Characterization of the Increase in Narcolepsy following the 2009 H1N1 Pandemic in Sweden
Abstract
1. Introduction
2. Materials and Methods
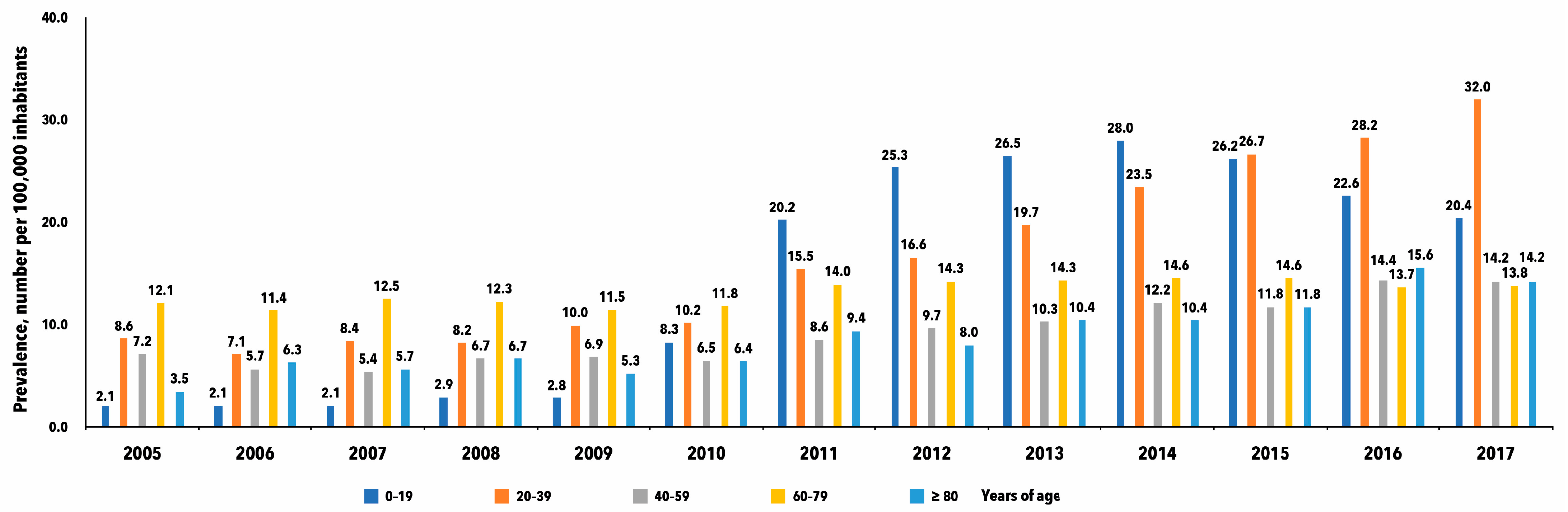
3. Results
4. Discussion
4.1. The National Patient Register (NPR)
4.2. Persisting Increase in the Prevalence of Narcolepsy
4.3. Ad Hoc Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kornum, B.R.; Knudsen, S.; Ollila, H.M.; Pizza, F.; Jennum, P.J.; Dauvilliers, Y.; Overeem, S. Narcolepsy. Nat. Rev. Dis. Primers. 2017, 3, 100. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, C.L.A.; Adamantidis, A.; Burdakov, D.; Han, F.; Gay, S.; Kallweit, U.; Khatami, R.; Koning, F.; Kornum, B.R.; Jan Lammers, G.; et al. Narcolepsy—Clinical spectrum, aetiopathophysiology, diagnosis and treatment. Nat. Rev. Neurol. 2019, 15, 519–539. [Google Scholar] [CrossRef] [PubMed]
- Schiappa, C.; Scarpelli, S.; D’atri, A.; Gorgoni, M.; De Gennaro, L. Narcolepsy and emotional experience: A review of the literature. Behav. Brain Funct. 2018, 14, 19. [Google Scholar] [CrossRef] [PubMed]
- Witt, S.T.; Drissi, N.M.; Tapper, S.; Wretman, A.; Szakács, A.; Hallböök, T.; Landtblom, A.-M.; Karlsson, T.; Lundberg, P.; Engström, M. Evidence for cognitive resource imbalance in adolescents with narcolepsy. Brain Imaging Behav. 2018, 12, 411–424. [Google Scholar] [CrossRef]
- Drissi, N.M.; Szakács, A.; Witt, S.T.; Wretman, A.; Ulander, M.; Ståhlbrandt, H.; Darin, N.; Hallböök, T.; Landtblom, A.-M.; Engström, M. Altered Brain Microstate Dynamics in Adolescents with Narcolepsy. Front. Hum. Neurosci. 2016, 10, 369. [Google Scholar] [CrossRef]
- Gauffin, H.; Fast, T.; Komkova, A.; Berntsson, S.; Boström, I.; Landtblom, A. Narcolepsy treatment in Sweden: An observational study. Acta Neurol. Scand. 2022, 145, 185–192. [Google Scholar] [CrossRef]
- Jennum, P.; Ibsen, R.; Petersen, E.R.; Knudsen, S.; Kjellberg, J. Health, social, and economic consequences of narcolepsy: A controlled national study evaluating the societal effect on patients and their partners. Sleep Med. 2012, 13, 1086–1093. [Google Scholar] [CrossRef]
- Nishino, S.; Ripley, B.; Overeem, S.; Lammers, G.J.; Mignot, E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet 2000, 355, 39–40. [Google Scholar] [CrossRef]
- Thannickal, T.C.; Moore, R.Y.; Nienhuis, R.; Ramanathan, L.; Gulyani, S.; Aldrich, M.; Cornford, M.; Siegel, J.M. Reduced Number of Hypocretin Neurons in Human Narcolepsy. Neuron 2000, 27, 469–474. [Google Scholar] [CrossRef]
- Drissi, N.M.; Warntjes, M.; Wessen, A.; Szakacs, A.; Darin, N.; Hallbook, T.; Landtblom, A.M.; Gauffin, H.; Engström, M. Structural anomaly in the reticular formation in narcolepsy type 1, suggesting lower levels of neuromelanin. Neuroimage Clin. 2019, 23, 101875. [Google Scholar] [CrossRef]
- Partinen, M.; Kornum, B.R.; Plazzi, G.; Jennum, P.; Julkunen, I.; Vaarala, O. Narcolepsy as an autoimmune disease: The role of H1N1 infection and vaccination. Lancet Neurol. 2014, 13, 600–613. [Google Scholar] [CrossRef] [PubMed]
- Longstreth, W., Jr.; Koepsell, T.D.; Ton, T.G.; Hendrickson, A.F.; van Belle, G. The Epidemiology of Narcolepsy. Sleep 2007, 30, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Thorpy, M.J.; Carls, G.; Black, J.; Cisternas, M.; Pasta, D.J.; Bujanover, S.; Hyman, D.; Villa, K.F. The Nexus Narcolepsy Registry: Methodology, study population characteristics, and patterns and predictors of narcolepsy diagnosis. Sleep Med. 2021, 84, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Silber, M.H.; Krahn, L.E.; Olson, E.J.; Pankratz, V.S. The Epidemiology of Narcolepsy in Olmsted County, Minnesota: A Population-Based Study. Sleep 2002, 25, 197–202. [Google Scholar] [CrossRef]
- Hallbook, T.; Szakacs, A.; Bialek, F.; Feltelius, N.; Landtblom, A.M.; Malmgren, K. Narcolepsy-rare disease that has received increased attention. Pandemrix vaccination caused a higher incidence among children and adolescents. Lakartidningen 2014, 111, 1770–1773. [Google Scholar] [PubMed]
- Wijnans, L.; Lecomte, C.; de Vries, C.; Weibel, D.; Sammon, C.; Hviid, A.; Svanström, H.; Mølgaard-Nielsen, D.; Heijbel, H.; Dahlström, L.A.; et al. The incidence of narcolepsy in Europe: Before, during, and after the influenza A(H1N1) pdm09 pandemic and vaccination campaigns. Vaccine 2013, 31, 1246–1254. [Google Scholar] [CrossRef]
- Kawai, M.; O’Hara, R.; Einen, M.; Lin, L.; Mignot, E. Narcolepsy in African Americans. Sleep 2015, 38, 1673–1681. [Google Scholar] [CrossRef]
- Scheer, D.; Schwartz, S.W.; Parr, M.; Zgibor, J.; Sanchez-Anguiano, A.; Rajaram, L. Prevalence and incidence of narcolepsy in a US health care claims database, 2008–2010. Sleep 2019, 42, zsz091. [Google Scholar] [CrossRef]
- Lee, R.U.; Radin, J.M. A population-based epidemiologic study of adult-onset narcolepsy incidence and associated risk factors, 2004–2013. J. Neurol. Sci. 2016, 370, 29–34. [Google Scholar] [CrossRef]
- Wu, H.; Zhuang, J.; Stone, W.S.; Zhang, L.; Zhao, Z.; Wang, Z.; Yang, Y.; Li, X.; Zhao, X.; Zhao, Z. Symptoms and occurrences of narcolepsy: A retrospective study of 162 patients during a 10-year period in Eastern China. Sleep Med. 2014, 15, 607–613. [Google Scholar] [CrossRef]
- Mignot, E.; Thorsby, E. Narcolepsy and the HLA System. N. Engl. J. Med. 2001, 344, 692. [Google Scholar] [CrossRef] [PubMed]
- Juji, T.; Satake, M.; Honda, Y.; Doi, Y. HLA antigens in Japanese patients with narcolepsy. All the patients were DR2 positive. Tissue Antigens 1984, 24, 316–319. [Google Scholar] [CrossRef] [PubMed]
- Mignot, E. Genetic and familial aspects of narcolepsy. Neurology 1998, 50 (Suppl. 1), S16–S22. [Google Scholar] [CrossRef] [PubMed]
- Aran, A.; Lin, L.; Nevsimalova, S.; Plazzi, G.; Hong, S.C.; Weiner, K.; Zeitzer, J.; Mignot, E. Elevated Anti-Streptococcal Antibodies in Patients with Recent Narcolepsy Onset. Sleep 2009, 32, 979–983. [Google Scholar] [CrossRef] [PubMed]
- Picchioni, D.; Hope, C.R.; Harsh, J.R. A Case-Control Study of the Environmental Risk Factors for Narcolepsy. Neuroepidemiology 2007, 29, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Lind, A.; Salami, F.; Landtblom, A.M.; Palm, L.; Lernmark, A.; Adolfsson, J.; Elding Larsson, H. Immunocyte single cell analysis of vaccine-induced narcolepsy. Eur. J. Immunol. 2021, 51, 247–249. [Google Scholar] [CrossRef]
- Hallberg, P.; Smedje, H.; Eriksson, N.; Kohnke, H.; Daniilidou, M.; Öhman, I.; Yue, Q.-Y.; Cavalli, M.; Wadelius, C.; Magnusson, P.K.; et al. Pandemrix-induced narcolepsy is associated with genes related to immunity and neuronal survival. EBioMedicine 2019, 40, 595–604. [Google Scholar] [CrossRef]
- Partinen, M.; Saarenpää-Heikkilä, O.; Ilveskoski, I.; Hublin, C.; Linna, M.; Olsén, P.; Nokelainen, P.; Alén, R.; Wallden, T.; Espo, M.; et al. Increased Incidence and Clinical Picture of Childhood Narcolepsy following the 2009 H1N1 Pandemic Vaccination Campaign in Finland. PLoS ONE 2012, 7, e33723. [Google Scholar] [CrossRef]
- Boström, I.; Berntsson, S.G.; Zheliba, N.; Gauffin, H.; Kristoffersson, A.; Niemelä, V.; Landtblom, A. Narcolepsy as a side effect of swine flu vaccination. J. Neurol. Sci. 2017, 381, 189. [Google Scholar] [CrossRef]
- Boström, I.; Lindberger, O.; Partinen, M.; Landtblom, A.-M. Vaccination against swine flu caused narcolepsy in several European countries. Health Risk Anal. 2020, 3, 180–185. [Google Scholar]
- Sarkanen, T.; Alakuijala, A.; Julkunen, I.; Partinen, M. Narcolepsy Associated with Pandemrix Vaccine. Curr. Neurol. Neurosci. Rep. 2018, 18, 43. [Google Scholar] [CrossRef] [PubMed]
- Szakacs, A.; Darin, N.; Hallbook, T. Increased childhood incidence of narcolepsy in western Sweden after H1N1 influenza vaccination. Neurology 2013, 80, 1315–1321. [Google Scholar] [CrossRef] [PubMed]
- Han, F.; Lin, L.; Warby, S.C.; Faraco, J.; Li, J.; Dong, S.X.; An, P.; Zhao, L.; Wang, L.H.; Li, Q.Y.; et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in china. Ann. Neurol. 2011, 70, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Thebault, S.; Vincent, A.; Gringras, P. Narcolepsy and H1N1 vaccination: A link? Curr. Opin. Pulm. Med. 2013, 19, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Landtblom, A.M.; Engstrom, M. The sleepy teenager—Diagnostic challenges. Front. Neurol. 2014, 5, 140. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xiao, F.; Wang, Y.; Deng, X.; Chen, Z.; Dong, X.; Wang, W.; Li, C.; Xu, Z.; Wu, H.; et al. Changed epidemiology of narcolepsy before, during, and after the 2009 H1N1 pandemic: A nationwide narcolepsy surveillance network study in mainland China, 1990–2017. Sleep 2023, 46, zsac325. [Google Scholar] [CrossRef] [PubMed]
- Masterman, T.; Ligers, A.; Olsson, T.; Andersson, M.; Olerup, O.; Hillert, J. HLA-DR15 is associated with lower age at onset in multiple sclerosis. Ann. Neurol. 2000, 48, 211–219. [Google Scholar] [CrossRef]
- Dunn, S.E.; Gunde, E.; Lee, H. Sex-Based Differences in Multiple Sclerosis (MS): Part II: Rising Incidence of Multiple Sclerosis in Women and the Vulnerability of Men to Progression of this Disease. Curr. Top. Behav. Neurosci. 2015, 26, 57–86. [Google Scholar]
- Alfredsson, L.; Olsson, T. Lifestyle and Environmental Factors in Multiple Sclerosis. Cold Spring Harb. Perspect. Med. 2019, 9, a028944. [Google Scholar] [CrossRef]
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women | |||||||||||||
| Cases (nr.) | 375 | 349 | 361 | 408 | 432 | 487 | 763 | 852 | 949 | 1042 | 1104 | 1136 | 1169 |
| Inhabitants | 4,561,202 | 4,589,734 | 4,619,006 | 4,652,637 | 4,691,668 | 4,725,326 | 4,756,021 | 4,789,988 | 4,830,507 | 4,875,115 | 4,920,051 | 4,981,806 | 5,037,580 |
| Prevalence /100,000 | 8.22 | 7.60 | 7.82 | 8.77 | 9.21 | 10.31 | 16.04 | 17.79 | 19.65 | 21.37 | 22.44 | 22.80 | 23.21 |
| Men | |||||||||||||
| Cases (nr.) | 262 | 225 | 259 | 266 | 271 | 354 | 578 | 664 | 717 | 819 | 818 | 843 | 875 |
| Inhabitants | 4,486,550 | 4,523,523 | 4,563,921 | 4,603,710 | 4,649,014 | 4,690,244 | 4,726,834 | 4,765,905 | 4,814,357 | 4,872,240 | 4,930,966 | 5,013,347 | 5,082,662 |
| Prevalence /100,000 | 5.84 | 4.97 | 5.67 | 5.78 | 5.83 | 7.55 | 12.23 | 13.93 | 14.89 | 16.81 | 16.59 | 16.82 | 17.22 |
| All | |||||||||||||
| Cases (nr) | 637 | 574 | 620 | 674 | 703 | 841 | 1341 | 1516 | 1666 | 1861 | 1922 | 1979 | 2044 |
| Inhabitants | 9,047,752 | 9,113,257 | 9,182,927 | 9,256,347 | 9,340,682 | 9,415,570 | 9,482,855 | 9,555,893 | 9,644,864 | 9,747,355 | 9,851,017 | 9,995,153 | 10,120,242 |
| Prevalence /100,000 | 7.04 | 6.30 | 6.75 | 7.28 | 7.53 | 8.93 | 14.14 | 15.86 | 17.27 | 19.09 | 19.51 | 19.80 | 20.20 |
| Sex ratio Women/Men | 1.4 | 1.5 | 1.4 | 1.5 | 1.6 | 1.4 | 1.3 | 1.3 | 1.3 | 1.3 | 1.4 | 1.4 | 1.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gauffin, H.; Boström, I.; Berntsson, S.G.; Kristoffersson, A.; Fredrikson, M.; Landtblom, A.-M. Characterization of the Increase in Narcolepsy following the 2009 H1N1 Pandemic in Sweden. J. Clin. Med. 2024, 13, 652. https://doi.org/10.3390/jcm13030652
Gauffin H, Boström I, Berntsson SG, Kristoffersson A, Fredrikson M, Landtblom A-M. Characterization of the Increase in Narcolepsy following the 2009 H1N1 Pandemic in Sweden. Journal of Clinical Medicine. 2024; 13(3):652. https://doi.org/10.3390/jcm13030652
Chicago/Turabian StyleGauffin, Helena, Inger Boström, Shala Ghaderi Berntsson, Anna Kristoffersson, Mats Fredrikson, and Anne-Marie Landtblom. 2024. "Characterization of the Increase in Narcolepsy following the 2009 H1N1 Pandemic in Sweden" Journal of Clinical Medicine 13, no. 3: 652. https://doi.org/10.3390/jcm13030652
APA StyleGauffin, H., Boström, I., Berntsson, S. G., Kristoffersson, A., Fredrikson, M., & Landtblom, A.-M. (2024). Characterization of the Increase in Narcolepsy following the 2009 H1N1 Pandemic in Sweden. Journal of Clinical Medicine, 13(3), 652. https://doi.org/10.3390/jcm13030652