Single-Port Versus Reduced-Port (1 + 1) Robotic Myomectomy and Hysterectomy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
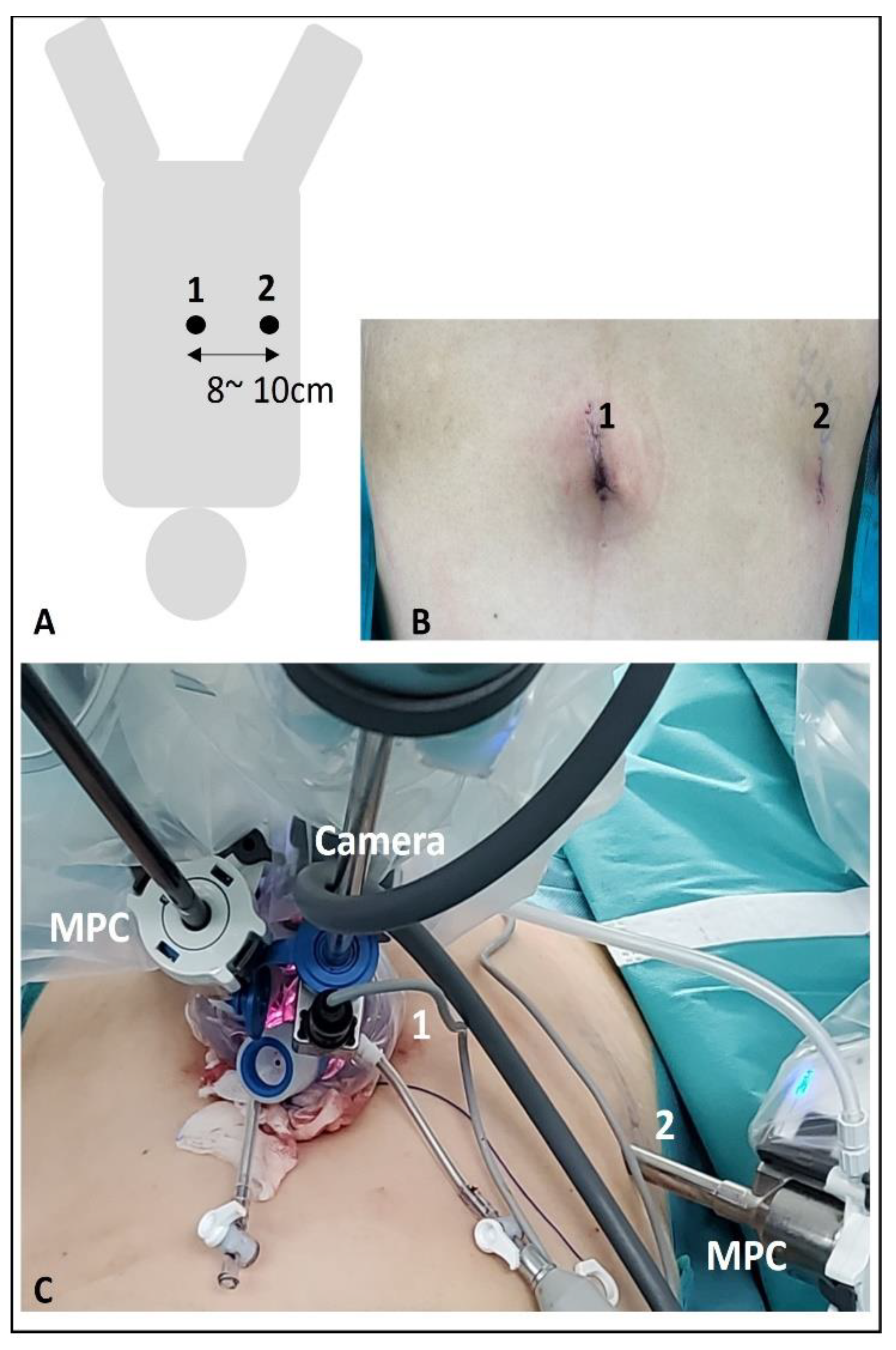
2.2. Surgical Procedures
2.3. Statistical Analysis
3. Results
3.1. Baseline Patient Characteristics
3.2. Comparison Between Single-Port Robotic Myomectomy and Reduced-Port Robotic Myomectomy
3.3. Comparison Between Single-Port Robotic Hysterectomy and Reduced-Port Robotic Hysterectomy
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Conrad, L.B.; Ramirez, P.T.; Burke, W.; Naumann, R.W.; Ring, K.L.; Munsell, M.F.; Frumovitz, M. Role of Minimally Invasive Surgery in Gynecologic Oncology: An Updated Survey of Members of the Society of Gynecologic Oncology. Int. J. Gynecol. Cancer 2015, 25, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Von Gruenigen, V.E.; Sawyer, M.D.; Ponsky, L.E.; Hurd, W.W. Recent Innovations in Minimally Invasive Surgery and Implications for Gynecology. J. Gynecol. Surg. 2009, 25, 67–72. [Google Scholar] [CrossRef]
- Kaouk, J.H.; Autorino, R.; Kim, F.J.; Han, D.H.; Lee, S.W.; Yinghao, S.; Cadeddu, J.A.; Derweesh, I.H.; Richstone, L.; Cindolo, L.; et al. Laparoendoscopic single-site surgery in urology: Worldwide multi-institutional analysis of 1076 cases. Eur. Urol. 2011, 60, 998–1005. [Google Scholar] [CrossRef] [PubMed]
- Yim, G.W.; Jung, Y.W.; Paek, J.; Lee, S.H.; Kwon, H.Y.; Nam, E.J.; Kim, S.; Kim, J.H.; Kim, Y.T.; Kim, S.W. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: Surgical outcomes. Am. J. Obstet. Gynecol. 2010, 203, 26.e1–26.e6. [Google Scholar] [CrossRef] [PubMed]
- Nelson, R.J.; Chavali, J.S.S.; Yerram, N.; Babbar, P.; Kaouk, J.H. Current status of robotic single-port surgery. Urol. Ann. 2017, 9, 217–222. [Google Scholar]
- Nam, E.J.; Kim, S.W.; Lee, M.; Yim, G.W.; Paek, J.H.; Lee, S.H.; Kim, S.; Kim, J.H.; Kim, J.W.; Kim, Y.T. Robotic single-port transumbilical total hysterectomy: A pilot study. J. Gynecol. Oncol. 2011, 22, 120–126. [Google Scholar] [CrossRef][Green Version]
- Morelli, L.; Guadagni, S.; Di Franco, G.; Palmeri, M.; Di Candio, G.; Mosca, F. Da Vinci single site© surgical platform in clinical practice: A systematic review. Int. J. Med. Robot. 2016, 12, 724–734. [Google Scholar] [CrossRef]
- Kane, S.; Stepp, K.J. Laparo-endoscopic single-site surgery hysterectomy using robotic lightweight endoscope assistants. J. Robot. Surg. 2010, 3, 253–255. [Google Scholar] [CrossRef]
- Cela, V.; Freschi, L.; Simi, G.; Ruggiero, M.; Tana, R.; Pluchino, N. Robotic single-site hysterectomy: Feasibility, learning curve and surgical outcome. Surg. Endosc. 2013, 27, 2638–2643. [Google Scholar] [CrossRef]
- Iavazzo, C.; Minis, E.E.; Gkegkes, I.D. Single-site port robotic-assisted hysterectomy: An update. J. Robot. Surg. 2018, 12, 201–213. [Google Scholar] [CrossRef]
- Lee, S.R. Robotic Single-Site(R) Sacrocolpopexy: First Report and Technique Using the Single-Site(R) Wristed Needle Driver. Yonsei Med. J. 2016, 57, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.S.; Shim, J.E.; Lee, S.R.; Jeong, K. The Comparison of Robotic Single-Site Surgery to Single-Port Laparoendoscopic Surgery for the Treatment of Advanced-Stage Endometriosis. J. Laparoendosc. Adv. Surg. Tech. A 2018, 28, 1483–1488. [Google Scholar] [CrossRef]
- Scheib, S.A.; Fader, A.N. Gynecologic robotic laparoendoscopic single-site surgery: Prospective analysis of feasibility, safety, and technique. Am. J. Obstet. Gynecol. 2015, 212, 179.e1–179.e8. [Google Scholar] [CrossRef]
- Choi, E.J.; Rho, A.M.; Lee, S.R.; Jeong, K.; Moon, H.S. Robotic Single-Site Myomectomy: Clinical Analysis of 61 Consecutive Cases. J. Minim. Invasive Gynecol. 2017, 24, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, M.K.; Kim, M.L.; Jung, Y.W.; Yun, B.S.; Seong, S.J. Robotic single-site myomectomy: A single-center experience of 101 consecutive cases. Int. J. Med. Robot. 2019, 15, e1959. [Google Scholar] [CrossRef]
- Lee, S.R.; Lee, E.S.; Eum, H.R.; Lee, Y.J.; Lee, S.W.; Park, J.Y.; Suh, D.S.; Kim, D.Y.; Kim, S.H.; Kim, Y.M.; et al. New surgical technique for robotic myomectomy: Continuous locking suture on myoma (LSOM) technique. J. Clin. Med. 2021, 10, 654. [Google Scholar] [CrossRef]
- Moawad, G.N.; Tyan, P.; Paek, J.; Tappy, E.E.; Park, D.; Choussein, S.; Srouji, S.S.; Gargiulo, A. Comparison between single-site and multiport robot-assisted myomectomy. J. Robot. Surg. 2019, 13, 757–764. [Google Scholar] [CrossRef]
- Shin, H.J.; Yoo, H.K.; Lee, J.H.; Lee, S.R.; Jeong, K.; Moon, H.S. Robotic single-port surgery using the da Vinci SP® surgical system for benign gynecologic disease: A preliminary report. Taiwan J. Obstet. Gynecol. 2020, 59, 243–247. [Google Scholar] [CrossRef]
- Misal, M.; Magtibay, P.M.; Yi, J. Robotic LESS and Reduced-Port Hysterectomy Using the da Vinci SP Surgical System: A Single-Institution Case Series. J. Minim. Invasive Gynecol. 2021, 28, 1095–1100. [Google Scholar] [CrossRef]
- Kwak, Y.H.; Lee, H.; Seon, K.; Lee, Y.J.; Lee, Y.J.; Kim, S.W. Da Vinci SP Single-Port Robotic Surgery in Gynecologic Tumors: Single Surgeon’s Initial Experience with 100 Cases. Yonsei Med. J. 2022, 63, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kim, M.R.; Seong, S.J.; Paek, J.; Lee, Y.S.; Nam, E.J.; Kim, Y.M.; Park, Y.H.; Kim, T.J.; Kim, Y.B. Trends in robotic surgery in Korean gynecology. Gyne Robot. Surg. 2020, 1, 50–56. [Google Scholar] [CrossRef]
| Characteristics | Myomectomy | Hysterectomy | Total |
|---|---|---|---|
| age (years, mean ± SD) | 36.57 ± 5.20 | 44.33 ± 7.85 | 38.76 ± 6.96 |
| BMI (kg/m2, mean ± SD) | 22.64 ± 3.66 | 23.28 ± 3.71 | 22.83 ± 3.69 |
| gravidity, median (range) | 0 (0–6) | 2 (0–6) | 0 (0–6) |
| parity, median (range) | 0 (0–3) | 1 (0–3) | 0 (0–3) |
| previous cesarean section history | |||
| 0, n (%) | 126 (95.45) | 33 (63.46) | 160 (86.96) |
| ≥1, n (%) | 6 (4.55) | 19 (36.54) | 24 (13.04) |
| previous pelvic surgery history | |||
| 0, n (%) | 122 (92.42) | 38 (73.08) | 160 (86.96) |
| ≥1, n (%) | 10 (7.58) | 14 (26.92) | 24 (13.04) |
| diseases | 10 (9.4) | 10 (9.4) | |
| Myoma, n (%) | 132 (100%) | 34 (65.39%) | 166 (90.23%) |
| Adenomyosis, n (%) | 10 (19.24%) | 10 (5.44%) | |
| Endometrial intraepithelial neoplasia, n (%) | 3 (5.77%) | 3 (1.63%) | |
| Cervical carcinoma in situ n (%) | 1 (1.92%) | 1 (0.54%) | |
| Endometrial hyperplasia, n (%) | 1 (1.92%) | 1 (0.54%) | |
| Endometrial polyp, n (%) | 1 (1.92%) | 1 (0.54%) | |
| Unicornuate uterus, n (%) | 1 (1.92%) | 1 (0.54%) | |
| Uterine didelphys, n (%) | 1 (1.92%) | 1 (0.54%) |
| Characteristics | |
|---|---|
| anesthesia time (min, mean ± SD) | 176.74 ± 56.07 |
| operation time (min, mean ± SD) | 146.68 ± 50.16 |
| conversion to multiport or laparotomy, n (%) | 0 (0) |
| estimated blood loss (mL, mean ± SD) | 172.02 ± 152.23 |
| postoperative hemoglobin change (g/dL, mean ± SD) | 2.61 ± 2.59 |
| transfusion | |
| 0, n (%) | 174 (94.56%) |
| ≥1, n (%) | 10 (5.44%) |
| postoperative hospital stay (day, mean ± SD) | 2.09 ± 0.48 |
| postoperative fever (within 48 h) | |
| 0, n (%) | 178 (96.74%) |
| ≥1, n (%) | 6 (3.26%) |
| SP-RM (n = 94) | RP-RM (n = 38) | p Value | |
|---|---|---|---|
| age (years, mean ± SD) | 36.51 ± 5.44 | 36.71 ± 4.60 | 0.842 |
| gravidity, median (range) | 0 (0–6) | 0 (0–3) | 0.261 |
| parity, median (range) | 0 (0–2) | 0 (0–3) | 0.259 |
| BMI (kg/m2, mean ± SD) | 22.42 ± 3.83 | 23.21 ± 3.19 | 0.261 |
| previous cesarean section history | |||
| 0, n (%) | 90 (95.7%) | 36 (94.7%) | 0.801 |
| ≥1, n (%) | 4 (4.3%) | 2 (5.3%) | |
| previous pelvic surgery history | |||
| 0, n (%) | 86 (91.5%) | 36 (94.7%) | 0.523 |
| ≥1, n (%) | 8 (8.5%) | 2 (5.3%) | |
| type of main myoma | |||
| intramural, n (%) | 79 (84.0%) | 31 (81.6%) | 0.819 |
| submucosal, n (%) | 2 (2.1%) | 2 (5.3%) | |
| subserosal, n (%) | 3 (3.2%) | 1 (2.6%) | |
| others (intraligamentary, cervical), n (%) | 10 (10.6%) | 4 (10.5%) | |
| maximal myoma diameter (cm, mean ± SD) | 8.22 ± 2.36 | 8.42 ± 2.70 | 0.676 |
| numbers of myomas, removed, median (range) * | 2.70 (1–11) | 4.26 (1–21) | 0.009 * |
| multiple myomas, n (%) | 41 (43.6) | 12 (31.6) | 0.201 |
| numbers of myomas > 3 cm, median (range) | 1.54 (1–7) | 1.74 (1–4) | 0.353 |
| weight of removed myomas (g, mean ± SD) | 218.77 ± 189.54 | 215.05 ± 150.23 | 0.914 |
| concomitant surgery, n (%) * | 29 (30.9) | 20 (52.6) | 0.019 * |
| anesthesia time (min, mean ± SD) | 184.70 ± 64.63 | 172.05 ± 31.50 | 0.252 |
| operation time (min, mean ± SD) | 150.55± 55.93 | 142.26 ± 29.87 | 0.389 |
| estimated blood loss (mL, mean ± SD) | 188.83 ± 182.79 | 182.37 ± 91.84 | 0.836 |
| postoperative hemoglobin change (g/dL, mean ± SD) | 2.66 ± 1.25 | 3.07 ± 1.32 | 0.094 |
| transfusion | |||
| 0, n (%) | 87 (92.6) | 38 (100) | 0.084 |
| ≥1, n (%) | 7 (7.4) | 0 (0) | |
| postoperative hospital stay (day, mean ± SD) | 2.04 ± 0.20 | 2.03 ± 0.16 | 0.661 |
| postoperative fever (within 48 h) | |||
| 0, n (%) | 90 (94.7) | 36 (94.7) | 0.99 |
| ≥1, n (%) | 4 (5.3) | 2 (5.3) |
| SP-RH (n = 33) | RP-RH (n = 19) | p Value | |
|---|---|---|---|
| age (years, mean ± SD) | 45.33 ± 7.59 | 42.58 ± 8.18 | 0.226 |
| gravidity, median (range) | 2 (0–6) | 1 (0–3) | 0.517 |
| parity, median (range) | 1 (0–3) | 1 (0–2) | 0.139 |
| BMI (kg/m2, mean ± SD) | 23.07 ± 3.32 | 23.66 ± 4.37 | 0.583 |
| previous cesarean section history | |||
| 0, n (%) | 20 (60.6) | 13 (68.4) | 0.34 |
| ≥1, n (%) | 13 (39.4) | 6 (31.6) | |
| previous pelvic surgery history | |||
| 0, n (%) | 25 (75.8) | 13 (68.4) | 0.566 |
| ≥1, n (%) | 8 (24.2) | 6 (31.6) | |
| weight of uterus (g, mean ± SD) | 326.67± 230.76 | 347.87± 271.75 | 0.766 |
| concomitant surgery, n (%) | 25 (75.7) | 9 (47.4) | 0.1 |
| anesthesia time (min, mean ± SD) * | 183.09 ± 55.17 | 135.74 ± 26.58 | 0.001 * |
| operation time (min, mean ± SD) * | 159.79 ± 55.04 | 113.58 ± 24.61 | 0.001 * |
| estimated blood loss (mL, mean ± SD) | 153.33 ± 131.69 | 94.21 ± 74.86 | 0.079 |
| postoperative hemoglobin change (g/dL, mean ± SD) | 2.28 ± 1.30 | 2.05 ± 1.06 | 0.506 |
| transfusion | |||
| 0, n (%) | 30 (90.9) | 19 (100) | 0.176 |
| ≥1, n (%) | 3 (9.1) | 0 (0) | |
| postoperative hospital stay (day, mean ± SD) | 2.19 ± 0.90 | 2.26 ± 0.81 | 0.764 |
| postoperative fever (within 48 h) | |||
| 0, n (%) | 33 (100) | 18 (94.7) | 0.183 |
| ≥1, n (%) | 0 (0) | 1 (5.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.Y.; Lee, S.R.; Song, J.Y. Single-Port Versus Reduced-Port (1 + 1) Robotic Myomectomy and Hysterectomy. J. Clin. Med. 2024, 13, 6563. https://doi.org/10.3390/jcm13216563
Lee SY, Lee SR, Song JY. Single-Port Versus Reduced-Port (1 + 1) Robotic Myomectomy and Hysterectomy. Journal of Clinical Medicine. 2024; 13(21):6563. https://doi.org/10.3390/jcm13216563
Chicago/Turabian StyleLee, So Young, Sa Ra Lee, and Jae Yen Song. 2024. "Single-Port Versus Reduced-Port (1 + 1) Robotic Myomectomy and Hysterectomy" Journal of Clinical Medicine 13, no. 21: 6563. https://doi.org/10.3390/jcm13216563
APA StyleLee, S. Y., Lee, S. R., & Song, J. Y. (2024). Single-Port Versus Reduced-Port (1 + 1) Robotic Myomectomy and Hysterectomy. Journal of Clinical Medicine, 13(21), 6563. https://doi.org/10.3390/jcm13216563





