Landmark Evolutions in Time and Indication for Cardiac Resynchronization Therapy: Results from a Multicenter Retrospective Registry
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Retrospective Registries
2.3. Arrangement by Time Periods and Indications
2.4. Endpoints
2.5. Statistical Analysis
3. Results
3.1. Demographics
3.2. Endpoint Analysis
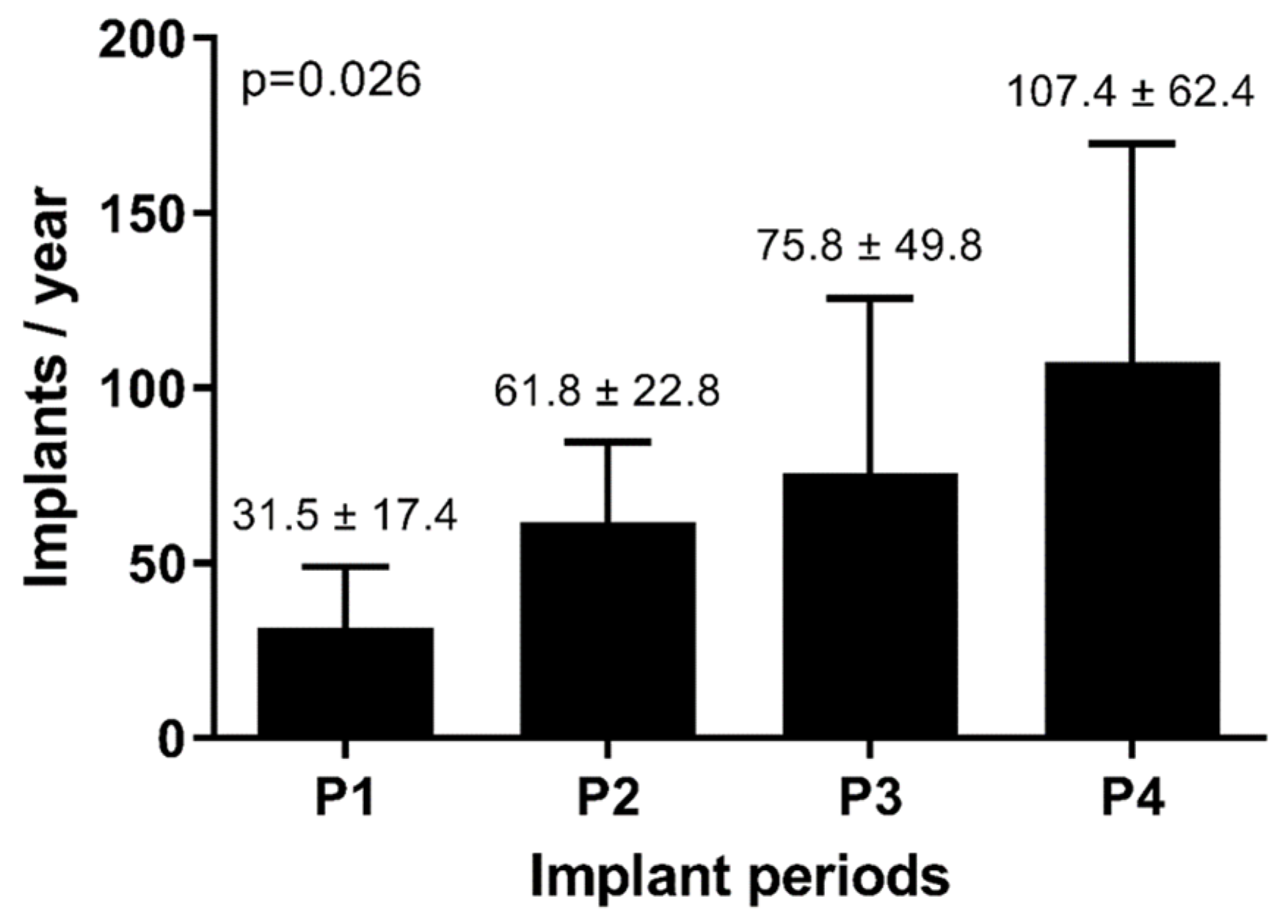
3.3. Evolution in Time
3.4. Endpoint Prediction over Time
3.5. Endpoint Prediction According to Rhythm and QRS Morphology
4. Discussion
4.1. Evolution over Time
4.2. Implant Indication
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Glikson, M.; Nielsen, J.C.; Kronborg, M.B.; Michowitz, Y.; Auricchio, A.; Barbash, I.M.; Barrabés, J.A.; Boriani, G.; Braunschweig, F.; Brignole, M.; et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur. Heart J. 2021, 42, 3427–3520. (In English) [Google Scholar] [CrossRef] [PubMed]
- Ballantyne, B.A.; Chew, D.S.; Vandenberk, B. Paradigm Shifts in Cardiac Pacing: Where Have We Been and What Lies Ahead? J. Clin. Med. 2023, 12, 2938. (In English) [Google Scholar] [CrossRef] [PubMed]
- Leyva, F.; Nisam, S.; Auricchio, A. 20 years of cardiac resynchronization therapy. J. Am. Coll. Cardiol. 2014, 64, 1047–1058. (In English) [Google Scholar] [CrossRef] [PubMed]
- Bristow, M.R.; Feldman, A.M.; Saxon, L.A. Heart failure management using implantable devices for ventricular resynchronization: Comparison of Medical Therapy, Pacing, and Defibrillation in Chronic Heart Failure (COMPANION) trial. COMPANION Steering Committee and COMPANION Clinical Investigators. J. Card. Fail. 2000, 6, 276–285. (In English) [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.G.; Daubert, J.-C.; Erdmann, E.; Freemantle, N.; Gras, D.; Kappenberger, L.; Tavazzi, L.; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 2005, 352, 1539–1549. (In English) [Google Scholar] [CrossRef] [PubMed]
- Tang, A.S.; Wells, G.A.; Talajic, M.; Arnold, M.O.; Sheldon, R.; Connolly, S.; Hohnloser, S.H.; Nichol, G.; Birnie, D.H.; Sapp, J.L.; et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N. Engl. J. Med. 2010, 363, 2385–2395. [Google Scholar] [CrossRef]
- Linde, C.; Abraham, W.T.; Gold, M.R.; Sutton, M.S.J.; Ghio, S.; Daubert, C.; REVERSE (REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction) Study Group. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and previous heart failure symptoms. J. Am. Coll. Cardiol. 2008, 52, 1834–1843. (In English) [Google Scholar] [CrossRef] [PubMed]
- Moss, A.J.; Hall, W.J.; Cannom, D.S.; Klein, H.; Brown, M.W.; Daubert, J.P.; Estes, N.A.M., III; Foster, E.; Greenberg, H.; Higgins, S.L.; et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 2009, 361, 1329–1338. (In English) [Google Scholar] [CrossRef] [PubMed]
- Trenson, S.; Voros, G.; Martens, P.; Ingelaere, S.; Betschart, P.; Voigt, J.; Dupont, M.; Breitenstein, A.; Steffel, J.; Willems, R.; et al. Long-term outcome after upgrade to cardiac resynchronization therapy: A propensity score-matched analysis. Eur. J. Heart Fail. 2023. (In English) [Google Scholar] [CrossRef]
- Brignole, M.; Auricchio, A.; Baron-Esquivias, G.; Bordachar, P.; Boriani, G.; Breithardt, O.-A.; Cleland, J.G.F.; Deharo, J.-C.; Delgado, V.; Elliott, P.M.; et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur. Heart J. 2013, 34, 2281–2329. (In English) [Google Scholar] [CrossRef]
- Behon, A.; Merkel, E.D.; Schwertner, W.R.; Kuthi, L.K.; Veres, B.; Masszi, R.; Kovács, A.; Lakatos, B.K.; Zima, E.; Gellér, L.; et al. Long-term outcome of cardiac resynchronization therapy patients in the elderly. Geroscience 2023, 45, 2289–2301. (In English) [Google Scholar] [CrossRef]
- Rijal, S.; Wolfe, J.; Rattan, R.; Durrani, A.; Althouse, A.D.; Marroquin, O.C.; Jain, S.; Mulukutla, S.; Saba, S. Lead related complications in quadripolar versus bipolar left ventricular leads. Indian Pacing Electrophysiol. J. 2017, 17, 3–7. (In English) [Google Scholar] [CrossRef]
- Boriani, G.; Connors, S.; Kalarus, Z.; Lemke, B.; Mullens, W.; Asensi, J.O.; Raatikainen, P.; Gazzola, C.; Farazi, T.G.; Leclercq, C. Cardiac Resynchronization Therapy with a Quadripolar Electrode Lead Decreases Complications at 6 Months: Results of the MORE-CRT Randomized Trial. JACC Clin. Electrophysiol. 2016, 2, 212–220. (In English) [Google Scholar] [CrossRef]
- Robertson, C.; Duffey, O.; Tang, P.; Fairhurst, N.; Monteiro, C.; Green, P.; Grogono, J.; Davies, M.; Lewis, A.; Wijesurendra, R.; et al. An active fixation quadripolar left ventricular lead for cardiac resynchronization therapy with reduced postoperative complication rates. J. Cardiovasc. Electrophysiol. 2022, 33, 458–463. (In English) [Google Scholar] [CrossRef]
- Pauwelyn, M.; Ingelaere, S.; Hoffmann, R.; Vijgen, J.; Mairesse, G.H.; Blankoff, I.; Vandekerckhove, Y.; Waroux, J.-B.I.P.d.; Vandenberk, B.; Willems, R. Implantable cardiac defibrillators in octogenarians. J. Geriatr. Cardiol. 2023, 20, 23–31. (In English) [Google Scholar] [CrossRef]
- Sapp, J.L.; Sivakumaran, S.; Redpath, C.J.; Khan, H.; Parkash, R.; Exner, D.V.; Healey, J.S.; Thibault, B.; Sterns, L.D.; Lam, N.H.N.; et al. Long-Term Outcomes of Resynchronization-Defibrillation for Heart Failure. N. Engl. J. Med. 2024, 390, 212–220. [Google Scholar] [CrossRef]
- Darden, D.; Peterson, P.N.; Xin, X.; Munir, M.B.; Minges, K.E.; Goldenberg, I.; Poole, J.E.; Feld, G.K.; Birgersdotter-Green, U.; Curtis, J.P.; et al. Temporal trends and long-term outcomes among recipients of cardiac resynchronization therapy with defibrillator in the United States, 2011-2015: Insights from the National Cardiovascular Data Registry. Heart Rhythm O2 2022, 3, 405–414. (In English) [Google Scholar] [CrossRef]
- Leyva, F.; Zegard, A.; Patel, P.; Stegemann, B.; Marshall, H.; Ludman, P.; de Bono, J.; Boriani, G.; Qiu, T. Improved prognosis after cardiac resynchronization therapy over a decade. Europace 2023, 25, euad141. (In English) [Google Scholar] [CrossRef]
- Mcmurray, J.J.V.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014, 371, 993–1004. (In English) [Google Scholar] [CrossRef]
- Birnie, D.H.; Ha, A.; Higginson, L.; Sidhu, K.; Green, M.; Philippon, F.; Thibault, B.; Wells, G.; Tang, A. Impact of QRS morphology and duration on outcomes after cardiac resynchronization therapy: Results from the Resynchronization-Defibrillation for Ambulatory Heart Failure Trial (RAFT). Circ. Heart Fail. 2013, 6, 1190–1198. (In English) [Google Scholar] [CrossRef]
- Zareba, W.; Klein, H.; Cygankiewicz, I.; Hall, W.J.; McNitt, S.; Brown, M.; Cannom, D.; Daubert, J.P.; Eldar, M.; Gold, M.R.; et al. Effectiveness of Cardiac Resynchronization Therapy by QRS Morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation 2011, 123, 1061–1072. (In English) [Google Scholar] [CrossRef]
- Sipahi, I.; Chou, J.C.; Hyden, M.; Rowland, D.Y.; Simon, D.I.; Fang, J.C. Effect of QRS morphology on clinical event reduction with cardiac resynchronization therapy: Meta-analysis of randomized controlled trials. Am. Heart. J. 2012, 163, 260–267.e3. (In English) [Google Scholar] [CrossRef]
- Cunnington, C.; Kwok, C.S.; Satchithananda, D.K.; Patwala, A.; Khan, M.A.; Zaidi, A.; Ahmed, F.Z.; Mamas, M.A. Cardiac resynchronisation therapy is not associated with a reduction in mortality or heart failure hospitalisation in patients with non-left bundle branch block QRS morphology: Meta-analysis of randomised controlled trials. Heart 2015, 101, 1456–1462. (In English) [Google Scholar] [CrossRef]
- Sipahi, I.; Carrigan, T.P.; Rowland, D.Y.; Stambler, B.S.; Fang, J.C. Impact of QRS duration on clinical event reduction with cardiac resynchronization therapy: Meta-analysis of randomized controlled trials. Arch. Intern. Med. 2011, 171, 1454–1462. (In English) [Google Scholar] [CrossRef]
- Cleland, J.G.; Abraham, W.T.; Linde, C.; Gold, M.R.; Young, J.B.; Daubert, J.C.; Sherfesee, L.; Wells, G.A.; Tang, A.S. An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur. Heart J. 2013, 34, 3547–3556. (In English) [Google Scholar] [CrossRef]
- Bilchick, K.C.; Kamath, S.; DiMarco, J.P.; Stukenborg, G.J. Bundle-branch block morphology and other predictors of outcome after cardiac resynchronization therapy in Medicare patients. Circulation 2010, 122, 2022–2030. (In English) [Google Scholar] [CrossRef]
- Adelstein, E.C.; Saba, S. Usefulness of baseline electrocardiographic QRS complex pattern to predict response to cardiac resynchronization. Am. J. Cardiol. 2009, 103, 238–242. (In English) [Google Scholar] [CrossRef]
- Rickard, J.; Kumbhani, D.J.; Gorodeski, E.Z.; Baranowski, B.; Wazni, O.; Martin, D.O.; Grimm, R.; Wilkoff, B.L. Cardiac resynchronization therapy in non-left bundle branch block morphologies. Pacing Clin. Electrophysiol. 2010, 33, 590–595. (In English) [Google Scholar] [CrossRef]
- Friedman, D.J.; Al-Khatib, S.M.; Dalgaard, F.; Fudim, M.; Abraham, W.T.; Cleland, J.G.; Curtis, A.B.; Gold, M.R.; Kutyifa, V.; Linde, C.; et al. Cardiac Resynchronization Therapy Improves Outcomes in Patients with Intraventricular Conduction Delay But Not Right Bundle Branch Block: A Patient-Level Meta-Analysis of Randomized Controlled Trials. Circulation 2023, 147, 812–823. (In English) [Google Scholar] [CrossRef]
- Ruschitzka, F.; Abraham, W.T.; Singh, J.P.; Bax, J.J.; Borer, J.S.; Brugada, J.; Dickstein, K.; Ford, I.; Gorcsan, J., III; Gras, D. Cardiac-resynchronization therapy in heart failure with a narrow QRS complex. N. Engl. J. Med. 2013, 369, 1395–1405. (In English) [Google Scholar] [CrossRef]
- Curtis, A.B.; Worley, S.J.; Adamson, P.B.; Chung, E.S.; Niazi, I.; Sherfesee, L.; Shinn, T.; Sutton, M.S.J. Biventricular pacing for atrioventricular block and systolic dysfunction. N. Engl. J. Med. 2013, 368, 1585–1593. [Google Scholar] [CrossRef]
- Caputo, M.L.; van Stipdonk, A.; Illner, A.; D’Ambrosio, G.; Regoli, F.; Conte, G.; Moccetti, T.; Klersy, C.; Prinzen, F.W.; Vernooy, K.; et al. The definition of left bundle branch block influences the response to cardiac resynchronization therapy. Int. J. Cardiol. 2018, 269, 165–169. (In English) [Google Scholar] [CrossRef]


| Variable | All Patients | Period 1 | Period 2 | Period 3 | Period 4 | p-Value |
|---|---|---|---|---|---|---|
| N | 2275 (100%) | 429 (18.9%) | 692 (30.4%) | 661 (29.1%) | 493 (21.7%) | |
| Age implant (y) | 70.3 (61.8–76.8) | 67.1 (58.8–73.4) | 69.5 (62.3–76.4) | 72.7 (64.7–78.6) | 71.1 (62.8–78.1) | <0.001 |
| Female | 596 (26.4%) | 97 (22.6%) | 194 (28.1%) | 192 (29.2%) | 113 (23.3%) | 0.026 |
| ICD | 1452 (63.9%) | 312 (72.9%) | 437 (63.2%) | 387 (58.6%) | 316 (64.4%) | <0.001 |
| Upgrade | 605 (26.6%) | 114 (26.6%) | 174 (25.1%) | 160 (24.2%) | 157 (32.0%) | 0.019 |
| Epicardial | 136 (6.0%) | 37 (8.6%) | 45 (6.5%) | 32 (4.9%) | 22 (4.5%) | 0.028 |
| ICMP | 962 (42.8%) | 211 (49.4%) | 303 (43.9%) | 255 (38.9%) | 193 (40.6%) | 0.005 |
| LVEF (%) | 27.0 (21.0–34.0) | 25.0 (20.0–30.0) | 28.0 (22.9–35.0) | 28.0 (22.0–35.0) | 29.0 (22.0–34.3) | <0.001 |
| LVEF ≤ 35% | 1890 (84.9%) | 386 (90.8%) | 578 (84.3%) | 536 (83.0%) | 390 (83.0%) | 0.002 |
| NYHA | ||||||
| I | 86 (3.9%) | 11 (2.6%) | 28 (4.1%) | 22 (3.4%) | 25 (5.4%) | <0.001 |
| II | 695 (31.3%) | 76 (17.8%) | 231 (33.5%) | 216 (33.5%) | 172 (37.1%) | |
| III | 1350 (60.7%) | 308 (72.3%) | 402 (58.4%) | 392 (60.9%) | 248 (53.5%) | |
| IV | 92 (4.1%) | 31 (7.3%) | 28 (4.1%) | 14 (2.2%) | 19 (4.1%) | |
| eGFR (mL/min) | 57.8 (41.2–74.7) | 56.0 (40.9–71.8) | 59.8 (41.3–76.2) | 59.9 (41.4–75.5) | 54.3 (40.2–72.5) | 0.065 |
| CKD 1-2 | 1043 (47.1%) | 186 (43.6%) | 334 (49.6%) | 317 (49.8%) | 206 (42.9%) | 0.178 |
| CKD 3a | 489 (22.1%) | 104 (24.4%) | 141 (21.0%) | 128 (20.1%) | 116 (24.2%) | |
| CKD 3b | 401 (18.1%) | 86 (20.1%) | 121 (18.0%) | 106 (16.6%) | 88 (18.3%) | |
| CKD 4-5 | 284 (12.8%) | 51 (11.9%) | 77 (11.4%) | 86 (13.5%) | 70 (14.6%) | |
| QRS duration (ms) | 158 (138–176) | 162 (138–182) | 160 (140–178) | 156 (136–172) | 158 (140–174) | 0.003 |
| ≤130 ms | 420 (18.9%) | 76 (18.1%) | 130 (18.9%) | 131 (20.3%) | 83 (17.5%) | 0.204 |
| 130–150 ms | 487 (21.9%) | 79 (18.9%) | 140 (20.4%) | 154 (23.9%) | 114 (24.0%) | |
| >150 ms | 1319 (59.3%) | 264 (63.0%) | 417 (60.7%) | 360 (55.8%) | 278 (58.5%) | |
| Ventricular conduction | ||||||
| Normal | 175 (7.8%) | 28 (6.7%) | 55 (8.0%) | 53 (8.2%) | 39 (8.2%) | <0.001 |
| RBBB | 198 (8.9%) | 27 (6.4%) | 63 (9.2%) | 71 (10.9%) | 37 (7.8%) | |
| LBBB | 1493 (66.8%) | 285 (67.7%) | 472 (68.6%) | 459 (70.7%) | 277 (58.2%) | |
| Unspecific | 193 (8.6%) | 33 (7.8%) | 47 (6.8%) | 35 (5.4%) | 78 (16.4%) | |
| Paced | 175 (7.8%) | 48 (11.4%) | 51 (7.4%) | 31 (4.8%) | 45 (9.5%) | |
| Rhythm | ||||||
| Sinus | 1680 (75.3%) | 319 (75.4%) | 514 (74.7%) | 514 (79.7%) | 333 (70.0%) | <0.001 |
| AF | 391 (17.5%) | 62 (14.7%) | 127 (18.5%) | 108 (16.7%) | 94 (19.8%) | |
| Atrial pacing | 161 (7.2%) | 42 (9.9%) | 47 (6.8%) | 23 (3.6%) | 49 (10.3%) | |
| ACE/ARB/ARNI | 1945 (86.2%) | 393 (91.6%) | 606 (88.0%) | 571 (87.0%) | 375 (77.6%) | <0.001 |
| BB | 1919 (85.0%) | 366 (85.3%) | 596 (86.5%) | 549 (83.7%) | 408 (84.5%) | 0.523 |
| MRA | 1368 (60.6%) | 245 (57.1%) | 434 (63.1%) | 397 (60.5%) | 292 (60.5%) | 0.265 |
| Loop diuretic | 1419 (63.2%) | 328 (78.1%) | 441 (64.0%) | 348 (53.3%) | 302 (62.7%) | <0.001 |
| Amiodarone | 514 (22.8%) | 120 (28.0%) | 144 (21.0%) | 142 (21.7%) | 108 (22.4%) | 0.041 |
| Hypertension | 1535 (68.0%) | 239 (55.7%) | 447 (64.7%) | 522 (79.7%) | 327 (67.7%) | <0.001 |
| Dyslipidemia | 1451 (64.5%) | 266 (62.2%) | 390 (56.7%) | 467 (71.5%) | 328 (68.1%) | <0.001 |
| History of stroke | 229 (10.2%) | 49 (11.5%) | 71 (10.3%) | 55 (8.4%) | 54 (11.4%) | 0.287 |
| Diabetes mellitus | 602 (26.6%) | 122 (26.1%) | 174 (25.2%) | 177 (27.0%) | 139 (28.7%) | 0.600 |
| Variable | Hazard Ratio | 95% CI | p-Value |
|---|---|---|---|
| Female | 0.64 | 0.52–0.80 | <0.001 |
| ICD | 0.66 | 0.55–0.79 | <0.001 |
| ICMP | 1.29 | 1.09–1.54 | 0.003 |
| LVEF (/%) | 0.98 | 0.97–0.99 | 0.003 |
| NYHA | |||
| I | reference | ||
| II | 1.80 | 0.86–3.74 | 0.116 |
| III or IV | 2.09 | 1.02–4.30 | 0.045 |
| Renal function | |||
| CKD 1-2 | reference | ||
| CKD 3a | 1.21 | 0.97–1.52 | 0.086 |
| CKD 3b | 1.66 | 1.33–2.07 | <0.001 |
| CKD 4-5 | 2.70 | 2.12–3.45 | <0.001 |
| QRS duration | |||
| ≤130 ms | reference | ||
| 130–150 ms | 0.75 | 0.57–0.97 | 0.030 |
| >150 ms | 0.78 | 0.63–0.97 | 0.027 |
| LBBB | 0.73 | 0.62–0.87 | 0.001 |
| ACE/ARB/ARNI | 0.58 | 0.46–0.73 | <0.001 |
| Diabetes mellitus | 1.21 | 1.02–1.44 | 0.029 |
| Stroke/TIA | 1.26 | 1.01–1.58 | 0.041 |
| Events (n,%) | Incidence Rate (%/y, 95% CI) | Cumulative Event Rate (%) | Cox Regression | ||||
|---|---|---|---|---|---|---|---|
| 1 y | 3 y | 5 y | Unadjusted | Adjusted | |||
| Mortality/HTX/VAD | 656 (29.2%) | 8.0% (7.4–8.6) | 8.1% | 20.0% | 31.8% | ||
| Period 1 | 260 (60.6%) | 9.9% (8.7–11.1) | 8.7% | 24.5% | 37.6% | reference | reference |
| Period 2 | 208 (30.4%) | 7.0% (6.1–8.0) | 7.5% | 19.4% | 29.3% | 0.73 (0.60–0.88) | 0.93 (0.75–1.14) |
| Period 3 | 105 (16.1%) | 5.9% (4.9–7.2) | 6.1% | 13.8% | 25.4% | 0.64 (0.50–0.81) | 0.87 (0.67–1.13) |
| Period 4 | 83 (17.2%) | 9.9% (8.0–12.3) | 11.0% | 23.8% | NA | 1.05 (0.80–1.38) | 1.02 (0.76–1.37) |
| Variable | SR + LBBB | SR + Non-LBBB | AF + LBBB | AF + Non-LBBB | QRS < 130 ms | p-Value |
|---|---|---|---|---|---|---|
| N | 986 | 170 | 149 | 49 | 310 | |
| Age implant (y) | 69.3 (60.9–75.8) | 68.4 (59.7–75.3) | 74.0 (67.4–80.2) | 72.8 (66.5–80.0) | 67.7 (59.6–75.0) | <0.001 |
| Female | 334 (33.7%) | 24 (14.1%) | 26 (17.3%) | 5 (10.2%) | 65 (20.8%) | <0.001 |
| ICD | 694 (70.1%) | 132 (77.7%) | 77 (51.3%) | 32 (65.3%) | 241 (77.2%) | <0.001 |
| Upgrade | 147 (14.9%) | 58 (34.1%) | 47 (31.3%) | 15 (30.6%) | 50 (16.0%) | <0001 |
| Epicardial | 47 (4.8%) | 9 (5.3%) | 10 (6.8%) | 1 (2.0%) | 12 (3.9%) | 0.604 |
| ICMP | 364 (36.8%) | 99 (58.6%) | 73 (48.7%) | 24 (49.0%) | 157 (50.7%) | <0.001 |
| LVEF (%) | 25.0 (20.0–30.0) | 25.0 (20.0–30.0 | 25.0 (20.0–30.0 | 29.0 (25.0–30.0) | 25.0 (20.0–30.0 | 0.309 |
| NYHA | ||||||
| I | 35 (3.6%) | 9 (5.4%) | 5 (3.4%) | 0 (0.0%) | 9 (2.9%) | 0.214 |
| II | 293 (29.8%) | 52 (51.1%) | 32 (21.5%) | 13 (27.7%) | 91 (29.6%) | |
| III | 621 (63.1%) | 98 (58.7%) | 100 (67.1%) | 33 (77.2%) | 191 (62.0%) | |
| IV | 36 (3.7%) | 8 (4.8%) | 12 (8.1%) | 1 (2.1%) | 17 (5.5%) | |
| eGFR (mL/min) | 60.6 (43.0–77.3) | 55.0 (40.6–70.7) | 48.7 (32.9–61.9) | 47.2 (35.8–60.4) | 59.6 (41.6–74.2) | <0.001 |
| CKD 1-2 | 500 (51.3%) | 72 (42.9%) | 44 (29.5%) | 13 (27.7%) | 151 (49.4%) | <0.001 |
| CKD 3a | 201 (20.6%) | 43 (25.6%) | 40 (26.9%) | 12 (25.5%) | 68 (22.2%) | |
| CKD 3b | 176 (18.1%) | 31 (18.5%) | 32 (21.5%) | 16 (34.0%) | 37 (12.1%) | |
| CKD 4-5 | 97 (10.0%) | 22 (13.1%) | 33 (22.2%) | 6 (12.8%) | 50 (16.3%) | |
| ACE/ARB/ARNI | 886 (89.5%) | 138 (81.2%) | 122 (81.3%) | 43 (87.8%) | 277 (88.8%) | 0.003 |
| BB | 865 (87.4%) | 143 (84.1%) | 130 (86.7%) | 40 (81.6%) | 276 (88.5%) | 0.521 |
| MRA | 651 (65.8%) | 105 (61.8%) | 98 (65.3%) | 23 (46.9%) | 208 (66.7%) | 0.075 |
| Loop diuretics | 594 (60.4%) | 123 (72.4%) | 113 (75.3%) | 35 (71.4%) | 217 (70.0%) | <0.001 |
| Amiodarone | 205 (20.7%) | 55 (32.4%) | 41 (27.3%) | 11 (22.5%) | 69 (22.2%) | 0.011 |
| Hypertension | 635 (64.2%) | 118 (69.4%) | 120 (80.0%) | 33 (67.4%) | 211 (67.6%) | 0.004 |
| Dyslipidemia | 613 (62.1%) | 121 (71.2%) | 105 (70.0%) | 28 (57.1%) | 198 (63.5%) | 0.069 |
| Stroke | 102 (10.4%) | 14 (8.2%) | 23 (15.4%) | 4 (8.2%) | 19 (6.1%) | 0.025 |
| Diabetes mellitus | 254 (25.7%) | 57 (33.5%) | 35 (23.3%) | 15 (30.6%) | 91 (29.2%) | 0.155 |
| Rhythm | Morphology | Events (n,%) | Incidence Rate (%/y, 95% CI) | Cumulative Event Rate (%) | Cox Regression | ||||
|---|---|---|---|---|---|---|---|---|---|
| 1 y | 3 y | 5 y | Unadjusted | Adjusted | |||||
| SR | LBBB | 986 | 246 (25.0%) | 6.1% (5.3–6.9) | 4.4% | 16.0% | 25.6% | reference | reference |
| SR | Non-LBBB | 170 | 62 (36.5%) | 11.8% (9.2–15.2) | 13.5% | 25.7% | 43.3% | 1.96 (1.49–2.60) | 1.51 (1.12–2.03) |
| AF | LBBB | 149 | 56 (37.6%) | 10.7% (8.3–13.9) | 13.0% | 27.2% | 40.3% | 1.80 (1.34–2.41) | 1.33 (0.97–1.80) |
| AF | Non-LBBB | 49 | 23 (46.9%) | 16.4% (10.8–25.0) | 24.1% | 40.6% | 47.1% | 2.76 (1.78–4.28) | 2.08 (1.30–3.33) |
| QRS < 130 ms | 310 | 100 (32.3%) | 9.9% (8.1–12.1) | 9.6% | 21.2% | 39.8% | 1.68 (1.33–2.13) | 1.64 (1.29–2.09) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bijnens, J.; Trenson, S.; Voros, G.; Martens, P.; Ingelaere, S.; Betschart, P.; Voigt, J.-U.; Dupont, M.; Breitenstein, A.; Steffel, J.; et al. Landmark Evolutions in Time and Indication for Cardiac Resynchronization Therapy: Results from a Multicenter Retrospective Registry. J. Clin. Med. 2024, 13, 1903. https://doi.org/10.3390/jcm13071903
Bijnens J, Trenson S, Voros G, Martens P, Ingelaere S, Betschart P, Voigt J-U, Dupont M, Breitenstein A, Steffel J, et al. Landmark Evolutions in Time and Indication for Cardiac Resynchronization Therapy: Results from a Multicenter Retrospective Registry. Journal of Clinical Medicine. 2024; 13(7):1903. https://doi.org/10.3390/jcm13071903
Chicago/Turabian StyleBijnens, Jeroen, Sander Trenson, Gabor Voros, Pieter Martens, Sebastian Ingelaere, Pascal Betschart, Jens-Uwe Voigt, Matthias Dupont, Alexander Breitenstein, Jan Steffel, and et al. 2024. "Landmark Evolutions in Time and Indication for Cardiac Resynchronization Therapy: Results from a Multicenter Retrospective Registry" Journal of Clinical Medicine 13, no. 7: 1903. https://doi.org/10.3390/jcm13071903
APA StyleBijnens, J., Trenson, S., Voros, G., Martens, P., Ingelaere, S., Betschart, P., Voigt, J.-U., Dupont, M., Breitenstein, A., Steffel, J., Willems, R., Ruschitzka, F., Mullens, W., Winnik, S., & Vandenberk, B. (2024). Landmark Evolutions in Time and Indication for Cardiac Resynchronization Therapy: Results from a Multicenter Retrospective Registry. Journal of Clinical Medicine, 13(7), 1903. https://doi.org/10.3390/jcm13071903






