Effects of Pain Neuroscience Education and Physiotherapy on Chronic Low Back Pain, Fear of Movement and Functional Status: A Randomised Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Questionnaires
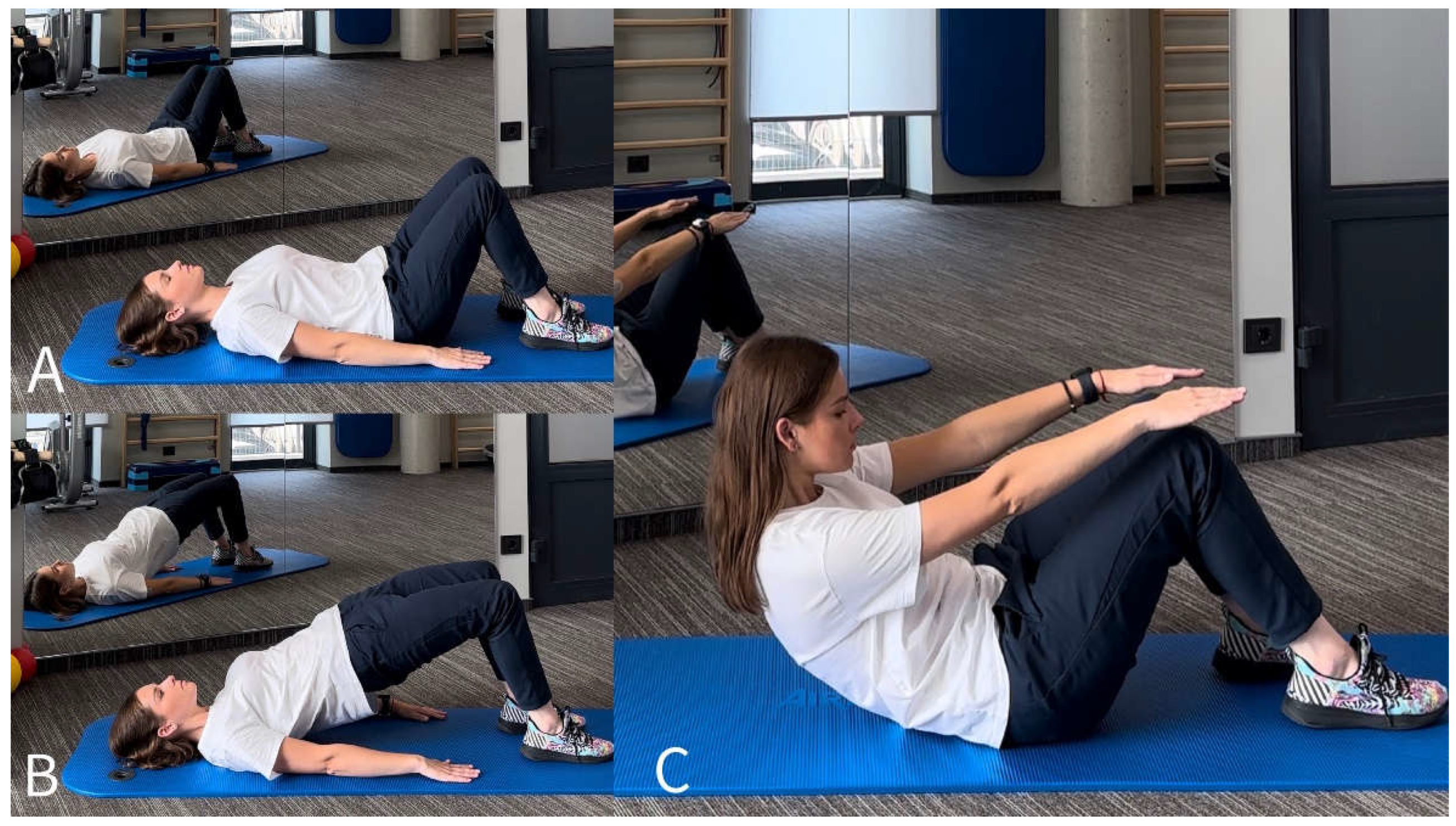
2.2. Physiotherapy Program
2.3. Pain Neuroscience Education Program
2.4. Statistics
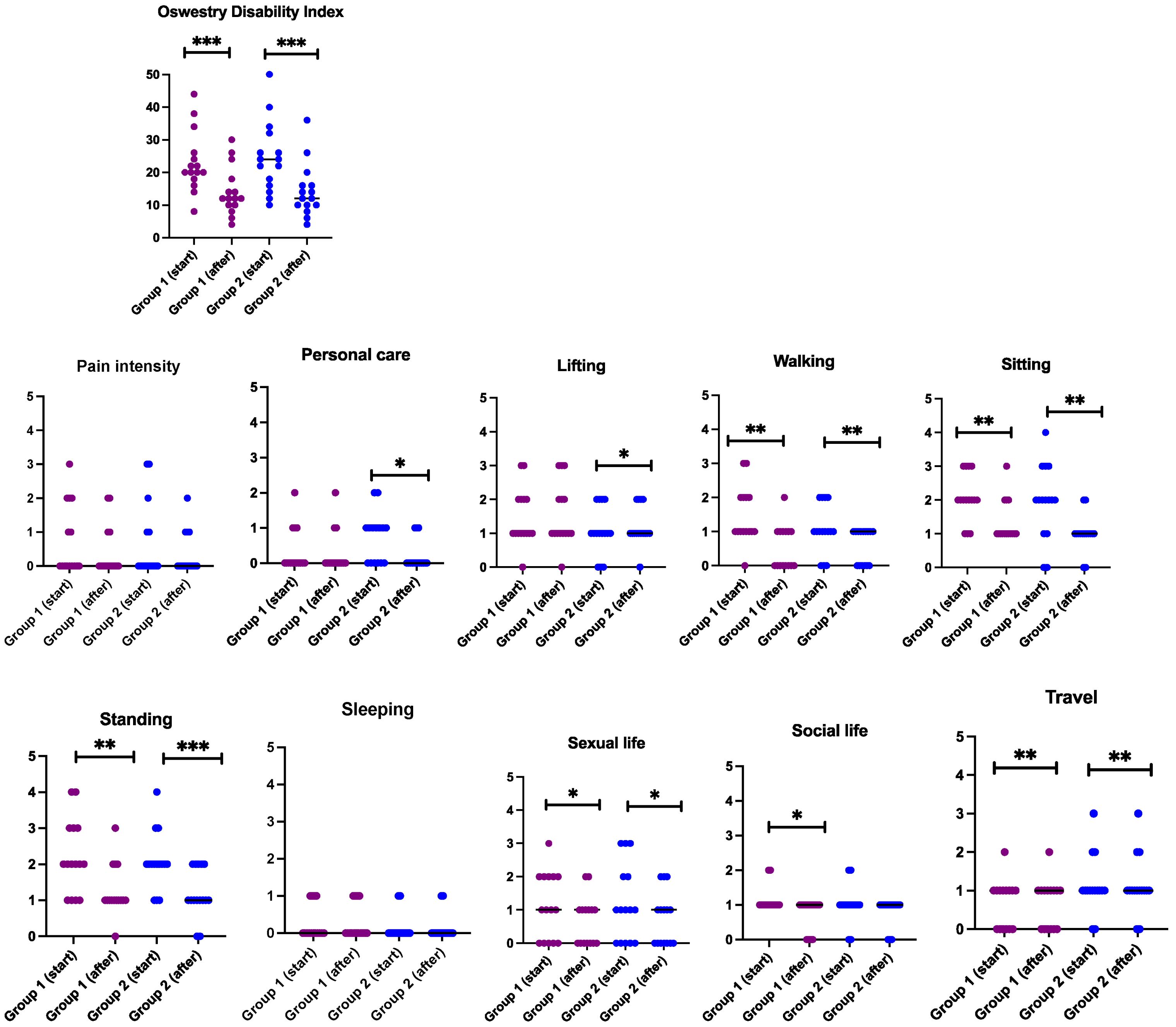
3. Results
3.1. Sociodemographic Data
3.2. Assessment of the Outcomes Measures
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef] [PubMed]
- Lietuvos Statistikos Departamentas. Rodiklių Duomenų bazė—Oficialiosios Statistikos Portalas. 2018. Available online: https://osp.stat.gov.lt/statistikos-leidiniu-katalogas?publication=33980 (accessed on 22 January 2024).
- O’Sullivan, P.B.; Caneiro, J.P.; O’Keeffe, M.; Smith, A.; Dankaerts, W.; Fersum, K.; O’Sullivan, K. Cognitive Functional Therapy: An Integrated Behavioral Approach for the Targeted Management of Disabling Low Back Pain. Phys. Ther. 2018, 98, 408–423. [Google Scholar] [CrossRef] [PubMed]
- Bardin, L.D.; King, P.; Maher, C.G. Diagnostic triage for low back pain: A practical approach for primary care. Med. J. Aust. 2017, 206, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Sahin, N.; Karahan, A.Y.; Albayrak, I. Effectiveness of physical therapy and exercise on pain and functional status in patients with chronic low back pain: A randomized-controlled trial. Turk. J. Phys. Med. Rehabil. 2018, 64, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Frizziero, A.; Pellizzon, G.; Vittadini, F.; Bigliardi, D.; Costantino, C. Efficacy of Core Stability in Non-Specific Chronic Low Back Pain. J. Funct. Morphol. Kinesiol. 2021, 6, 37. [Google Scholar] [CrossRef]
- Sipaviciene, S.; Kliziene, I. Effect of different exercise programs on non-specific chronic low back pain and disability in people who perform sedentary work. Clin. Biomech. 2020, 73, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Smrcina, Z.; Woelfel, S.; Burcal, C. A Systematic Review of the Effectiveness of Core Stability Exercises in Patients with Non-Specific Low Back Pain. Int. J. Sports Phys. Ther. 2022, 17, 766–774. [Google Scholar] [CrossRef]
- Fatemi, R.; Javid, M.; Najafabadi, E.M. Effects of William training on lumbosacral muscles function, lumbar curve and pain. J. Back Musculoskelet. Rehabil. 2015, 28, 591–597. [Google Scholar] [CrossRef]
- Szulc, P.; Wendt, M.; Waszak, M.; Tomczak, M.; Cieslik, K.; Trzaska, T. Impact of McKenzie Method Therapy Enriched by Muscular Energy Techniques on Subjective and Objective Parameters Related to Spine Function in Patients with Chronic Low Back Pain. Med. Sci. Monit. 2015, 21, 2918–2932. [Google Scholar] [CrossRef]
- Shariat, A.; Cleland, J.A.; Danaee, M.; Kargarfard, M.; Sangelaji, B.; Tamrin, S.B.M. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: A randomized controlled trial. Braz. J. Phys. Ther. 2018, 22, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Coggon, D.; Falah-Hassani, K. Exercise for the Prevention of Low Back Pain: Systematic Review and Meta-Analysis of Controlled Trials. Am. J. Epidemiol. 2018, 187, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.; Bloxham, S. A Systematic Review of the Effects of Exercise and Physical Activity on Non-Specific Chronic Low Back Pain. Healthcare 2016, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.; Hendrick, P.A. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur. J. Pain 2019, 23, 234–249. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Zimney, K.; O’Hotto, C.; Hilton, S. The clinical application of teaching people about pain. Physiother. Theory Pract. 2016, 32, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Puentedura, E.J.; Flynn, T. Combining manual therapy with pain neuroscience education in the treatment of chronic low back pain: A narrative review of the literature. Physiother. Theory Pract. 2016, 32, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Robins, H.; Perron, V.; Heathcote, L.C.; Simons, L.E. Pain Neuroscience Education: State of the Art and Application in Pediatrics. Children 2016, 3, 43. [Google Scholar] [CrossRef] [PubMed]
- Wijma, A.J.; Speksnijder, C.M.; Crom-Ottens, A.F.; Knulst-Verlaan, J.M.C.; Keizer, D.; Nijs, J.; van Wilgen, C.P. What is important in transdisciplinary pain neuroscience education? A qualitative study. Disabil. Rehabil. 2018, 40, 2181–2191. [Google Scholar] [CrossRef] [PubMed]
- Meise, R.; Ferreira Carvalho, G.; Thiel, C.; Luedtke, K. Additional effects of pain neuroscience education combined with physiotherapy on the headache frequency of adult patients with migraine: A randomized controlled trial. Cephalalgia 2023, 43, 3331024221144781. [Google Scholar] [CrossRef]
- Williamson, A.; Hoggart, B. Pain: A review of three commonly used pain rating scales. J. Clin. Nurs. 2005, 14, 798–804. [Google Scholar] [CrossRef]
- French, D.J.; France, C.R.; Vigneau, F.; French, J.A.; Evans, R.T. Fear of movement/(re)injury in chronic pain: A psychometric assessment of the original English version of the Tampa scale for kinesiophobia (TSK). Pain 2007, 127, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952, discussion 2952. [Google Scholar] [CrossRef] [PubMed]
- Samėnienė J, M.T.; Medzevičiūtė, R.; Valančiūtė, A.; Brazauskaitė, L.; Narauskas, R. Nugaros skausmo įtaka paciento funkcinei būklei ir gyvenimo kokybei bei jo vertinimas reabilitacijoje. Skausmo Med. 2005, 2, 11–13. [Google Scholar]
- Roland, M.; Fairbank, J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000, 25, 3115–3124. [Google Scholar] [CrossRef] [PubMed]
- Iversen, V.M.; Vasseljen, O.; Mork, P.J.; Berthelsen, I.R.; Borke, J.B.; Berheussen, G.F.; Tveter, A.T.; Salvesen, O.; Fimland, M.S. Resistance training in addition to multidisciplinary rehabilitation for patients with chronic pain in the low back: Study protocol. Contemp. Clin. Trials Commun. 2017, 6, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.J.; Choi, K.H.; Kim, D.H.; Kim, H.J.; Cho, Y.K.; Lee, K.H.; Kim, J.H.; Choi, Y.J. Effect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back pain. Ann. Rehabilitation Med. 2013, 37, 110–117. [Google Scholar] [CrossRef]
- Boucher, J.A.; Preuss, R.; Henry, S.M.; Dumas, J.P.; Lariviere, C. The effects of an 8-week stabilization exercise program on lumbar movement sense in patients with low back pain. BMC Musculoskelet. Disord. 2016, 17, 23. [Google Scholar] [CrossRef] [PubMed]
- Gorji, S.M.; Mohammadi Nia Samakosh, H.; Watt, P.; Henrique Marchetti, P.; Oliveira, R. Pain Neuroscience Education and Motor Control Exercises versus Core Stability Exercises on Pain, Disability, and Balance in Women with Chronic Low Back Pain. Int. J. Environ. Res. Public Health 2022, 19, 2694. [Google Scholar] [CrossRef]
- Malfliet, A.; Kregel, J.; Coppieters, I.; De Pauw, R.; Meeus, M.; Roussel, N.; Cagnie, B.; Danneels, L.; Nijs, J. Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA Neurol. 2018, 75, 808–817. [Google Scholar] [CrossRef]
- Kim, K.S.; An, J.; Kim, J.O.; Lee, M.Y.; Lee, B.H. Effects of Pain Neuroscience Education Combined with Lumbar Stabilization Exercise on Strength and Pain in Patients with Chronic Low Back Pain: Randomized Controlled Trial. J. Pers. Med. 2022, 12, 303. [Google Scholar] [CrossRef]
- Watson, J.A.; Ryan, C.G.; Cooper, L.; Ellington, D.; Whittle, R.; Lavender, M.; Dixon, J.; Atkinson, G.; Cooper, K.; Martin, D.J. Pain Neuroscience Education for Adults with Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J. Pain 2019, 20, 1140.e1–1140.e22. [Google Scholar] [CrossRef] [PubMed]
- Wijma, A.J.; van Wilgen, C.P.; Meeus, M.; Nijs, J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiother. Theory Pract. 2016, 32, 368–384. [Google Scholar] [CrossRef] [PubMed]
- Gul, H.; Erel, S.; Toraman, N.F. Physiotherapy combined with therapeutic neuroscience education versus physiotherapy alone for patients with chronic low back pain: A pilot, randomized-controlled trial. Turk. J. Phys. Med. Rehabil. 2021, 67, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Siddall, B.; Ram, A.; Jones, M.D.; Booth, J.; Perriman, D.; Summers, S.J. Short-term impact of combining pain neuroscience education with exercise for chronic musculoskeletal pain: A systematic review and meta-analysis. Pain 2022, 163, e20–e30. [Google Scholar] [CrossRef] [PubMed]


| Participants with Low Back Pain (n = 30) | |
| I group (n = 15) | II group (n = 15) |
| I assessment | |
| 1. Assessment of pain intensity using the numeric rating scale (NRS); 2. Assessment of fear of movement using the Tampa scale; 3. Assessment of the impact of back pain on the patient’s functional capacity according to the Oswestry disability index; 4. Assessment of functional disability using the Roland–Morris questionnaire. | |
| Intervention | |
| I group (n = 15) | II group (n = 15) |
| 1. Physiotherapy | 1. Physiotherapy |
| (a) Spinal stabilization exercises; (b) Muscle strength training exercises; (c) Stretching exercises. Session duration—45 min/2 times per week for 10 weeks. | |
| 2. The educational program about the pain and its recognition (2 times, each 30 min). | |
| II assessment | |
| Analysis of results | |
| Method | Description |
|---|---|
| Numeric rating scale (NRS) | This is used for the quantitative assessment of pain. The intensity of pain is compared before and after the intervention. At the same time, the effectiveness of the treatment for the patients is evaluated. The numeric rating scale (NRS) consists of 11 numbers on a scale from 0 to 10 [21]. Pain scoring: 0 points—no pain; 1–3 points—mild pain; 4–5 points—moderate pain; 6–8 points—severe pain; 9–10 points—very severe pain. |
| Tampa scale of kinesiophobia | The scale is used to assess fear of movement or re-injury in individuals who experience pain. Higher fear of movement scores are associated with depression and anxiety.The questionnaire consists of 17 questions, which have 4 answer options:
|
| Oswestry disability index | Intended to assess the impact of back pain on the patient’s functional ability, including various life situations and daily activities. The questionnaire consists of 10 questions with 6 answers each (A-F). The letter of each answer is scored: A—0; B—1; C—2; D–3; E—4; F—5. Zero points is the highest rating for the feature, 50 points is the lowest. The obtained scores are multiplied by two and converted into percentages [23]. Assessment was adapted according to Samėnienė et al. [24]: 0–20 percent—minimal dysfunction; 2–40 percent—moderate dysfunction; 40–60 percent—severe dysfunction; 60–80 percent—disability; 80–100 percent—bed rest (or simulated symptoms). |
| Roland–Morris disability questionnaire | Intended to assess the impact of lower back pain on the patient’s functional condition. Based on the SIP (sickness impact profile) questionnaire. The effectiveness of the intervention is evaluated after the repeated filling of this questionnaire after the applied effect so as to monitor the patient’s functional status. Rating scale—0–24. The lower the score, the lower the impact of lower back pain on the functional state of the person [25]. |
| Demographic Factors | I Group (Physiotherapy) | II Group (Physiotherapy with PNE) | In General | Comparison between the Groups | |
|---|---|---|---|---|---|
| Age | 33.13 ± 4.37 | 33.8 ± 4.51 | 33.47 ± 4.38 | U = 102.0; p = 0.683 | |
| Gender | Women | 53.3 (8) | 73.3 (11) | 63.3 (19) | χ2(1) = 1.292; p = 0.256 |
| Men | 46.7 (7) | 26.7 (4) | 36.7 (11) | ||
| Do you often complain of pain in the lower back? | Every day | 53.3 (8) | 33.3 (5) | 43.3 (13) | U = 86.0; p = 0.301 |
| Once or several times a week | 33.3 (5) | 40 (6) | 36.7 (11) | ||
| More rarely | 13.3 (2) | 26.7 (4) | 20 (6) | ||
| Have you ever had a spinal injury or disease? | Yes | 13.3 (2) | 6.7 (1) | 10 (3) | U = 105.0; p = 1.0 |
| No | 86.7 (13) | 93.3 (14) | 90 (27) | ||
| Do you have any co-morbidities? | Yes | 13.3 (2) | - | 6.7 (2) | U = 97.5; p = 0.483 |
| No | 86.7 (13) | 100 (15) | 93.3 (28) | ||
| Does the pain limit daily activities and functions? | Yes | 100 (15) | 93.3 (14) | 96.7 (29) | U = 105.0; p = 1.0 |
| No | - | 6.7 (1) | 3.3 (1) | ||
| Do you take medication for lower back pain? | Yes | 26.7 (4) | 20 (3) | 23.3 (7) | U = 105.0; p = 1.0 |
| No | 73.3 (11) | 80 (12) | 76.7 (23) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lendraitienė, E.; Styraitė, B.; Šakalienė, R.; Misytė, G.; Bileviciute-Ljungar, I. Effects of Pain Neuroscience Education and Physiotherapy on Chronic Low Back Pain, Fear of Movement and Functional Status: A Randomised Pilot Study. J. Clin. Med. 2024, 13, 2081. https://doi.org/10.3390/jcm13072081
Lendraitienė E, Styraitė B, Šakalienė R, Misytė G, Bileviciute-Ljungar I. Effects of Pain Neuroscience Education and Physiotherapy on Chronic Low Back Pain, Fear of Movement and Functional Status: A Randomised Pilot Study. Journal of Clinical Medicine. 2024; 13(7):2081. https://doi.org/10.3390/jcm13072081
Chicago/Turabian StyleLendraitienė, Eglė, Barbora Styraitė, Rasa Šakalienė, Gabija Misytė, and Indre Bileviciute-Ljungar. 2024. "Effects of Pain Neuroscience Education and Physiotherapy on Chronic Low Back Pain, Fear of Movement and Functional Status: A Randomised Pilot Study" Journal of Clinical Medicine 13, no. 7: 2081. https://doi.org/10.3390/jcm13072081
APA StyleLendraitienė, E., Styraitė, B., Šakalienė, R., Misytė, G., & Bileviciute-Ljungar, I. (2024). Effects of Pain Neuroscience Education and Physiotherapy on Chronic Low Back Pain, Fear of Movement and Functional Status: A Randomised Pilot Study. Journal of Clinical Medicine, 13(7), 2081. https://doi.org/10.3390/jcm13072081








