SHBG Levels Do Not Correlate with Insulin Levels in PCOS with Appropriate Fasting Insulin Sensitivity
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Collected Data
2.3. Statistical Analysis
3. Results
3.1. Basic Parameters and Insulin Sensitivity Parameters
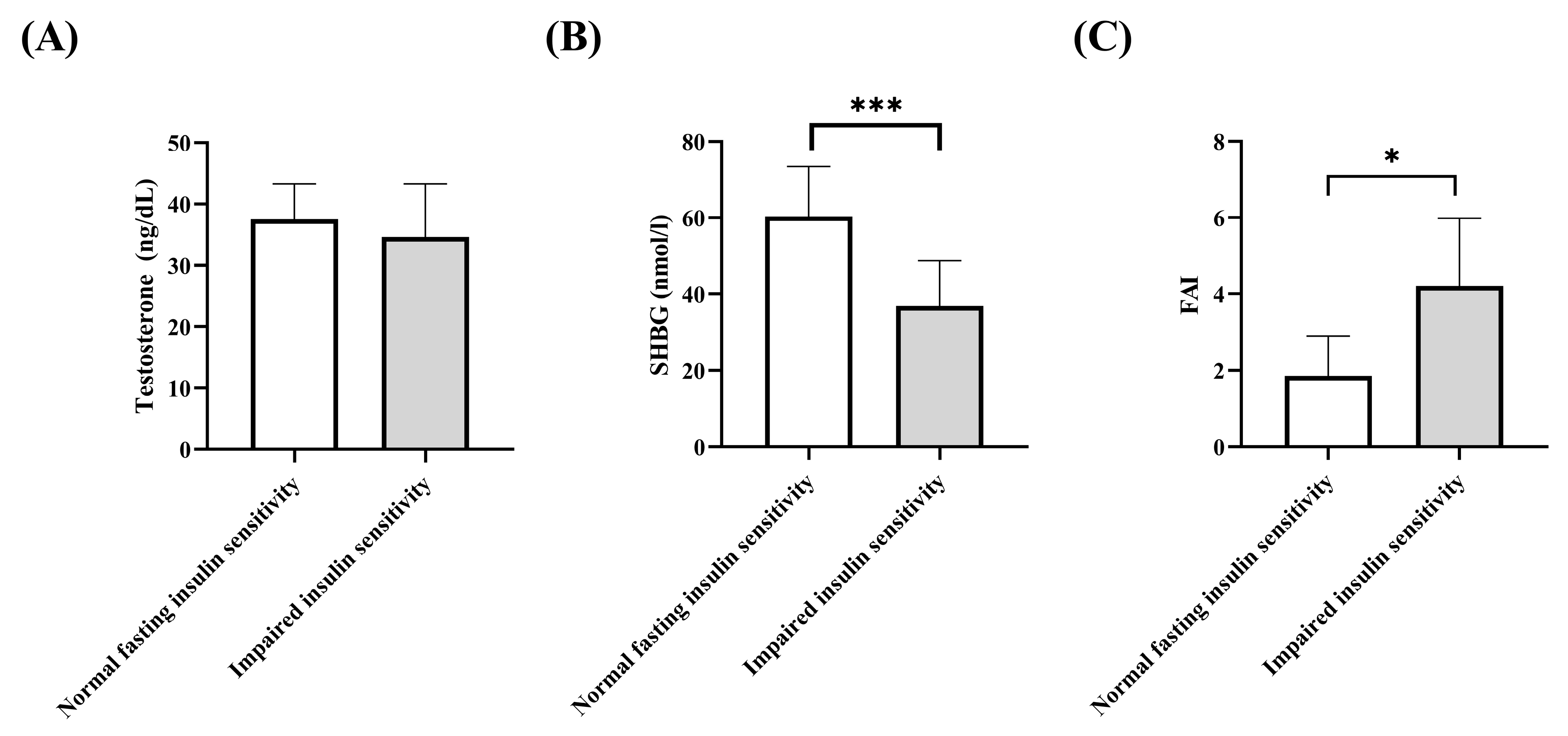
3.2. Testosterone, Free Androgen Index, SHBG
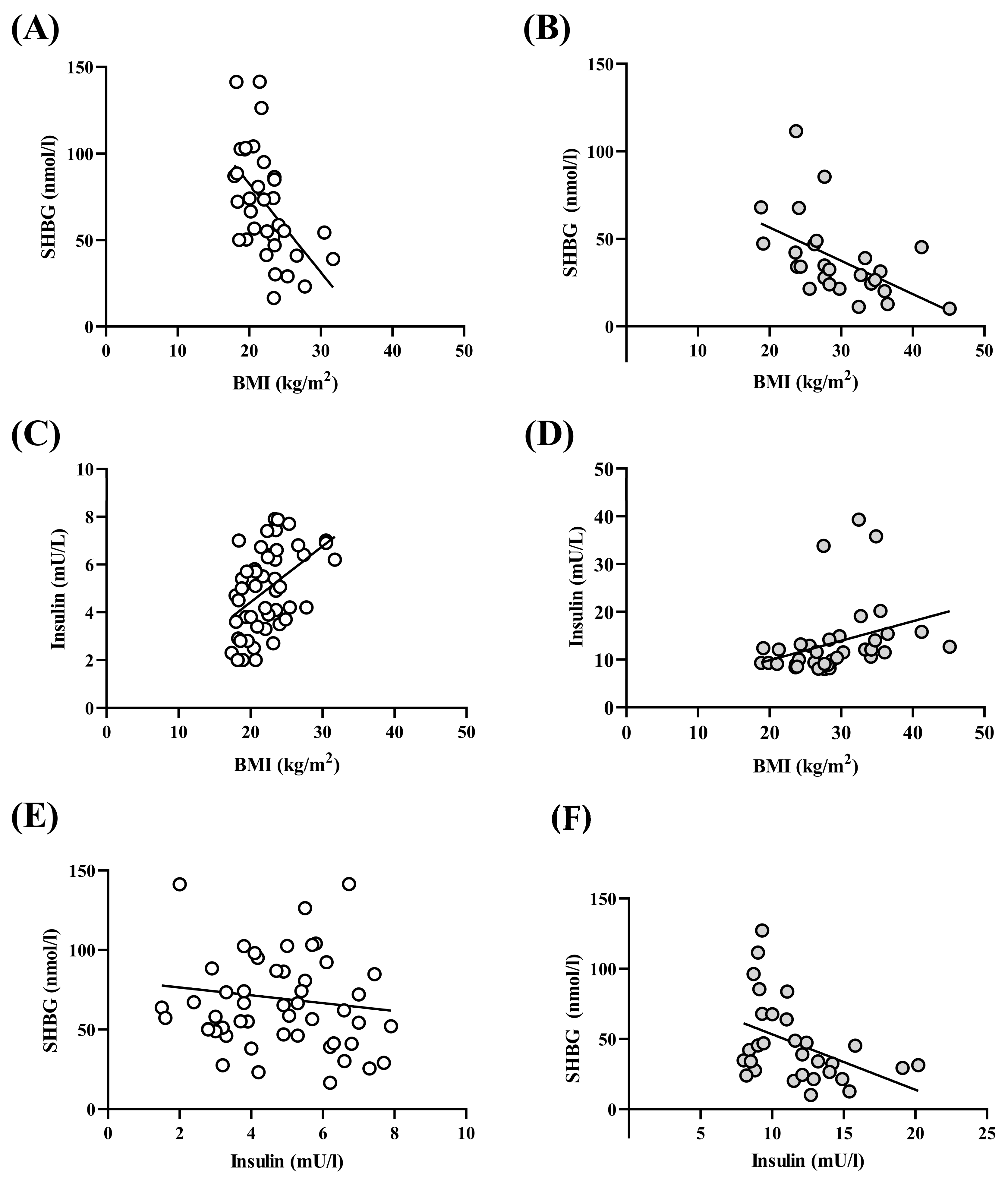
3.3. BMI–Insulin–SHBG–Correlation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deswal, R.; Narwal, V.; Dang, A.; Pundir, C.S. The Prevalence of Polycystic Ovary Syndrome: A Brief Systematic Review. J. Hum. Reprod. Sci. 2020, 13, 261–271. [Google Scholar] [CrossRef]
- Elting, M.W.; Korsen, T.J.; Bezemer, P.D.; Schoemaker, J. Prevalence of diabetes mellitus, hypertension and cardiac complaints in a follow-up study of a Dutch PCOS population. Hum. Reprod. 2001, 16, 556–560. [Google Scholar] [CrossRef]
- Bhathena, R.K. Insulin resistance and the long-term consequences of polycystic ovary syndrome. J. Obstet Gynaecol. 2011, 31, 105–110. [Google Scholar] [CrossRef]
- Nestler, J.E.; Jakubowicz, D.J. Lean women with polycystic ovary syndrome respond to insulin reduction with decreases in ovarian P450c17 alpha activity and serum androgens. J. Clin. Endocrinol. Metab. 1997, 82, 4075–4079. [Google Scholar] [CrossRef]
- Diamanti-Kandarakis, E.; Dunaif, A. Insulin resistance and the polycystic ovary syndrome revisited: An update on mechanisms and implications. Endocr. Rev. 2012, 33, 981–1030. [Google Scholar] [CrossRef]
- Geffner, M.E.; Golde, D.W. Selective insulin action on skin, ovary, and heart in insulin-resistant states. Diabetes Care 1988, 11, 500–505. [Google Scholar] [CrossRef]
- Dunaif, A. Insulin resistance and the polycystic ovary syndrome: Mechanism and implications for pathogenesis. Endocr. Rev. 1997, 18, 774–800. [Google Scholar] [CrossRef]
- Boden, G.; Ruiz, J.; Urbain, J.L.; Chen, X. Evidence for a circadian rhythm of insulin secretion. Am. J. Physiol. 1996, 271, E246–E252. [Google Scholar] [CrossRef]
- Altuntas, Y.; Bilir, M.; Ucak, S.; Gundogdu, S. Reactive hypoglycemia in lean young women with PCOS and correlations with insulin sensitivity and with beta cell function. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005, 119, 198–205. [Google Scholar] [CrossRef]
- DeFronzo, R.A.; Tobin, J.D.; Andres, R. Glucose clamp technique: A method for quantifying insulin secretion and resistance. Am. J. Physiol. 1979, 237, E214–E223. [Google Scholar] [CrossRef] [PubMed]
- Stepto, N.K.; Cassar, S.; Joham, A.E.; Hutchison, S.K.; Harrison, C.L.; Goldstein, R.F.; Teede, H.J. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum. Reprod. 2013, 28, 777–784. [Google Scholar] [CrossRef]
- Saxena, P.; Prakash, A.; Nigam, A. Efficacy of 2-hour post glucose insulin levels in predicting insulin resistance in polycystic ovarian syndrome with infertility. J. Hum. Reprod. Sci. 2011, 4, 20–22. [Google Scholar] [CrossRef]
- Bartoli, E.; Fra, G.P.; Carnevale Schianca, G.P. The oral glucose tolerance test (OGTT) revisited. Eur. J. Intern. Med. 2011, 22, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Bogdanet, D.; O’Shea, P.; Lyons, C.; Shafat, A.; Dunne, F. The Oral Glucose Tolerance Test-Is It Time for a Change?-A Literature Review with an Emphasis on Pregnancy. J. Clin. Med. 2020, 9, 3451. [Google Scholar] [CrossRef]
- Winters, S.J.; Gogineni, J.; Karegar, M.; Scoggins, C.; Wunderlich, C.A.; Baumgartner, R.; Ghooray, D.T. Sex hormone-binding globulin gene expression and insulin resistance. J. Clin. Endocrinol. Metab. 2014, 99, E2780–E2788. [Google Scholar] [CrossRef]
- Plymate, S.R.; Matej, L.A.; Jones, R.E.; Friedl, K.E. Inhibition of sex hormone-binding globulin production in the human hepatoma (Hep G2) cell line by insulin and prolactin. J. Clin. Endocrinol. Metab. 1988, 67, 460–464. [Google Scholar] [CrossRef]
- Deswal, R.; Yadav, A.; Dang, A.S. Sex hormone binding globulin—An important biomarker for predicting PCOS risk: A systematic review and meta-analysis. Syst. Biol. Reprod. Med. 2018, 64, 12–24. [Google Scholar] [CrossRef]
- Chen, F.; Liao, Y.; Chen, M.; Yin, H.; Chen, G.; Huang, Q.; Chen, L.; Yang, X.; Zhang, W.; Wang, P.; et al. Evaluation of the Efficacy of Sex Hormone-Binding Globulin in Insulin Resistance Assessment Based on HOMA-IR in Patients with PCOS. Reprod. Sci. 2021, 28, 2504–2513. [Google Scholar] [CrossRef] [PubMed]
- Okubo, M.; Tokui, M.; Egusa, G.; Yamakido, M. Association of sex hormone-binding globulin and insulin resistance among Japanese-American subjects. Diabetes Res. Clin. Pract. 2000, 47, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Biernacka-Bartnik, A.; Kocełak, P.; Owczarek, A.J.; Choręza, P.S.; Markuszewski, L.; Madej, P.; Puzianowska-Kuźnicka, M.; Chudek, J.; Olszanecka-Glinianowicz, M. The cut-off value for HOMA-IR discriminating the insulin resistance based on the SHBG level in women with polycystic ovary syndrome. Front. Med. 2023, 10, 1100547. [Google Scholar] [CrossRef]
- Dahan, M.H.; Goldstein, J. Serum sex hormone-binding globulin levels show too much variability to be used effectively as a screening marker for insulin resistance in women with polycystic ovary syndrome. Fertil. Steril. 2006, 86, 934–941. [Google Scholar] [CrossRef]
- Cai, W.Y.; Luo, X.; Song, J.; Ji, D.; Zhu, J.; Duan, C.; Wu, W.; Wu, X.K.; Xu, J. Effect of Hyperinsulinemia and Insulin Resistance on Endocrine, Metabolic, and Reproductive Outcomes in Non-PCOS Women Undergoing Assisted Reproduction: A Retrospective Cohort Study. Front. Med. 2021, 8, 736320. [Google Scholar] [CrossRef]
- Selva, D.M.; Hammond, G.L. Thyroid hormones act indirectly to increase sex hormone-binding globulin production by liver via hepatocyte nuclear factor-4alpha. J. Mol. Endocrinol. 2009, 43, 19–27. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Ali, A.T.; Al-Ani, O.; Al-Ani, F.; Guidozzi, F. Polycystic ovary syndrome and metabolic disorders: A review of the literature. Afr. J. Reprod. Health 2022, 26, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Ludvik, B.; Nolan, J.J.; Baloga, J.; Sacks, D.; Olefsky, J. Effect of obesity on insulin resistance in normal subjects and patients with NIDDM. Diabetes 1995, 44, 1121–1125. [Google Scholar] [CrossRef] [PubMed]
- Sethi, N.; Puri, S.; Malhotra, A. A comparative study of insulin levels in lean versus obese polycystic ovarian syndrome patients. Int. J. Reprod. Contracept. Obstet. Gynecol. 2023, 12, 893–897. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, Y.; Fang, X.; Kwak-Kim, J.; Wu, L. Insulin Resistance Adversely Affect IVF Outcomes in Lean Women Without PCOS. Front. Endocrinol. 2021, 12, 734638. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.J.; Nakamura, R.M.; Judd, H.L.; Kaplan, S.A. Insulin resistance in nonobese patients with polycystic ovarian disease. J. Clin. Endocrinol. Metab. 1983, 57, 356–359. [Google Scholar] [CrossRef]
- Xing, C.; Zhang, J.; Zhao, H.; He, B. Effect of Sex Hormone-Binding Globulin on Polycystic Ovary Syndrome: Mechanisms, Manifestations, Genetics, and Treatment. Int. J. Womens Health 2022, 14, 91–105. [Google Scholar] [CrossRef]
- Guastella, E.; Longo, R.A.; Carmina, E. Clinical and endocrine characteristics of the main polycystic ovary syndrome phenotypes. Fertil. Steril. 2010, 94, 2197–2201. [Google Scholar] [CrossRef]
- Ladrón de Guevara, A.; Fux-Otta, C.; Crisosto, N.; Szafryk de Mereshian, P.; Echiburú, B.; Iraci, G.; Perez-Bravo, F.; Sir-Petermann, T. Metabolic profile of the different phenotypes of polycystic ovary syndrome in two Latin American populations. Fertil. Steril. 2014, 101, 1732–1739.e2. [Google Scholar] [CrossRef]
- Neubronner, S.A.; Indran, I.R.; Chan, Y.H.; Thu, A.W.P.; Yong, E.L. Effect of body mass index (BMI) on phenotypic features of polycystic ovary syndrome (PCOS) in Singapore women: A prospective cross-sectional study. BMC Womens Health 2021, 21, 135. [Google Scholar] [CrossRef]
- Purwar, A.; Nagpure, S. Insulin Resistance in Polycystic Ovarian Syndrome. Cureus 2022, 14, e30351. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadis, G.; Mitrou, P.; Lambadiari, V.; Maratou, E.; Raptis, S.A. Insulin effects in muscle and adipose tissue. Diabetes Res Clin. Pract. 2011, 93 (Suppl. 1), S52–S59. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Zhang, J.; Zhang, F.; Zhang, S.; Chen, X.; Liang, W.; Xie, Q. Resistance to the Insulin and Elevated Level of Androgen: A Major Cause of Polycystic Ovary Syndrome. Front. Endocrinol. 2021, 12, 741764. [Google Scholar] [CrossRef] [PubMed]
- Franks, S.; Gilling-Smith, C.; Watson, H.; Willis, D. Insulin action in the normal and polycystic ovary. Endocrinol. Metab. Clin. N. Am. 1999, 28, 361–378. [Google Scholar] [CrossRef] [PubMed]
- Poretsky, L.; Cataldo, N.A.; Rosenwaks, Z.; Giudice, L.C. The insulin-related ovarian regulatory system in health and disease. Endocr. Rev. 1999, 20, 535–582. [Google Scholar] [CrossRef]
- Legro, R.S.; Kunselman, A.R.; Dodson, W.C.; Dunaif, A. Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: A prospective, controlled study in 254 affected women. J. Clin. Endocrinol. Metab. 1999, 84, 165–169. [Google Scholar] [CrossRef]
- Norman, R.J.; Masters, L.; Milner, C.R.; Wang, J.X.; Davies, M.J. Relative risk of conversion from normoglycaemia to impaired glucose tolerance or non-insulin dependent diabetes mellitus in polycystic ovarian syndrome. Hum. Reprod. 2001, 16, 1995–1998. [Google Scholar] [CrossRef]
- Wallace, I.R.; McKinley, M.C.; Bell, P.M.; Hunter, S.J. Sex hormone binding globulin and insulin resistance. Clin. Endocrinol. 2013, 78, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Norman, R.J.; Davies, M.J.; Moran, L.J. The effect of obesity on polycystic ovary syndrome: A systematic review and meta-analysis. Obes. Rev. 2013, 14, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Dadachanji, R.; Shaikh, N.; Mukherjee, S. Genetic Variants Associated with Hyperandrogenemia in PCOS Pathophysiology. Genet. Res. Int. 2018, 2018, 7624932. [Google Scholar] [CrossRef]
- Miller, K.K.; Rosner, W.; Lee, H.; Hier, J.; Sesmilo, G.; Schoenfeld, D.; Neubauer, G.; Klibanski, A. Measurement of free testosterone in normal women and women with androgen deficiency: Comparison of methods. J. Clin. Endocrinol. Metab. 2004, 89, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Al Kindi, M.K.; Al Essry, F.S.; Al Essry, F.S.; Mula-Abed, W.A. Validity of serum testosterone, free androgen index, and calculated free testosterone in women with suspected hyperandrogenism. Oman. Med. J. 2012, 27, 471–474. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, A.; Singh, T.A. Comparison of clinical features and health manifestations in lean vs. obese Indian women with polycystic ovarian syndrome. J. Hum. Reprod. Sci. 2009, 2, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Tawfeek, M.A.; Alfadhli, E.M.; Alayoubi, A.M.; El-Beshbishy, H.A.; Habib, F.A. Sex hormone binding globulin as a valuable biochemical marker in predicting gestational diabetes mellitus. BMC Womens Health 2017, 17, 18. [Google Scholar] [CrossRef]
- Misra, S.; Gada, J.; Dhole, C.; Varthakavi, P.; Bhagwat, N. Comparative Study of Insulin Sensitivity and Resistance and Their Correlation with Androgens in Lean and Obese Women with Polycystic Ovary Syndrome. Reprod. Sci. 2023. [Google Scholar] [CrossRef]
- Esser, N.; Utzschneider, K.M.; Kahn, S.E. Early beta cell dysfunction vs insulin hypersecretion as the primary event in the pathogenesis of dysglycaemia. Diabetologia 2020, 63, 2007–2021. [Google Scholar] [CrossRef]
- Dunaif, A.; Finegood, D.T. Beta-cell dysfunction independent of obesity and glucose intolerance in the polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 1996, 81, 942–947. [Google Scholar] [CrossRef]
- Goodarzi, M.O.; Erickson, S.; Port, S.C.; Jennrich, R.I.; Korenman, S.G. beta-Cell function: A key pathological determinant in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2005, 90, 310–315. [Google Scholar] [CrossRef]
- Del Prato, S. Loss of early insulin secretion leads to postprandial hyperglycaemia. Diabetologia 2003, 46 (Suppl. 1), M2–M8. [Google Scholar] [CrossRef]
- Kahn, S.E. Clinical review 135: The importance of beta-cell failure in the development and progression of type 2 diabetes. J. Clin. Endocrinol. Metab. 2001, 86, 4047–4058. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, T.; Boyko, E.J.; Sato, K.K.; McNeely, M.J.; Leonetti, D.L.; Kahn, S.E.; Fujimoto, W.Y. Patterns of insulin concentration during the OGTT predict the risk of type 2 diabetes in Japanese Americans. Diabetes Care 2013, 36, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Ellerbrock, J.; Spaanderman, B.; Drongelen, J.V.; Mulder, E.; Lopes van Balen, V.; Schiffer, V.; Jorissen, L.; Alers, R.J.; Leenen, J.; Ghossein-Doha, C.; et al. Role of Beta Cell Function and Insulin Resistance in the Development of Gestational Diabetes Mellitus. Nutrients 2022, 14, 2444. [Google Scholar] [CrossRef] [PubMed]
| Normal Fasting Insulin Sensitivity Group | Impaired Insulin Sensitivity Group | Statistical Level | |
|---|---|---|---|
| N | 88 | 46 | |
| Age (years) | 35 ± 6 | 36 + 6 | p = 0.73 |
| Body weight (kg) | 62 (59–65) | 80 (74–86) | p < 0.0001 |
| BMI (kg/m2) | 22.0 (20.7–23.4) | 28.1 (26.6–30.3) | p < 0.0001 |
| Fasting insulin (mU/L) | 4.5 (4.0–5.3) | 11.05 (9.4–12.4) | p < 0.0001 |
| Fasting glucose (mg/dL) | 87.1 (84.6–88.2) | 91.8 (86.4–94.7) | p < 0.01 |
| HOMA-IR | 0.96 (0.83–1.15) | 2.38 (2.26–2.89) | p < 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tűű, L.; Nas, K.; Török, M.; Várbíró, S. SHBG Levels Do Not Correlate with Insulin Levels in PCOS with Appropriate Fasting Insulin Sensitivity. J. Clin. Med. 2024, 13, 838. https://doi.org/10.3390/jcm13030838
Tűű L, Nas K, Török M, Várbíró S. SHBG Levels Do Not Correlate with Insulin Levels in PCOS with Appropriate Fasting Insulin Sensitivity. Journal of Clinical Medicine. 2024; 13(3):838. https://doi.org/10.3390/jcm13030838
Chicago/Turabian StyleTűű, László, Katalin Nas, Marianna Török, and Szabolcs Várbíró. 2024. "SHBG Levels Do Not Correlate with Insulin Levels in PCOS with Appropriate Fasting Insulin Sensitivity" Journal of Clinical Medicine 13, no. 3: 838. https://doi.org/10.3390/jcm13030838
APA StyleTűű, L., Nas, K., Török, M., & Várbíró, S. (2024). SHBG Levels Do Not Correlate with Insulin Levels in PCOS with Appropriate Fasting Insulin Sensitivity. Journal of Clinical Medicine, 13(3), 838. https://doi.org/10.3390/jcm13030838







