The Efficacy and Outcomes of Renal Replacement Therapy in Pediatric Metabolic Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Pre-Dialysis Medical Treatment
2.3. Dialysis Modalities and Implementation Protocols
2.3.1. Hemodialysis
2.3.2. Peritoneal Dialysis
2.4. Vascular Access
2.5. Analysis
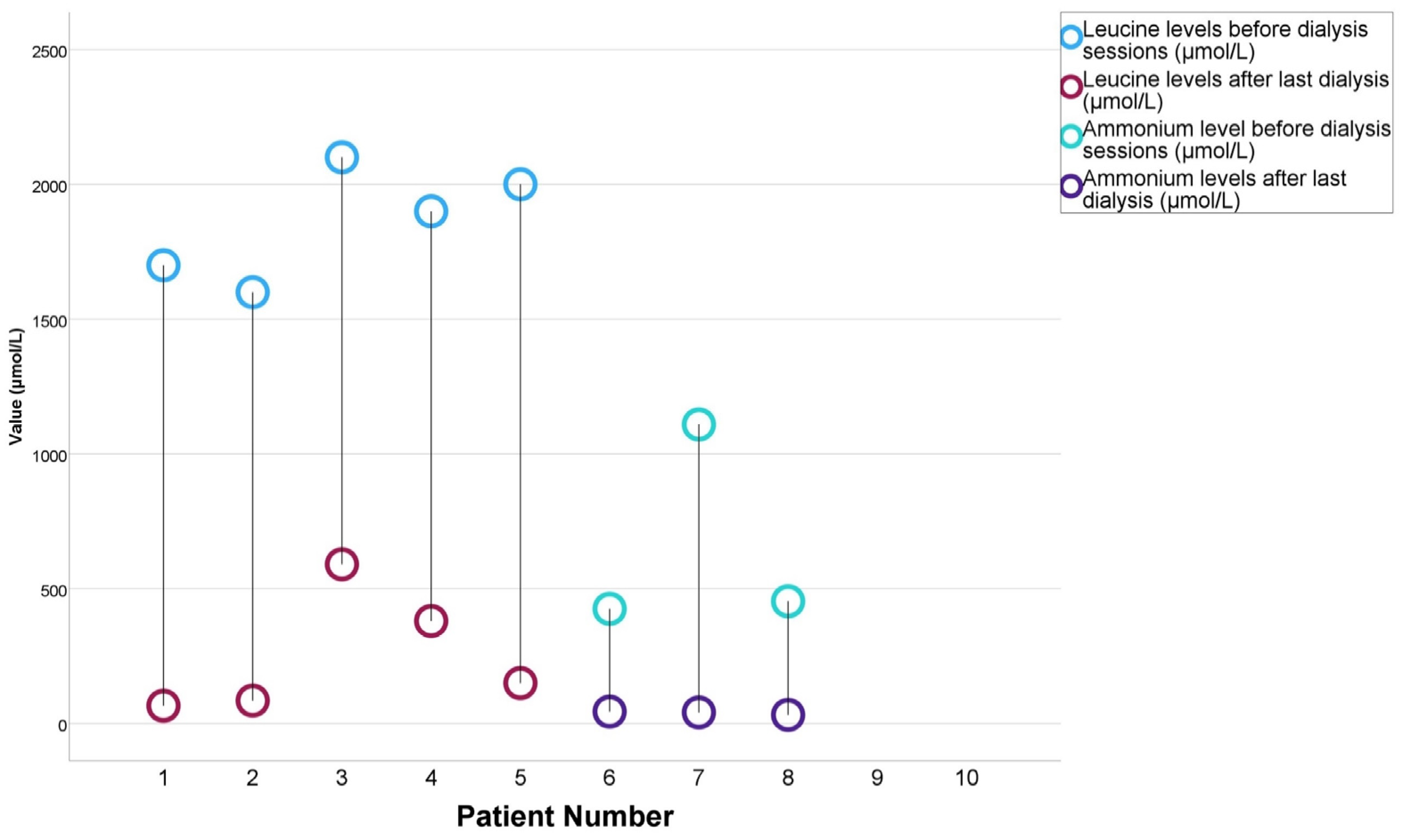
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferreira, C.R.; van Karnebeek, C.D.M. Inborn errors of metabolism. Handb. Clin. Neurol. 2019, 162, 449–481. [Google Scholar] [PubMed]
- Saudubray, J.M.; Garcia-Cazorla, À. Inborn Errors of Metabolism Overview: Pathophysiology, Manifestations, Evaluation, and Management. Pediatr. Clin. N. Am. 2018, 65, 179–208. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, U. Inborn Errors of Metabolism-Approach to Diagnosis and Management in Neonates. Indian J. Pediatr. 2021, 88, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, A.N.; Gallagher, R.C.; Wang, Y.; Currier, R.J.; Amatuni, G.; Bassaganyas, L.; Chen, F.; Kundu, K.; Kvale, M.; Brenner, S.E.; et al. The role of exome sequencing in newborn screening for inborn errors of metabolism. Nat. Med. 2020, 26, 1392–1397. [Google Scholar] [CrossRef] [PubMed]
- Altun, I.; Kiykim, A.; Zubarioglu, T.; Burtecene, N.; Hopurcuoglu, D.; Topcu, B.; Cansever, M.S.; Kiykim, E.; Cokugras, H.C.; Zeybek, A.C.A. Altered immune response in organic acidemia. Pediatr. Int. 2022, 64, e15082. [Google Scholar] [CrossRef]
- Guilder, L.L.; Kronick, J.B. Organic Acidemias. Pediatr. Rev. 2022, 43, 123–134. [Google Scholar] [CrossRef]
- Blackburn, P.R.; Gass, J.M.; Vairo, F.P.E.; Farnham, K.M.; Atwal, H.K.; Macklin, S.; Klee, E.W.; Atwal, P.S. Maple syrup urine disease: Mechanisms and management. Appl. Clin. Genet. 2017, 10, 57–66. [Google Scholar] [CrossRef]
- Deon, M.; Guerreiro, G.; Girardi, J.; Ribas, G.; Vargas, C.R. Treatment of maple syrup urine disease: Benefits, risks, and challenges of liver transplantation. Int. J. Dev. Neurosci. 2023, 83, 489–504. [Google Scholar] [CrossRef]
- Zelei, T.; Kovács, S.; Finn, P.; Nagy, D.; Sikirica, V.; Carlson, K.B.; Vokó, Z. Systematic literature review of the epidemiology of glycogen storage disease type 1a. J. Pediatr. Endocrinol. Metab. 2023, 36, 809–817. [Google Scholar] [CrossRef]
- Ramoser, G.; Caferri, F.; Radlinger, B.; Brunner-Krainz, M.; Herbst, S.; Huemer, M.; Hufgard-Leitner, M.; Kircher, S.G.; Konstantopoulou, V.; Löscher, W.; et al. 100 years of inherited metabolic disorders in Austria-A national registry of minimal birth prevalence, diagnosis, and clinical outcome of inborn errors of metabolism in Austria between 1921 and 2021. J. Inherit. Metab. Dis. 2022, 45, 144–156. [Google Scholar] [CrossRef]
- Slagle, C.; Askenazi, D.; Starr, M. Recent Advances in Kidney Replacement Therapy in Infants: A Review. Am. J. Kidney Dis. 2024, 83, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Ranchin, B.; Plaisant, F.; Demède, D.; de Guillebon, J.M.; Javouhey, E.; Bacchetta, J. Review: Neonatal dialysis is technically feasible but ethical and global issues need to be addressed. Acta Paediatr. 2021, 110, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Strauss, K.A.; Carson, V.J.; Soltys, K.; Young, M.E.; Bowser, L.E.; Puffenberger, E.G.; Brigatti, K.W.; Williams, K.B.; Robinson, D.L.; Morton, D.H.; et al. Branched-chain α-ketoacid dehydrogenase deficiency (maple syrup urine disease): Treatment, biomarkers, and outcomes. Mol. Genet. Metab. 2020, 129, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Li, F.; Zhou, J.; Liu, X.; Peng, J.; Gong, L. Neonatal maple syrup urine disease case report and literature review. Medicine 2022, 101, e32174. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Lu, D.; Xu, F.; Ji, W.; Zhan, X.; Gao, X.; Qiu, W.; Zhang, H.; Liang, L.; Gu, X.; et al. Newborn screening of maple syrup urine disease and the effect of early diagnosis. Clin. Chim. Acta 2023, 548, 117483. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, R.; Rajendran, S.; Arunkumar, S.; Karthik Narayanan, R.; Yadav, R. Continuous Venovenous Hemodiafilteration for Extremely High Ammonia Levels in Methyl Malonic Acidemia. Indian J. Pediatr. 2021, 88, 272–273. [Google Scholar] [CrossRef]
- Gabbi, P.; Nogueira, V.; Haupental, F.; Rodrigues, F.S.; Nascimento, P.S.D.; Barbosa, S.; Arend, J.; Furian, A.F.; Oliveira, M.S.; dos Santos, A.R.S.; et al. Ammonia role in glial dysfunction in methylmalonic acidemia. Toxicol. Lett. 2018, 295, 237–248. [Google Scholar] [CrossRef]
- Siegel, C.; Arnon, R.; Florman, S.; Bucuvalas, J.; Oishi, K. Nutritional Management and Biochemical Outcomes during the Immediate Phase after Liver Transplant for Methylmalonic Acidemia. Nutrients 2020, 12, 2976. [Google Scholar] [CrossRef]
- Hannah, W.B.; Derks, T.G.J.; Drumm, M.L.; Grünert, S.C.; Kishnani, P.S.; Vissing, J. Glycogen storage diseases. Nat. Rev. Dis. Primers 2023, 9, 46. [Google Scholar] [CrossRef]
- Gümüş, E.; Özen, H. Glycogen storage diseases: An update. World J. Gastroenterol. 2023, 29, 3932–3963. [Google Scholar] [CrossRef]
- Wright, T.L.F.; Umaña, L.A.; Ramirez, C.M. Update on glycogen storage disease: Primary hepatic involvement. Curr. Opin. Pediatr. 2022, 34, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Porta, F.; Peruzzi, L.; Bonaudo, R.; Pieretti, S.; Busso, M.; Cocchi, E.; Conio, A.; Pagliardini, V.; Spada, M. Differential response to renal replacement therapy in neonatal-onset inborn errors of metabolism. Nephrology 2018, 23, 957–961. [Google Scholar] [CrossRef] [PubMed]
- Eisenstein, I.; Pollack, S.; Hadash, A.; Eytan, D.; Attias, O.; Halberthal, M.; Ben-Ari, J.; Bar-Joseph, G.; Zelikovic, I.; Mandel, H.; et al. Acute hemodialysis therapy in neonates with inborn errors of metabolism. Pediatr. Nephrol. 2022, 37, 2725–2732. [Google Scholar] [CrossRef] [PubMed]
- Celik, M.; Akdeniz, O.; Ozgun, N.; Ipek, M.S.; Ozbek, M.N. Short-term results of continuous venovenous haemodiafiltration versus peritoneal dialysis in 40 neonates with inborn errors of metabolism. Eur. J. Pediatr. 2019, 178, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Aygun, F.; Aygun, D.; Erbek Alp, F.; Zubarıoglu, T.; Zeybek, C.; Cam, H. The impact of continuous renal replacement therapy for metabolic disorders in infants. Pediatr. Neonatol. 2018, 59, 85–90. [Google Scholar] [CrossRef]
- Arbeiter, A.K.; Kranz, B.; Wingen, A.M.; Bonzel, K.-E.; Dohna-Schwake, C.; Hanssler, L.; Neudorf, U.; Hoyer, P.F.; Büscher, R. Continuous venovenous haemodialysis (CVVHD) and continuous peritoneal dialysis (CPD) in the acute management of 21 children with inborn errors of metabolism. Nephrol. Dial. Transplant. 2010, 25, 1257–1265. [Google Scholar] [CrossRef]
| Characteristic | N (%)/Median (IQR) | |
|---|---|---|
| Sex | Female | 8 (80%) |
| Male | 2 (20%) | |
| Etiology | MSUD | 5 (50%) |
| MMA | 3 (30%) | |
| GSD | 2 (20%) | |
| Age (days) | 637.5 (3.75–4148.75) | |
| Weight (kg) | 9.75 (3.23–18) | |
| Long-term Survival | 6 (60%) | |
| Patients | Sex | Etiology | Weight (kg) | Dialysis Type | Dialysis Initiation Day | Dialysis Indication | Age at Dialysis (Days) | Number of Dialysis Sessions |
|---|---|---|---|---|---|---|---|---|
| P1 | M | MSUD | 48 | HD | 1 | High leucine + Encephalopathy | 5260 | 8 |
| P2 | F | MSUD | 4.2 | PD | 10 | Seizure + Encephalopathy | 10 | 3 |
| P3 | F | MSUD | 2.4 | PD | 3 | High leucine + Kidney failure | 3 | 12 |
| P4 | F | MSUD | 1.51 | PD | 4 | High leucine | 4 | 10 |
| P5 | F | MSUD | 3.5 | PD | 2 | High leucine | 2 | 3 |
| P6 | M | MMA | 7.5 | HD | 2 | Encephalopathy + Septic shock + Kidney failure | 455 | 3 |
| P7 | F | MMA | 17 | HD | 1 | Seizure + Septic shock | 820 | 4 |
| P8 | F | MMA | 21 | HD | 3 | Septic shock + Kidney failure | 4745 | 2 |
| P9 | F | GSD (T1) | 12 | HD | 3 | Metabolic crisis | 3950 | 3 |
| P10 | F | GSD (FBS) | 15 | HD | 2 | Metabolic crisis | 3285 | 5 |
| Characteristic | Hemodialysis (n = 6) | Peritoneal Dialysis (n = 4) | p |
|---|---|---|---|
| Age (days), median (IQR) | 3617.5 (728.75–4873.75) | 3.5 (2.25–8.5) | 0.01 |
| Sex (female), N (%) | 4 (66.7%) | 4 (100%) | |
| Weight (kg), median (IQR) | 16 (10.88–27.75) | 2.95 (1.73–4.03) | 0.01 |
| Etiology, N (%) | |||
| MSUD | 1 (16.7%) | 4 (100%) | |
| MMA | 3 (50%) | 0 (0%) | |
| GSD | 2 (33.3%) | 0 (0%) | |
| First dialysis day, median (IQR) | 2 (1–3) | 3.5 (2.25–8.5) | 0.114 |
| Number of dialysis sessions, median (IQR) | 3.5 (2.75–5.75) | 6.5 (3–11.5) | 0.476 |
| Toxin reduction (%), median (IQR) | 94.5 (90.4–96.2) | 86 (73.3–93.5) | 0.200 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Önal, H.G.; Nalçacıoğlu, H.; Özer, I.; Karalı, D.T. The Efficacy and Outcomes of Renal Replacement Therapy in Pediatric Metabolic Disorders. J. Clin. Med. 2024, 13, 6452. https://doi.org/10.3390/jcm13216452
Önal HG, Nalçacıoğlu H, Özer I, Karalı DT. The Efficacy and Outcomes of Renal Replacement Therapy in Pediatric Metabolic Disorders. Journal of Clinical Medicine. 2024; 13(21):6452. https://doi.org/10.3390/jcm13216452
Chicago/Turabian StyleÖnal, Hülya Gözde, Hülya Nalçacıoğlu, Işıl Özer, and Demet Tekcan Karalı. 2024. "The Efficacy and Outcomes of Renal Replacement Therapy in Pediatric Metabolic Disorders" Journal of Clinical Medicine 13, no. 21: 6452. https://doi.org/10.3390/jcm13216452
APA StyleÖnal, H. G., Nalçacıoğlu, H., Özer, I., & Karalı, D. T. (2024). The Efficacy and Outcomes of Renal Replacement Therapy in Pediatric Metabolic Disorders. Journal of Clinical Medicine, 13(21), 6452. https://doi.org/10.3390/jcm13216452






