The Significance of the Myocardial Performance Index and Fetal Doppler Abnormalities in Growth-Restricted Fetuses: A Systematic Review of the Literature
Abstract
1. Introduction
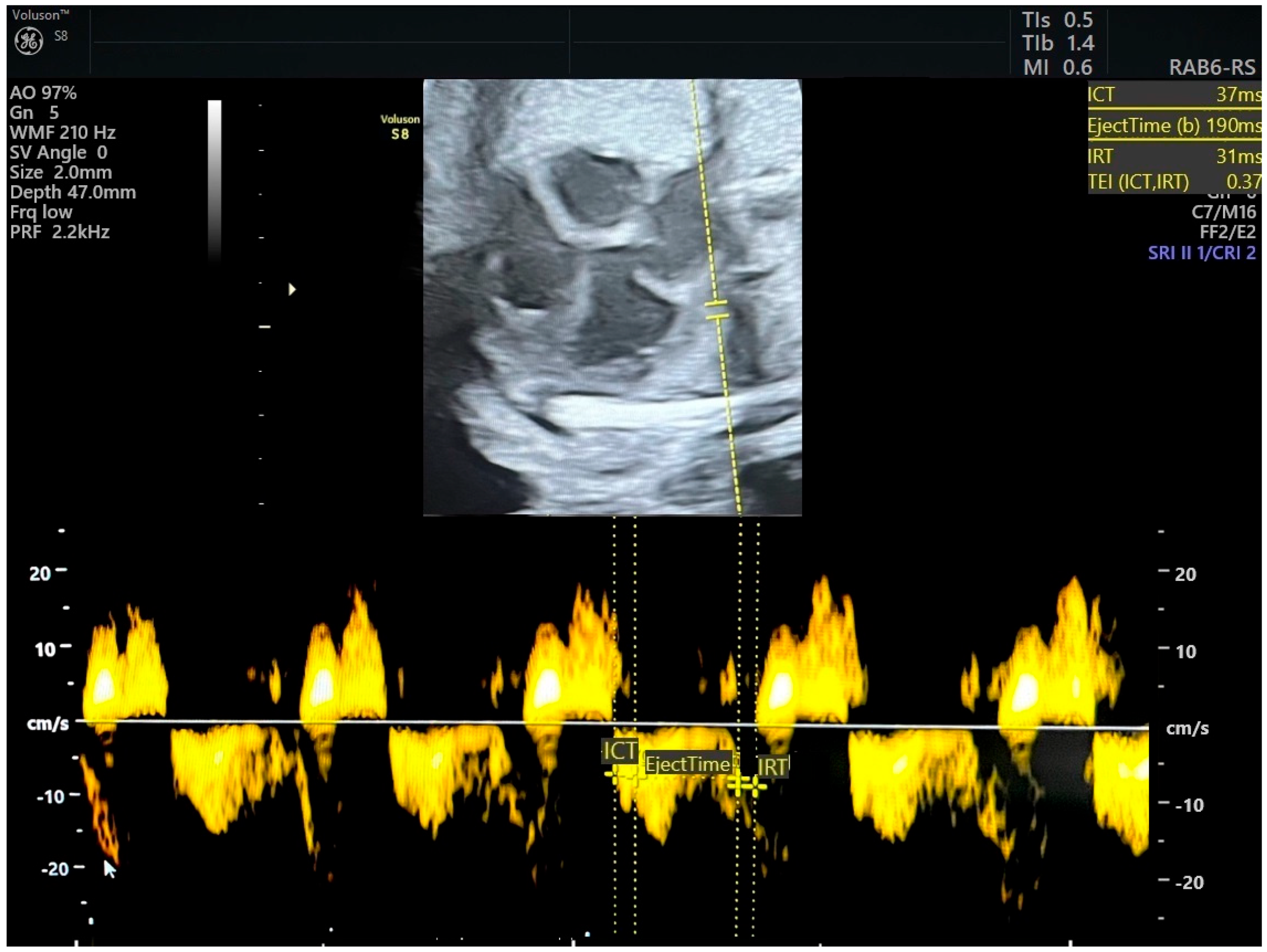
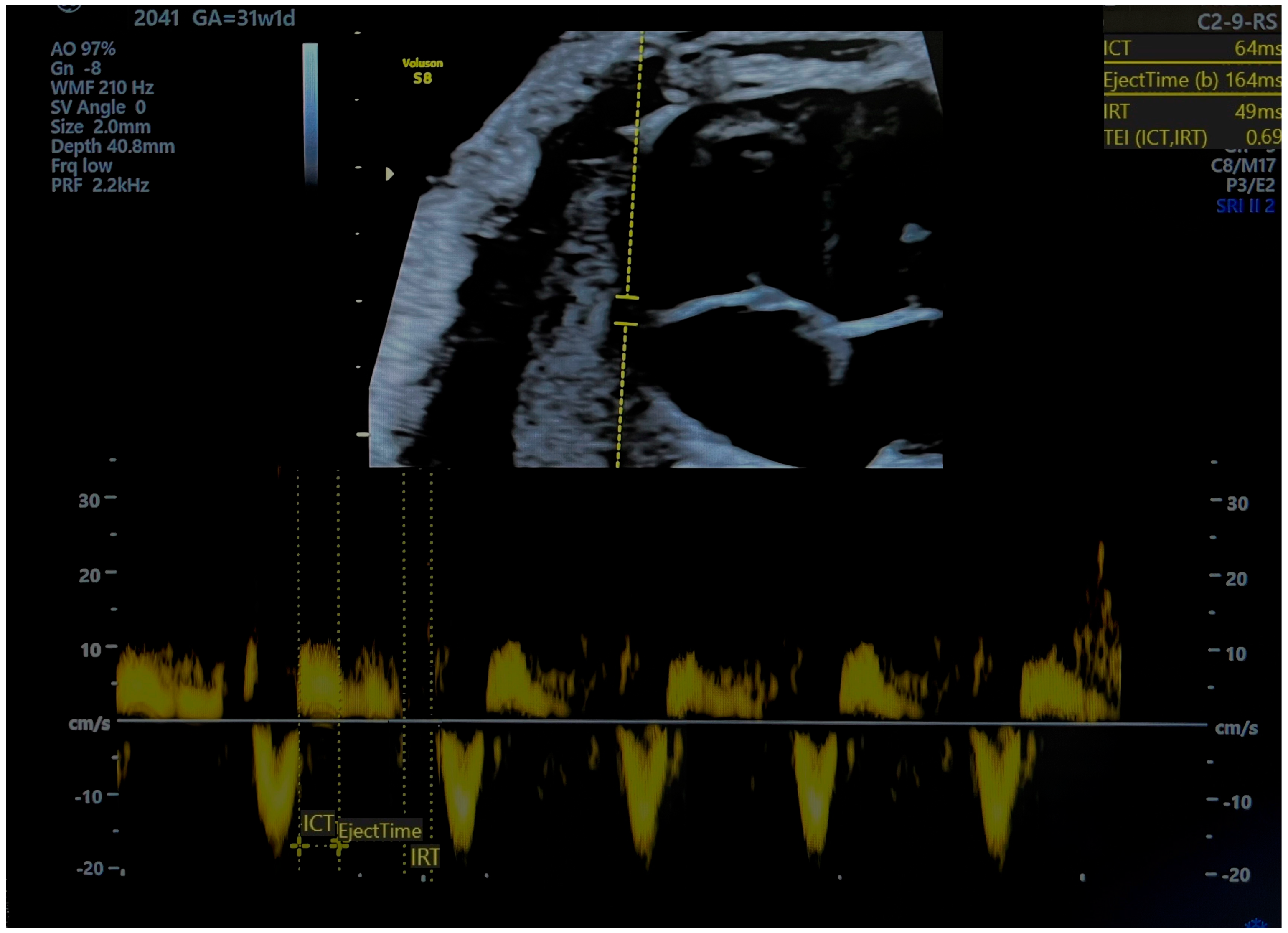
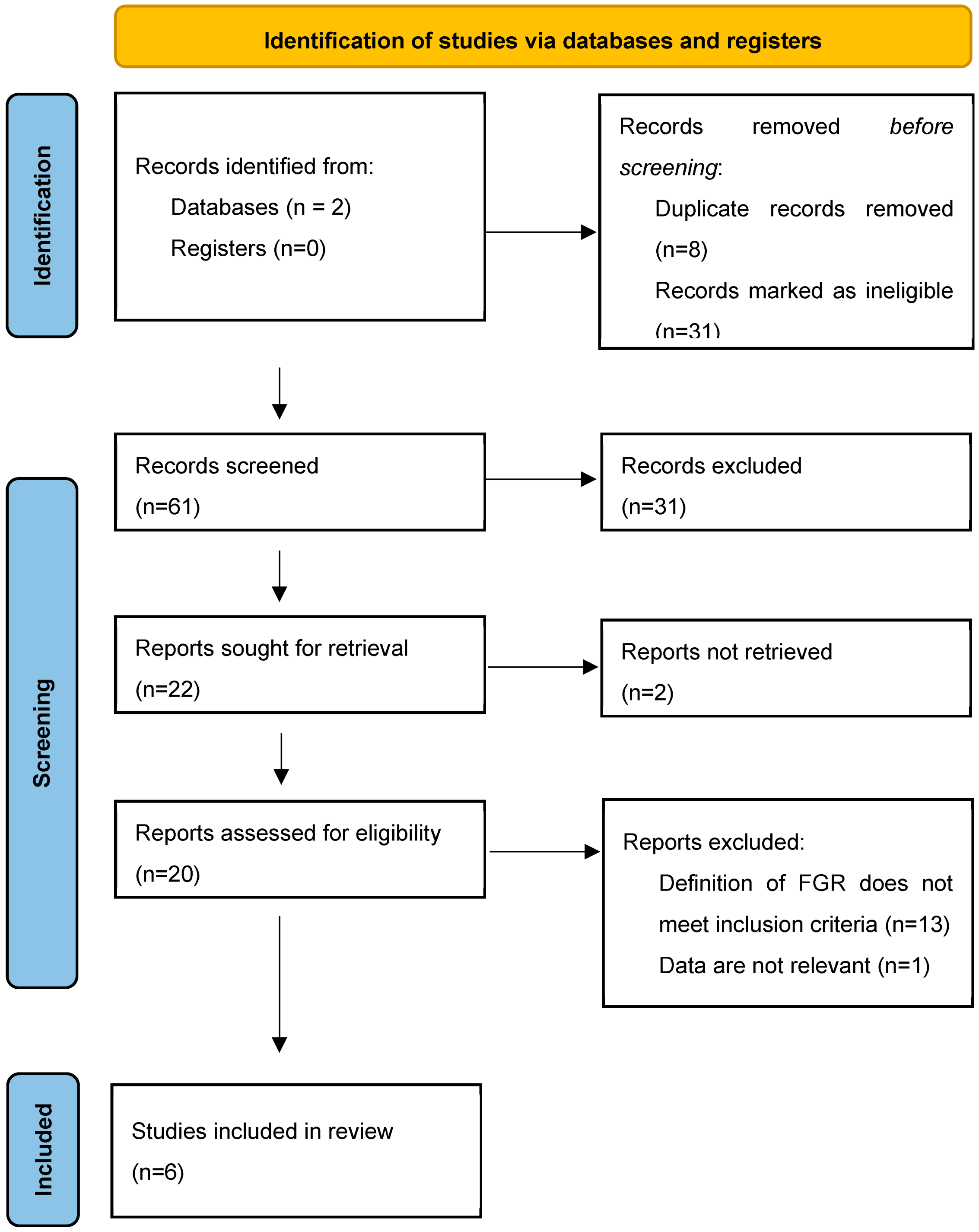
2. Methods
3. Results
4. Discussion
4.1. Main Findings
4.2. Interprettion
4.2.1. Early-Onset FGR
4.2.2. Late-Onset FGR
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Opie, L.H.; Commerford, P.J.; Gersh, B.J.; Pfeffer, M.A. Controversies in ventricular remodelling. Lancet 2006, 367, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Fantasia, I.; Zamagni, G.; Lees, C.; Mylrea-Foley, B.; Monasta, L.; Mullins, E.; Prefumo, F.; Stampalija, T. Current practice in the diagnosis and management of fetal growth restriction: An international survey. Acta Obs. Gynecol. Scand. 2022, 101, 1431–1439. [Google Scholar] [CrossRef] [PubMed]
- Bilardo, C.M.; Hecher, K.; Visser, G.H.A.; Papageorghiou, A.T.; Marlow, N.; Thilaganathan, B.; Van Wassenaer-Leemhuis, A.; Todros, T.; Marsal, K.; Frusca, T.; et al. Severe fetal growth restriction at 26–32 weeks: Key messages from the TRUFFLE study. Ultrasound Obs. Gynecol. 2017, 50, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Figueras, F.; Puerto, B.; Martinez, J.M.; Cararach, V.; Vanrell, J.A. Cardiac function monitoring of fetuses with growth restriction. Eur. J. Obs. Gynecol. Reprod. Biol. 2003, 110, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Han, J.; Zhang, N.; Li, Z.; Wang, J.; Xuan, Y.; Kagan, K.O.; Wu, Q.; Sun, L. Assessment of fetal modified myocardial performance index in early-onset and late-onset fetal growth restriction. Echocardiography 2019, 36, 1159–1164. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tei, C. New non-invasive index for combined systolic and diastolic ventricular function. J. Cardiol. 1995, 26, 135–136. [Google Scholar] [PubMed]
- Nair, A.; Radhakrishnan, S. Fetal left ventricular myocardial performance index: Defining normal values for Indian population and a review of literature. Ann. Pediatr. Cardiol. 2016, 9, 132–136. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hernandez-Andrade, E.; Figueroa-Diesel, H.; Kottman, C.; Illanes, S.; Arraztoa, J.; Acosta-Rojas, R.; Gratacós, E. Gestational-age-adjusted reference values for the modified myocardial performance index for evaluation of fetal left cardiac function. Ultrasound Obs. Gynecol. 2007, 29, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Cruz, M.; Cruz-Lemini, M.; Fernandez, M.T.; Parra, J.A.; Bartrons, J.; Gómez-Roig, M.D.; Crispi, F.; Gratacós, E. Fetal cardiac function in late-onset intrauterine growth restriction vs. small-for-gestational age, as defined by estimated fetal weight, cerebroplacental ratio and uterine artery Doppler. Ultrasound Obs. Gynecol. 2015, 46, 465–471. [Google Scholar] [CrossRef]
- Cruz-Martinez, R.; Figueras, F.; Benavides-Serralde, A.; Crispi, F.; Hernandez-Andrade, E.; Gratacós, E. Sequence of changes in myocardial performance index in relation to aortic isthmus and ductus venous Doppler in fetuses with early-onset intrauterine growth restriction. Ultrasound Obstet. Gynecol. 2011, 38, 170–184. [Google Scholar]
- Palalioglu, R.M.; Erbiyik, H.I.; Kaya, B.; Kiyak, H.; Gedikbasi, A. Investigation of fetal cardiac function using tissue doppler imaging in fetuses compromised by growth restriction. Ginekol. Pol. 2021, 92, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Figueras, F.; Gratacós, E. Update on the diagnosis and classification of fetal growth restriction and proposal of a stage-based management protocol. Fetal Diagn. Ther. 2014, 36, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Kaya, B.; Tayyar, A.; Afar, D.K.; Kaya, S. Comparison of fetal cardiac functions between small-for-gestational age fetuses and late-onset growth-restricted fetuses. J. Perinat. Med. 2019, 47, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Lemini, M.; Crispi, F.; Van Mieghem, T.; Pedraza, D.; Cruz-Martínez, R.; Acosta-Rojas, R.; Figueras, F.; Parra-Cordero, M.; Deprest, J.; Gratacós, E. Risk of perinatal death in early-onset intrauterine growth restriction according to gestational age and cardiovascular Doppler indices: A multicenter study. Fetal Diagn. Ther. 2012, 32, 116–122. [Google Scholar] [CrossRef]
- Hernandez-Andrade, E.; Crispi, F.; Benavides-Serralde, J.; Plasencia, W.; Diesel, H.; Eixarch, E.; Acosta-Rojas, R.; Figueras, F.; Nicolaides, K.; Gratacós, E. Contribution of the myocardial performance index and aortic isthmus blood flow index to predicting mortality in preterm growth-restricted fetuses. Ultrasound Obs. Gynecol. 2009, 34, 430–436. [Google Scholar] [CrossRef]
- Bhorat, I.; Bagratee, J.; Pillay, M.; Reddy, T. Determination of the myocardial performance index in deteriorating grades of intrauterine growth restriction and its link to adverse outcomes. Prenat. Diagn. 2015, 35, 266–273. [Google Scholar] [CrossRef]
- Gordijn, S.J.; Beune, I.M.; Thilaganathan, B.; Papageorghiou, A.; Baschat, A.A.; Baker, P.N.; Silver, R.M.; Wynia, K.; Ganzevoort, W. Consensus definition of fetal growth restriction: A Delphi procedure. Ultrasound Obs. Gynecol. 2016, 48, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.; Buyon, J.; Kim, M.; Glickstein, J.S. Fetal cardiac function assessed by Doppler myocardial performance index (Tei Index). Ultrasound Obs. Gynecol. 2003, 21, 33–36. [Google Scholar] [CrossRef]
- Crispi, F.; Gratacós, E. Fetal cardiac function: Technical considerations and potential research and clinical applications. Fetal Diagn. Ther. 2012, 32, 47–64. [Google Scholar] [CrossRef] [PubMed]
- Comas, M.; Crispi, F.; Cruz-Martinez, R.; Martinez, J.M.; Figueras, F.; Gratacós, E. Usefulness of myocardial tissue Doppler vs. conventional echocardiography in the evaluation of cardiac dysfunction in early-onset intrauterine growth restriction. Am. J. Obs. Gynecol. 2010, 203, 45.E1–45.E7. [Google Scholar] [CrossRef] [PubMed]
- Bligard, K.H.; Doering, M.; Porat, S.; Rosenbloom, J.I. Reference Ranges for Left Modified Myocardial Performance Index: Systematic Review and Meta-Analysis. Fetal Diagn. Ther. 2024, 51, 159–167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Şimşek, A.; Köse, S. Modified Myocardial Performance Index in Fetal Growth Disturbances as Diagnostic and Prognostic Adjunct. Anatol. J. Cardiol. 2023, 27, 34–40. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Reference | Group Studied | Gestational Age | Inclusion Criteria | Exclusion Criteria | MPI Used | Pulse Doppler Parameters Studied | Perinatal Outcomes Studied | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Palalioglu et al. (2021) [11] | EO-FGR (30) controls (46) | 24–34 weeks | EFW < 3rd pc, or EFW < 10th pc with UA PI > 95th pc and/or CPR < 5th pc and/or mean UtA-PI > 95th pc | multiple pregnancies, fetal structural or chromosomal anomaly, diabetes, cholestasis, preeclampsia, FGR diagnosis below the viability limit, early membrane rupture, oligohydramnios, fetal heart complication, or any maternal medical illness | TDI/RMPI | UA PI, UA PI pc, MCA PI, MCA PI pc, CPR, CPR pc, DV PI, DV PI pc, UtA PI, UtA PI pc | GA at delivery, birth weight, 1 min Apgar score, 5 min Apgar score, umbilical artery pH, duration of NICU hospitalization |
|
| Kaya et al. (2019) [14] | LO-FGR (40) SGA (40) controls (40) | 34–37 weeks | EFW < 3rd pc, or EFW < 10th pc with UA PI > 95th pc and/or cerebroplacental ratio (CPR) < 5th pc and/or mean UtA-PI > 95th pc. SGA was defined as an EFW between 3rd and 9th pc with normal Doppler indices. | multiple pregnancies, fetal structural or chromosomal anomaly, fetal infection, presence of fetal arrhythmia or non-reassuring fetal heart rate pattern, presence of maternal comorbidities (chronic hypertension, preeclampsia, diabetes mellitus, chronic renal disease), maternal tobacco use | TDI/RMPI | UA PI, MCA PI, CPR, DV PI, UtA PI | interval between diagnosis and delivery, GA at delivery, birth weight, 1 min Apgar score, 5 min Apgar score, umbilical artery pH, NICU stay >14 days |
|
| Perez-Cruz et al. (2015) [9] | LO-FGR (150) SGA (59) controls (150) | Delivery >34 weeks | EFW < 3rd pc, or EFW < 10th pc with cerebroplacental ratio (CPR) < 5th pc and/or mean UtA-PI > 95th pc. SGA was defined as an EFW between 3rd and 9th pc with normal Doppler indices. | fetal structural or chromosomal anomalies, fetal infection, gestational diabetes, multiple pregnancy, IVF, or ICSI pregnancies | TDI and SD/RMPI, LMPI, septal MPI | UA PI, MCA PI, CPR, DV PI, UtA PI | GA at delivery, birth weight, birth weight percentile, 5 min Apgar score < 8, umbilical artery pH, cord blood glucose, NICU stay >14 days, morbidity *, mortality |
|
| Cruz-Lemini et al. (2012) [15] | EO-FGR (157) | delivery or death <34 weeks | EFW < 10th and UA-PI > 95th pc | twin pregnancies, fetal structural or chromosomal abnormalities, birth weight >10th percentile, fetal infection | SD/LMPI | UA PI, MCA PI, DV PI, AoI IFI | GA at delivery, birth weight, 5 min Apgar score, umbilical cord arterial pH |
|
| Cruz-Martinez et al. (2011) [10] | EO-FGR (115) | Delivery <34 weeks | EFW < 10th and UA-PI > 95th pc | congenital malformations and chromosomal abnormalities, birth weight >10th percentile | SD/LMPI | UA PI, DV PI, AoI PI | not applicable |
|
| Hernandez-Andrade et al. (2009) [8] | EO-FGR (97) | delivery or death between 24 and 34 weeks | EFW < 10th and UA-PI > 95th pc | fetal structural or chromosomal abnormalities, fetal infection, birth weight >10th percentile | SD/LMPI | UA PI MCA PI DV PI AoI IFI | GA at delivery, birth weight, birth weight percentile, 5 min Apgar score <7, umbilical artery pH < 7.2, days in NICU, perinatal death, bronchopulmonary dysplasia, intraventricular hemorrhage III–IV, necrotizing enterocolitis, adverse outcome |
|
| Early-Onset FGR | Late-Onset FGR |
|---|---|
| RMPI TDI Values: Average 0.36 (0.28–0.44). Normal RMPI cut-off: 0.47 and below. | RMPI TDI Values:
|
| Timing: MPI alters before AoI and DV by 26, 12, and 5 days before delivery, respectively, which means that diastolic dysfunction occur prior to hypoxia. | Timing: MPI becomes altered before AoI and DV flow, which means that diastolic dysfunction occurs prior to hypoxia. |
Cardiac Impairment:
| Cardiac Impairment:
|
Predictive Value:
| Predictive Value: A proportion of fetuses classified as SGA have increased MPI values; therefore, these fetuses may suffer true growth restriction, and the MPI becomes altered before changes in the blood flow reach cut-off values for FGR. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czapska, A.H.; Kosińska-Kaczyńska, K. The Significance of the Myocardial Performance Index and Fetal Doppler Abnormalities in Growth-Restricted Fetuses: A Systematic Review of the Literature. J. Clin. Med. 2024, 13, 6469. https://doi.org/10.3390/jcm13216469
Czapska AH, Kosińska-Kaczyńska K. The Significance of the Myocardial Performance Index and Fetal Doppler Abnormalities in Growth-Restricted Fetuses: A Systematic Review of the Literature. Journal of Clinical Medicine. 2024; 13(21):6469. https://doi.org/10.3390/jcm13216469
Chicago/Turabian StyleCzapska, Agnieszka Helena, and Katarzyna Kosińska-Kaczyńska. 2024. "The Significance of the Myocardial Performance Index and Fetal Doppler Abnormalities in Growth-Restricted Fetuses: A Systematic Review of the Literature" Journal of Clinical Medicine 13, no. 21: 6469. https://doi.org/10.3390/jcm13216469
APA StyleCzapska, A. H., & Kosińska-Kaczyńska, K. (2024). The Significance of the Myocardial Performance Index and Fetal Doppler Abnormalities in Growth-Restricted Fetuses: A Systematic Review of the Literature. Journal of Clinical Medicine, 13(21), 6469. https://doi.org/10.3390/jcm13216469






