New Frontiers in Electrocardiography, Cardiac Arrhythmias, and Arrhythmogenic Disorders
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Podolec, P.; Baranchuk, A.; Brugada, J.; Kukla, P.; Lelakowski, J.; Kopec, G.; Rubis, P.; Stepniewski, J.; Podolec, J.; Komar, M.; et al. Clinical classification of rare cardiac arrhythmogenic and conduction disorders, and rare arrhythmias. Pol. Arch. Intern. Med. 2019, 129, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Verheul, L.M.; van der Ree, M.H.; Groeneveld, S.A.; Mulder, B.A.; Christiaans, I.; Kapel, G.F.L.; Alings, M.; Bootsma, M.; Barge-Schaapveld, D.; Balt, J.C.; et al. The genetic basis of apparently idiopathic ventricular fibrillation: A retrospective overview. Europace 2023, 25, euad336. [Google Scholar] [CrossRef] [PubMed]
- Borowiec, K.; Wozniak, O.; Wrobel, A.; Smigielski, W.; Skrzypczynska-Banasik, U.; Kowalik, E.; Lutynska, A.; Hoffman, P.; Biernacka, E.K. A new model for predicting adverse outcomes in arrhythmogenic right ventricular cardiomyopathy. Pol. Arch. Intern. Med. 2023, 133, 16443. [Google Scholar] [CrossRef] [PubMed]
- Matusik, P.T.; Heleniak, Z.; Papuga-Szela, E.; Plens, K.; Lelakowski, J.; Undas, A. Chronic Kidney Disease and Its Impact on a Prothrombotic State in Patients with Atrial Fibrillation. J. Clin. Med. 2020, 9, 2476. [Google Scholar] [CrossRef] [PubMed]
- Holmstrom, L.; Zhang, F.Z.; Ouyang, D.; Dey, D.; Slomka, P.J.; Chugh, S.S. Artificial Intelligence in Ventricular Arrhythmias and Sudden Death. Arrhythm. Electrophysiol. Rev. 2023, 12, e17. [Google Scholar] [CrossRef] [PubMed]
- Mizner, J.; Waldauf, P.; Grieco, D.; Linkova, H.; Ionita, O.; Vijayaraman, P.; Petr, R.; Rakova, R.; Vesela, J.; Stros, P.; et al. A randomized comparison of HBP versus RVP: Effect on left ventricular function and biomarkers of collagen metabolism. Kardiol. Pol. 2023, 81, 472–481. [Google Scholar] [CrossRef] [PubMed]
- Kempa, M.; Budrejko, S.; Tajstra, M.; Syska, P.; Lewandowski, M.; Fabiszak, T.; Michalak, M.; Stanek, A.; Nowak, K.; Mitkowski, P.; et al. Subcutaneous implantable cardioverter-defibrillator therapy in Poland: Results of the Polish S-ICD Registry. Kardiol. Pol. 2023, 81, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Neugebauer, F.; Noti, F.; van Gool, S.; Roten, L.; Baldinger, S.H.; Seiler, J.; Madaffari, A.; Servatius, H.; Ryser, A.; Tanner, H.; et al. Leadless atrioventricular synchronous pacing in an outpatient setting: Early lessons learned on factors affecting atrioventricular synchrony. Heart Rhythm. 2022, 19, 748–756. [Google Scholar] [CrossRef]
- Knops, R.E.; Reddy, V.Y.; Ip, J.E.; Doshi, R.; Exner, D.V.; Defaye, P.; Canby, R.; Bongiorni, M.G.; Shoda, M.; Hindricks, G.; et al. A Dual-Chamber Leadless Pacemaker. N. Engl. J. Med. 2023, 388, 2360–2370. [Google Scholar] [CrossRef] [PubMed]
- Callahan, T.D.T.; Wilkoff, B.L. Extraction of a 5-year-old leadless pacemaker using a competing manufacturer’s removal tool. HeartRhythm Case Rep. 2023, 9, 441–444. [Google Scholar] [CrossRef]
- Scheinman, M.M.; Morady, F.; Hess, D.S.; Gonzalez, R. Catheter-induced ablation of the atrioventricular junction to control refractory supraventricular arrhythmias. JAMA 1982, 248, 851–855. [Google Scholar] [CrossRef] [PubMed]
- Gerstenfeld, E.P. Contact force-sensing catheters: Evolution or revolution in catheter ablation technology? Circ. Arrhythm. Electrophysiol. 2014, 7, 5–6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoffmayer, K.S.; Gerstenfeld, E.P. Contact force-sensing catheters. Curr. Opin. Cardiol. 2015, 30, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, K.; Nakagawa, H.; Shah, D.C.; Lambert, H.; Leo, G.; Aeby, N.; Ikeda, A.; Pitha, J.V.; Sharma, T.; Lazzara, R.; et al. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ. Arrhythm. Electrophysiol. 2008, 1, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Mussigbrodt, A.; Grothoff, M.; Dinov, B.; Kosiuk, J.; Richter, S.; Sommer, P.; Breithardt, O.A.; Rolf, S.; Bollmann, A.; Arya, A.; et al. Irrigated tip catheters for radiofrequency ablation in ventricular tachycardia. Biomed. Res. Int. 2015, 2015, 389294. [Google Scholar] [CrossRef] [PubMed]
- Bravo, L.; Atienza, F.; Eidelman, G.; Avila, P.; Pelliza, M.; Castellanos, E.; Loughlin, G.; Datino, T.; Torrecilla, E.G.; Almendral, J.; et al. Safety and efficacy of cryoablation vs. radiofrequency ablation of septal accessory pathways: Systematic review of the literature and meta-analyses. Europace 2018, 20, 1334–1342. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Haines, D.E.; Boersma, L.V.; Sood, N.; Natale, A.; Marchlinski, F.E.; Calkins, H.; Sanders, P.; Packer, D.L.; Kuck, K.H.; et al. Pulsed Field Ablation for the Treatment of Atrial Fibrillation: PULSED AF Pivotal Trial. Circulation 2023, 147, 1422–1432. [Google Scholar] [CrossRef] [PubMed]
- Rauber, M.; Manninger, M.; Eberl, A.S.; Scherr, D. Zero-fluoroscopy ablation with multielectrode pulse field ablation system: Case series. Pacing Clin. Electrophysiol. 2024, 47, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Miszczyk, M.; Sajdok, M.; Bednarek, J.; Latusek, T.; Wojakowski, W.; Tomasik, B.; Wita, K.; Jadczyk, T.; Kurzelowski, R.; Drzewiecka, A.; et al. Stereotactic management of arrhythmia-radiosurgery in treatment of ventricular tachycardia (SMART-VT). Results of a prospective safety trial. Radiother. Oncol. 2023, 188, 109857. [Google Scholar] [CrossRef] [PubMed]
- Aziz, H.M.; Zarzecki, M.P.; Garcia-Zamora, S.; Kim, M.S.; Bijak, P.; Tse, G.; Won, H.H.; Matusik, P.T. Pathogenesis and Management of Brugada Syndrome: Recent Advances and Protocol for Umbrella Reviews of Meta-Analyses in Major Arrhythmic Events Risk Stratification. J. Clin. Med. 2022, 11, 1912. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Belley-Cote, E.P.; Qiu, Y.; Belesiotis, P.; Tao, B.; Wolf, A.; Kaur, H.; Ibrahim, A.; Wong, J.A.; Wang, M.K.; et al. Rhythm vs. Rate Control in Patients with Postoperative Atrial Fibrillation after Cardiac Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 4534. [Google Scholar] [CrossRef] [PubMed]
- Bun, S.S.; Heme, N.; Asarisi, F.; Squara, F.; Scarlatti, D.; Moceri, P.; Ferrari, E. Prevalence and Clinical Characteristics of Patients with Torsades de Pointes Complicating Acquired Atrioventricular Block. J. Clin. Med. 2023, 12, 1067. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, E.A.; Schwamm, L.H.; Adeoye, O.M.; Alabi, O.; Jahangir, E.; Misra, S.; Still, C.H.; American Heart Association Council on Cardiovascular Radiology and Intervention; Council on Hypertension, Council on the Kidney in Cardiovascular Disease; Stroke, C. An Overview of Telehealth in the Management of Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2022, 146, e558–e568. [Google Scholar] [CrossRef] [PubMed]
- Matusik, P.; Mazur, P.; Stepien, E.; Pfitzner, R.; Sadowski, J.; Undas, A. Architecture of intraluminal thrombus removed from abdominal aortic aneurysm. J. Thromb. Thrombolysis 2010, 30, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Rubis, P.; Wisniowska-Smialek, S.; Biernacka-Fijalkowska, B.; Rudnicka-Sosin, L.; Wypasek, E.; Kozanecki, A.; Dziewiecka, E.; Faltyn, P.; Karabinowska, A.; Khachatryan, L.; et al. Left ventricular reverse remodeling is not related to biopsy-detected extracellular matrix fibrosis and serum markers of fibrosis in dilated cardiomyopathy, regardless of the definition used for LVRR. Heart Vessels 2017, 32, 714–725. [Google Scholar] [CrossRef] [PubMed]
- Matusik, P.; Dubiel, M.; Wizner, B.; Fedyk-Lukasik, M.; Zdrojewski, T.; Opolski, G.; Dubiel, J.; Grodzicki, T. Age-related gap in the management of heart failure patients. The National Project of Prevention and Treatment of Cardiovascular Diseases—POLKARD. Cardiol. J. 2012, 19, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Ferrick, A.M.; Raj, S.R.; Deneke, T.; Kojodjojo, P.; Lopez-Cabanillas, N.; Abe, H.; Boveda, S.; Chew, D.S.; Choi, J.I.; Dagres, N.; et al. 2023 HRS/EHRA/APHRS/LAHRS Expert Consensus Statement on Practical Management of the Remote Device Clinic. Europace 2023, 25, euad123. [Google Scholar] [CrossRef]
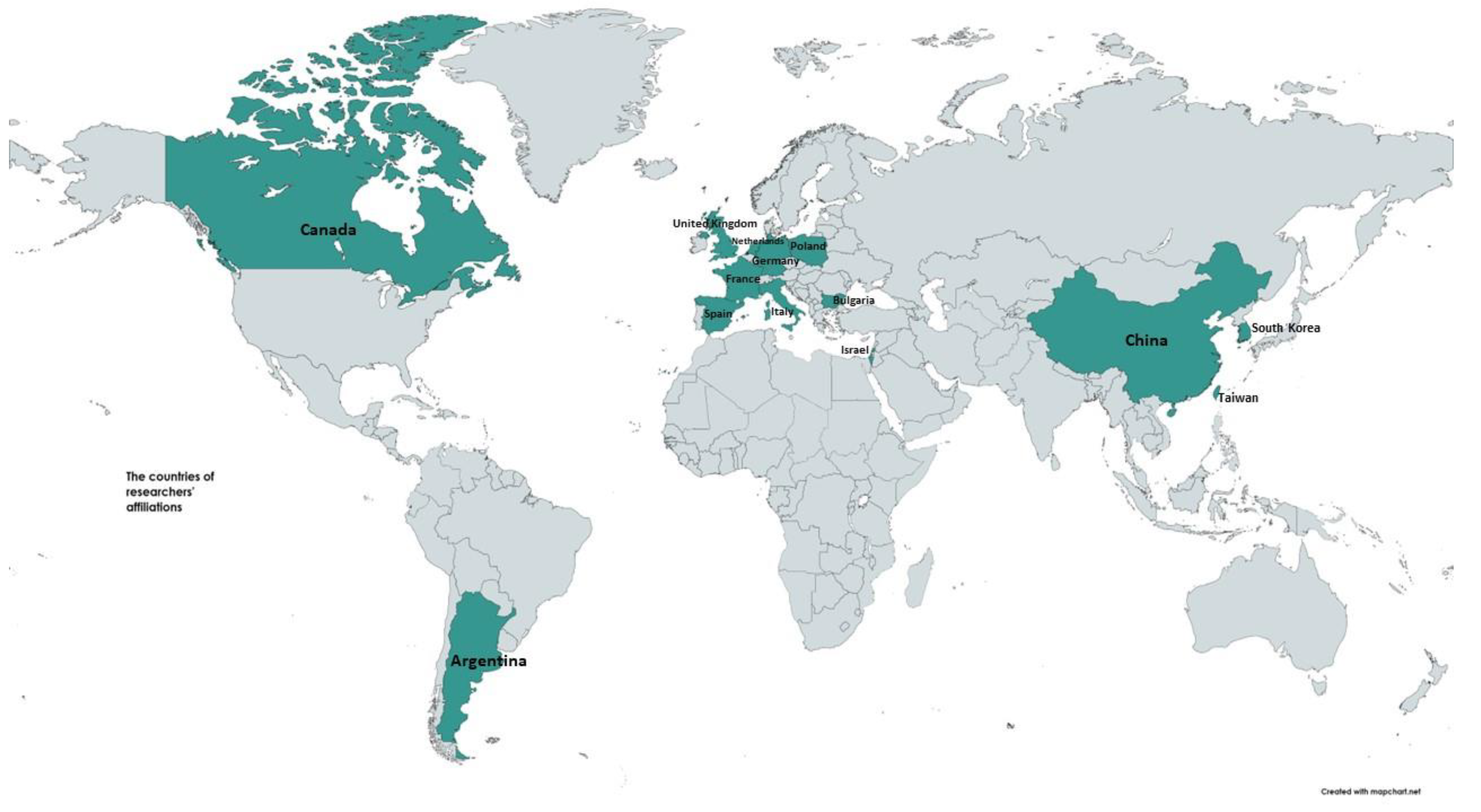
| Contribution Number | Reference | Type of Publication | Number of Authors/Affiliations | Locations of Authors’ Affiliations |
|---|---|---|---|---|
| 1 | Bijak, P.; et al. Fever-Induced Brugada Sign: Clue for Clinical Management with Non-Negligible Risk of Sudden Cardiac Death. J. Clin. Med. 2023, 12. | Editorial | 6/7 | Poland, Bulgaria, Israel, Italy, Germany |
| 2 | Bun, S.-S.; et al. Prevalence and Clinical Characteristics of Patients with Torsades de Pointes Complicating Acquired Atrioventricular Block. J. Clin. Med. 2023, 12, 1067. | Article | 7/1 | France |
| 3 | Lisicka, M.; et al. Heart Rate Variability Impairment Is Associated with Right Ventricular Overload and Early Mortality Risk in Patients with Acute Pulmonary Embolism. J. Clin. Med. 2023, 12, 753. | Article | 6/2 | Poland |
| 4 | Buś, S.; et al. Statistical and Diagnostic Properties of pRRx Parameters in Atrial Fibrillation Detection. J. Clin. Med. 2022, 11, 5702. | Article | 3/2 | Poland |
| 5 | Buś, S.; et al. Using Minimum Redundancy Maximum Relevance Algorithm to Select Minimal Sets of Heart Rate Variability Parameters for Atrial Fibrillation Detection. J. Clin. Med. 2022, 11, 4004. | Article | 3/2 | Poland |
| 6 | Giovanardi, P.; et al. Combined Effects of Age and Comorbidities on Electrocardiographic Parameters in a Large Non-Selected Population. J. Clin. Med. 2022, 11, 3737. | Article | 6/7 | Italy |
| 7 | Matusik, P.S.; et al. Clinical Data, Chest Radiograph and Electrocardiography in the Screening for Left Ventricular Hypertrophy: The CAR2E2 Score. J. Clin. Med. 2022, 11, 3585. | Article | 5/5 | Poland |
| 8 | Tymińska, A.; et al. Fifteen-Year Differences in Indications for Cardiac Resynchronization Therapy in Inter-national Guidelines—Insights from the Heart Failure Registries of the European Society of Cardiology. J. Clin. Med. 2022, 11, 3236. | Article | 11/5 | Poland, Spain, Italy, France |
| 9 | Li, G.-Y.; et al. Sinus Node Dysfunction after Successful Atrial Flutter Ablation during Follow-Up: Clinical Characteristics and Predictors. J. Clin. Med. 2022, 11, 3212. | Article | 16/3 | Taiwan |
| 10 | Okólska, M.; et al. Prevalence of Arrhythmia in Adults after Fontan Operation. J. Clin. Med. 2022, 11, 1968. | Article | 9/7 | Poland |
| 11 | Kowalik, R.; et al. In-Hospital and One-Year Outcomes of Patients after Early and Late Resuscitated Cardiac Arrest Complicating Acute Myocardial Infarction—Data from a Nationwide Database. J. Clin. Med. 2022, 11, 609. | Article | 10/4 | Poland |
| 12 | Karkowski, G.; et al. Contact Force-Sensing versus Standard Catheters in Non-Fluoroscopic Radiofrequency Catheter Ablation of Idiopathic Outflow Tract Ventricular Arrhythmias. J. Clin. Med. 2022, 11, 593. | Article | 7/5 | Poland |
| 13 | Bun, S.-S.; et al. Prevalence and Clinical Characteristics of Patients with Pause-Dependent Atrioventricular Block. J. Clin. Med. 2022, 11, 449. | Article | 9/2 | France |
| 14 | Ozierański, K.; et al. Sex Differences in Incidence, Clinical Characteristics and Outcomes in Children and Young Adults Hospitalized for Clinically Suspected Myocarditis in the Last Ten Years—Data from the MYO-PL Nationwide Database. J. Clin. Med. 2021, 10, 5502. | Article | 8/3 | Poland |
| 15 | Tsai, C.-F.; et al. Long-Term Prognosis of Febrile Individuals with Right Precordial Coved-Type ST-Segment Elevation Brugada Pattern: A 10-Year Prospective Follow-Up Study. J. Clin. Med. 2021, 10, 4997. | Article | 4/3 | Taiwan |
| 16 | Ozierański, K.; et al. Occurrence, Trends, Management and Outcomes of Patients Hospitalized with Clinically Suspected Myocarditis—Ten-Year Perspectives from the MYO-PL Nationwide Database. J. Clin. Med. 2021, 10, 4672. | Article | 7/2 | Poland |
| 17 | Okólska, M.; et al. Heart Rate Variability and Its Associations with Organ Complications in Adults after Fontan Operation. J. Clin. Med. 2021, 10, 4492. | Article | 7/5 | Poland |
| 18 | Wałek, P.; et al. Echocardiographic Evaluation of Atrial Remodelling for the Prognosis of Maintaining Sinus Rhythm after Electrical Cardioversion in Patients with Atrial Fibrillation. J. Clin. Med. 2023, 12, 5158. | Review | 4/3 | Poland |
| 19 | Aziz, H.M.; et al. Pathogenesis and Management of Brugada Syndrome: Recent Advances and Protocol for Umbrella Reviews of Meta-Analyses in Major Arrhythmic Events Risk Stratification. J. Clin. Med. 2022, 11, 1912. | Review | 8/11 | Poland, Argentina, Korea, China, the United Kingdom |
| 20 | He, M.; et al. Caveolin-3 and Arrhythmias: Insights into the Molecular Mechanisms. J. Clin. Med. 2022, 11, 1595. | Review | 5/1 | China |
| 21 | Ahmed, M.; et al. Rhythm vs. Rate Control in Patients with Postoperative Atrial Fibrillation after Cardiac Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 4534. | Systematic review | 15/4 | Canada |
| 22 | Oliva, A.; et al. Structural Heart Alterations in Brugada Syndrome: Is it Really a Channelopathy? A Systematic Review. J. Clin. Med. 2022, 11, 4406. | Systematic review | 21/11 | Spain, Italy, The Netherlands |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Król, R.; Karnaś, M.; Ziobro, M.; Bednarek, J.; Kollias, G.; Sohns, C.; Matusik, P.T. New Frontiers in Electrocardiography, Cardiac Arrhythmias, and Arrhythmogenic Disorders. J. Clin. Med. 2024, 13, 2047. https://doi.org/10.3390/jcm13072047
Król R, Karnaś M, Ziobro M, Bednarek J, Kollias G, Sohns C, Matusik PT. New Frontiers in Electrocardiography, Cardiac Arrhythmias, and Arrhythmogenic Disorders. Journal of Clinical Medicine. 2024; 13(7):2047. https://doi.org/10.3390/jcm13072047
Chicago/Turabian StyleKról, Rafał, Michał Karnaś, Michał Ziobro, Jacek Bednarek, Georgios Kollias, Christian Sohns, and Paweł T. Matusik. 2024. "New Frontiers in Electrocardiography, Cardiac Arrhythmias, and Arrhythmogenic Disorders" Journal of Clinical Medicine 13, no. 7: 2047. https://doi.org/10.3390/jcm13072047
APA StyleKról, R., Karnaś, M., Ziobro, M., Bednarek, J., Kollias, G., Sohns, C., & Matusik, P. T. (2024). New Frontiers in Electrocardiography, Cardiac Arrhythmias, and Arrhythmogenic Disorders. Journal of Clinical Medicine, 13(7), 2047. https://doi.org/10.3390/jcm13072047





