Abstract
Background: Gait disturbances in children with cerebral palsy can increase the hindrance caused by loss of independence and social engagement. The Lokomat, developed by Hocoma, shows promise as a supplementary tool for gait rehabilitation. This study investigates the impact of Lokomat training on gait parameters and trends observed during training. Methods: A total of 26 children (13 male individuals) with a diagnosis of cerebral palsy (CP), aged 4 to 23 years, were enrolled in the study. Patients participated in a standard comprehensive rehabilitation program with additional Lokomat training sessions. Gait function was assessed using the Timed Up and Go Test (TUG) and the 10 m walking test (10mWT) at the beginning and end of the rehabilitation period. Changes in Lokomat parameters (step number, session duration, speed, body weight support, and guidance force) were also analysed. Results: The median duration of the 10mWT and TUG significantly decreased across the groups after the treatment program. The highest increases were observed for the number of steps taken. Across the entire cohort, the linear trend curves for distance and number of steps exhibited near-perpendicular alignment with the horizontal axis, suggesting significant improvement in these parameters. A consistent trend was noted for speed, with the trend line aligned parallel with the horizontal axis. Decreasing trends were observed for body weight support and guidance force. Conclusions: Therapy with the Lokomat functioning as the active gait orthosis can be used as a form of support to the standard rehabilitation protocol for patients with CP.
1. Introduction
Cerebral palsy (CP) encompasses a spectrum of motor impairment and non-progressive postural syndromes emerging in early childhood [1]. Due to abnormal development or damage to the brain areas responsible for muscle control and coordination [2,3], CP is often associated with movement, posture, and balance issues and co-occurs with sensory, cognitive, communication, and behavioural disorders. Hu et al. [2] demonstrated that CP poses a significant public health challenge and imposes a substantial socioeconomic burden worldwide. Hence, the CP issue affects various disciplines, including paediatrics, neurology, paediatric orthopaedics, rehabilitation medicine, orthopaedics, and genetics [4].
Therapy for patients with CP is a lifelong journey. Koman et al. [1] and Mu et al. [5] highlighted that the primary objective of therapy should be its early initiation to enhance functionality and skills while promoting health in multiple domains, such as locomotor function, cognitive development, social integration, and independence. Management strategies cover a spectrum of approaches, including physiotherapy, occupational therapy, and speech therapy. Such strategies also involve applying orthotics, device-assisted modalities, pharmacological interventions, and orthopaedic or neurosurgical procedures [1,6]. Hu et al. [2] showed that an accurate diagnosis of genetic or metabolic causes is crucial for determining treatment options, accurate prognosis, and counselling for patients with CP. Mu et al. [5] identified three commonly used therapies for children with cerebral palsy: botulinum toxin, constraint-induced movement therapy (CIMT), and acupuncture. Botulinum toxin is frequently employed to relieve spasticity and dystonia, thereby increasing range of motion and functional abilities in children diagnosed with CP [7]. CIMT represents an evolving methodology and promotes greater utilization of affected upper limbs spontaneously while reducing the consequences of acquired disuse [8]. In some regions, e.g., in Asia, acupuncture is widely adopted, purportedly prompting stimulation within the cerebral cortex and peripheral nerves and consequently facilitating reductions in muscle tension [9].
In addition to the previously mentioned therapies, gait therapy has emerged as a crucial element for individuals with CP [10,11]. Advances in robotics and computer technology have stimulated collaboration among engineers, physicians, and physiotherapists to create equipment capable of facilitating therapeutic interventions under dynamic weight support conditions, thereby promoting an independent gait. Among these innovations, the Lokomat is an example of a robotic exoskeleton designed to support gait rehabilitation [12,13]. The scientific underpinning of robot-assisted gait training is rooted in spinal automatism (central pattern generators), central nervous system plasticity, and motor learning [14,15]. Numerous studies have demonstrated the effectiveness of robot-assisted locomotor therapy in improving gait among adult stroke survivors, those with brain or spinal injuries [16,17], and individuals with other neurological conditions, including Parkinson’s disease [18] and multiple sclerosis [19]. In addition, this therapy positively affected postural alignment, cardiovascular health, muscle metabolism, bowel motility, tissue health, and overall quality of life [16]. However, despite these benefits, Pawłowski et al. [13] highlighted the lack of specific guidelines for Lokomat training, noting the absence of consensus on optimal training parameters such as duration, intensity, and patient weight support levels. Meyer-Heim et al. [20] conducted an average of 15.1 ± 4.1 training sessions, during which patients walked an average distance of 842 ± 291 m per session, with each session lasting approximately 31.5 ± 7.1 min. Borggraefe et al. [21] implemented therapy sessions with an average duration of 34 min. The mean walking distance per session was 927 m. Over the course of the 3-week trial, the total walking distance reached 11.129 m. Moreover, the authors reported that body weight unloading initially started at 50% and was gradually reduced to nearly zero over the course of the therapy sessions, without causing significant knee buckling. Additionally, a 50% leading force was applied using the impedance control strategy. Despite these limitations, observational assessments and patient-reported outcomes provide valuable insights into the impact of Lokomat training on functional independence and quality of life for children with cerebral palsy. Some authors [20,21,22,23] have demonstrated the positive effects of Lokomat training on functional capacity levels in CP patients, although they have not explored trends in various parameters recorded by the Lokomat. This study aimed to investigate the influence of Lokomat training on gait parameters and discern trends in the parameters applied and assessed during training.
2. Materials and Methods
2.1. Participants’ Characteristics
This study was conducted in the Park Zdrowia Modern Rehabilitation Centre in Kampinos. The study included 26 ambulatory patients (13 male and 13 female individuals) with CP (Table 1).

Table 1.
Summary of patients’ anthropometric data: mean ± standard deviation, extreme values, and median with quartile distribution.
The inclusion criteria were participant age from 3 to 24 years; diagnosis of cerebral palsy; ability to independently perform the Timed Up and Go test (TUG) and 10 m walk test (10mWT test), including the use of orthopaedic equipment; classification I–III according to the Gross Motor Function Classification System (GMFCS) [24]; understanding of instructions and verbal commands; physical disposition to begin a cycle of sessions on the Lokomat; ability to report any pain or discomfort that might occur during therapy; and no previous experience with the robot-assisted gait training.
Exclusion criteria encompassed conditions that might hinder locomotor training or present physical limitations upon using the robotic device. According to the Lokomat manufacturer’s manual (Hocoma AG, Volketswil, Switzerland), children should be excluded if they have severe lower-extremity muscle contractures (>20° knee extension deficit, >40° hip extension deficit), hip instability/subluxation >45%, received botulinum toxin A injections to lower limbs within the last three months, undergone neurosurgical or orthopedic interventions in the lower limbs within the nine months preceding therapy with Lokomat, an uncontrolled seizure disorder, vascular disorders of the lower limbs or have open skin lesions, or if they are unable to cooperate or be adequately positioned within the Lokomat [25].
The Gross Motor Function Classification System (GMFCS) was used to assess the motor skills of children with CP. The GMFCS consists of five levels, briefly described as follows: Level I—the patient moves without limitations; Level II—the patient moves with some restrictions on uneven surfaces, inclines, and in crowded areas; Level III—the patient walks indoors or outdoors on a level surface with the assistance of a mobility device or manually propels a wheelchair; Level IV—the patient may walk short distances with a walker or increasingly rely on wheeled mobility aids at home and in the community. Those classified at Level V experience significant limitations in antigravity movement, with all areas of motor function being restricted [24].
Consequently, the patients participating in the study were representatives of the following levels: Level I (4 people), Level II (12 people), and Level III (10 people). As per the GMFCS scale, these individuals could walk with or without manual support devices. While six subjects did not require orthopaedic assistance in their daily activities, the majority used assistive devices such as crutches (1 person), a tripod (3 persons), an anterior walker (7 participants), and a posterior walker (9 participants) (Table 1).
2.2. Ethical Approval
The study protocol was approved by the Institutional Review Board of Józef Piłsudski University of Physical Education in Warsaw, Poland (protocol code SKE01-15/2023 and date of approval 24 March 2023). This work was carried out in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study aged over 16 and/or their parents (for patients under 18).
2.3. Devices, Procedures and Outcome Measures
2.3.1. Lokomat Training Sessions
The Lokomat Pro 6 (Hocoma AG, Volketswil, Switzerland) is a driven gait orthosis designed for intensive and repetitive gait therapy, suitable for children and adults (Figure 1). This device comprises an exoskeleton adaptable to individual patients, a dynamic body weight support system, and a treadmill [26]. During the 4-week standard rehabilitation program, the children participated in Lokomat training sessions (Table 1). The duration of Lokomat therapy was capped at 45 min, though the length of training varied based on the patient’s capabilities. Before the first training session of each cycle, the Lokomat, with its orthosis, was adjusted to fit the individual. This adjustment aimed to provide comfortable training conditions, following the manufacturer’s instructions (Hocoma AG, Volketswil, Switzerland). Workout parameters were tailored to each patient’s abilities and progress, ensuring the ability to maintain speed while providing tracking feedback on the screen. The supervising therapist encouraged active participation and proper positioning throughout the sessions.

Figure 1.
The Lokomat Pro 6 (Hocoma AG, Volketswil, Switzerland) (picture provided from the manufacturer’s resources).
The analysis included parameters of training sessions from Lokomat, all defined and stored in the system, enabling comparison over time within a patient. These parameters included (1) session time [min, s]—the duration of a single training session, with a default duration of 45 min. The duration could change depending on the patient’s disposition or fatigue; (2) walking distance [m]—the distance covered during a training session; (3) number of steps—the number of steps during a single training session; (4) body weight support (BWS) [%]—the amount of the offloading of the patient’s body weight; (5) guidance force (GF) [%], which determines the degree to which the patient’s movements are guided by the Lokomat orthoses during walking; and (6) mean walking speed [km/h], which determines the mean velocity of the treadmill, thus influencing the patient’s gait speed. This value is adjustable from 0.5 to 3.2 km/h [26,27].
2.3.2. 10 m Walk Test (10mWT) and Timed Up and Go (TUG) Test
The measurements for the 10 m walk test (10mWT) and Timed Up and Go (TUG) test were taken on both the first and last day of the rehabilitation process, once each, in the following sequence: 10mWT, followed by TUG. Patients rested in a seated position for 3 min between tests. The time of the tests was recorded in seconds with precision to the hundredth of a second, using the Kalenji ON Rhythm 110 (Decathlon, Paris, France) digital stopwatch. Before the test, an experienced therapist provided instructions on conducting the test. Running during tests was not allowed.
The 10 m walk test (10mWT) is a clinical assessment used to measure the time it takes for an individual to walk a distance of 10 m in a straight line. The time was counted from the command “start” until the moment the ten-meter line was crossed.
The Timed Up and Go (TUG) test is a clinical assessment used to evaluate mobility and functional mobility in individuals. At the beginning of the test, the patient sat on a chair with feet on the floor. On the command “start”, the patient raised and covered a distance of 3 m in a straight line, turned and walked back to the chair, and sat down. Both tests are commonly used in rehabilitation to assess changes in walking ability over time or in response to interventions [28,29]. The full protocol is described in Figure 2.

Figure 2.
The study protocol.
2.4. Statistical Analysis
Statistical analysis was performed using Statistica v. 12 (TIBCO Software, Inc., Palo Alto, CA, USA). The threshold for statistical significance was set at p < 0.05. Wilcoxon’s test was used for the 10mWT and TUG results separately in the female and male groups, as well as in the whole group.
The minimum and maximal values for each parameter measured by Lokomat during therapy were exported for each group, i.e., females, males, and the entire cohort. Wilcoxon’s test was then applied to assess the statistical significance of these values. Additionally, the percentage increase or decrease resulting from Lokomat training in each parameter was calculated, thus elucidating its effect.
The last step involved the trend analysis. A time progress curve was plotted for each Lokomat parameter for each individual separately. Following this, a linear trend function of the form f(x) = ax + b was determined, where a represents the directional coefficient, indicating the slope of the line, and b represents the y-intercept [30]. The directional coefficient of the function equals the tangent of the angle (alpha) formed by the slope of the function’s graph with the abscissa (horizontal) axis. Thus, a = tan (alpha). Calculating the angle of alpha (alpha = arctan (a)) made it possible to show what the trend was, i.e., increasing (if the values of the angle were positive) or decreasing (if the values of the angle were negative), and how strong the trend was (the bigger the alpha, the faster the line goes up) (Figure 3).
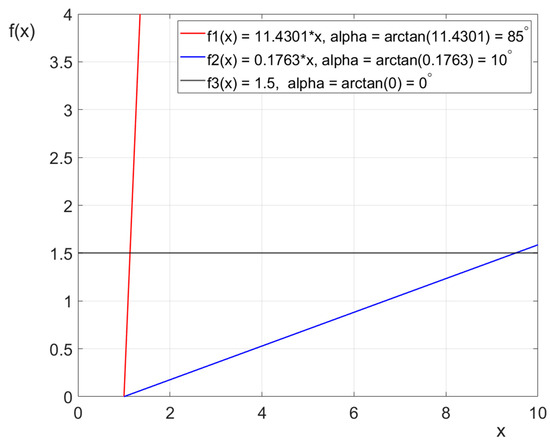
Figure 3.
An example of three linear trend functions without free expression demonstrates how the slope of their graphs changes based on the value of the directional coefficient.
3. Results
3.1. 10 m Walk Test (10mWT) and Timed Up and Go (TUG) Test
The median duration of the 10 m walk test significantly (p = 0.001) decreased in the whole group and in the male and female groups by 1.12 s (~4.99%), 2.81 s (~11.3%), and 0.76 s (~4%), respectively. The median duration of the TUG test decreased significantly in all the above-mentioned groups by 1.67 s (~4.01%), 0.06 s (~0.16%), and 3.61 s (~7.97%). The results of the 10mWT and TUG are presented in Table 2.

Table 2.
Summary of TUG and 10mWT test results (median with quartile distribution) before and after therapy with the robot-assisted Lokomat orthosis in the whole group, the male group, and the female group, separately.
3.2. Persistent Trends in Lokomat Therapy
The analysis covered six Lokomat parameters, capturing their minimum and maximum values (Table 3). Across all subjects, a consistent pattern emerged. Typically, the minimum values were achieved during the initial training session, while the maximum values were consistently observed during the final or one of the penultimate meetings. This trend was the opposite for the body weight support and guidance force values.

Table 3.
Median with quartile distribution of minimum and maximum parameter values exported from Lokomat sessions during therapy with Lokomat robot-assisted orthosis, analyzed separately for the whole group, the male group, and the female group.
Examining the difference between the median of the minimum and maximum values, it is evident that within the female group, the smallest increase occurred in session time, registering at 1.73%. The situation was similar in the male group (3.45%) and the entire cohort (2.48%). The highest increases, amounting to 61.86% and 41.94%, were observed in the male group and the entire cohort, respectively, for the number of steps taken. Notably, the median percentage of body weight support decreased by 42.91% in the male group, 39.24% in the female group, and 40.59% across the entire group.
The findings outlined in Table 4 support the preceding analysis (Table 3). Across the male group, the female group, and the entire cohort, the linear trend curves for distance and number of steps exhibited near perpendicular alignment with the horizontal axis. This alignment suggests significant improvement in these parameters, with values showing a consistent upward trend, as evidenced by the positivity and high magnitude of values in both the first and third quartile. In contrast, a consistent trend was noted for speed, with the trend line aligned parallel with the horizontal axis. The median slope angle of the trend line ranged from 1.6° in the female group to 1.92° in the male group. Decreasing trends were observed for body weight support and guidance force. The slope angles of the trend lines for body weight support averaged between −12.52° for females and −13.93° for males. Similarly, guidance force exhibited a monotonic decline, with median slope angles of −30.75° for males and −35.75° for females.

Table 4.
Median with quartile distribution of the slope angle of the linear trend curve for parameters exported from Lokomat sessions during therapy with the Lokomat robot-assisted orthosis, analyzed separately for the whole group as well as male and female individuals.
4. Discussion
This study aimed to examine the impact of Lokomat training on gait parameters and identify trends in the parameters used and evaluated during training. The study comprised 13 male and 13 female individuals, all exhibiting similar levels on the GMFCS scale. Within both groups, two individuals were classified at Level I, six at Level II, and five at Level III. Although the male group was older, taller, and heavier, and male individuals also used different number of walking aids compared to the girls (anterior walker (male individuals: 5, female individuals: 2), a tripod (male: 1, females: 2), crutches (male: 1, female: 0), a posterior walker (male individuals: 3, female individuals: 6), and no walking aid (male individuals: 3, female individuals: 3), there were no other significant differences between the groups in the study results. Therefore, the subsequent discussion will be concerned with the entire group’s results.
The results of the 10mWT and TUG tests revealed significant decreases following Lokomat therapy, with an approximately 4.99% decline in the 10mWT and a 4.01% decline in the TUG for the entire group. These findings are consistent with those reported in previous studies [13,20,21,31,32], although the decrease in values observed in the cited studies was notably higher. Likewise, the values for both the pre- and post-therapy tests were considerably lower in the cited papers than in the present study, suggesting that the subjects in those studies exhibited faster performance.
According to van Dellen and Labruyère [11], Lokomat therapy seems to be equally as effective as standard therapy approaches such as over-ground walking or manual treadmill therapy. One reason for this might be that the most commonly adjusted parameters—including the regulation of gait speed, the amount of unloading (referred to as body weight support), and a scaling factor for the force field that maintains the legs on the desired spatiotemporal trajectory (referred to as guidance force)—are not optimally used [33]. Talaty and Esquenazi [34] similarly underscore the importance of in-hospital rehabilitation for patients following an acute stroke. They highlight that both Lokomat and conventional gait training (CGT) significantly enhance functional outcomes as evidenced by improvements in measures such as the Functional Independence Measure and the 10 m walk test. The authors showed that the CGT group benefited from a greater number of therapy sessions than the Lokomat group. This suggests that while both interventions are effective, Lokomat may provide a more efficient approach to gait retraining by delivering a higher therapeutic “dose” despite requiring fewer sessions.
In the present study, the consistent trend was for speed, with the trend line aligned almost parallel with the horizontal axis. The slope angle of the trend line was low, measuring 1.79° across the whole group. However, the median speed during Lokomat training increased by only 25%. Koenig et al. [35] demonstrated that increasing gait speed raises the heart rate, thus intensifying therapy. Moreover, van Kammen et al. [36] showed that increasing gait speed in patients with cerebral palsy enhances muscle activation. Nevertheless, some evidence supports reducing walking speed to activate supra spinal centres [37,38]. Van Dellen and Labruyère [11] conducted a comprehensive review revealing diverse strategies for body weight support. Most studies maintained weight support below 50% [39,40,41], while others consistently kept it at or above this threshold [42,43,44]. In the present investigation, body weight support initially had median value 64.11%, decreasing to 45.6% by therapy’s end. Notably, existing evidence underscores that reducing body weight support can heighten metabolic costs [45] and elevate heart rates [35], attributed to increased muscle activation [36,43,44]. The setting of guidance force represents the final parameter adjusted during training sessions. While some therapists advocate for minimizing robot–patient interactions, favouring a low guidance force [42], others advocate resistance training with the Lokomat [31,46]. In the present study, the guidance force had a consistent decline, with median slope angles of −33.43°. This downward trend resulted in a notable 23.89% difference between initial and final values. Studies by van Kammen et al. [36,47], demonstrated that reducing guidance force can heighten muscle activation. Similarly, Krishnan et al. [42] showed that during trajectory tracking tasks in the Lokomat, employing a low guidance force can enhance muscle activation and diminish tracking errors.
The last that should be discussed is the number of steps and distance covered during the Lokomat training. In the present study, the linear trend curves for distance and number of steps displayed nearly perpendicular alignment to the horizontal axis, measuring at 87.78° and 88.74°, respectively. This alignment strongly indicates significant enhancements in these metrics, with values consistently trending upward. This notion is supported by a substantial 39.38% increase in distance covered and a 41.94% increase in the number of steps observed after the rehabilitation treatment. These findings not only highlight the effectiveness of Lokomat training in promoting increased mobility but also emphasize the potential of this therapy to facilitate meaningful improvements in gait parameters for children with cerebral palsy.
This study has some limitations that should be mentioned. Firstly, the study did not include a control group, which would have allowed for a more robust comparison between Lokomat therapy and standard rehabilitation approaches. Without a control group, it is challenging to attribute the observed improvements solely to Lokomat therapy, as other factors, such as natural progression or concurrent therapies, could also have contributed to the outcomes. It must be pointed out that it was not possible to blind the study due to the nature of Lokomat training. The second limitation of this study is the relatively small sample size, which may have limited the generalizability of the findings. This study included 26 children affected by cerebral palsy with different ages and GMFCS levels, which, while sufficient for an exploratory investigation, may not fully capture the diversity of responses to Lokomat therapy across different demographic and clinical profiles. Furthermore, the study duration was limited to a 4-week rehabilitation program, which may not capture the full extent of long-term effects or potential plateauing of benefits over time. Future studies with larger sample sizes, randomized controlled designs, and longer follow-up periods would provide more definitive insights into the efficacy and optimal parameters of Lokomat therapy for children with cerebral palsy.
5. Conclusions
This study identified a consistent trend of increasing gait speed during therapy, albeit at a modest rate. While the literature suggests that higher speeds may intensify therapy, contradictory evidence suggests benefits in reducing speed to activate certain neural centres. Body weight support exhibited a decreasing trend throughout therapy, potentially influencing metabolic costs and muscle activation. Similarly, guidance force decreased steadily during sessions, with evidence suggesting its impact on muscle activation and tracking accuracy. Furthermore, significant enhancements were noted in the distance covered and number of steps during Lokomat training, indicating positive progress in locomotor capabilities. Overall, this study contributes insights into the efficacy of Lokomat therapy and underscores the importance of optimizing adjustable parameters to maximize therapeutic benefits. Further research is warranted to explore individualized approaches and long-term outcomes in diverse patient populations.
Author Contributions
Conceptualization, M.B.; methodology, M.B., A.H.; software, M.B.; validation, M.B., A.H.; formal analysis, M.B.; investigation, M.B.; resources, M.B.; data curation, M.B.; writing—original draft preparation, M.B.; writing—review and editing, M.B., A.H.; visualization, M.B., A.H.; supervision, M.B.; project administration, M.B.; funding acquisition, M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Józef Piłsudski University of Physical Education in Warsaw, Poland (protocol code SKE01-15/2023 and date of approval 24 March 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study aged over 16 and/or their parents (for patients under 18).
Data Availability Statement
The measurement data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
We would like to thank Kacper Sroka for his help in data collection.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Koman, L.A.; Smith, B.P.; Shilt, J.S. Cerebral palsy. Lancet 2004, 363, 1619–1631. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Zheng, Y.; Yang, Y.; Fang, W.; Huang, M.; Li, D.; Xu, Z.; Xu, F.; Wang, J. A bibliometric analysis of cerebral palsy from 2003 to 2022. Front. Neurol. 2024, 15, 1292587. [Google Scholar] [CrossRef]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S.; et al. Cerebral palsy. Nat. Rev. Dis. Primers 2016, 2, 15082. [Google Scholar] [CrossRef]
- Mu, Y.; Li, N.; Guan, L.; Wang, C.; Shang, S.; Wang, Y. Therapies for children with cerebral palsy: A Web of Science-based literature analysis. Neural Regen. Res. 2012, 7, 2632–2639. [Google Scholar] [CrossRef]
- Elmas Bodur, B.; Erdoğanoğlu, Y.; Asena Sel, S. Effects of robotic-assisted gait training on physical capacity, and quality of life among chronic stroke patients: A randomized controlled study. J. Clin. Neurosci. 2024, 120, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.G.; Jang, D.H.; Lee, D.; Oh, J.Y.; Han, M.H. Botulinum Toxin Injection in Children with Hemiplegic Cerebral Palsy: Correction of Growth through Comparison of Treated and Unaffected Limbs. Toxins 2019, 11, 688. [Google Scholar] [CrossRef]
- Palomo-Carrión, R.; Romero-Galisteo, R.P.; Pinero-Pinto, E.; López-Muñoz, P.; Romay-Barrero, H.; José, F.G.S. Application of Low-Intensity Modified Constraint-Induced Movement Therapy to Improve the Affected Upper Limb Functionality in Infantile Hemiplegia with Moderate Manual Ability: Case Series. Children 2020, 7, 127. [Google Scholar] [CrossRef]
- Hsieh, C.L. Modulation of cerebral cortex in acupuncture stimulation: A study using sympathetic skin response and somatosensory evoked potentials. Am. J. Chin. Med. 1998, 26, 1–11. [Google Scholar] [CrossRef]
- Llamas-Ramos, R.; Sánchez-González, J.L.; Llamas-Ramos, I. Robotic Systems for the Physiotherapy Treatment of Children with Cerebral Palsy: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5116. [Google Scholar] [CrossRef]
- van Dellen, F.; Labruyère, R. Settings matter: A scoping review on parameters in robot-assisted gait therapy identifies the importance of reporting standards. J. Neuroeng. Rehabil. 2022, 19, 40. [Google Scholar] [CrossRef] [PubMed]
- Baronchelli, F.; Zucchella, C.; Serrao, M.; Intiso, D.; Bartolo, M. The Effect of Robotic Assisted Gait Training With Lokomat(R) on Balance Control After Stroke: Systematic Review and Meta-Analysis. Front. Neurol. 2021, 12, 661815. [Google Scholar] [CrossRef] [PubMed]
- Pawłowski, M.; Gąsior, J.S.; Mrozek, P.; Bonikowski, M.; Błaszczyk, J.W.; Dąbrowski, M.J. Evaluation of training using Lokomat (Hocoma) ® in physiotherapy process of children and adolescents with cerebral palsy—Preliminary report. Child Neurol. 2015, 23. [Google Scholar]
- Barbeau, H. Locomotor training in neurorehabilitation: Emerging rehabilitation concepts. Neurorehabilit. Neural Repair 2003, 17, 3–11. [Google Scholar] [CrossRef]
- Wiart, L.; Rosychuk, R.J.; Wright, F.V. Evaluation of the effectiveness of robotic gait training and gait-focused physical therapy programs for children and youth with cerebral palsy: A mixed methods RCT. BMC Neurol. 2016, 16, 86. [Google Scholar] [CrossRef]
- Shackleton, C.; Evans, R.; Shamley, D.; West, S.; Albertus, Y. Effectiveness of over-ground robotic locomotor training in improving walking performance, cardiovascular demands, secondary complications and user-satisfaction in individuals with spinal cord injuries: A systematic review. J. Rehabil. Med. 2019, 51, 723–733. [Google Scholar] [CrossRef]
- Mekki, M.; Delgado, A.D.; Fry, A.; Putrino, D.; Huang, V. Robotic Rehabilitation and Spinal Cord Injury: A Narrative Review. Neurother. J. Am. Soc. Exp. NeuroTherapeutics 2018, 15, 604–617. [Google Scholar] [CrossRef] [PubMed]
- Furnari, A.; Calabrò, R.S.; De Cola, M.C.; Bartolo, M.; Castelli, A.; Mapelli, A.; Buttacchio, G.; Farini, E.; Bramanti, P.; Casale, R. Robotic-assisted gait training in Parkinson’s disease: A three-month follow-up randomized clinical trial. Int. J. Neurosci. 2017, 127, 996–1004. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.; Dattola, V.; De Cola, M.C.; Logiudice, A.L.; Porcari, B.; Cannavò, A.; Sciarrone, F.; De Luca, R.; Molonia, F.; Sessa, E.; et al. The role of robotic gait training coupled with virtual reality in boosting the rehabilitative outcomes in patients with multiple sclerosis. Int. J. Rehabil. Res. 2018, 41, 166–172. [Google Scholar] [CrossRef]
- Meyer-Heim, A.; Ammann-Reiffer, C.; Schmartz, A.; Schäfer, J.; Sennhauser, F.H.; Heinen, F.; Knecht, B.; Dabrowski, E.; Borggraefe, I. Improvement of walking abilities after robotic-assisted locomotion training in children with cerebral palsy. Arch. Dis. Child. 2009, 94, 615–620. [Google Scholar] [CrossRef]
- Borggraefe, I.; Meyer-Heim, A.; Kumar, A.; Schaefer, J.S.; Berweck, S.; Heinen, F. Improved gait parameters after robotic-assisted locomotor treadmill therapy in a 6-year-old child with cerebral palsy. Mov. Disord. Off. J. Mov. Disord. Soc. 2008, 23, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Westlake, K.P.; Patten, C. Pilot study of Lokomat versus manual-assisted treadmill training for locomotor recovery post-stroke. J. Neuroeng. Rehabil. 2009, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- Borggraefe, I.; Schaefer, J.S.; Klaiber, M.; Dabrowski, E.; Ammann-Reiffer, C.; Knecht, B.; Berweck, S.; Heinen, F.; Meyer-Heim, A. Robotic-assisted treadmill therapy improves walking and standing performance in children and adolescents with cerebral palsy. Eur. J. Paediatr. Neurol. 2010, 14, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Klobucká, S.; Klobucký, R.; Kollár, B. Effect of robot-assisted gait training on motor functions in adolescent and young adult patients with bilateral spastic cerebral palsy: A randomized controlled trial. NeuroRehabilitation 2020, 47, 495–508. [Google Scholar] [CrossRef]
- Aurich-Schuler, T.; Gut, A.; Labruyère, R. The FreeD module for the Lokomat facilitates a physiological movement pattern in healthy people—A proof of concept study. J. Neuroeng. Rehabil. 2019, 16, 26. [Google Scholar] [CrossRef]
- Riener, R.; Lünenburger, L.; Maier, I.C.; Colombo, G.; Dietz, V. Locomotor Training in Subjects with Sensori-Motor Deficits: An Overview of the Robotic Gait Orthosis Lokomat. J. Healthc. Eng. 2010, 1, 517674. [Google Scholar] [CrossRef]
- Chrysagis, N.; Skordilis, E.K.; Koutsouki, D. Validity and clinical utility of functional assessments in children with cerebral palsy. Arch. Phys. Med. Rehabil. 2014, 95, 369–374. [Google Scholar] [CrossRef]
- Thompson, P.; Beath, T.; Bell, J.; Jacobson, G.; Phair, T.; Salbach, N.M.; Wright, F.V. Test-retest reliability of the 10-metre fast walk test and 6-minute walk test in ambulatory school-aged children with cerebral palsy. Dev. Med. Child Neurol. 2008, 50, 370–376. [Google Scholar] [CrossRef]
- Kaczmarczyk, K.; Błażkiewicz, M.; Wiszomirska, I.; Pietrasik, K.; Zdrodowska, A.; Wit, A.; Barton, G.; Skarżyński, H. Assessing Gait Stability before and after Cochlear Implantation. BioMed Res. Int. 2019, 2019, 2474273. [Google Scholar] [CrossRef]
- Wu, L.; Xu, G.; Wu, Q. The effect of the Lokomat(®) robotic-orthosis system on lower extremity rehabilitation in patients with stroke: A systematic review and meta-analysis. Front. Neurol. 2023, 14, 1260652. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, P.; Li, C. Systematic review and network meta-analysis of robot-assisted gait training on lower limb function in patients with cerebral palsy. Neurol. Sci. 2023, 44, 3863–3875. [Google Scholar] [CrossRef] [PubMed]
- Colombo, G.; Wirz, M.; Dietz, V. Driven gait orthosis for improvement of locomotor training in paraplegic patients. Spinal Cord 2001, 39, 252–255. [Google Scholar] [CrossRef] [PubMed]
- Talaty, M.; Esquenazi, A. Feasibility and outcomes of supplemental gait training by robotic and conventional means in acute stroke rehabilitation. J. Neuroeng. Rehabil. 2023, 20, 134. [Google Scholar] [CrossRef]
- Koenig, A.; Caruso, A.; Bolliger, M.; Somaini, L.; Omlin, X.; Morari, M.; Riener, R. Model-based heart rate control during robot-assisted gait training. In Proceedings of the 2011 IEEE International Conference on Robotics and Automation, Shanghai, China, 9–13 May 2011; pp. 4151–4156. [Google Scholar]
- van Kammen, K.; Reinders-Messelink, H.A.; Elsinghorst, A.L.; Wesselink, C.F.; Meeuwisse-de Vries, B.; van der Woude, L.H.V.; Boonstra, A.M.; den Otter, R. Amplitude and stride-to-stride variability of muscle activity during Lokomat guided walking and treadmill walking in children with cerebral palsy. Eur. J. Paediatr. Neurol. 2020, 29, 108–117. [Google Scholar] [CrossRef]
- Prideaux, N.; van den Berg, M.; Drummond, C.; Barr, C. Augmented Performance Feedback during Robotic Gait Therapy Results in Moderate Intensity Cardiovascular Exercise in Subacute Stroke. J. Stroke Cerebrovasc. Dis. 2020, 29, 104758. [Google Scholar] [CrossRef]
- Rodrigues, T.A.; Goroso, D.G.; Westgate, P.M.; Carrico, C.; Batistella, L.R.; Sawaki, L. Slow Versus Fast Robot-Assisted Locomotor Training After Severe Stroke: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2017, 96, S165–S170. [Google Scholar] [CrossRef]
- Bergmann, J.; Krewer, C.; Jahn, K.; Muller, F. Robot-assisted gait training to reduce pusher behavior: A randomized controlled trial. Neurology 2018, 91, e1319–e1327. [Google Scholar] [CrossRef]
- Schwartz, I.; Sajina, A.; Neeb, M.; Fisher, I.; Katz-Luerer, M.; Meiner, Z. Locomotor training using a robotic device in patients with subacute spinal cord injury. Spinal Cord 2011, 49, 1062–1067. [Google Scholar] [CrossRef]
- Mıdık, M.; Paker, N.; Buğdaycı, D.; Mıdık, A.C. Effects of robot-assisted gait training on lower extremity strength, functional independence, and walking function in men with incomplete traumatic spinal cord injury. Turk. J. Phys. Med. Rehabil. 2020, 66, 54–59. [Google Scholar] [CrossRef]
- Krishnan, C.; Kotsapouikis, D.; Dhaher, Y.Y.; Rymer, W.Z. Reducing robotic guidance during robot-assisted gait training improves gait function: A case report on a stroke survivor. Arch. Phys. Med. Rehabil. 2013, 94, 1202–1206. [Google Scholar] [CrossRef] [PubMed]
- Cherni, Y.; Hajizadeh, M.; Dal Maso, F.; Turpin, N.A. Effects of body weight support and guidance force settings on muscle synergy during Lokomat walking. Eur. J. Appl. Physiol. 2021, 121, 2967–2980. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Hu, G.; Ran, J.; Chen, L.; Zhang, X.; Zhang, Y. Effects of bodyweight support and guidance force on muscle activation during Locomat walking in people with stroke: A cross-sectional study. J. Neuroeng. Rehabil. 2020, 17, 5. [Google Scholar] [CrossRef] [PubMed]
- Krewer, C.; Müller, F.; Husemann, B.; Heller, S.; Quintern, J.; Koenig, E. The influence of different Lokomat walking conditions on the energy expenditure of hemiparetic patients and healthy subjects. Gait Posture 2007, 26, 372–377. [Google Scholar] [CrossRef]
- Lam, T.; Pauhl, K.; Ferguson, A.; Malik, R.N.; Krassioukov, A.; Eng, J.J. Training with robot-applied resistance in people with motor-incomplete spinal cord injury: Pilot study. J. Rehabil. Res. Dev. 2015, 52, 113–129. [Google Scholar] [CrossRef]
- van Kammen, K.; Boonstra, A.M.; van der Woude, L.H.V.; Visscher, C.; Reinders-Messelink, H.A.; den Otter, R. Lokomat guided gait in hemiparetic stroke patients: The effects of training parameters on muscle activity and temporal symmetry. Disabil. Rehabil. 2020, 42, 2977–2985. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).