. 2023, 24, 1169. [Google Scholar] [CrossRef] [PubMed]
- Teperman, J.; Carruthers, D.; Guo, Y.; Barnett, M.P.; Harris, A.A.; Sedlis, S.P.; Pillinger, M.; Babaev, A.; Staniloae, C.; Attubato, M.; et al. Relationship between neutrophil-lymphocyte ratio and severity of lower extremity peripheral artery disease. Int. J. Cardiol. 2017, 228, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Erturk, M.; Cakmak, H.A.; Surgit, O.; Celik, O.; Aksu, H.U.; Akgul, O.; Gurdogan, M.; Bulut, U.; Ozalp, B.; Akbay, E.; et al. Predictive value of elevated neutrophil to lymphocyte ratio for long-term cardiovascular mortality in peripheral arterial occlusive disease. J. Cardiol. 2014, 64, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Bath, J.; Smith, J.B.; Kruse, R.L.; Vogel, T.R. Neutrophil-lymphocyte ratio predicts disease severity and outcome after lower extremity procedures. J. Vasc. Surg. 2020, 72, 622–631. [Google Scholar] [CrossRef]
- Pourafkari, L.; Choi, C.; Garajehdaghi, R.; Tajlil, A.; Dosluoglu, H.H.; Nader, N.D. Neutrophil-lymphocyte ratio is a marker of survival and cardiac complications rather than patency following revascularization of lower extremities. Vasc. Med. 2018, 23, 437–444. [Google Scholar] [CrossRef]
- González-Fajardo, J.A.; Brizuela-Sanz, J.A.; Aguirre-Gervás, B.; Merino-Díaz, B.; Del Río-Solá, L.; Martín-Pedrosa, M.; Vaquero-Puerta, C. Prognostic significance of an elevated neutrophil-lymphocyte ratio in the amputation-free survival of patients with chronic critical limb ischemia. Ann. Vasc. Surg. 2014, 28, 999–1004. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.; Puckridge, P.; Ullah, S.; Delaney, C.; Spark, J.I. Neutrophil-lymphocyte ratio as a prognostic marker of outcome in infrapopliteal percutaneous interventions for critical limb ischemia. J. Vasc. Surg. 2014, 60, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Martelli, E.; Enea, I.; Zamboni, M.; Federici, M.; Bracale, U.M.; Sangiorgi, G.; Martelli, A.R.; Messina, T.; Settembrini, A.M. Focus on the most common paucisymptomatic vasculopathic population, from diagnosis to secondary prevention of complications. Diagnostics 2023, 13, 2356. [Google Scholar] [CrossRef]
- Kochar, A.; Mulder, H.; Rockhold, F.W.; Baumgartner, I.; Berger, J.S.; Blomster, J.I.; Fowkes, F.G.R.; Katona, B.G.; Lopes, R.D.; Al-Khalidi, H.R.; et al. Cause of death among patients with peripheral artery disease: Insights from the EUCLID Trial. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e006550. [Google Scholar] [CrossRef] [PubMed]


| All Patients (n = 128) | |
|---|---|
| Age, years | 71.5 ± 8.25 |
| Men | 87 (68.0) |
| Neutrophil-to-lymphocyte ratio | 4.13 ± 4.11 |
| Serum albumin (g/dL) | 3.81 ± 0.59 |
| Statin use | 80 (62.5) |
| Hypertension | 109 (85.2) |
| Dyslipidemia | 94 (73.4) |
| Diabetes mellitus | 82 (64.1) |
| Coronary artery disease | 54 (42.2) |
| Cerebrovascular disease | 26 (20.3) |
| COPD | 20 (15.6) |
| End-stage renal disease | 35 (27.3) |
| Ever smoked | 100 (78.1) |
| Non-ambulatory status | 8 (6.3) |
| Rutherford classification | |
| 3 | 80 (62.5) |
| 4 | 20 (15.6) |
| 5 | 27 (21.1) |
| 6 | 1 (0.8) |
| Low NLR (n = 87) | High NLR (n = 41) | p-Value | |
|---|---|---|---|
| Age, years | 71.8 ± 8.29 | 71.4 ± 8.22 | 0.784 |
| Men | 54 (62.1) | 33 (80.5) | 0.037 |
| NLR | 2.46 ± 0.76 | 7.65 ± 5.76 | <0.001 |
| Serum albumin (g/dL) | 3.98 ± 0.50 | 3.46 ± 0.63 | <0.001 |
| Statin use | 56 (64.4) | 24 (58.5) | 0.525 |
| Hypertension | 72 (82.8) | 37 (90.2) | 0.302 |
| Dyslipidemia | 65 (74.7) | 29 (70.7) | 0.634 |
| Diabetes mellitus | 55 (63.2) | 27 (65.9) | 0.772 |
| Coronary artery disease | 35 (40.2) | 19 (46.3) | 0.514 |
| Cerebrovascular disease | 15 (17.2) | 11 (26.8) | 0.208 |
| COPD | 13 (14.9) | 7 (17.1) | 0.757 |
| End-stage renal disease | 13 (14.9) | 22 (53.7) | <0.001 |
| Ever smoked | 69 (79.3) | 31 (75.6) | 0.637 |
| Non-ambulatory status | 2 (2.3) | 6 (14.6) | 0.013 |
| CLTI | 23 (26.4) | 25 (61.0) | <0.001 |
| Low NLR (n = 87) | High NLR (n = 41) | p Value | |
|---|---|---|---|
| Simple endarterectomy | 20 (23.0) | 12 (29.3) | 0.444 |
| Endarterectomy + inflow procedure | 45 (51.7) | 16 (39.0) | 0.180 |
| Endarterectomy + outflow procedure | 34 (39.1) | 22 (53.7) | 0.121 |
| Complications within 30 days | 12 (13.8) | 8 (19.5) | 0.406 |
| Cardiac failure | 0 (0.0) | 1 (2.4) | |
| Cerebrovascular complications | 1 (1.1) | 3 (7.3) | |
| Wound complications | 4 (4.6) | 0 (0.0) | |
| Bleeding | 5 (5.7) | 3 (7.3) | |
| Major amputation | 1 (1.1) | 1 (2.4) | |
| Ischemic colitis | 1 (1.1) | 0 (0.0) | |
| Death within 30 days | 1 (1.1) | 2 (4.9) | 0.240 |
| Postoperative hospital stay (days) | 9 (8–13.5) | 12 (7–30.25) | 0.034 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Risk Factor | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| Age | 1.01 (0.96–1.06) | 0.715 | ||
| WBC count > 10 × 109/L | 2.02 (0.47–8.58) | 0.343 | ||
| NLR > 4.0 | 5.24 (2.31–11.93) | <0.001 | 2.60 (1.05–6.45) | 0.039 |
| Albumin < 3.5 g/dL | 5.17 (2.33–11.43) | <0.001 | 2.08 (0.83–5.20) | 0.119 |
| Hypertension | 5.30 (0.72–39.17) | 0.103 | 4.38 (0.53–35.98) | 0.169 |
| Dyslipidemia | 0.79 (0.34–1.84) | 0.592 | ||
| Diabetes mellitus | 1.68 (0.67–4.22) | 0.266 | ||
| Coronary artery disease | 1.14 (0.52–2.51) | 0.746 | ||
| Cerebrovascular disease | 2.77 (1.26–6.10) | 0.011 | 1.11 (0.45–2.74) | 0.813 |
| COPD | 1.22 (0.48–3.06) | 0.676 | ||
| End-stage renal disease | 5.34 (2.36–12.11) | <0.001 | 1.56 (0.57–4.28) | 0.385 |
| Ever smoked | 1.36 (0.47–3.97) | 0.572 | ||
| Non-ambulatory status | 1.70 (0.40–7.24) | 0.472 | ||
| CLTI | 4.52 (1.95–10.51) | <0.001 | 2.41 (0.87–6.65) | 0.091 |
| Statin use | 0.62 (0.28–1.37) | 0.238 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, Y.; Kazama, A.; Kikuchi, T.; Kudo, T. Preoperative Neutrophil-to-Lymphocyte Ratio as a Predictor of Clinical Outcomes in Patients Undergoing Femoral Endarterectomy. J. Clin. Med. 2025, 14, 211. https://doi.org/10.3390/jcm14010211
Yamamoto Y, Kazama A, Kikuchi T, Kudo T. Preoperative Neutrophil-to-Lymphocyte Ratio as a Predictor of Clinical Outcomes in Patients Undergoing Femoral Endarterectomy. Journal of Clinical Medicine. 2025; 14(1):211. https://doi.org/10.3390/jcm14010211
Chicago/Turabian StyleYamamoto, Yohei, Ai Kazama, Toru Kikuchi, and Toshifumi Kudo. 2025. "Preoperative Neutrophil-to-Lymphocyte Ratio as a Predictor of Clinical Outcomes in Patients Undergoing Femoral Endarterectomy" Journal of Clinical Medicine 14, no. 1: 211. https://doi.org/10.3390/jcm14010211
APA StyleYamamoto, Y., Kazama, A., Kikuchi, T., & Kudo, T. (2025). Preoperative Neutrophil-to-Lymphocyte Ratio as a Predictor of Clinical Outcomes in Patients Undergoing Femoral Endarterectomy. Journal of Clinical Medicine, 14(1), 211. https://doi.org/10.3390/jcm14010211







