Ethnic Disparities of Arrival Following ST Elevation Myocardial Infarction in South Israel
Abstract
1. Introduction
2. Materials and Methods
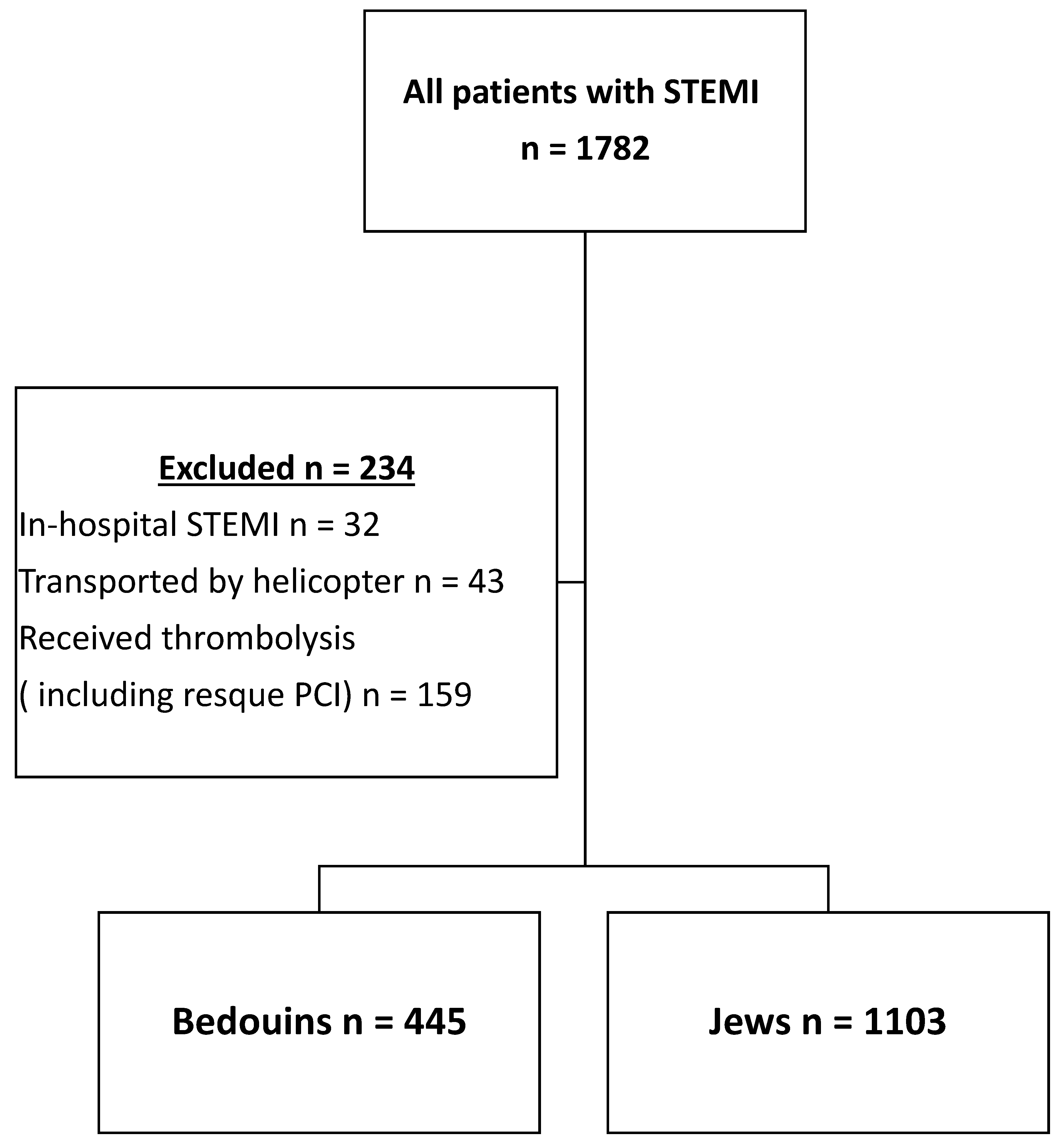
2.1. Patient Population
2.2. Statistical Analysis
3. Results
3.1. Patient Population
3.2. Mode of Transportation, Door-to-Balloon Time and Total Ischemic Time
3.3. Outcomes and Predictors for 1-Year Mortality
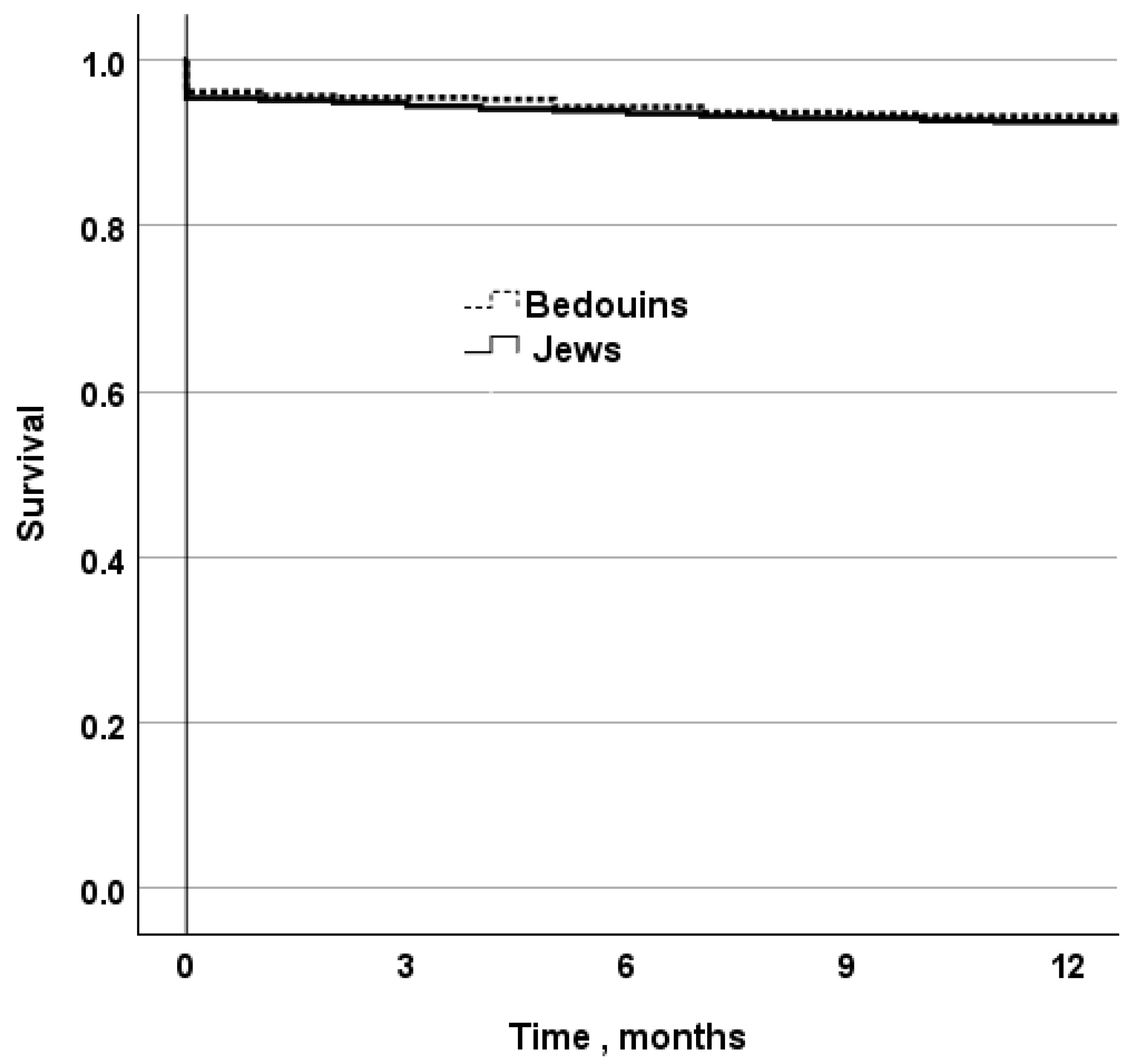
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826, Erratum in Eur. Heart J. 2024, 45, 1145. [Google Scholar] [CrossRef] [PubMed]
- Lawton, J.S.; Tamis-Holland, J.E.; Bangalore, S.; Bates, E.R.; Beckie, T.M.; Bischoff, J.M.; Bittl, J.A.; Cohen, M.G.; DiMaio, J.M.; Don, C.W.; et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e18–e114, Erratum in Circulation 2022, 145, e772. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.M.; Zhang, R.; Findlay, I.; Robertson, K.; Lindsay, M.; Morris, T.; Forbes, B.; Papworth, R.; McConnachie, A.; Mangion, K.; et al. Healthcare disparities for women hospitalized with myocardial infarction and angina. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 6, 156–165. [Google Scholar] [CrossRef]
- Terkelsen, C.J.; Sørensen, J.T.; Maeng, M.; Jensen, L.O.; Tilsted, H.H.; Trautner, S.; Vach, W.; Johnsen, S.P.; Thuesen, L.; Lassen, J.F. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010, 304, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Jortveit, J.; Pripp, A.H.; Halvorsen, S. Outcomes after delayed primary percutaneous coronary intervention vs. pharmaco-invasive strategy in ST-segment elevation myocardial infarction in Norway. Eur. Heart J. Cardiovasc. Pharmacother. 2022, 8, 442–451. [Google Scholar] [CrossRef]
- Larsen, A.I.; Løland, K.H.; Hovland, S.; Bleie, Ø.; Eek, C.; Fossum, E.; Trovik, T.; Juliebø, V.; Hegbom, K.; Moer, R.; et al. Guideline-recommended time less than 90 minutes from ECG to primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction is associated with major survival benefits, especially in octogenarians: A contemporary report in 11,226 patients from NORIC. J. Am. Heart Assoc. 2022, 11, e024849. [Google Scholar] [CrossRef]
- Kontos, M.C.; Gunderson, M.R.; Zegre-Hemsey, J.K.; Lange, D.C.; French, W.J.; Henry, T.D.; McCarthy, J.J.; Corbett, C.; Jacobs, A.K.; Jollis, J.G.; et al. Prehospital activation of hospital resources (PreAct) ST-segment-elevation myocardial infarction (STEMI): A standardized approach to prehospital activation and direct to the catheterization laboratory for STEMI recommendations from the American Heart Association’s mission: Lifeline program. J. Am. Heart Assoc. 2020, 9, e011963. [Google Scholar] [CrossRef]
- Squire, B.T.; Tamayo-Sarver, J.H.; Rashi, P.; Koenig, W.; Niemann, J.T. Effect of prehospital cardiac catheterization lab activation on door-to-balloon time, mortality, and false-positive activation. Prehosp. Emerg. Care 2014, 18, 1–8. [Google Scholar] [CrossRef]
- Fordyce, C.B.; Al-Khalidi, H.R.; Jollis, J.G.; Roettig, M.L.; Gu, J.; Bagai, A.; Berger, P.B.; Corbett, C.C.; Dauerman, H.L.; Fox, K.; et al. Association of rapid care process implementation on reperfusion times across multiple ST-segment-elevation myocardial infarction networks. Circ. Cardiovasc. Interv. 2017, 10, e004061. [Google Scholar] [CrossRef]
- Shavadia, J.S.; Roe, M.T.; Chen, A.Y.; Lucas, J.; Fanaroff, A.C.; Kochar, A.; Berger, P.B.; Corbett, C.C.; Dauerman, H.L.; Fox, K.; et al. Association between cardiac catheterization laboratory pre-activation and reperfusion timing metrics and outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: A report from the ACTION registry. JACC Cardiovasc. Interv. 2018, 11, 1837–1847. [Google Scholar] [CrossRef]
- Stowens, J.C.; Sonnad, S.S.; Rosenbaum, R.A. Using EMS dispatch to trigger STEMI alerts decreases door-to-balloon times. West J. Emerg. Med. 2015, 16, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Huber, K.; De Caterina, R.; Kristensen, S.D.; Verheugt, F.W.A.; Montalescot, G.; Maestro, L.B.; Werf, F.V.D. Pre-hospital reperfusion therapy: A strategy to improve therapeutic outcome in patients with ST-elevation myocardial infarction. Eur. Heart J. 2005, 26, 2063–2074. [Google Scholar] [CrossRef] [PubMed]
- Meisel, S.R.; Kleiner-Shochat, M.; Abu-Fanne, R.; Frimerman, A.; Danon, A.; Minha, S.; Levi, Y.; Blatt, A.; Mohsen, J.; Shotan, A.; et al. Direct admission of patients with ST-segment-elevation myocardial infarction to the catheterization laboratory shortens pain-to-balloon and door-to-balloon time intervals but only the pain-to-balloon interval impacts short- and long-term mortality. J. Am. Heart Assoc. 2021, 10, e018343. [Google Scholar] [CrossRef]
- Bagai, A.; Jollis, J.G.; Dauerman, H.L.; Peng, S.A.; Rokos, I.C.; Bates, E.R.; Bates, E.R.; French, W.J.; Granger, C.B.; Roe, M.T. Emergency department bypass for ST-segment-elevation myocardial infarction patients identified with a prehospital electrocardiogram: A report from the American Heart Association Mission: Lifeline program. Circulation 2013, 128, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Scholz, K.H.; Friede, T.; Meyer, T.; Jacobshagen, C.; Lengenfelder, B.; Jung, J.; Fleischmann, C.; Moehlis, H.; Olbrich, H.G.; Ott, R.; et al. Prognostic significance of emergency department bypass in stable and unstable patients with ST-segment elevation myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Karkabi, B.; Zafrir, B.; Jaffe, R.; Shiran, A.; Jubran, A.; Adawi, S.; Ben-Dov, N.; Iakobishvili, Z.; Beigel, R.; Cohen, M.; et al. Ethnic Differences Among Acute Coronary Syndrome Patients in Israel. Cardiovasc. Revasc. Med. 2020, 21, 1431–1435. [Google Scholar] [CrossRef] [PubMed]
- Plakht, Y.; Gilutz, H.; Shiyovich, A.; Zahger, D.; Weitzman, S. Gender and ethnic disparities in outcome following acute myocardial infarction among Bedouins and Jews in southern Israel. Eur. J. Public Health 2011, 21, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.D.; Gefen, K.; Ozer, A.; Bagola, N.; Milrad, V.; Cohen, L.; Abu-Hammad, T.; Abu-Rabia, Y.; Hazanov, I.; Vardy, D.A. Diabetes control in the Bedouin population in southern Israel. Med. Sci. Monit. 2005, 11, CR376–CR380. [Google Scholar] [PubMed]
- Callachan, E.L.; Alsheikh-Ali, A.A.; Nair, S.C.; Bruijns, S.; Wallis, L.A. Outcomes by Mode of Transport of ST Elevation MI Patients in the United Arab Emirates. West. J. Emerg. Med. 2017, 18, 349–355. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Najafi, H.; Bahramali, E.; Bijani, M.; Dehghan, A.; Amirkhani, M.; Balaghi Inaloo, M. Comparison of the outcomes of EMS vs. Non-EMS transport of patients with ST-segment elevation myocardial infarction (STEMI) in Southern Iran: A population-based study. BMC Emerg. Med. 2022, 22, 46, Erratum in BMC Emerg. Med. 2022, 22, 72. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mathews, R.; Peterson, E.D.; Li, S.; Roe, M.T.; Glickman, S.W.; Wiviott, S.D.; Saucedo, J.F.; Antman, E.M.; Jacobs, A.K.; Wang, T.Y. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: Findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get with the Guidelines. Circulation 2011, 124, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Newport, R.; Grey, C.; Dicker, B.; Ameratunga, S.; Harwood, M. Ethnic differences of the care pathway following an out-of-hospital cardiac event: A systematic review. Resuscitation 2023, 193, 110017. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Jews n = 1103 | Bedouins n= 445 | p-Value | Jews (After Propensity Score Matching) n = 445 | Bedouins n = 445 | p = Value |
|---|---|---|---|---|---|---|
| Age, years, mean ± SD | 62.6 ± 12.6 | 56.1 ± 12.6 | <0.001 | 61± 13.3 | 56.1 ± 12.6 | <0.001 |
| Male, n (%) | 881 (79.9) | 387 (87) | <0.001 | 362 (81.3) | 387 (87) | 0.02 |
| Ischemic heart disease, n (%) | 245 (22.2) | 121 (27.2) | 0.04 | 96 (21.6) | 121 (27.2) | 0.06 |
| Hypertension, n (%) | 548 (49.7) | 198 (44.5) | 0.06 | 221 (49.7) | 198 (44.5) | 0.1 |
| Diabetes mellitus, n (%) | 336 (30.5) | 174 (39.1) | 0.001 | 125 (28.1) | 174 (39.1) | <0.001 |
| Smoking, n (%) | 517 (46.9) | 305 (68.5) | <0.001 | 200 (44.9) | 305 (68.5) | <0.001 |
| Dyslipidemia, n (%) | 752 (68.2) | 305 (68.5) | 0.9 | 291 (65.4) | 305 (68.5) | 0.3 |
| Charlson’s score, median, IQR | 2 (1; 4) | 2 (1; 3) | <0.001 | 2 (1; 4) | 2 (1; 3) | 0.02 |
| Direct Arrival to Catheterization laboratory or ICCU, n (%) | 572 (51.9) | 194 (43.6) | 0.003 | 251 (56.4) | 194 (43.6) | 0.1 |
| Pathways of arrival to the hospital | ||||||
| Self-transportation, n (%) | 200 (18.1) | 91 (20.4) | 0.3 | 91 (20.4) | 91 (20.4) | 1 |
| Arrival by ambulance, n (%) | 628 (56.9) | 142 (31.9) | <0.001 | 219 (49.2) | 142 (31.9) | <0.001 |
| Arrival from outpatient clinic, n (%) | 275 (24.9) | 212 (47.6) | <0.001 | 135 (30.3) | 212 (47.6) | <0.001 |
| Time to first medical contact, min, median (IQR) | 80 (40; 180) | 90 (45; 195) | 0.17 | 85 (40; 190) | 90 (45; 195) | 0.3 |
| Symptom-onset to hospital-arrival time, min, median (IQR) | 120 (75; 227) | 130 (80; 240) | 0.16 | 122 (70; 225) | 130 (80; 240) | 0.2 |
| Time from arrival to hospital to catheterization, min, median (IQR) | 47 (30; 70) | 50 (30; 76) | 0.019 | 47 (47; 69) | 50 (30; 76) | 0.048 |
| Door-to-balloon time, min, median (IQR) | 62 (44; 85) | 65 (45; 89) | 0.044 | 62 (45; 85) | 65 (45; 89) | 0.1 |
| Pain-to-balloon time, min, median (IQR) | 190 (140; 302) | 200 (147; 305) | 0.058 | 195 (137; 302) | 200 (147; 305) | 0.7 |
| Significant left ventricular dysfunction, n (%) | 601 (54.5) | 256 (57.5) | 0.3 | 254 (57.1) | 256 (57.5) | 0.9 |
| Sustained ventricular tachycardia or ventricular fibrillation, n (%) | 94 (8.5) | 50 (11.2) | 0.1 | 38 (8.5) | 50 (11.2) | 0.1 |
| Complete atrioventricular block, n (%) | 37 (3.4) | 8 (1.8) | 0.084 | 8 (1.8) | 8 (1.8) | 1 |
| Cardiogenic Shock, n (%) | 61 (5.5) | 21 (4.7) | 0.5 | 22 (4.9) | 21 (4.7) | 0.8 |
| Outcomes | Jews n = 1103 | Bedouins n= 445 | p-Value |
|---|---|---|---|
| 30-day mortality, n (%) | 71 (6.4) | 31 (7.0) | 0.3 |
| Self-transportation, n (%) | 10 (5) | 2 (2.2) | 0.3 |
| Arrival by ambulance, n (%) | 49 (7.8) | 14 (9.9) | 0.3 |
| Arrival from outpatient clinic, n (%) | 12 (4.4) | 15 (7.1) | 0.004 |
| In- hospital ortality, n (%) | 68 (6.2) | 27 (6.1) | 0.9 |
| Self-transportation, n (%) | 10 (5) | 2 (2.2) | 0.3 |
| Arrival by ambulance, n (%) | 47 (7.5) | 13 (9.2) | 0.5 |
| Arrival from outpatient clinic, n (%) | 11 (4) | 12 (5.7) | 0.4 |
| One-year mortality, n (%) | 119 (10.8) | 47 (10.8) | 0.96 |
| Self-transportation, n (%) | 18 (9) | 2 (2.2) | 0.06 |
| Arrival by ambulance, n (%) | 85 (13.5) | 20 (14.1) | 0.8 |
| Arrival from outpatient clinic, n (%) | 16 (5.8) | 22 (10.4) | <0.001 |
| Factor | Hazard Ratio | 95% CI | p-Value |
|---|---|---|---|
| Cardiogenic Shock | 7.8 | 5.6–11.1 | <0.001 |
| Charlson comorbidity index, increment for each point | 1.5 | 1.4–1.7 | <0.001 |
| Significant left ventricular dysfunction vs. mild dysfunction or preserved systolic function | 3.2 | 2.1–4.9 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeldetz, V.; Nevzorov, R.; Weissberg, I.; Jotkowitz, A.B.; Shamia, D.; Slutsky, T.; Schwarzfuchs, D. Ethnic Disparities of Arrival Following ST Elevation Myocardial Infarction in South Israel. J. Clin. Med. 2024, 13, 6516. https://doi.org/10.3390/jcm13216516
Zeldetz V, Nevzorov R, Weissberg I, Jotkowitz AB, Shamia D, Slutsky T, Schwarzfuchs D. Ethnic Disparities of Arrival Following ST Elevation Myocardial Infarction in South Israel. Journal of Clinical Medicine. 2024; 13(21):6516. https://doi.org/10.3390/jcm13216516
Chicago/Turabian StyleZeldetz, Vladimir, Roman Nevzorov, Itai Weissberg, Alan B. Jotkowitz, David Shamia, Tzachi Slutsky, and Dan Schwarzfuchs. 2024. "Ethnic Disparities of Arrival Following ST Elevation Myocardial Infarction in South Israel" Journal of Clinical Medicine 13, no. 21: 6516. https://doi.org/10.3390/jcm13216516
APA StyleZeldetz, V., Nevzorov, R., Weissberg, I., Jotkowitz, A. B., Shamia, D., Slutsky, T., & Schwarzfuchs, D. (2024). Ethnic Disparities of Arrival Following ST Elevation Myocardial Infarction in South Israel. Journal of Clinical Medicine, 13(21), 6516. https://doi.org/10.3390/jcm13216516







