Patients with Type 2 Diabetes, Higher Blood Pressure, and Infrequent Fundus Examinations Have a Higher Risk of Sight-Threatening Retinopathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Demographic Data, and Medical Records
2.2. Metabolic Risk Factors
2.3. Ophthalmologic Retinal Examination
2.4. Statistical Analysis
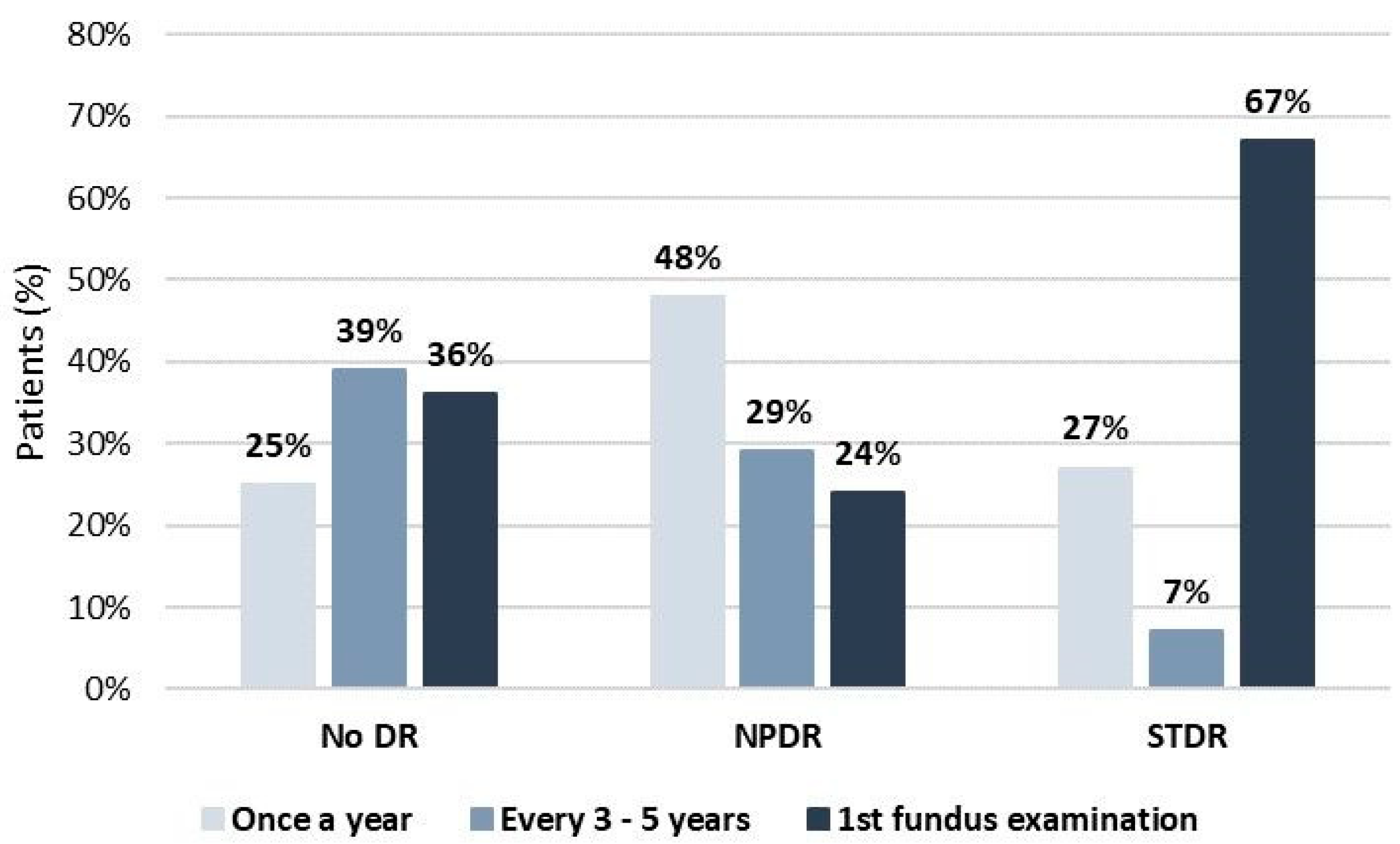
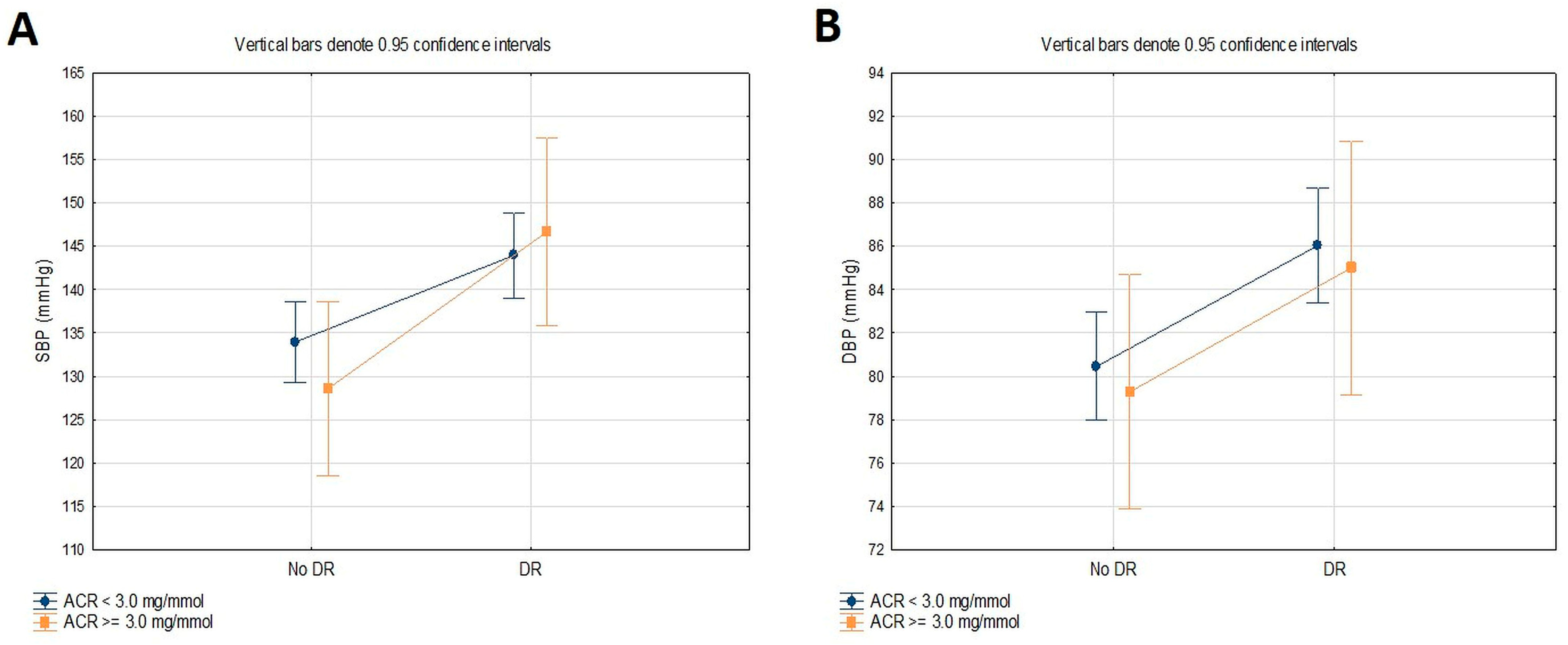
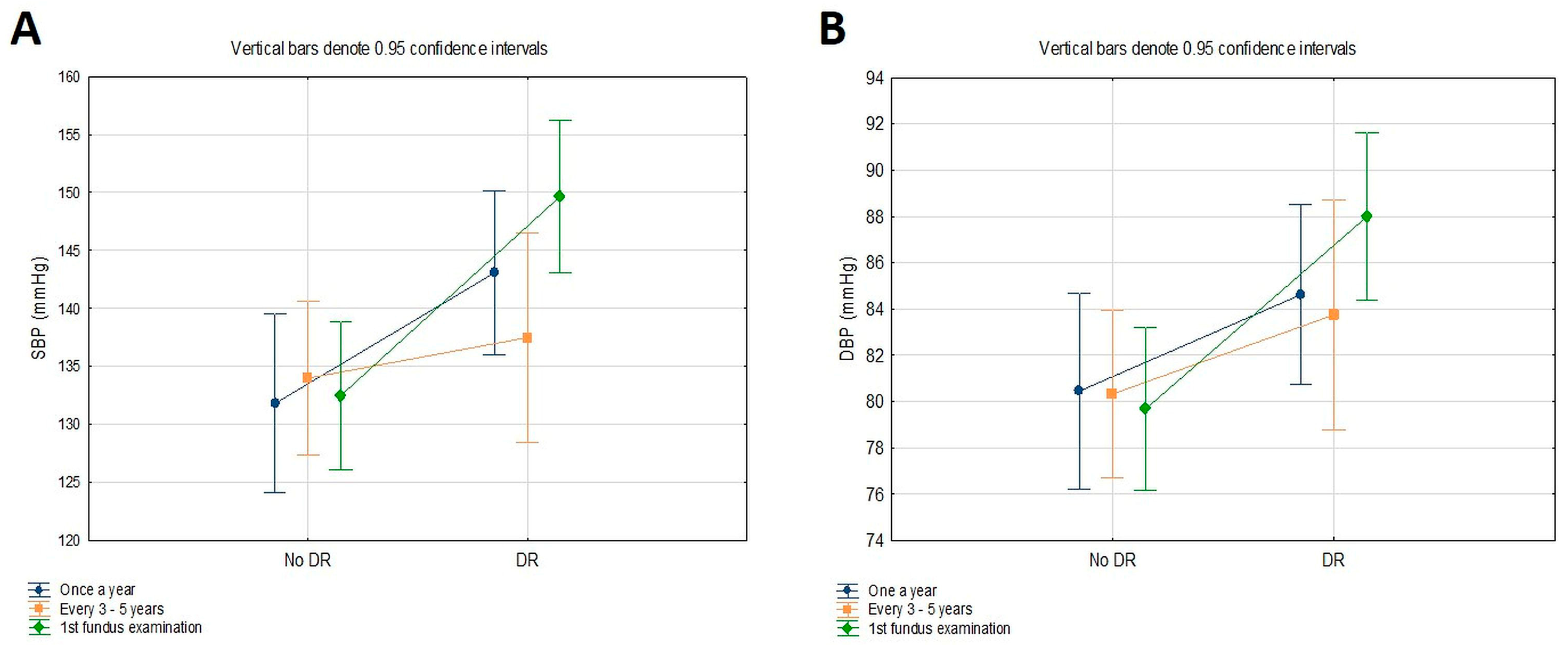
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021; Available online: http://www.diabetesatlas.org/ (accessed on 20 December 2023).
- Flaxman, S.R.; Bourne, R.R.A.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global causes of blindness and distance vision impairment 1990–2020: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef]
- Teo, Z.L.; Tham, Y.C.; Yu, M.; Chee, M.L.; Rim, T.H.; Cheung, N.; Bikbov, M.M.; Wang, Y.X.; Tang, Y.; Lu, Y.; et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: Systematic review and meta-analysis. Ophthalmology 2021, 128, 1580–1591. [Google Scholar] [CrossRef]
- Liew, G.; Michaelides, M.; Bunce, C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16–64 years), 1999–2000 with 2009–2010. BMJ. Open 2014, 4, e004015. [Google Scholar] [CrossRef]
- Claessen, H.; Kvitkina, T.; Narres, M.; Trautner, C.; Zöllner, I.; Bertram, B.; Icks, A. Markedly decreasing incidence of blindness in people with and without diabetes in southern Germany. Diabetes Care 2018, 41, 478–484. [Google Scholar] [CrossRef]
- Wong, T.Y.; Sun, J.; Kawasaki, R.; Ruamviboonsuk, P.; Gupta, N.; Lansingh, V.C.; Maia, M.; Mathenge, W.; Moreker, S.; Muqit, M.M.K.; et al. Guidelines on diabetic eye care: The international council of ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology 2018, 125, 1608–16622. [Google Scholar] [CrossRef]
- World Health Organization—Regional Office for Europe (WHO/Europe). Diabetic Retinopathy Screening: A Short Guide: Increase Effectiveness, Maximize Benefits and Minimize Harm; World Health Organization—Regional Office for Europe: Copenhagen, Denmark, 2020; Available online: https://apps.who.int/iris/handle/10665/336660 (accessed on 20 December 2023).
- Scanlon, P.H. The English National Screening Programme for diabetic retinopathy 2003–2016. Acta. Diabetol. 2017, 54, 515–525. [Google Scholar] [CrossRef]
- Pandey, R.; Morgan, M.M.; Murphy, C.; Kavanagh, H.; Acheson, R.; Cahill, M.; McGettrick, P.; O’Toole, L.; Hamroush, F.; Mooney, T.; et al. Irish National Diabetic RetinaScreen Programme: Report on five rounds of retinopathy screening and screen-positive referrals (INDEAR study report no. 1). Br. J. Ophthalmol. 2022, 106, 409–414. [Google Scholar] [CrossRef]
- Vujosevic, S.; Midena, E. Diabetic retinopathy in Italy: Epidemiology data and telemedicine screening programs. J. Diabetes. Res. 2016, 2016, 3627465. [Google Scholar] [CrossRef]
- Poljičanin, T.; Buble, T. National Diabetes Registry CroDiab—Report for 2021; Croatian Institute of Public Health: Zagreb, Croatia, 2022. [Google Scholar]
- Levey, A.S.; Stevens, L.A. Estimating GFR using the CKD Epidemiology Collaboration (CKD-EPI) creatinine equation: More accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am. J. Kidney Dis. 2010, 55, 622–627. [Google Scholar] [CrossRef]
- Aldington, S.J.; Kohner, E.M.; Meuer, S.; Klein, R.; Sjølie, A.K. Methodology for retinal photography and assessment of diabetic retinopathy: The EURODIAB IDDM complications study. Diabetologia 1995, 38, 437–4344. [Google Scholar] [CrossRef]
- Wilkinson, C.P.; Ferris, F.L., 3rd; Klein, R.E.; Lee, P.P.; Agardh, C.D.; Davis, M.; Dills, D.; Kampik, A.; Pararajasegaram, R.; Verdaguer, J.T.; et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003, 110, 1677–1682. [Google Scholar] [CrossRef]
- Diabetes Association Professional Practice Committee. Cardiovascular Disease and risk management. Standards of Medical Care in Diabetes-2024. Diabetes Care 2024, 47 (Suppl. S1), S179–S218. [Google Scholar] [CrossRef]
- Diabetes Association Professional Practice Committee. Glycemic Targets: Standards of Medical Care in Diabetes-2022. Diabetes Care 2022, 45 (Suppl. S1), S83–S96. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2022. Diabetes Care 2022, 45 (Suppl. S1), S144–S174. [Google Scholar] [CrossRef]
- Liebl, A.; Mata, M.; Eschwege, E. Evaluation of risk factors for development of complications in type II diabetes in Europe. Diabetologia 2002, 45, S23–S28. [Google Scholar] [CrossRef]
- de Pablos-Velasco, P.; Parhofer, K.G.; Bradley, C.; Eschwège, E.; Gönder-Frederick, L.; Maheux, P.; Wood, I.; Simon, D. Current level of glycaemic control and its associated factors in patients with type 2 diabetes across Europe: Data from the PANORAMA study. Clin. Endocrinol. 2014, 80, 47–56. [Google Scholar] [CrossRef]
- UK Prospective Diabetes Study Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998, 352, 837–853. [Google Scholar] [CrossRef]
- Matthews, D.R.; Stratton, I.M.; Aldington, S.J.; Holman, R.R.; Kohner, E.M. Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus (UKPDS 69). Arch. Ophthalmol. 2004, 122, 1631–1640. [Google Scholar] [CrossRef]
- Li, Y.-T.; Wang, Y.; Hu, X.-J.; Chen, J.-H.; Li, Y.-Y.; Zhong, Q.-Y.; Cheng, H.; Mohammed, B.H.; Liang, X.-L.; Hernandez, J.; et al. Association between Systolic Blood Pressure and Diabetic Retinopathy in Both Hypertensive and Normotensive Patients with Type 2 Diabetes: Risk Factors and Healthcare Implications. Healthcare 2021, 9, 580. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef]
- Zhang, M.; Wu, J.; Wang, Y.; Wu, J.; Hu, W.; Jia, H.; Sun, X. Associations between blood pressure levels and diabetic retinopathy in patients with diabetes mellitus: A population-based study. Heliyon 2023, 9, e16830. [Google Scholar] [CrossRef]
- Williams, M.E. The goal of blood pressure control for prevention of early diabetic microvascular complications. Curr. Diab. Rep. 2011, 11, 323–329. [Google Scholar] [CrossRef]
- Grunwald, J.E.; Dupont, J.; Riva, C.E. Retinal hemodynamics in patients with early diabetes mellitus. Br. J. Ophthalmol. 1996, 80, 327–331. [Google Scholar] [CrossRef]
- Del Pinto, R.; Mulè, G.; Vadalà, M.; Carollo, C.; Cottone, S.; Agabiti Rosei, C.; De Ciuceis, C.; Rizzoni, D.; Ferri, C.; Muiesan, M.L. Arterial Hypertension and the Hidden Disease of the Eye: Diagnostic Tools and Therapeutic Strategies. Nutrients 2022, 14, 2200. [Google Scholar] [CrossRef]
- Ansari, P.; Tabasumma, N.; Snigdha, N.N.; Siam, N.H.; Panduru, R.V.N.R.S.; Azam, S.; Hannan, J.M.A.; Abdel-Wahab, Y.H.A. Diabetic Retinopathy: An Overview on Mechanisms, Pathophysiology and Pharmacotherapy. Diabetology 2022, 3, 159–175. [Google Scholar] [CrossRef]
- Chang, Y.C.; Wu, W.C. Dyslipidemia and diabetic retinopathy. Rev. Diabet. Stud. 2013, 10, 121–132. [Google Scholar] [CrossRef]
- Gupta, A.; Gupta, V.; Thapar, S.; Bhansali, A. Lipid-lowering drug atorvastatin as an adjunct in the management of diabetic macular oedema. Am. J. Ophthalmol. 2004, 137, 675–682. [Google Scholar] [CrossRef]
- Keech, A.C.; Mitchell, P.; Summanen, P.A.; O’Day, J.; Davis, T.M.; Moffilitt, M.S.; Taskinen, M.-R.; Simes, R.J.; Tse, D.; Williamson, E.; et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): A randomised controlled trial. Lancet 2007, 370, 1687–1697. [Google Scholar] [CrossRef]
- Harb, W.; Harb, G.; Chamoun, N.; Kanbar, A.; Harb, M.; Chanbour, W. Severity of diabetic retinopathy at the first ophthalmological examination in the Lebanese population. Ther. Adv. Ophthalmol. 2018, 10, 2515841418791950. [Google Scholar] [CrossRef]
- Hristova, E.; Koseva, D.; Zlatarova, Z.; Dokova, K. Diabetic retinopathy screening and registration in Europe—Narrative review. Healthcare 2021, 9, 745. [Google Scholar] [CrossRef]
- Andersen, N.; Hjortdal, J.Ø.; Schielke, K.C.; Bek, T.; Grauslund, J.; Laugesen, C.S.; Lund-Andersen, H.; Cerqueira, C.; Andresen, J. The Danish Registry of Diabetic Retinopathy. Clin. Epidemiol. 2016, 8, 613–619. [Google Scholar] [CrossRef]
- Gudbjörnsdottir, S.; Cederholm, J.; Nilsson, P.M.; Eliasson, B.; Steering Committee of the Swedish National Diabetes Register. The National Diabetes Register in Sweden: An implementation of the St. Vincent Declaration for Quality Improvement in Diabetes Care. Diabetes Care 2003, 26, 1270–1276. [Google Scholar] [CrossRef]
- Carlsen, S.; Skrivarhaug, T.; Thue, G.; Cooper, J.G.; Gøransson, L.; Løvaas, K.; Sandberg, S. Glycemic control and complications in patients with type 1 diabetes—A registry-based longitudinal study of adolescents and young adults. Pediatr. Diabetes 2017, 18, 188–195. [Google Scholar] [CrossRef]
- Garg, S.; Jani, P.D.; Kshirsagar, A.V.; King, B.; Chaum, E. Telemedicine and retinal imaging for improving diabetic retinopathy evaluation. Arch. Intern. Med. 2012, 172, 1677–1678. [Google Scholar] [CrossRef][Green Version]
- Padhy, S.K.; Takkar, B.; Chawla, R.; Kumar, A. Artificial intelligence in diabetic retinopathy: A natural step to the future. Indian J. Ophthalmol. 2019, 67, 1004–1009. [Google Scholar] [CrossRef]
- Huemer, J.; Wagner, S.K.; Sim, D.A. The evolution of diabetic retinopathy screening programmes: A chronology of retinal photography from 35 mm slides to artificial intelligence. Clin. Ophthalmol. 2020, 14, 2021–2035. [Google Scholar] [CrossRef]
- Tomić, M.; Vrabec, R.; Hendelja, Đ.; Kolarić, V.; Bulum, T.; Rahelić, D. Diagnostic Accuracy of Hand-Held Fundus Camera and Artificial Intelligence in Diabetic Retinopathy Screening. Biomedicines 2024, 12, 34. [Google Scholar] [CrossRef]
- Mansberger, S.L.; Sheppler, C.; Barker, G.; Gardiner, S.K.; Demirel, S.; Wooten, K.; Becker, T.M. Long-term Comparative Effectiveness of Telemedicine in Providing Diabetic Retinopathy Screening Examinations: A Randomized Clinical Trial. JAMA Ophthalmol. 2015, 133, 518–525. [Google Scholar] [CrossRef]
- van der Heijden, A.A.; Abramoff, M.D.; Verbraak, F.; van Hecke, M.V.; Liem, A.; Nijpels, G. Validation of automated screening for referable diabetic retinopathy with the IDx-DR device in the Hoorn Diabetes Care System. Acta. Ophthalmol. 2018, 96, 63–68. [Google Scholar] [CrossRef]
| No DR (n = 84) | NPDR (n = 44) | STDR (n = 28) | p-Value | |
|---|---|---|---|---|
| Age (yr) | 65.53 ± 7.52 | 64.68 ± 7.23 | 63.97 ± 7.74 | 0.139 |
| Gender (m/f) (%) | 52/48 | 59/41 | 68/32 | 0.195 |
| Diabetes duration (yr) | 11.83 ± 6.77 | 15.28 ± 5.44 | 17.03 ± 4.28 | 0.015 |
| BMI (kg/m2) | 29.59 ± 4.70 | 31.39 ± 5.38 | 28.21 ± 2.49 | 0.119 |
| SBP (mmHg) | 132.85 ± 11.21 | 140.45 ± 15.58 | 151.07 ± 10.77 | <0.001 |
| DBP (mmHg) | 80.12 ± 5.24 | 85.23 ± 9.69 | 86.79 ± 6.68 | 0.002 |
| HbA1c (%) | 6.7 (5.5–9.4) | 7.3 (5.8–9.7) | 7.9 (5.9–12.2) | 0.004 |
| Total cholesterol (mmol/L) | 4.7 (2.7–10.2) | 4.6 (3.1–6.3) | 5.3 (2.7–7.1) | 0.587 |
| HDL cholesterol (mmol/L) | 1.4 (0.8–2.6) | 1.2 (0.8–2.1) | 1.2 (1.0–2.0) | 0.258 |
| LDL cholesterol (mmol/L) | 2.5 (1.1–7.1) | 2.4 (0.9–4.3) | 2.9 (1.3–4.9) | 0.328 |
| Triglycerides (mmol/L) | 1.6 (0.5–6.3) | 1.9 (0.8–7.0) | 1.3 (0.5–3.4) | 0.099 |
| Serum creatinine (μmol/L) | 73.5 (50–130) | 77.5 (49–135) | 74 (42–156) | 0.680 |
| eGFR (mL/min/1.73 m2) | 85.5 (43–108) | 82 (35–105) | 89.5 (38–108) | 0.412 |
| ACR (mg/mmol) | 1.4 (0.3–9.0) | 1.3 (0.5–18.1) | 1.1 (0.4–19.1) | 0.772 |
| Variable | OR (95% CI) | p-Value | AOR (95% CI) * | p-Value * |
|---|---|---|---|---|
| Diabetes duration | 1.11 (1.05–1.21) | 0.007 | / | |
| HbA1c | 1.98 (1.20–3.27) | 0.006 | / | |
| SBP | 1.07 (1.02–1.12) | <0.001 | 1.07 (1.02–1.12) | 0.003 |
| DBP | 1.14 (1.05–1.23) | 0.002 | 1.13 (1.04–1.24) | 0.005 |
| <130/80 mmHg (n = 42) | ≥130/80 mmHg (n = 114) | p-Value | |
|---|---|---|---|
| DR status (No DR/DR) (%) | 88/12 | 50/50 | 0.043 |
| Age (yr) | 63.37 ± 10.79 | 64.31 ± 7.38 | 0.746 |
| Gender (m/f) (%) | 87/13 | 56/44 | 0.083 |
| Diabetes duration (yr) | 9.50 ± 7.80 | 14.38 ± 6.96 | 0.067 |
| BMI (kg/m2) | 25.36 ± 3.03 | 30.37 ± 4.57 | 0.003 |
| SBP (mmHg) | 120.62 ± 6.78 | 140.28 ± 13.35 | <0.001 |
| DBP (mmHg) | 73.12 ± 4.58 | 84.86 ± 3.97 | <0.001 |
| HbA1c (%) | 6.6 (5.6–9.1) | 7.1 (5.5–12.1) | 0.553 |
| Total cholesterol (mmol/L) | 4.5 (3.8–7.4) | 4.6 (2.7–10.2) | 0.680 |
| HDL cholesterol (mmol/L) | 1.4 (1.2–1.9) | 1.3 (0.8–2.5) | 0.429 |
| LDL cholesterol (mmol/L) | 2.5 (1.6–4.7) | 2.4 (0.9–7.1) | 0.415 |
| Triglycerides (mmol/L) | 1.3 (0.5–2.7) | 1.6 (0.5–7.0) | 0.323 |
| Serum creatinine (μmol/L) | 79.0 (56–90) | 74.5 (42–156) | 0.993 |
| eGFR (mL/min/1.73 m2) | 96.0 (68–104) | 85.5 (35–119) | 0.202 |
| ACR (mg/mmol) | 0.9 (0.3–6.4) | 1.4 (0.4–19.1) | 0.033 |
| SBP | DBP | |||||
|---|---|---|---|---|---|---|
| df | F | p | df | F | p | |
| DR | 1 | 12.023 | <0.001 | 1 | 6.613 | 0.012 |
| ACR | 1 | 0.108 | 0.743 | 1 | 0.252 | 0.617 |
| DR and ACR | 1 | 0.990 | 0.323 | 1 | 0.001 | 0.975 |
| SBP | DBP | |||||
|---|---|---|---|---|---|---|
| df | F | p | df | F | p | |
| DR | 1 | 12.647 | <0.001 | 1 | 10.428 | 0.002 |
| Frequency of fundus examination | 1 | 1.185 | 0.312 | 1 | 0.467 | 0.630 |
| DR and frequency of fundus examination | 1 | 1.767 | 0.178 | 1 | 0.952 | 0.392 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomić, M.; Vrabec, R.; Ljubić, S.; Prkačin, I.; Bulum, T. Patients with Type 2 Diabetes, Higher Blood Pressure, and Infrequent Fundus Examinations Have a Higher Risk of Sight-Threatening Retinopathy. J. Clin. Med. 2024, 13, 2496. https://doi.org/10.3390/jcm13092496
Tomić M, Vrabec R, Ljubić S, Prkačin I, Bulum T. Patients with Type 2 Diabetes, Higher Blood Pressure, and Infrequent Fundus Examinations Have a Higher Risk of Sight-Threatening Retinopathy. Journal of Clinical Medicine. 2024; 13(9):2496. https://doi.org/10.3390/jcm13092496
Chicago/Turabian StyleTomić, Martina, Romano Vrabec, Spomenka Ljubić, Ingrid Prkačin, and Tomislav Bulum. 2024. "Patients with Type 2 Diabetes, Higher Blood Pressure, and Infrequent Fundus Examinations Have a Higher Risk of Sight-Threatening Retinopathy" Journal of Clinical Medicine 13, no. 9: 2496. https://doi.org/10.3390/jcm13092496
APA StyleTomić, M., Vrabec, R., Ljubić, S., Prkačin, I., & Bulum, T. (2024). Patients with Type 2 Diabetes, Higher Blood Pressure, and Infrequent Fundus Examinations Have a Higher Risk of Sight-Threatening Retinopathy. Journal of Clinical Medicine, 13(9), 2496. https://doi.org/10.3390/jcm13092496










