Lesion Localization and Limb Outcomes in Elderly Patients with and Without Type 2 Diabetes Mellitus Who Undergo Atherectomy-Assisted Endovascular Revascularization due to Symptomatic Peripheral Artery Disease
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design and Ethics Disclosures
2.2. Patient Population
2.3. Endovascular Procedure Protocol
2.4. Analysis of Angiographic Data
2.5. Follow-Up and Study Endpoints
2.6. Statistical Analysis
3. Results
3.1. Demographic Data, Clinical Presentation, and Laboratory Parameters
3.2. Lesion Localization, Length, and Calcification
3.3. Technical and Procedural Data
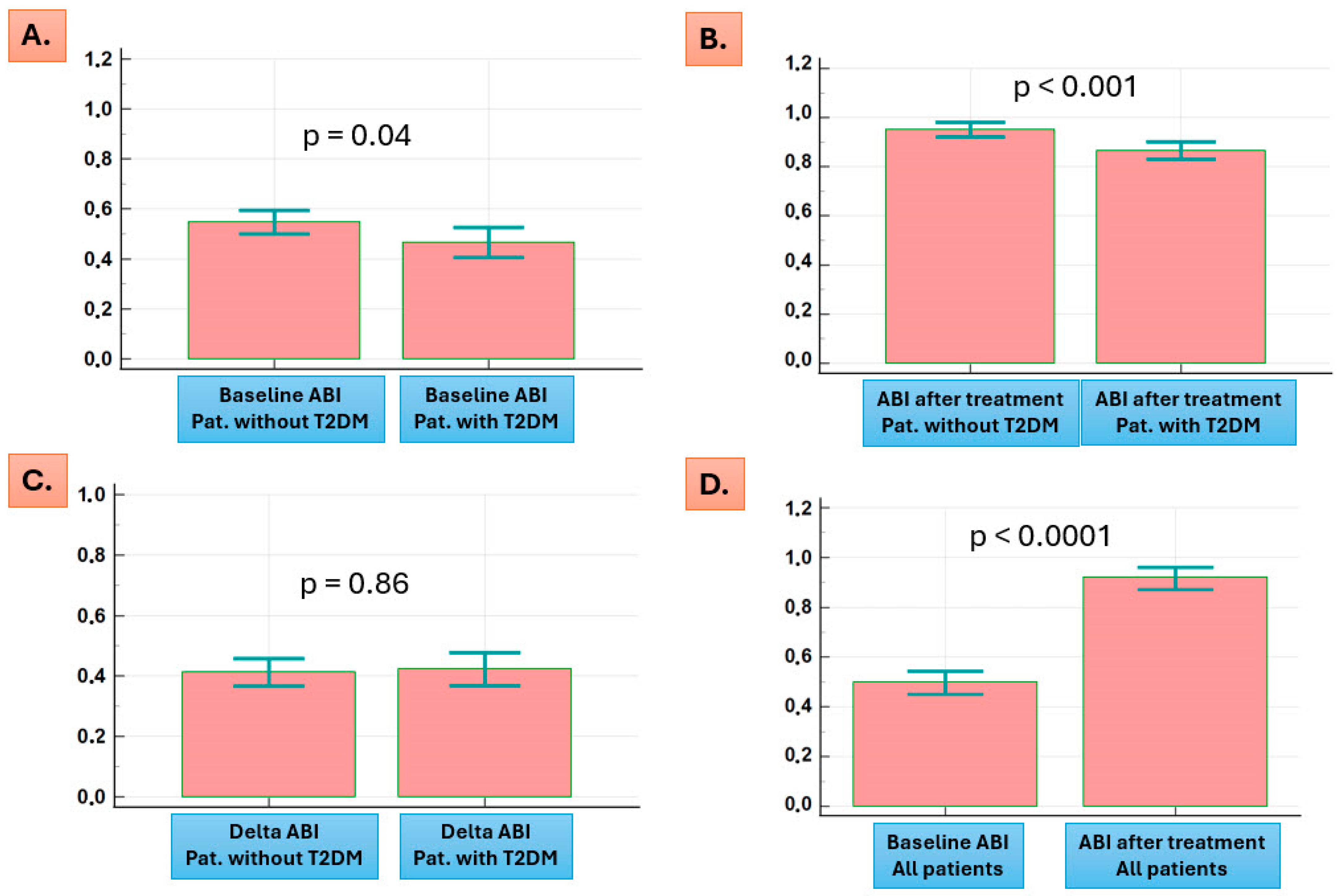
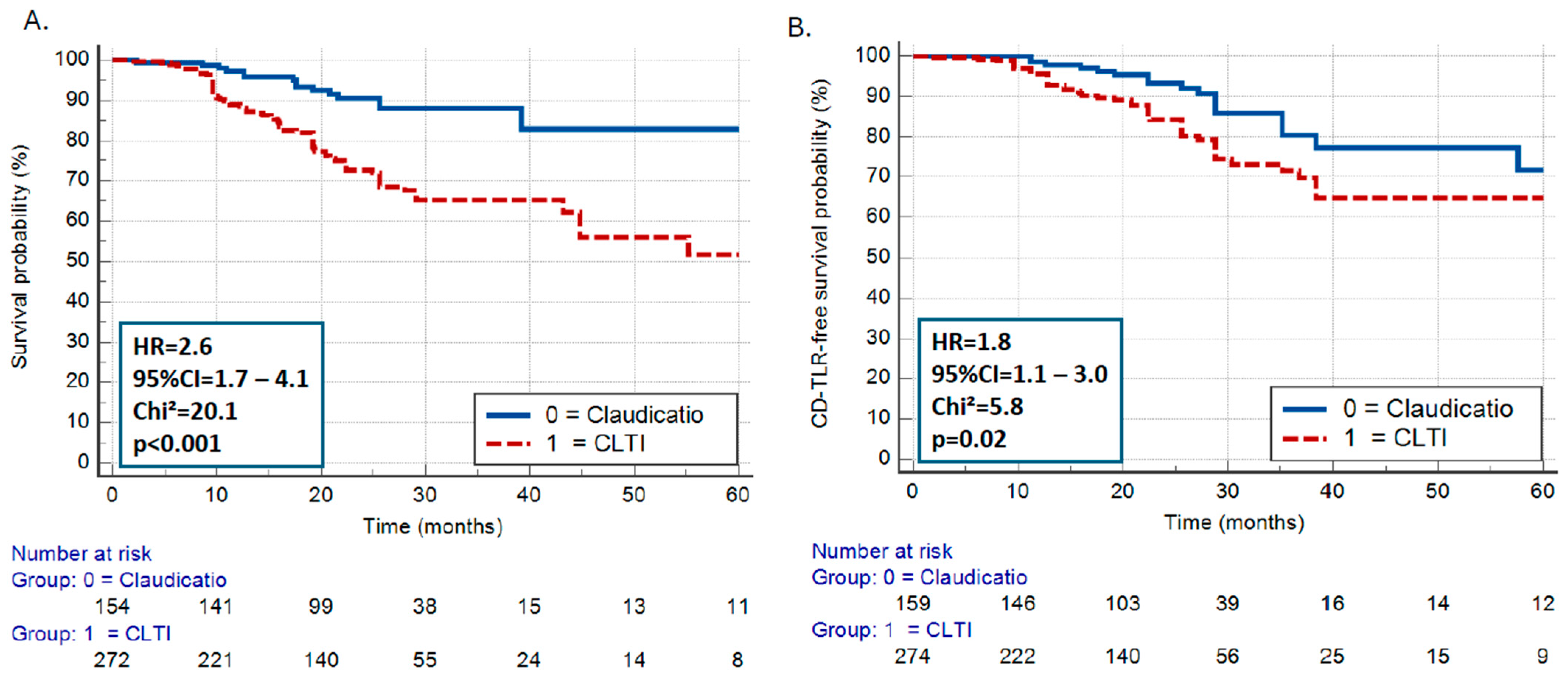
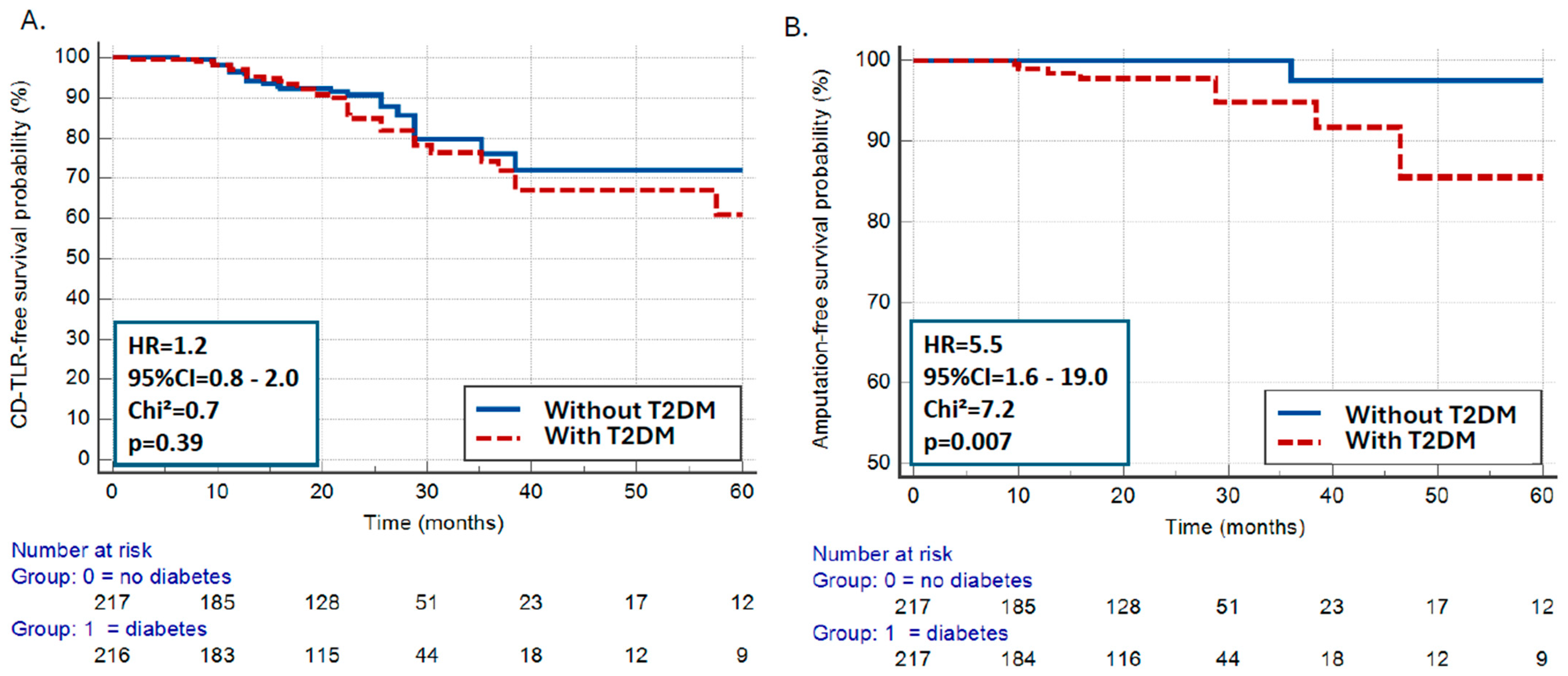
3.4. Clinical Endpoints
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Verma, S.; Leiter, L.A.; Mangla, K.K.; Nielsen, N.F.; Hansen, Y.; Bonaca, M.P. Epidemiology and Burden of Peripheral Artery Disease in People with Type 2 Diabetes: A Systematic Literature Review. Diabetes Ther. 2024, 15, 1893–1961. [Google Scholar] [CrossRef] [PubMed]
- Rammos, C.; Steinmetz, M.; Lortz, J.; Mahabadi, A.A.; Petrikhovich, O.; Kirsch, K.; Hering, R.; Schulz, M.; Rassaf, T. Peripheral artery disease in Germany (2009–2018): Prevalence, frequency of specialized ambulatory care and use of guideline-recommended therapy—A population-based study. Lancet Reg. Health Eur. 2021, 5, 100113. [Google Scholar] [CrossRef] [PubMed]
- Gornik, H.L.; Aronow, H.D.; Goodney, P.P.; Arya, S.; Brewster, L.P.; Byrd, L.; Chandra, V.; Drachman, D.E.; Eaves, J.M.; Ehrman, J.K.; et al. 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS Guideline for the Management of Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2024, 149, e1313–e1410. [Google Scholar] [CrossRef] [PubMed]
- Soyoye, D.O.; Abiodun, O.O.; Ikem, R.T.; Kolawole, B.A.; Akintomide, A.O. Diabetes and peripheral artery disease: A review. World J. Diabetes 2021, 12, 827–838. [Google Scholar] [CrossRef] [PubMed]
- Sprenger, L.; Mader, A.; Larcher, B.; Machler, M.; Vonbank, A.; Zanolin-Purin, D.; Leiherer, A.; Muendlein, A.; Drexel, H.; Saely, C.H. Type 2 diabetes and the risk of cardiovascular events in peripheral artery disease versus coronary artery disease. BMJ Open Diabetes Res. Care 2021, 9, e002407. [Google Scholar] [CrossRef]
- Singh, M.V.; Dokun, A.O. Diabetes mellitus in peripheral artery disease: Beyond a risk factor. Front. Cardiovasc. Med. 2023, 10, 1148040. [Google Scholar] [CrossRef]
- Katsiki, N.; Giannoukas, A.D.; Athyros, V.G.; Mikhailidis, D.P. Lipid-lowering treatment in peripheral artery disease. Curr. Opin. Pharmacol. 2018, 39, 19–26. [Google Scholar] [CrossRef]
- Katsiki, N.; Purrello, F.; Tsioufis, C.; Mikhailidis, D.P. Cardiovascular disease prevention strategies for type 2 diabetes mellitus. Expert. Opin. Pharmacother. 2017, 18, 1243–1260. [Google Scholar] [CrossRef]
- Donas, K.P.; Psyllas, A.; Pitoulias, A.G.; Kazemtash, M.; Dahi, F.; Abu Bakr, N.; Korosoglou, G. Periprocedural Outcomes of Rotational Atherectomy-Assisted Balloon Angioplasty in Isolated Atherosclerotic Popliteal Artery Lesions: The ISO-POP Trial. J. Clin. Med. 2023, 12, 2797. [Google Scholar] [CrossRef]
- Giusca, S.; Hagstotz, S.; Lichtenberg, M.; Heinrich, U.; Eisenbach, C.; Andrassy, M.; Korosoglou, G. Phoenix atherectomy for patients with peripheral artery disease. EuroIntervention 2022, 18, e432–e442. [Google Scholar] [CrossRef]
- Korosoglou, G.; Schmidt, A.; Stavroulakis, K.; Pollert, D.; Giusca, S.; Lichtenberg, M.; Scheinert, D.; Torsello, G.; Andrassy, M.; Blessing, E. Retrograde Access for the Recanalization of Lower-Limb Occlusive Lesions: A German Experience Report in 1,516 Consecutive Patients. JACC Cardiovasc. Interv. 2022, 15, 348–351. [Google Scholar] [CrossRef] [PubMed]
- Trenkler, C.; Blessing, E.; Jehn, A.; Karcher, J.; Schoefthaler, C.; Schmidt, A.; Korosoglou, G. Retrospective Case Control Matched Comparison of the Antegrade versus Retrograde Strategy after Antegrade Recanalisation Failure in Complex de novo Femoropopliteal Occlusive Lesions. Eur. J. Vasc. Endovasc. Surg. 2024, 67, 799–808. [Google Scholar] [CrossRef] [PubMed]
- Lichtenberg, M.; Korosoglou, G. Atherectomy plus antirestenotic therapy for SFA lesions: Evolving evidence for better patency rates in complex lesions. J. Cardiovasc. Surg. (Torino) 2019, 60, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Inker, L.A.; Eneanya, N.D.; Coresh, J.; Tighiouart, H.; Wang, D.; Sang, Y.; Crews, D.C.; Doria, A.; Estrella, M.M.; Froissart, M.; et al. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N. Engl. J. Med. 2021, 385, 1737–1749. [Google Scholar] [CrossRef] [PubMed]
- Korosoglou, G.; Schmidt, A.; Lichtenberg, M.; Torsello, G.; Grozinger, G.; Mustapha, J.; Varcoe, R.L.; Zeller, T.; Blessing, E.; Langhoff, R. Crossing Algorithm for Infrainguinal Chronic Total Occlusions: An Interdisciplinary Expert Opinion Statement. JACC Cardiovasc. Interv. 2023, 16, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Korosoglou, G.; Feld, J.; Langhoff, R.; Lichtenberg, M.; Stausberg, J.; Hoffmann, U.; Rammos, C.; Malyar, N.; Investigators, R. Safety and Effectiveness of Debulking for the Treatment of Infrainguinal Peripheral Artery Disease. Data From the Recording Courses of vascular Diseases Registry in 2910 Patients. Angiology 2024, 33197241263381. [Google Scholar] [CrossRef] [PubMed]
- Korosoglou, G.; Giusca, S.; Langhoff, R.; Lichtenberg, M.; Lawall, H.; Schellong, S.; Stausberg, J.; Hoffmann, U.; Enders, D.; Malyar, N. Safety and Effectiveness of Endovascular Therapy for the Treatment of Peripheral Artery Disease in Patients with and without Diabetes Mellitus. Angiology 2022, 73, 956–966. [Google Scholar] [CrossRef]
- Fanelli, F.; Cannavale, A.; Gazzetti, M.; Lucatelli, P.; Wlderk, A.; Cirelli, C.; d’Adamo, A.; Salvatori, F.M. Calcium burden assessment and impact on drug-eluting balloons in peripheral arterial disease. Cardiovasc. Interv. Radiol. 2014, 37, 898–907. [Google Scholar] [CrossRef]
- Committee, T.S.; Jaff, M.R.; White, C.J.; Hiatt, W.R.; Fowkes, G.R.; Dormandy, J.; Razavi, M.; Reekers, J.; Norgren, L. An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Vasc. Med. 2015, 20, 465–478. [Google Scholar] [CrossRef]
- DeMarsilis, A.; Reddy, N.; Boutari, C.; Filippaios, A.; Sternthal, E.; Katsiki, N.; Mantzoros, C. Pharmacotherapy of type 2 diabetes: An update and future directions. Metabolism 2022, 137, 155332. [Google Scholar] [CrossRef]
- Plantinga, L.C.; Crews, D.C.; Coresh, J.; Miller, E.R., 3rd; Saran, R.; Yee, J.; Hedgeman, E.; Pavkov, M.; Eberhardt, M.S.; Williams, D.E.; et al. Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or prediabetes. Clin. J. Am. Soc. Nephrol. 2010, 5, 673–682. [Google Scholar] [CrossRef]
- Katsiki, N.; Mikhailidis, D.P.; Mantzoros, C.S. Non-alcoholic fatty liver disease and dyslipidemia: An update. Metabolism 2016, 65, 1109–1123. [Google Scholar] [CrossRef] [PubMed]
- Kokkorakis, M.; Boutari, C.; Katsiki, N.; Mantzoros, C.S. From non-alcoholic fatty liver disease (NAFLD) to steatotic liver disease (SLD): An ongoing journey towards refining the terminology for this prevalent metabolic condition and unmet clinical need. Metabolism 2023, 147, 155664. [Google Scholar] [CrossRef] [PubMed]
- Kokkorakis, M.; Muzurovic, E.; Volcansek, S.; Chakhtoura, M.; Hill, M.A.; Mikhailidis, D.P.; Mantzoros, C.S. Steatotic Liver Disease: Pathophysiology and Emerging Pharmacotherapies. Pharmacol. Rev. 2024, 76, 454–499. [Google Scholar] [CrossRef] [PubMed]
- Katsiki, N.; Kolovou, G.; Melidonis, A.; Banach, M. The Cardiac-Kidney-Liver (CKL) syndrome: The “real entity” of type 2 diabetes mellitus. Arch. Med. Sci. 2024, 20, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Katsiki, N.; Ferrannini, E.; Mantzoros, C. New American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) guidelines for the pharmacotherapy of type 2 diabetes: Placing them into a practicing physician’s perspective. Metabolism 2020, 107, 154218. [Google Scholar] [CrossRef]
- Katsiki, N.; Banach, M.; Mikhailidis, D.P. Is type 2 diabetes mellitus a coronary heart disease equivalent or not? Do not just enjoy the debate and forget the patient! Arch. Med. Sci. 2019, 15, 1357–1364. [Google Scholar] [CrossRef]
- Rorth, R.; Jhund, P.S.; Kristensen, S.L.; Desai, A.S.; Kober, L.; Rouleau, J.L.; Solomon, S.D.; Swedberg, K.; Zile, M.R.; Packer, M.; et al. The prognostic value of troponin T and N-terminal pro B-type natriuretic peptide, alone and in combination, in heart failure patients with and without diabetes. Eur. J. Heart Fail. 2019, 21, 40–49. [Google Scholar] [CrossRef]
- Ali, F.; Naqvi, S.A.; Bismillah, M.; Wajid, N. Comparative analysis of biochemical parameters in diabetic and non-diabetic acute myocardial infarction patients. Indian. Heart J. 2016, 68, 325–331. [Google Scholar] [CrossRef]
- Cimaglia, P.; Dalla Paola, L.; Carone, A.; Scavone, G.; Manfrini, M.; Brogneri, S.; Tenti, E.; Pavasini, R.; Bernucci, D.; Passarini, G.; et al. High-Sensitivity Cardiac Troponin Predicts Major Cardiovascular Events in Diabetic Patients with Critical Limb Ischemia and Foot Lesions. Front. Cardiovasc. Med. 2021, 8, 595701. [Google Scholar] [CrossRef]
- Vrsalovic, M.; Vrsalovic Presecki, A.; Aboyans, V. Cardiac troponins predict mortality and cardiovascular outcomes in patients with peripheral artery disease: A systematic review and meta-analysis of adjusted observational studies. Clin. Cardiol. 2022, 45, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Mouselimis, D.; Hagstotz, S.; Lichtenberg, M.; Donas, K.P.; Heinrich, U.; Avranas, K.; Dimitriadis, Z.; Blessing, E.; Langhoff, R.; Frey, N.; et al. Cardiac Troponins for the Clinical Management of Patients with Claudication and without Cardiac Symptoms. J. Clin. Med. 2022, 11, 7287. [Google Scholar] [CrossRef] [PubMed]
- Howard, D.P.; Banerjee, A.; Fairhead, J.F.; Hands, L.; Silver, L.E.; Rothwell, P.M.; Oxford Vascular, S. Population-Based Study of Incidence, Risk Factors, Outcome, and Prognosis of Ischemic Peripheral Arterial Events: Implications for Prevention. Circulation 2015, 132, 1805–1815. [Google Scholar] [CrossRef] [PubMed]
- Spreen, M.I.; Gremmels, H.; Teraa, M.; Sprengers, R.W.; Verhaar, M.C.; Statius van Eps, R.G.; de Vries, J.P.; Mali, W.P.; van Overhagen, H.; on behalf of the PADI and JUVENTAS Study Groups. Diabetes Is Associated with Decreased Limb Survival in Patients with Critical Limb Ischemia: Pooled Data From Two Randomized Controlled Trials. Diabetes Care 2016, 39, 2058–2064. [Google Scholar] [CrossRef] [PubMed]
- Luscher, T.F.; Creager, M.A.; Beckman, J.A.; Cosentino, F. Diabetes and vascular disease: Pathophysiology, clinical consequences, and medical therapy: Part II. Circulation 2003, 108, 1655–1661. [Google Scholar] [CrossRef] [PubMed]
- Ying, A.F.; Tang, T.Y.; Jin, A.; Chong, T.T.; Hausenloy, D.J.; Koh, W.P. Diabetes and other vascular risk factors in association with the risk of lower extremity amputation in chronic limb-threatening ischemia: A prospective cohort study. Cardiovasc. Diabetol. 2022, 21, 7. [Google Scholar] [CrossRef]
- Barnes, J.A.; Eid, M.A.; Creager, M.A.; Goodney, P.P. Epidemiology and Risk of Amputation in Patients with Diabetes Mellitus and Peripheral Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1808–1817. [Google Scholar] [CrossRef]
- Li, Q.; Birmpili, P.; Atkins, E.; Johal, A.S.; Waton, S.; Williams, R.; Boyle, J.R.; Harkin, D.W.; Pherwani, A.D.; Cromwell, D.A. Illness Trajectories after Revascularization in Patients with Peripheral Artery Disease: A Unified Approach to Understanding the Risk of Major Amputation and Death. Circulation 2024, 150, 261–271. [Google Scholar] [CrossRef]
- Hicks, C.W.; Najafian, A.; Farber, A.; Menard, M.T.; Malas, M.B.; Black, J.H., 3rd; Abularrage, C.J. Diabetes does not worsen outcomes following infrageniculate bypass or endovascular intervention for patients with critical limb ischemia. J. Vasc. Surg. 2016, 64, 1667–1674. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2024. Diabetes Care 2024, 47 (Suppl. S1), S158–S178. [Google Scholar] [CrossRef]

| Demographic Data, Clinical Presentation, Laboratory Parameters, and Procedural Data | All Patients (n = 500) | Patients with T2DM (n = 245) | Patients without T2DM (n = 255) | p-Values |
|---|---|---|---|---|
| Demographic data | ||||
| Age (years) | 78.0 (70.0–84.0) | 78.0 (70.0–83.0) | 79.0 (69.0–84.0) | 0.30 |
| Female gender, n (%) | 201 (40.2%) | 87 (35.5%) | 114 (44.7%) | 0.04 |
| Arterial hypertension, n (%) | 482 (96.4%) | 238 (97.1%) | 244 (95.7%) | 0.37 |
| Hyperlipidemia, n (%) | 440 (88.0%) | 221 (90.2%) | 219 (85.9%) | 0.14 |
| Active or former smoking, n (%) | 210 (42.0%) | 95 (38.8%) | 115 (45.1%) | 0.15 |
| History of CAD, n (%) | 221 (44.2%) | 126 (51.4%) | 95 (37.2%) | 0.001 |
| History of myocardial infarction | 97 (19.4%) | 56 (22.9%) | 41 (16.1%) | 0.06 |
| History of coronary bypass surgery | 57 (11.4%) | 35 (14.3%) | 22 (8.6%) | 0.05 |
| History of atrial fibrillation | 140 (28.0%) | 76 (31.0%) | 64 (25.1%) | 0.17 |
| PAD clinical presentation by Rutherford categories | ||||
| Rutherford category 2–3 (claudication) | 179 (35.8%) | 57 (23.3%) | 122 (47.8%) | <0.0001 * |
| Rutherford category 4 (resting pain) | 45 (9.0%) | 18 (7.3%) | 27 (10.6%) | |
| Rutherford category 5 (wound healing/tissue loss) | 276 (55.2%) | 170 (69.4%) | 106 (41.6%) | |
| Drug therapy | ||||
| Dual platelet therapy after treatment | 306 (61.2%) | 144 (58.8%) | 162 (63.5%) | 0.58 |
| Oral anticoagulants | 158 (31.6%) | 77 (31.4%) | 81 (31.8%) | 0.94 |
| ACE inhibitors or AT2 receptor blockers | 214 (42.8%) | 107 (43.7%) | 107 (41.9%) | 0.80 |
| ß-Blockers | 320 (64.0%) | 169 (68.9%) | 151 (59.2%) | 0.05 |
| Diuretics | 226 (45.2%) | 126 (51.4%) | 100 (39.2%) | 0.04 |
| Statins | 463 (92.6%) | 226 (92.2%) | 237 (92.9%) | 0.59 |
| Laboratory parameters | ||||
| Creatinine (mg/dL) | 1.01 (0.83–1.39) | 1.12 (0.87–1.57) | 0.94 (0.80–1.18) | <0.0001 |
| eGFR (mL/min/1.73 m2) | 54.0 (44.3–74.8) | 51.0 (35.0–68.8) | 56.0 (44.3–74.8) | 0.001 |
| Urea (mg/dL) | 39.0 (29.0–53.0) | 42 (33.0–64.3) | 36 (27.0–49.2) | <0.001 |
| Hemoglobin (mg/dL) | 12.8 (11.1–14.1) | 12.7 (10.8–14.0) | 13.0 (11.4–14.3) | 0.05 |
| High-sensitivity troponin T (ng/L) | 14.1 (9.3–23.3) | 18.8 (11.9–30.0) | 13.0 (8.3–19.7) | <0.0001 |
| HbA1c (%) | NA | 7.2 (6.3–7.9) | NA | NA |
| Procedural data | ||||
| Contrast agent administration (mL) | 120.0 (90.0–160.0) | 110.0 (80.0–150.0) | 120.0 (100.0–162.5) | 0.02 |
| Procedural duration (min) | 67.5 (51.0–89.0) | 62.0 (48.3–84.0) | 70.0 (54.0–93.8) | 0.006 |
| Radiation exposure (cGY × cm2) | 1254 (542–3469) | 1056 (496–3748) | 1328 (581–3342) | 0.39 |
| All Patients (n = 500) | Patients with T2DM (n = 245) | Patients without T2DM (n = 255) | p-Values | |
|---|---|---|---|---|
| Lesion localization | ||||
| Target lesions | n = 614 | n = 302 | n = 312 | |
| Iliac artery lesions | 22 (3.6%) | 9 (3.0%) | 13 (4.2%) | 0.44 |
| Femoropopliteal artery lesions | 383 (62.4%) | 170 (56.3%) | 213 (68.3%) | 0.0005 |
| Below-the-knee (BTK) artery lesions | 209 (34.0%) | 123 (40.7%) | 86 (27.5%) | 0.0002 |
| Lesion length and presence of occlusion | ||||
| Lesion length (cm) in femoropopliteal lesions | 17.0 (8.1–26.0) | 18.0 (10.0–26.0) | 16.0 (8.0–26.0) | 0.24 |
| Lesion length (cm) in BTK lesions | 22.0 (14.0–33.0) | 22.0 (13.2–32.0) | 22.0 (14.0–35.0) | 0.68 |
| Occlusion length (cm) in femoropopliteal lesions | 8.0 (2.8–18.0) | 6.0 (2.0–18.0) | 8.9 (4.0–18.0) | 0.10 |
| Occlusion length (cm) in BTK lesions | 12.0 (4.0–22.0) | 8.0 (4.0–22.0) | 12.0 (5.8–21.5) | 0.49 |
| Patients with at least 1 total occlusion | 278 (55.6%) | 127 (51.8%) | 151 (59.2%) | 0.10 |
| Number of CTO lesions per patient | 1.0 (0–1–0) | 1.0 (0–1–0) | 1.0 (0–1–0) | 0.13 |
| Lesion calcification by PACSS | ||||
| PACSS score 0–2, number of patients (%) | 121 (24.2%) | 54 (22.0%) | 67 (26.3%) | 0.87 |
| PACSS score 3, number of patients (%) | 175 (35.0%) | 98 (40.0%) | 77 (30.2%) | |
| PACSS score 4, number of patients (%) | 204 (40.8%) | 93 (38.0%) | 111 (43.5%) | |
| Lesion complexity by TASC | ||||
| TASC A/B, number of patients (%) | 94 (18.8%) | 54 (22.0%) | 40 (15.7%) | 0.19 |
| TASC C, number of patients (%) | 289 (57.8%) | 136 (55.5%) | 153 (60.0%) | |
| TASC D, number of patients (%) | 117 (23.4%) | 55 (22.5%) | 62 (24.3%) | |
| Coefficient | Standard Error | Wald | Hazard Ratios | 95% Cl | p-Values | |
|---|---|---|---|---|---|---|
| Age | 0.012 | 0.033 | 0.14 | 1.01 | 0.94 to 1.08 | 0.70 |
| Gender | −0.64 | 0.73 | 0.77 | 0.52 | 0.12 to 2.20 | 0.37 |
| T2DM | 2.22 | 1.07 | 4.31 | 9.29 | 1.13 to 76.19 | 0.04 |
| TASC classification | −0.041 | 0.52 | 0.006 | 0.95 | 0.34 to 2.69 | 0.93 |
| Calcification by PACSS | −0.30 | 0.38 | 0.64 | 0.73 | 0.34 to 1.55 | 0.42 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katsiki, N.; Geiss, E.; Giesen, A.; Jehn, A.; Rammos, C.; Karcher, J.C.; Schöfthaler, C.; Korosoglou, G. Lesion Localization and Limb Outcomes in Elderly Patients with and Without Type 2 Diabetes Mellitus Who Undergo Atherectomy-Assisted Endovascular Revascularization due to Symptomatic Peripheral Artery Disease. J. Clin. Med. 2024, 13, 6385. https://doi.org/10.3390/jcm13216385
Katsiki N, Geiss E, Giesen A, Jehn A, Rammos C, Karcher JC, Schöfthaler C, Korosoglou G. Lesion Localization and Limb Outcomes in Elderly Patients with and Without Type 2 Diabetes Mellitus Who Undergo Atherectomy-Assisted Endovascular Revascularization due to Symptomatic Peripheral Artery Disease. Journal of Clinical Medicine. 2024; 13(21):6385. https://doi.org/10.3390/jcm13216385
Chicago/Turabian StyleKatsiki, Niki, Eva Geiss, Alexander Giesen, Amila Jehn, Christos Rammos, Jan C. Karcher, Christoph Schöfthaler, and Grigorios Korosoglou. 2024. "Lesion Localization and Limb Outcomes in Elderly Patients with and Without Type 2 Diabetes Mellitus Who Undergo Atherectomy-Assisted Endovascular Revascularization due to Symptomatic Peripheral Artery Disease" Journal of Clinical Medicine 13, no. 21: 6385. https://doi.org/10.3390/jcm13216385
APA StyleKatsiki, N., Geiss, E., Giesen, A., Jehn, A., Rammos, C., Karcher, J. C., Schöfthaler, C., & Korosoglou, G. (2024). Lesion Localization and Limb Outcomes in Elderly Patients with and Without Type 2 Diabetes Mellitus Who Undergo Atherectomy-Assisted Endovascular Revascularization due to Symptomatic Peripheral Artery Disease. Journal of Clinical Medicine, 13(21), 6385. https://doi.org/10.3390/jcm13216385








