Sex-Based Differences in Polytraumatized Patients between 1995 and 2020: Experiences from a Level I Trauma Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients’ Population
2.2. Statistical Analyses
3. Results
3.1. Overall Results
3.1.1. Baseline Characteristics
3.1.2. Injury Patterns and Injury Severity
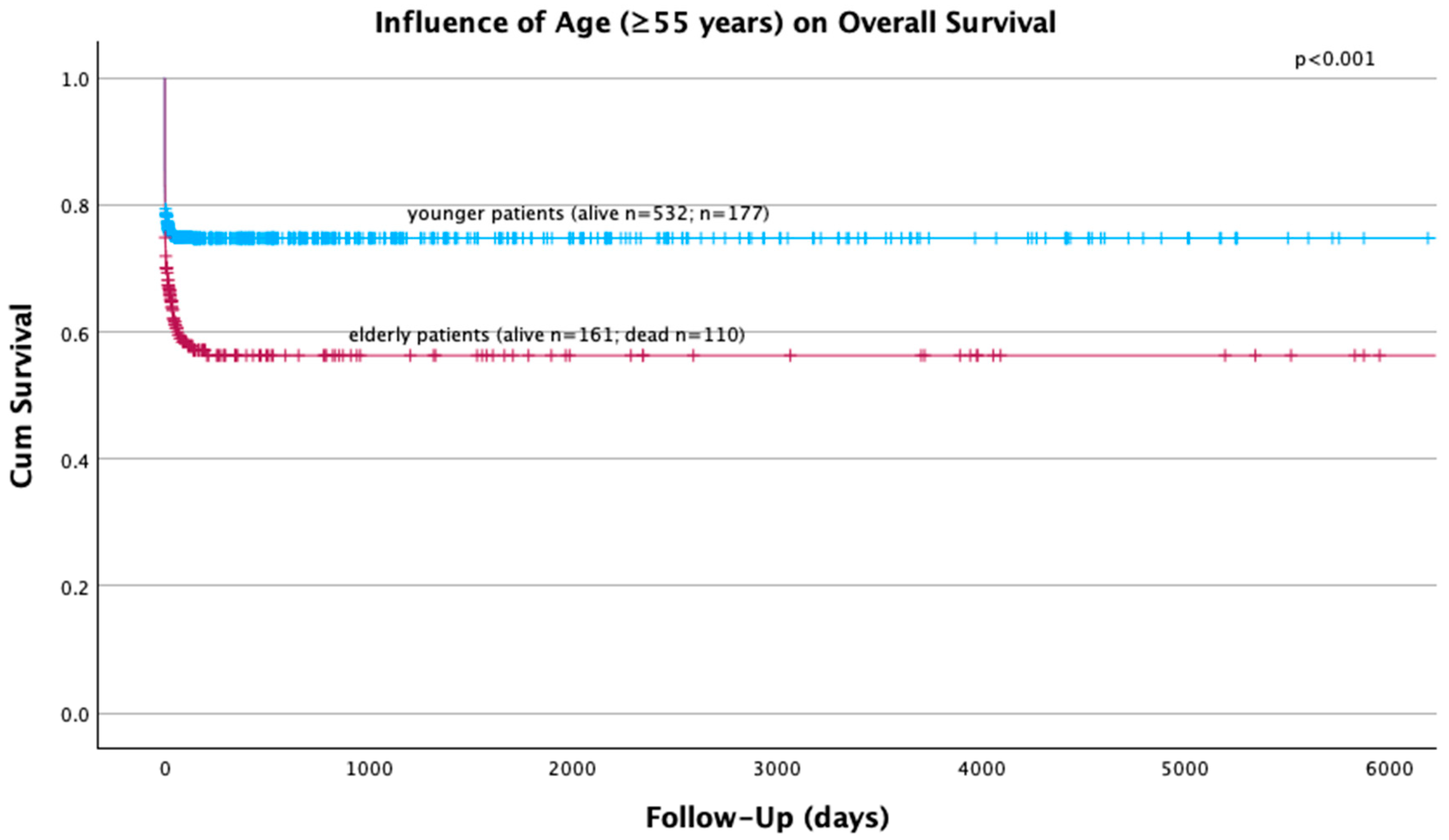
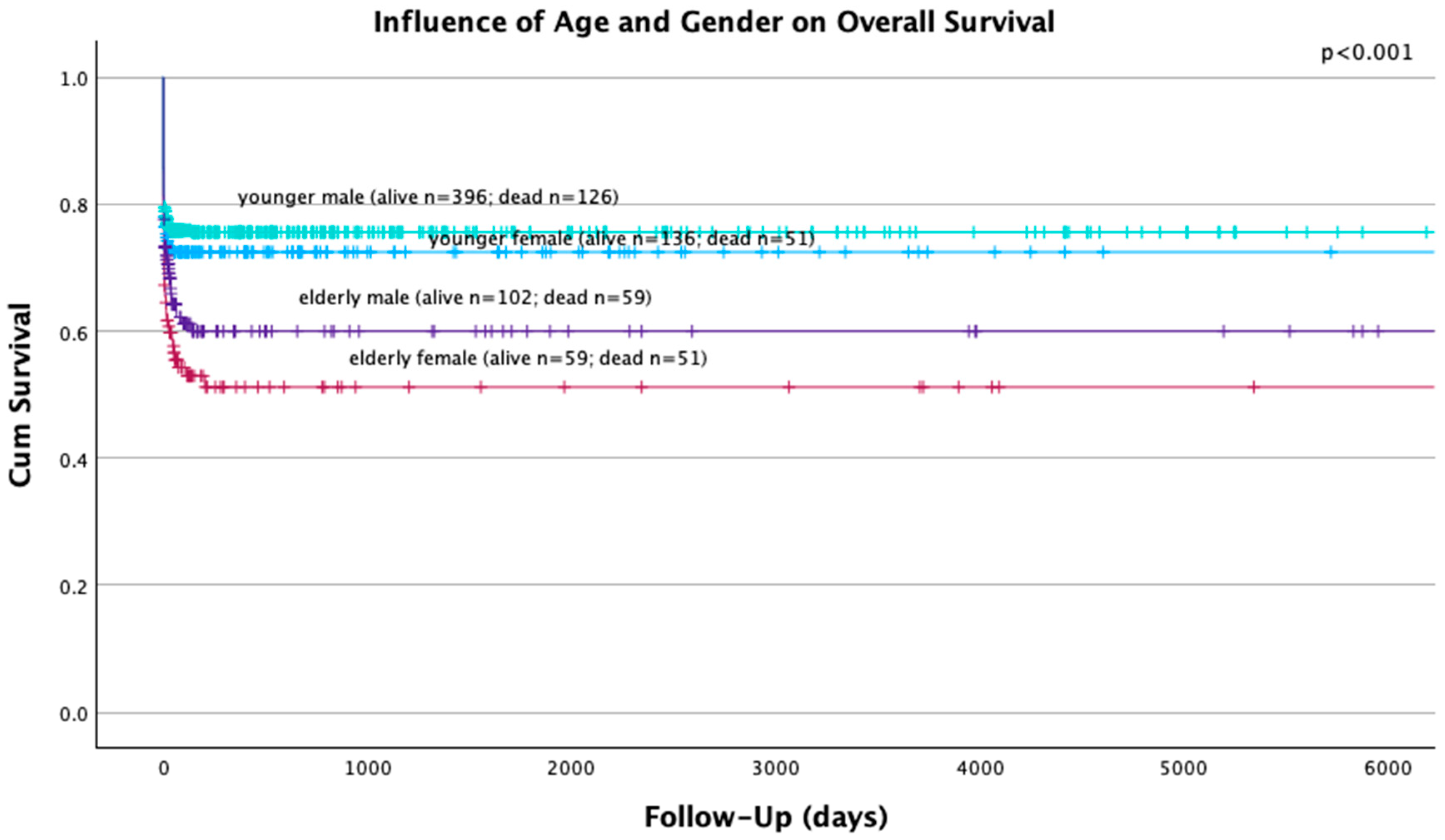
3.1.3. Survival
3.2. Sex-Related Differences in Elderly Patients
3.2.1. Baseline Characteristics of Elderly Patients
3.2.2. Injury Patterns and Injury Severity of Elderly Patients
3.2.3. Survival in Elderly Polytrauma Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pape, H.C.; Lefering, R.; Butcher, N.; Peitzman, A.; Leenen, L.; Marzi, I.; Lichte, P.; Josten, C.; Bouillon, B.; Schmucker, U.; et al. The definition of polytrauma revisited: An international consensus process and proposal of the new ‘Berlin definition’. J. Trauma. Acute Care Surg. 2014, 77, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Butcher, N.; Balogh, Z.J. AIS > 2 in at least two body regions: A potential new anatomical definition of polytrauma. Injury 2012, 43, 196–199. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases; Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Saad, S.; Mohamed, N.; Moghazy, A.; Ellabban, G.; El-Kamash, S. Venous glucose, serum lactate and base deficit as biochemical predictors of mortality in patients with polytrauma. Ulus. Travma Acil Cerrahi Derg. 2016, 22, 29–33. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tornetta, P., 3rd; Mostafavi, H.; Riina, J.; Turen, C.; Reimer, B.; Levine, R.; Behrens, F.; Geller, J.; Ritter, C.; Homel, P. Morbidity and mortality in elderly trauma patients. J. Trauma. 1999, 46, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Bingold, T.M.; Lefering, R.; Zacharowski, K.; Meybohm, P.; Waydhas, C.; Rosenberger, P.; Scheller, B.; DIVI Intensive Care Registry Group. Individual Organ Failure and Concomitant Risk of Mortality Differs According to the Type of Admission to ICU—A Retrospective Study of SOFA Score of 23,795 Patients. PLoS ONE 2015, 10, e0134329. [Google Scholar] [CrossRef]
- Lichte, P.; Kobbe, P.; Almahmoud, K.; Pfeifer, R.; Andruszkow, H.; Hildebrand, F.; Lefering, R.; Pape, H.C.; Trauma Register, D.G.U. Post-traumatic thrombo-embolic complications in polytrauma patients. Int. Orthop. 2015, 39, 947–954. [Google Scholar] [CrossRef]
- Peltan, I.D.; Vande Vusse, L.K.; Maier, R.V.; Watkins, T.R. An International Normalized Ratio-Based Definition of Acute Traumatic Coagulopathy Is Associated with Mortality, Venous Thromboembolism, and Multiple Organ Failure after Injury. Crit. Care Med. 2015, 43, 1429–1438. [Google Scholar] [CrossRef]
- Lefering, R.; Huber-Wagner, S.; Nienaber, U.; Maegele, M.; Bouillon, B. Update of the trauma risk adjustment model of the TraumaRegister DGU: The Revised Injury Severity Classification, version II. Crit. Care 2014, 18, 476. [Google Scholar] [CrossRef]
- Huber, S.; Biberthaler, P.; Delhey, P.; Trentzsch, H.; Winter, H.; van Griensven, M.; Lefering, R.; Huber-Wagner, S.; Trauma Register, D.G.U. Predictors of poor outcomes after significant chest trauma in multiply injured patients: A retrospective analysis from the German Trauma Registry (Trauma Register DGU (R)). Scand. J. Trauma. Resusc. Emerg. Med. 2014, 22, 52. [Google Scholar] [CrossRef]
- Wong, T.H.; Krishnaswamy, G.; Nadkarni, N.V.; Nguyen, H.V.; Lim, G.H.; Bautista, D.C.; Chiu, M.T.; Chow, K.Y.; Ong, M.E. Combining the new injury severity score with an anatomical polytrauma injury variable predicts mortality better than the new injury severity score and the injury severity score: A retrospective cohort study. Scand. J. Trauma. Resusc. Emerg. Med. 2016, 24, 25. [Google Scholar] [CrossRef]
- Weihs, V.; Heel, V.; Dedeyan, M.; Lang, N.W.; Frenzel, S.; Hajdu, S.; Heinz, T. Age and traumatic brain injury as prognostic factors for late-phase mortality in patients defined as polytrauma according to the New Berlin Definition: Experiences from a level I trauma center. Arch. Orthop. Trauma. Surg. 2021, 141, 1677–1681. [Google Scholar] [CrossRef]
- van Breugel, J.M.M.; Niemeyer, M.J.S.; Houwert, R.M.; Groenwold, R.H.H.; Leenen, L.P.H.; van Wessem, K.J.P. Global changes in mortality rates in polytrauma patients admitted to the ICU—A systematic review. World J. Emerg. Surg. 2020, 15, 55. [Google Scholar] [CrossRef] [PubMed]
- Wohltmann, C.D.; Franklin, G.A.; Boaz, P.W.; Luchette, F.A.; Kearney, P.A.; Richardson, J.D.; Spain, D.A. A multicenter evaluation of whether gender dimorphism affects survival after trauma. Am. J. Surg. 2001, 181, 297–300. [Google Scholar] [CrossRef] [PubMed]
- Schoeneberg, C.; Kauther, M.D.; Hussmann, B.; Keitel, J.; Schmitz, D.; Lendemans, S. Gender-specific differences in severely injured patients between 2002 and 2011: Data analysis with matched-pair analysis. Crit. Care 2013, 17, R277. [Google Scholar] [CrossRef] [PubMed]
- Larsson, E.; Lindstrom, A.C.; Eriksson, M.; Oldner, A. Impact of gender on post- traumatic intensive care and outcomes. Scand. J. Trauma. Resusc. Emerg. Med. 2019, 27, 115. [Google Scholar] [CrossRef]
- Joestl, J.; Lang, N.W.; Kleiner, A.; Platzer, P.; Aldrian, S. The Importance of Sex Differences on Outcome after Major Trauma: Clinical Outcome in Women versus Men. J. Clin. Med. 2019, 8, 1263. [Google Scholar] [CrossRef]
- Pape, M.; Giannakopoulos, G.F.; Zuidema, W.P.; de Lange-Klerk, E.S.M.; Toor, E.J.; Edwards, M.J.R.; Verhofstad, M.H.J.; Tromp, T.N.; van Lieshout, E.M.M.; Bloemers, F.W.; et al. Is there an association between female gender and outcome in severe trauma? A multi-center analysis in The Netherlands. Scand. J. Trauma. Resusc. Emerg. Med. 2019, 27, 16. [Google Scholar] [CrossRef]
- Yang, K.C.; Zhou, M.J.; Sperry, J.L.; Rong, L.; Zhu, X.G.; Geng, L.; Wu, W.; Zhao, G.; Billiar, T.R.; Feng, Q.M. Significant sex-based outcome differences in severely injured Chinese trauma patients. Shock 2014, 42, 11–15. [Google Scholar] [CrossRef]
- Fakhry, S.M.; Morse, J.L.; Garland, J.M.; Wilson, N.Y.; Shen, Y.; Wyse, R.J.; Watts, D.D. Redefining geriatric trauma: 55 is the new 65. J. Trauma. Acute Care Surg. 2021, 90, 738–743. [Google Scholar] [CrossRef]
- Choudhry, M.A.; Bland, K.I.; Chaudry, I.H. Trauma and immune response—Effect of gender differences. Injury 2007, 38, 1382–1391. [Google Scholar] [CrossRef]
- Aufmkolk, M.; Voggenreiter, G.; Majetschak, M.; Neudeck, F.; Schmit-Neuerburg, K.P.; Obertacke, U. Injuries due to falls from a great height. A comparative analysis of injuries and their outcome following suicide-related and accidental falls. Unfallchirurg 1999, 102, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Piazzalunga, D.; Ruberta, F.; Fugazzola, P.; Allievi, N.; Ceresoli, M.; Magnone, S.; Pisano, M.; Coccolini, F.; Tomasoni, M.; Montori, G.; et al. Suicidal fall from heights trauma: Difficult management and poor results. Eur. J. Trauma. Emerg. Surg. 2020, 46, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Shang, X.; Qi, P.; Ma, S. Sex-based differences in outcomes after severe injury: An analysis of blunt trauma patients in China. Scand. J. Trauma. Resusc. Emerg. Med. 2017, 25, 47. [Google Scholar] [CrossRef] [PubMed]
- Schoeneberg, C.; Schmitz, D.; Schoeneberg, S.; Hussmann, B.; Lendemans, S. Gender-specific differences in therapy and laboratory parameters and validation of mortality predictors in severely injured patients—Results of a German level 1 trauma center. Langenbecks Arch. Surg. 2015, 400, 781–790. [Google Scholar] [CrossRef]
- Weihs, V.; Frenzel, S.; Dedeyan, M.; Hruska, F.; Staats, K.; Hajdu, S.; Negrin, L.L.; Aldrian, S. 25-Year experience with adult polytraumatized patients in a European level 1 trauma center: Polytrauma between 1995 and 2019. What has changed? A retrospective cohort study. Arch. Orthop. Trauma. Surg. 2022, 143, 2409–2415. [Google Scholar] [CrossRef] [PubMed]
- James, S.L.; Theadom, A.; Ellenbogen, R.G.; Bannick, M.S.; Montjoy-Venning, W.; Lucchesi, L.R.; Abbasi, N.; Abdulkader, R.; Abraha, H.N.; Adsuar, J.C.; et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019, 18, 56–87. [Google Scholar] [CrossRef]
- Kristiansen, T.; Lossius, H.M.; Rehn, M.; Kristensen, P.; Gravseth, H.M.; Roislien, J.; Soreide, K. Epidemiology of trauma: A population-based study of geographical risk factors for injury deaths in the working-age population of Norway. Injury 2014, 45, 23–30. [Google Scholar] [CrossRef]
- de Vries, R.; Reininga, I.H.F.; de Graaf, M.W.; Heineman, E.; El Moumni, M.; Wendt, K.W. Older polytrauma: Mortality and complications. Injury 2019, 50, 1440–1447. [Google Scholar] [CrossRef]
- Yucel, N.; Ozturk Demir, T.; Derya, S.; Oguzturk, H.; Bicakcioglu, M.; Yetkin, F. Potential Risk Factors for In-Hospital Mortality in Patients with Moderate-to-Severe Blunt Multiple Trauma Who Survive Initial Resuscitation. Emerg. Med. Int. 2018, 2018, 6461072. [Google Scholar] [CrossRef]
- Callcut, R.A.; Kornblith, L.Z.; Conroy, A.S.; Robles, A.J.; Meizoso, J.P.; Namias, N.; Meyer, D.E.; Haymaker, A.; Truitt, M.S.; Agrawal, V.; et al. The why and how our trauma patients die: A prospective Multicenter Western Trauma Association study. J. Trauma. Acute Care Surg. 2019, 86, 864–870. [Google Scholar] [CrossRef] [PubMed]
| All Polytraumatized Patients (n = 980) | |
|---|---|
| Female sex | 30.3% (n = 297) |
| Male sex | 69.7% (n = 683) |
| Age (median) | 39 years (IQR 29) |
| Geriatric patients | 27.7% (n = 271) |
| ISS (median) | 34 points (IQR 16) |
| Injury mechanisms | |
| Traffic-related accident | 59.8% (n = 586) |
| Fall from greater height | 25.5% (n = 250) |
| Fall from lesser height | 6.1% (n = 60) |
| Penetrating injury | 2.7% (n = 26) |
| Other/unknown | 5.9% (n = 58) |
| Suicidal attempt | 19.7% (n = 190) |
| Survival | |
| Overall death | 29.3% (n = 287) |
| Acute-phase death | 19.1% (n = 187) |
| Late-phase death | 10.2% (n = 100) |
| Causes of death | |
| Trauma/hemorrhage | 14.5% (n = 142) |
| TBI | 9.5% (n = 93) |
| MOF | 2.6% (n = 25) |
| Injury pattern | |
| Head (AIS > 2) | 59.3% (n = 565) |
| Thorax (AIS > 2) | 78.1% (n = 742) |
| Abdomen (AIS > 2) | 35.7% (n = 337) |
| Pelvis/extremities (AIS > 2) | 55.0% (n = 521) |
| Spine (AIS > 2) | 13.1% (n = 123) |
| Female (n = 110) | Male (n = 161) | p Value | |
|---|---|---|---|
| Median age | 67.0 years of age (IQR 17) | ||
| Age | 70.18 ± 10.33 | 67.11 ± 10.03 | 0.008 * |
| Geriatric patients | |||
| Median ISS | 33 points (IQR 16) | ||
| ISS | 35.70 ± 14.52 | 33.51 ± 14.26 | 0.110 |
| Injury mechanism | |||
| Traffic-related accident | 62.8% (n = 68) | 58.4% (n = 94) | 0.899 |
| Fall from greater height | 15.5% (n = 17) | 18.0% (n = 29) | |
| Fall from lesser height | 16.4% (n = 18) | 14.9% (n = 24) | |
| Penetrating injury | 0.9% (n = 1) | 1.9% (n = 3) | |
| Other/unknown | 5.5% (n = 6) | 6.8% (n = 11) | |
| Suicidal attempt | 11.9% (n = 13) | 5.6% (n = 9) | 0.064 |
| Survival | |||
| Overall death | 46.4% (n = 51) | 36.6% (n = 59) | 0.110 |
| Acute-phase death | 27.3% (n = 30) | 18.6% (n = 30) | 0.093 |
| Late-phase death | 19.1% (n = 21) | 18.0% (n = 29) | 0.822 |
| Causes of death | |||
| Trauma/hemorrhage | 20.0% (n = 22) | 12.4% (n = 20) | 0.390 |
| TBI | 14.5% (n = 16) | 11.8% (n = 19) | |
| MOF | 4.5% (n = 5) | 6.2% (n = 10) | |
| Injury pattern | |||
| Head (AIS > 2) | 69.8% (n = 74) | 62.7% (n = 99) | 0.231 |
| Thorax (AIS > 2) | 75.7% (n = 81) | 75.3% (n = 119) | 0.943 |
| Abdomen (AIS > 2) | 24.3% (n = 25) | 26.1% (n = 40) | 0.736 |
| Pelvis/extremities (AIS > 2) | 57.0% (n = 61) | 49.7% (n = 77) | 0.243 |
| Spine (AIS > 2) | 10.8% (n = 11) | 10.7% (n = 16) | 0.976 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weihs, V.; Babeluk, R.; Negrin, L.L.; Aldrian, S.; Hajdu, S. Sex-Based Differences in Polytraumatized Patients between 1995 and 2020: Experiences from a Level I Trauma Center. J. Clin. Med. 2024, 13, 5998. https://doi.org/10.3390/jcm13195998
Weihs V, Babeluk R, Negrin LL, Aldrian S, Hajdu S. Sex-Based Differences in Polytraumatized Patients between 1995 and 2020: Experiences from a Level I Trauma Center. Journal of Clinical Medicine. 2024; 13(19):5998. https://doi.org/10.3390/jcm13195998
Chicago/Turabian StyleWeihs, Valerie, Rita Babeluk, Lukas L. Negrin, Silke Aldrian, and Stefan Hajdu. 2024. "Sex-Based Differences in Polytraumatized Patients between 1995 and 2020: Experiences from a Level I Trauma Center" Journal of Clinical Medicine 13, no. 19: 5998. https://doi.org/10.3390/jcm13195998
APA StyleWeihs, V., Babeluk, R., Negrin, L. L., Aldrian, S., & Hajdu, S. (2024). Sex-Based Differences in Polytraumatized Patients between 1995 and 2020: Experiences from a Level I Trauma Center. Journal of Clinical Medicine, 13(19), 5998. https://doi.org/10.3390/jcm13195998






