Hospitalizations of Patients with Atrial Fibrillation (AF) in Poland: A Nationwide Study Based on over One Million AF Hospitalizations in 2017–2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Methods
2.2. Statistical Analysis
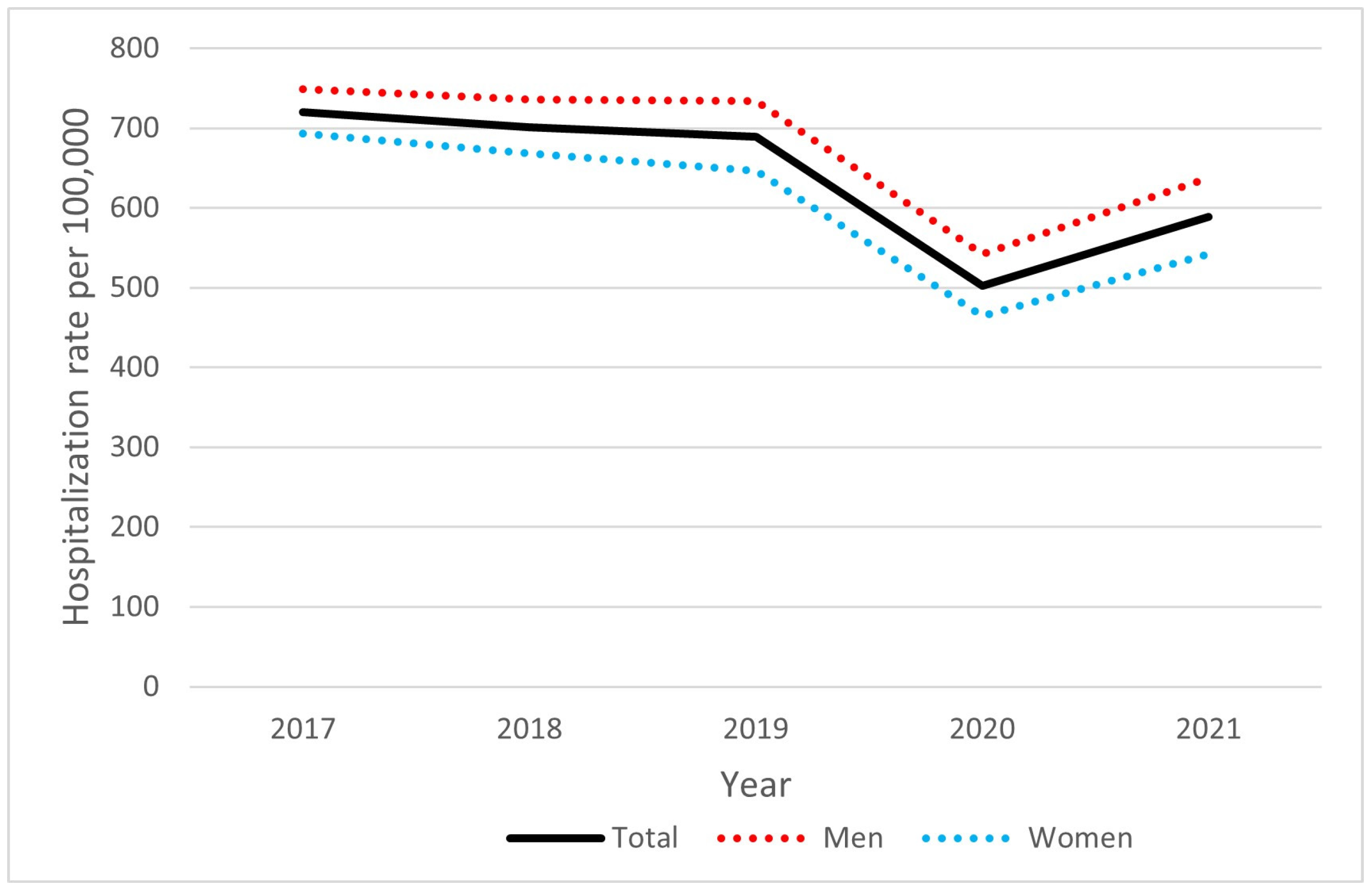
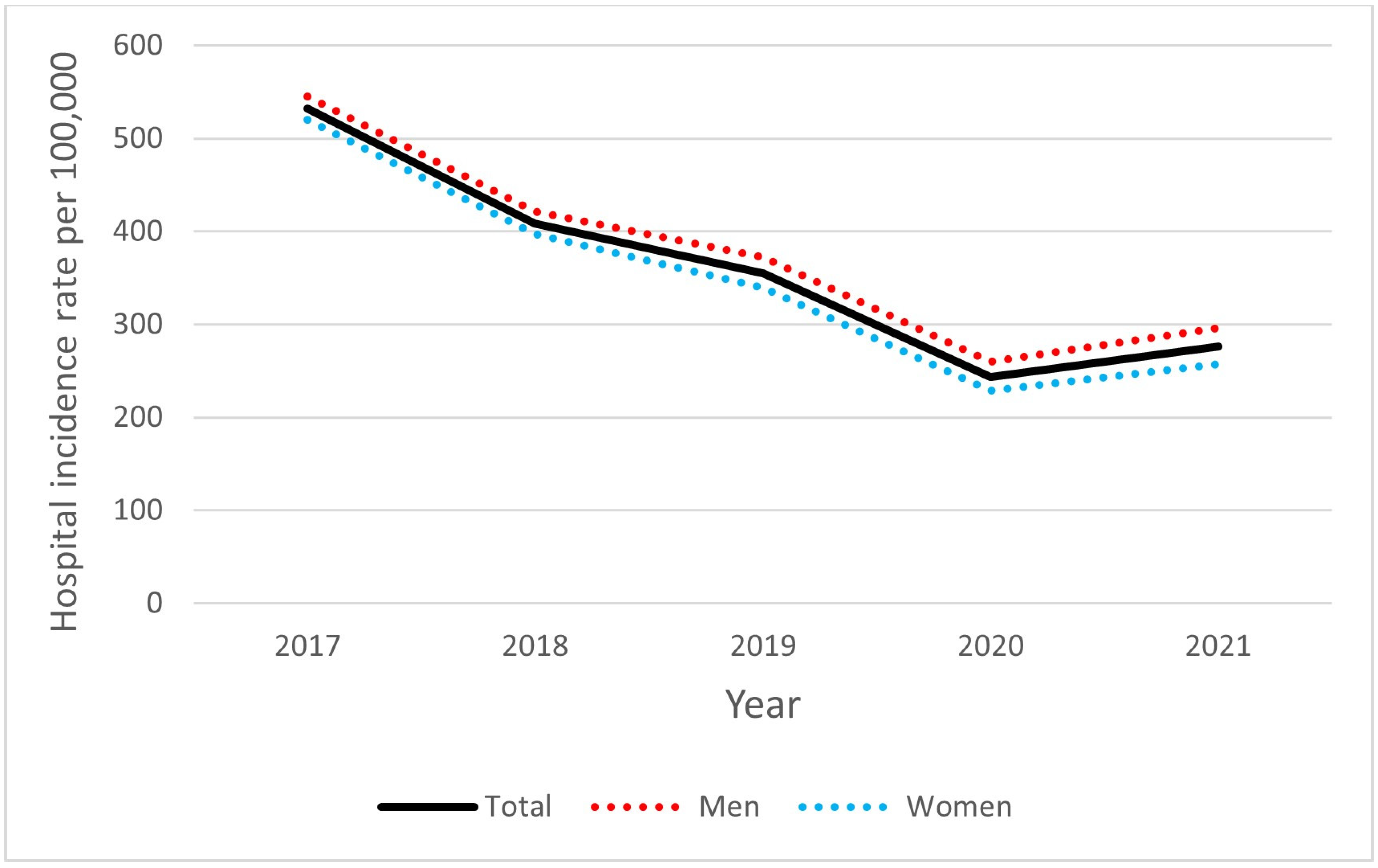
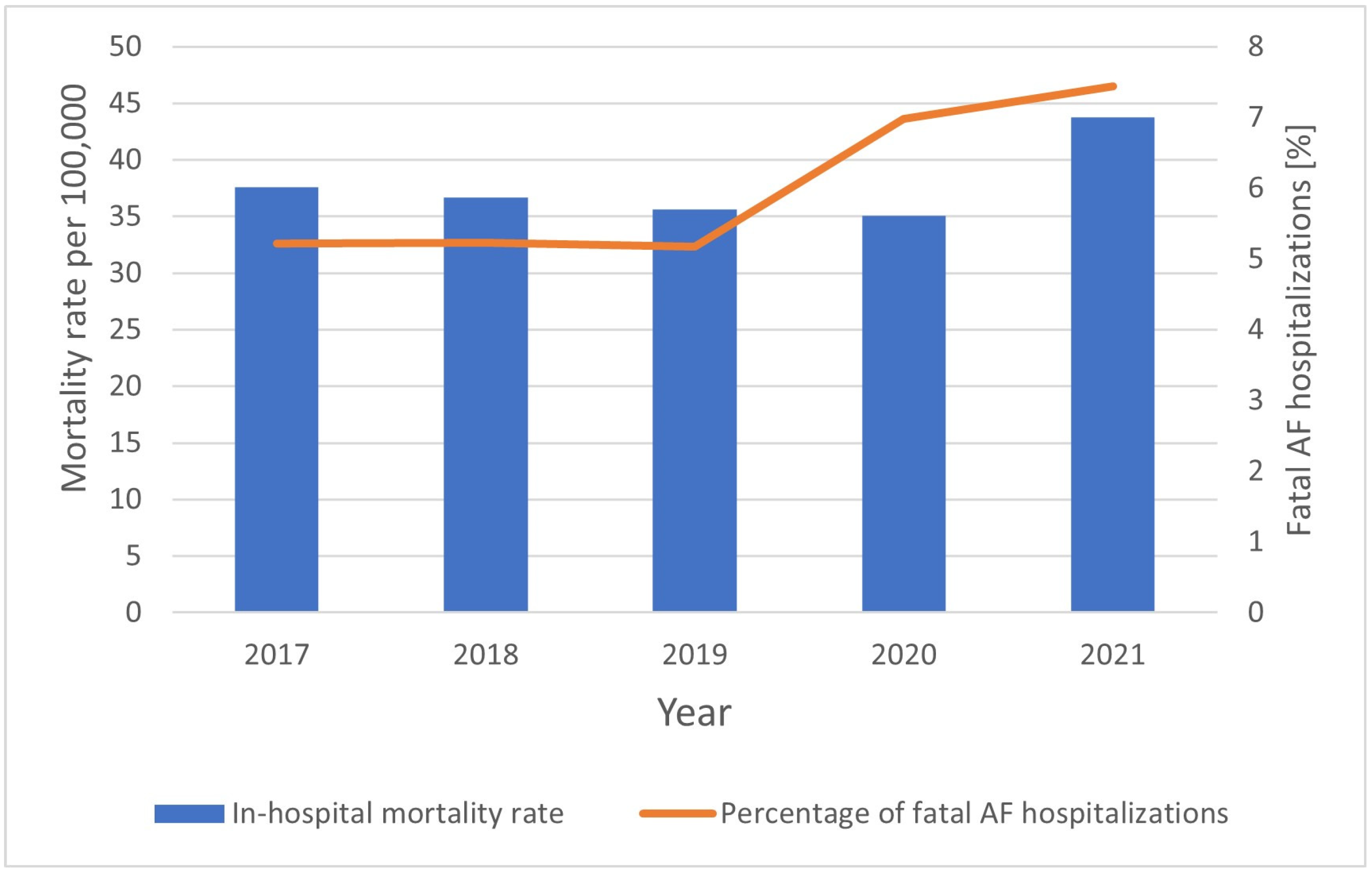
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lippi, G.; Sanchis-Gomar, F.; Cervellin, G. Global Epidemiology of Atrial Fibrillation: An Increasing Epidemic and Public Health Challenge. Int. J. Stroke Off. J. Int. Stroke Soc. 2021, 16, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Rahman, F.; Kwan, G.F.; Benjamin, E.J. Global Epidemiology of Atrial Fibrillation. Nat. Rev. Cardiol. 2014, 11, 639–654. [Google Scholar] [CrossRef] [PubMed]
- Vermond, R.A.; Geelhoed, B.; Verweij, N.; Tieleman, R.G.; Van der Harst, P.; Hillege, H.L.; Van Gilst, W.H.; Van Gelder, I.C.; Rienstra, M. Incidence of Atrial Fibrillation and Relationship With Cardiovascular Events, Heart Failure, and Mortality: A Community-Based Study From the Netherlands. J. Am. Coll. Cardiol. 2015, 66, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Hobbelt, A.H.; Siland, J.E.; Geelhoed, B.; Van Der Harst, P.; Hillege, H.L.; Van Gelder, I.C.; Rienstra, M. Clinical, Biomarker, and Genetic Predictors of Specific Types of Atrial Fibrillation in a Community-Based Cohort: Data of the PREVEND Study. Europace 2017, 19, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Dewland, T.A.; Olgin, J.E.; Vittinghoff, E.; Marcus, G.M. Incident Atrial Fibrillation among Asians, Hispanics, Blacks, and Whites. Circulation 2013, 128, 2470–2477. [Google Scholar] [CrossRef]
- Boriani, G.; Savelieva, I.; Dan, G.-A.; Deharo, J.C.; Ferro, C.; Israel, C.W.; Lane, D.A.; La Manna, G.; Morton, J.; Mitjans, A.M.; et al. Chronic Kidney Disease in Patients with Cardiac Rhythm Disturbances or Implantable Electrical Devices: Clinical Significance and Implications for Decision Making-a Position Paper of the European Heart Rhythm Association Endorsed by the Heart Rhythm Society and the Asia Pacific Heart Rhythm Society. EP Europace 2015, 17, 1169–1196. [Google Scholar] [CrossRef]
- Aune, D.; Feng, T.; Schlesinger, S.; Janszky, I.; Norat, T.; Riboli, E. Diabetes Mellitus, Blood Glucose and the Risk of Atrial Fibrillation: A Systematic Review and Meta-Analysis of Cohort Studies. J. Diabetes Complicat. 2018, 32, 501–511. [Google Scholar] [CrossRef]
- Nalliah, C.J.; Sanders, P.; Kalman, J.M. The Impact of Diet and Lifestyle on Atrial Fibrillation. Curr. Cardiol. Rep. 2018, 20, 137. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Coca, A.; Kahan, T.; Boriani, G.; Manolis, A.S.; Olsen, M.H.; Oto, A.; Potpara, T.S.; Steffel, J.; Marín, F.; et al. Hypertension and Cardiac Arrhythmias: A Consensus Document from the European Heart Rhythm Association (EHRA) and ESC Council on Hypertension, Endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE). EP Europace 2017, 19, 891–911. [Google Scholar] [CrossRef]
- Mou, L.; Norby, F.L.; Chen, L.Y.; O’Neal, W.T.; Lewis, T.T.; Loehr, L.R.; Soliman, E.Z.; Alonso, A. Lifetime Risk of Atrial Fibrillation by Race and Socioeconomic Status: ARIC Study (Atherosclerosis Risk in Communities). Circ. Arrhythm. Electrophysiol. 2018, 11, e006350. [Google Scholar] [CrossRef]
- Boriani, G.; Laroche, C.; Diemberger, I.; Fantecchi, E.; Popescu, M.I.; Rasmussen, L.H.; Sinagra, G.; Petrescu, L.; Tavazzi, L.; Maggioni, A.P.; et al. Asymptomatic Atrial Fibrillation: Clinical Correlates, Management, and Outcomes in the EORP-AF Pilot General Registry. Am. J. Med. 2015, 128, 509–518.e2. [Google Scholar] [CrossRef] [PubMed]
- Siontis, K.C.; Gersh, B.J.; Killian, J.M.; Noseworthy, P.A.; McCabe, P.; Weston, S.A.; Roger, V.L.; Chamberlain, A.M. Typical, Atypical, and Asymptomatic Presentations of New-Onset Atrial Fibrillation in the Community: Characteristics and Prognostic Implications. Heart Rhythm 2016, 13, 1418–1424. [Google Scholar] [CrossRef]
- Andrew, N.E.; Thrift, A.G.; Cadilhac, D.A. The Prevalence, Impact and Economic Implications of Atrial Fibrillation in Stroke: What Progress Has Been Made? Neuroepidemiology 2013, 40, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Kotecha, D.; Piccini, J.P. Atrial Fibrillation in Heart Failure: What Should We Do? Eur. Heart J. 2015, 36, 3250–3257. [Google Scholar] [CrossRef] [PubMed]
- Magnussen, C.; Niiranen, T.J.; Ojeda, F.M.; Gianfagna, F.; Blankenberg, S.; Njølstad, I.; Vartiainen, E.; Sans, S.; Pasterkamp, G.; Hughes, M.; et al. Sex Differences and Similarities in Atrial Fibrillation Epidemiology, Risk Factors, and Mortality in Community Cohorts: Results From the BiomarCaRE Consortium (Biomarker for Cardiovascular Risk Assessment in Europe). Circulation 2017, 136, 1588–1597. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.-J.; Wang, B.-B.; Hou, F.-F.; Jiao, Y.; Li, H.-W.; Lv, S.-P.; Li, F.-H. Global Burden of Atrial Fibrillation/Atrial Flutter and Its Attributable Risk Factors from 1990 to 2019. EP Europace 2023, 25, 793–803. [Google Scholar] [CrossRef]
- Schnabel, R.B.; Yin, X.; Gona, P.; Larson, M.G.; Beiser, A.S.; McManus, D.D.; Newton-Cheh, C.; Lubitz, S.A.; Magnani, J.W.; Ellinor, P.T.; et al. 50 Year Trends in Atrial Fibrillation Prevalence, Incidence, Risk Factors, and Mortality in the Framingham Heart Study: A Cohort Study. Lancet 2015, 386, 154–162. [Google Scholar] [CrossRef]
- Wilke, T.; Groth, A.; Mueller, S.; Pfannkuche, M.; Verheyen, F.; Linder, R.; Maywald, U.; Bauersachs, R.; Breithardt, G. Incidence and Prevalence of Atrial Fibrillation: An Analysis Based on 8.3 Million Patients. EP Europace 2013, 15, 486–493. [Google Scholar] [CrossRef]
- Wu, J.; Nadarajah, R.; Nakao, Y.M.; Nakao, K.; Wilkinson, C.; Mamas, M.A.; Camm, A.J.; Gale, C.P. Temporal Trends and Patterns in Atrial Fibrillation Incidence: A Population-Based Study of 3·4 Million Individuals. Lancet Reg. Health Eur. 2022, 17, 100386. [Google Scholar] [CrossRef]
- Krijthe, B.P.; Kunst, A.; Benjamin, E.J.; Lip, G.Y.H.; Franco, O.H.; Hofman, A.; Witteman, J.C.M.; Stricker, B.H.; Heeringa, J. Projections on the Number of Individuals with Atrial Fibrillation in the European Union, from 2000 to 2060. Eur. Heart J. 2013, 34, 2746–2751. [Google Scholar] [CrossRef]
- Di Carlo, A.; Bellino, L.; Consoli, D.; Mori, F.; Zaninelli, A.; Baldereschi, M.; Cattarinussi, A.; D’Alfonso, M.G.; Gradia, C.; Sgherzi, B.; et al. Prevalence of Atrial Fibrillation in the Italian Elderly Population and Projections from 2020 to 2060 for Italy and the European Union: The FAI Project. EP Europace 2019, 21, 1468–1475. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Hylek, E.M.; Phillips, K.A.; Chang, Y.; Henault, L.E.; Selby, J.V.; Singer, D.E. Prevalence of Diagnosed Atrial Fibrillation in Adults: National Implications for Rhythm Management and Stroke Prevention: The AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001, 285, 2370–2375. [Google Scholar] [CrossRef] [PubMed]
- Miyasaka, Y.; Barnes, M.E.; Gersh, B.J.; Cha, S.S.; Bailey, K.R.; Abhayaratna, W.P.; Seward, J.B.; Tsang, T.S.M. Secular Trends in Incidence of Atrial Fibrillation in Olmsted County, Minnesota, 1980 to 2000, and Implications on the Projections for Future Prevalence. Circulation 2006, 114, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Kalarus, Z.; Średniawa, B.; Mitręga, K.; Wierucki, Ł.; Sokal, A.; Lip, G.; Bandosz, P.; Stokwiszewski, J.; Boidol, J.; Zieleniewicz, P.; et al. Prevalence of Atrial Fibrillation in the 65 or over Polish Population. Report of Cross-Sectional NOMED-AF Study. Kardiol. Pol. 2023, 81, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Wodchis, W.P.; Bhatia, R.S.; Leblanc, K.; Meshkat, N.; Morra, D. A Review of the Cost of Atrial Fibrillation. Value Health J. Int. Soc. Pharmacoecon. Outcomes Res. 2012, 15, 240–248. [Google Scholar] [CrossRef]
- Kirchhof, P.; Schmalowsky, J.; Pittrow, D.; Rosin, L.; Kirch, W.; Wegscheider, K.; Meinertz, T. ATRIUM Study Group Management of Patients with Atrial Fibrillation by Primary-Care Physicians in Germany: 1-Year Results of the ATRIUM Registry. Clin. Cardiol. 2014, 37, 277–284. [Google Scholar] [CrossRef]
- Christiansen, C.B.; Olesen, J.B.; Gislason, G.; Lock-Hansen, M.; Torp-Pedersen, C. Cardiovascular and Non-Cardiovascular Hospital Admissions Associated with Atrial Fibrillation: A Danish Nationwide, Retrospective Cohort Study. BMJ Open 2013, 3, e001800. [Google Scholar] [CrossRef]
- Mauro, V.; Lorenzo, M.; Paolo, C.; Sergio, H. Treat All COVID 19-Positive Patients, but Do Not Forget Those Negative with Chronic Diseases. Intern. Emerg. Med. 2020, 15, 787–790. [Google Scholar] [CrossRef]
- TIBCO Software Inc. Statistica (Data Analysis Software System), Version 13; TIBCO Software Inc.: Palo Alto, CA, USA, 2017; Available online: https://www.statistica.com/en/software/tibco-data-science-/-tibco-statistica (accessed on 29 October 2024).
- Abramson, J.H. WINPEPI Updated: Computer Programs for Epidemiologists, and Their Teaching Potential. Epidemiol. Persp. Innov. 2011, 8, 1. [Google Scholar] [CrossRef]
- Statistics Poland. Available online: http://stat.gov.pl (accessed on 30 July 2024).
- Patel, N.J.; Deshmukh, A.; Pant, S.; Singh, V.; Patel, N.; Arora, S.; Shah, N.; Chothani, A.; Savani, G.T.; Mehta, K.; et al. Contemporary Trends of Hospitalization for Atrial Fibrillation in the United States, 2000 Through 2010. Circulation 2014, 129, 2371–2379. [Google Scholar] [CrossRef]
- Naderi, S.; Wang, Y.; Miller, A.L.; Rodriguez, F.; Chung, M.K.; Radford, M.J.; Foody, J.M. The Impact of Age on the Epidemiology of Atrial Fibrillation Hospitalizations. Am. J. Med. 2014, 127, 158.e1–158.e7. [Google Scholar] [CrossRef] [PubMed]
- Charlemagne, A.; Blacher, J.; Cohen, A.; Collet, J.-P.; Diévart, F.; de Groote, P.; Hanon, O.; Leenhardt, A.; Pinel, J.-F.; Pisica-Donose, G.; et al. Epidemiology of Atrial Fibrillation in France: Extrapolation of International Epidemiological Data to France and Analysis of French Hospitalization Data. Arch. Cardiovasc. Dis. 2011, 104, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Ueberham, L.; König, S.; Pellissier, V.; Hohenstein, S.; Meier-Hellmann, A.; Kuhlen, R.; Hindricks, G.; Bollmann, A. Admission Rates and Care Pathways in Patients with Atrial Fibrillation during the COVID-19 Pandemic-Insights from the German-Wide Helios Hospital Network. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Noubiap, J.J.; Thomas, G.; Agbaedeng, T.A.; Fitzgerald, J.L.; Gallagher, C.; Middeldorp, M.E.; Sanders, P. Sex Differences in Clinical Profile, Management, and Outcomes of Patients Hospitalized for Atrial Fibrillation in the United States. Eur. Heart J. Qual. Care Clin. Outcomes 2022, 8, 852–860. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Q.; Shantsila, A.; Lane, D.A.; Zhou, Q.; Liu, Y.; Shen, Y.; Cheng, X.; Hong, K.; Lip, G.Y.H. Sex Differences in Clinical Characteristics and Inpatient Outcomes among 2442 Hospitalized Chinese Patients with Nonvalvular Atrial Fibrillation: The Nanchang Atrial Fibrillation Project. Int. J. Cardiol. 2015, 201, 195–199. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Laroche, C.; Boriani, G.; Cimaglia, P.; Dan, G.-A.; Santini, M.; Kalarus, Z.; Rasmussen, L.H.; Popescu, M.I.; Tica, O.; et al. Sex-Related Differences in Presentation, Treatment, and Outcome of Patients with Atrial Fibrillation in Europe: A Report from the Euro Observational Research Programme Pilot Survey on Atrial Fibrillation. EP Europace 2015, 17, 24–31. [Google Scholar] [CrossRef]
- Baroutidou, A.; Kartas, A.; Samaras, A.; Papazoglou, A.S.; Vrana, E.; Moysidis, D.V.; Akrivos, E.; Papanastasiou, A.; Vouloagkas, I.; Botis, M.; et al. Associations of Atrial Fibrillation Patterns with Mortality and Cardiovascular Events: Implications of the MISOAC-AF Trial. J. Cardiovasc. Pharmacol. Ther. 2022, 27, 10742484211069422. [Google Scholar] [CrossRef]
- Lee, E.; Choi, E.-K.; Han, K.-D.; Lee, H.; Choe, W.-S.; Lee, S.-R.; Cha, M.-J.; Lim, W.-H.; Kim, Y.-J.; Oh, S. Mortality and Causes of Death in Patients with Atrial Fibrillation: A Nationwide Population-Based Study. PLoS ONE 2018, 13, e0209687. [Google Scholar] [CrossRef]
- Andersson, T.; Magnuson, A.; Bryngelsson, I.-L.; Frøbert, O.; Henriksson, K.M.; Edvardsson, N.; Poçi, D. All-Cause Mortality in 272,186 Patients Hospitalized with Incident Atrial Fibrillation 1995-2008: A Swedish Nationwide Long-Term Case-Control Study. Eur. Heart J. 2013, 34, 1061–1067. [Google Scholar] [CrossRef]
- Bucci, T.; Proietti, M.; Shantsila, A.; Romiti, G.F.; Teo, W.-S.; Park, H.-W.; Shimizu, W.; Tse, H.-F.; Lip, G.Y.H.; Chao, T.-F.; et al. Integrated Care for Atrial Fibrillation Using the ABC Pathway in the Prospective APHRS-AF Registry. JACC Asia 2023, 3, 580–591. [Google Scholar] [CrossRef]
- Guo, Y.; Lane, D.A.; Wang, L.; Zhang, H.; Wang, H.; Zhang, W.; Wen, J.; Xing, Y.; Wu, F.; Xia, Y.; et al. Mobile Health Technology to Improve Care for Patients with Atrial Fibrillation. J. Am. Coll. Cardiol. 2020, 75, 1523–1534. [Google Scholar] [CrossRef] [PubMed]
- Marrouche, N.F.; Brachmann, J.; Andresen, D.; Siebels, J.; Boersma, L.; Jordaens, L.; Merkely, B.; Pokushalov, E.; Sanders, P.; Proff, J.; et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N. Engl. J. Med. 2018, 378, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Myrda, K.; Błachut, A.; Buchta, P.; Skrzypek, M.; Wnuk-Wojnar, A.-M.; Hoffmann, A.; Nowak, S.; Kowalski, O.; Pruszkowska, P.; Sokal, A.; et al. Clinical Characteristics of Patients with Atrial Fibrillation or Atrial Flutter Hospitalized during the COVID-19 Pandemic: A Population Analysis of Nearly 5 Million People. Pol. Arch. Intern. Med. 2021, 131, 574–577. [Google Scholar] [CrossRef] [PubMed]
- Wojtyniak, B.; Goryński, P. Health Status of Polish Population and Its Determinants 2022. Available online: https://www.pzh.gov.pl/raport-sytuacja-zdrowotna-ludnosci-polski-i-jej-uwarunkowania (accessed on 29 August 2024).
- Daoudi, S.; John, K.; Chalhoub, F.; Chee, J.; Infeld, M.; Elbaz-Greener, G.; Homoud, M.; Ruskin, J.N.; Heist, E.K.; Madias, C.; et al. Nationwide Trends in Hospitalizations for Atrial Fibrillation and Flutter in the United States before and during the Outbreak of the COVID-19 Pandemic. J. Clin. Med. 2024, 13, 4883. [Google Scholar] [CrossRef]
- Holt, A.; Gislason, G.H.; Schou, M.; Zareini, B.; Biering-Sørensen, T.; Phelps, M.; Kragholm, K.; Andersson, C.; Fosbøl, E.L.; Hansen, M.L.; et al. New-Onset Atrial Fibrillation: Incidence, Characteristics, and Related Events Following a National COVID-19 Lockdown of 5.6 Million People. Eur. Heart J. 2020, 41, 3072–3079. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dąbrowska, M.; Rząd, M.; Kanecki, K.; Lewtak, K.; Tyszko, P.; Goryński, P.; Nitsch-Osuch, A. Hospitalizations of Patients with Atrial Fibrillation (AF) in Poland: A Nationwide Study Based on over One Million AF Hospitalizations in 2017–2021. J. Clin. Med. 2024, 13, 6592. https://doi.org/10.3390/jcm13216592
Dąbrowska M, Rząd M, Kanecki K, Lewtak K, Tyszko P, Goryński P, Nitsch-Osuch A. Hospitalizations of Patients with Atrial Fibrillation (AF) in Poland: A Nationwide Study Based on over One Million AF Hospitalizations in 2017–2021. Journal of Clinical Medicine. 2024; 13(21):6592. https://doi.org/10.3390/jcm13216592
Chicago/Turabian StyleDąbrowska, Martyna, Michał Rząd, Krzysztof Kanecki, Katarzyna Lewtak, Piotr Tyszko, Paweł Goryński, and Aneta Nitsch-Osuch. 2024. "Hospitalizations of Patients with Atrial Fibrillation (AF) in Poland: A Nationwide Study Based on over One Million AF Hospitalizations in 2017–2021" Journal of Clinical Medicine 13, no. 21: 6592. https://doi.org/10.3390/jcm13216592
APA StyleDąbrowska, M., Rząd, M., Kanecki, K., Lewtak, K., Tyszko, P., Goryński, P., & Nitsch-Osuch, A. (2024). Hospitalizations of Patients with Atrial Fibrillation (AF) in Poland: A Nationwide Study Based on over One Million AF Hospitalizations in 2017–2021. Journal of Clinical Medicine, 13(21), 6592. https://doi.org/10.3390/jcm13216592





