Effectiveness of Treating Obstructive Sleep Apnea by Surgeries and Continuous Positive Airway Pressure: Evaluation Using Objective Sleep Parameters and Patient-Reported Outcomes
Abstract
1. Introduction
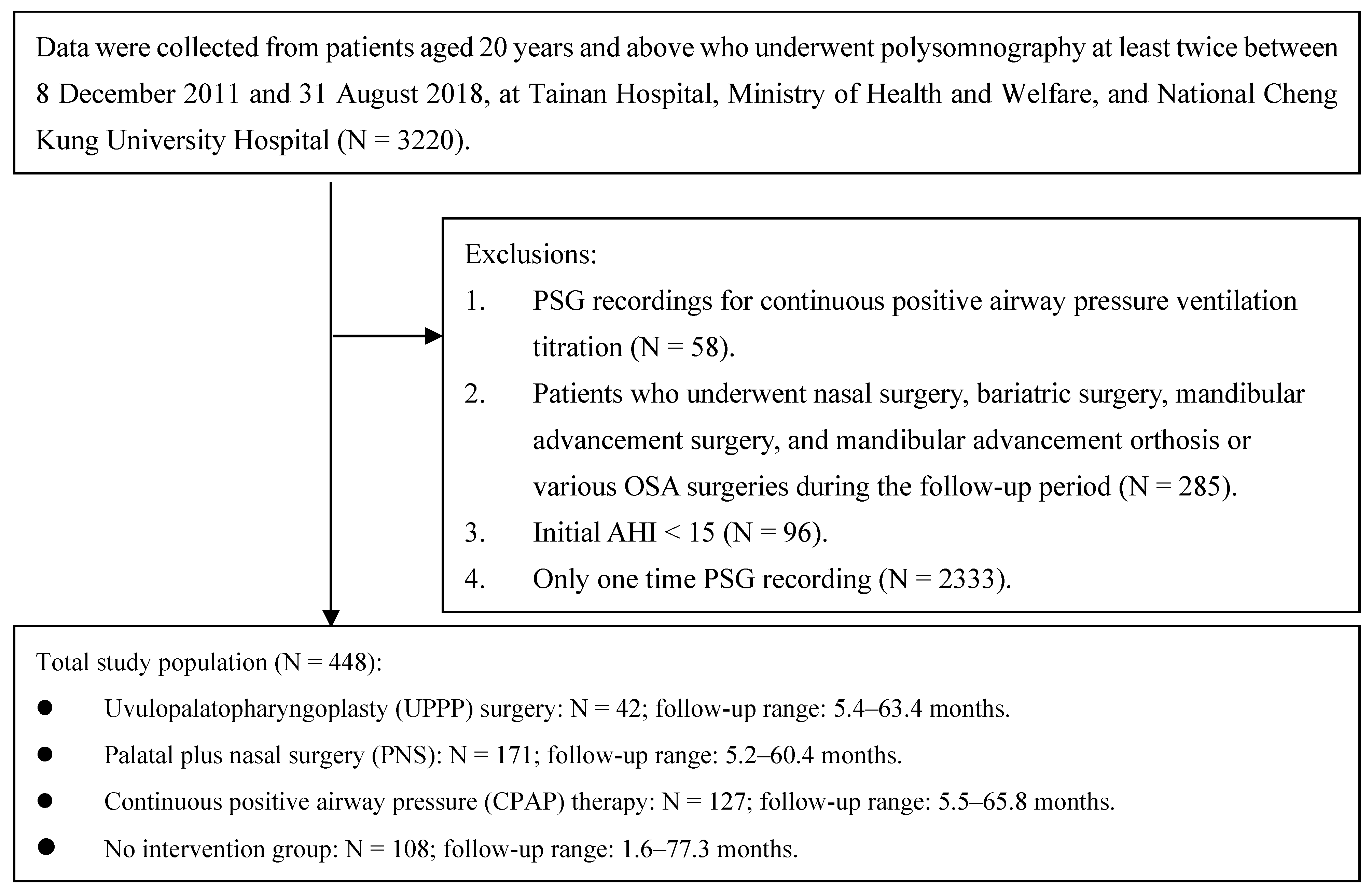
2. Materials and Methods
2.1. Study Population and Study Design
2.2. Outcome Measurement
2.2.1. Objective Sleep Parameters
2.2.2. Subjective Sleep Parameters (PROs)
2.2.3. Covariates
2.2.4. Follow-Up Time
2.3. Statistical Analysis
3. Results
3.1. Study Cohort
3.2. Mixed-Effect Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.-L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Lyons, M.M.; Bhatt, N.Y.; Pack, A.I.; Magalang, U.J. Global burden of sleep-disordered breathing and its implications. Respirology 2020, 25, 690–702. [Google Scholar] [CrossRef] [PubMed]
- Lavalle, S.; Masiello, E.; Iannella, G.; Magliulo, G.; Pace, A.; Lechien, J.R.; Calvo-Henriquez, C.; Cocuzza, S.; Parisi, F.M.; Favier, V.; et al. Unraveling the Complexities of Oxidative Stress and Inflammation Biomarkers in Obstructive Sleep Apnea Syndrome: A Comprehensive Review. Life 2024, 14, 425. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ouyang, Y.; Wang, Z.; Zhao, G.; Liu, L.; Bi, Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 2013, 169, 207–214. [Google Scholar] [CrossRef]
- Martinez-Garcia, M.A.; Campos-Rodriguez, F.; Barbé, F.; Gozal, D.; Agustí, A. Precision medicine in obstructive sleep apnoea. Lancet Respir. Med. 2019, 7, 456–464. [Google Scholar] [CrossRef]
- Knauert, M.; Naik, S.; Gillespie, M.B.; Kryger, M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J. Otorhinolaryngol.-Head Neck Surg. 2015, 1, 17–27. [Google Scholar] [CrossRef]
- Patil, S.P.; Ayappa, I.A.; Caples, S.M.; Kimoff, R.J.; Patel, S.R.; Harrod, C.G. Treatment of adult obstructive sleep apnea with positive airway pressure: An American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 2019, 15, 335–343. [Google Scholar] [CrossRef]
- Rotenberg, B.W.; Murariu, D.; Pang, K.P. Trends in CPAP adherence over twenty years of data collection: A flattened curve. J. Otolaryngol.-Head Neck Surg. 2016, 45, 43. [Google Scholar] [CrossRef]
- Kent, D.; Stanley, J.; Aurora, R.N.; Levine, C.G.; Gottlieb, D.J.; Spann, M.D.; Torre, C.A.; Green, K.; Harrod, C.G. Referral of adults with obstructive sleep apnea for surgical consultation: An American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J. Clin. Sleep Med. 2021, 17, 2507–2531. [Google Scholar] [CrossRef]
- Certal, V.; Nishino, N.; Camacho, M.; Capasso, R. Reviewing the systematic reviews in OSA surgery. Otolaryngol.-Head Neck Surg. 2013, 149, 817–829. [Google Scholar] [CrossRef]
- MacKay, S.; Carney, A.S.; Catcheside, P.G.; Chai-Coetzer, C.L.; Chia, M.; Cistulli, P.A.; Hodge, J.C.; Jones, A.; Kaambwa, B.; Lewis, R.; et al. Effect of multilevel upper airway surgery vs medical management on the apnea-hypopnea index and patient-reported daytime sleepiness among patients with moderate or severe obstructive sleep apnea: The SAMS randomized clinical trial. JAMA 2020, 324, 1168–1179. [Google Scholar] [CrossRef] [PubMed]
- Browaldh, N.; Nerfeldt, P.; Lysdahl, M.; Bring, J.; Friberg, D. SKUP3 randomised controlled trial: Polysomnographic results after uvulopalatopharyngoplasty in selected patients with obstructive sleep apnoea. Thorax 2013, 68, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.; Kim, E.J.; Kim, Y.S.; Kim, T.H.; Choi, J.; Kwon, S.Y.; Lee, H.M.; Lee, S.H.; Lee, S.H. Effectiveness of nasal surgery alone on sleep quality, architecture, position, and sleep-disordered breathing in obstructive sleep apnea syndrome with nasal obstruction. Am. J. Rhinol. Allergy 2011, 25, 338–341. [Google Scholar] [CrossRef]
- Rosvall, B.R.; Chin, C.J. Is uvulopalatopharyngoplasty effective in obstructive sleep apnea? Laryngoscope 2017, 127, 2201–2202. [Google Scholar] [CrossRef] [PubMed]
- Verse, T.; Maurer, J.T.; Pirsig, W. Effect of nasal surgery on sleep-related breathing disorders. Laryngoscope 2002, 112, 64–68. [Google Scholar] [CrossRef]
- Pack, A.I.; Magalang, U.J.; Singh, B.; Kuna, S.T.; Keenan, B.T.; Maislin, G. Randomized clinical trials of cardiovascular disease in obstructive sleep apnea: Understanding and overcoming bias. Sleep 2021, 44, zsaa229. [Google Scholar] [CrossRef] [PubMed]
- Real-World Data: Assessing Electronic Health Records and Medical Claims Data to Support Regulatory Decision-Making for Drug and Biological Products Draft Guidance for Industry. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/real-world-data-assessing-electronic-health-records-and-medical-claims-data-support-regulatory (accessed on 4 December 2021).
- Zinchuk, A.; Yaggi, H.K. Phenotypic subtypes of OSA: A challenge and opportunity for precision medicine. Chest 2020, 157, 403–420. [Google Scholar] [CrossRef]
- Continuous Positive Airway Pressure (CPAP) Devices, Accessories, & Therapy. 2024. Available online: https://www.medicare.gov/coverage/continuous-positive-airway-pressure-devices (accessed on 15 March 2024).
- Billings, M.E.; Kapur, V.K. Medicare long-term CPAP coverage policy: A cost-utility analysis. J. Clin. Sleep Med. 2013, 9, 1023–1029. [Google Scholar] [CrossRef]
- 0 Respiratory Equipment and Supplies Benefits List. 2024. Available online: https://www.sac-isc.gc.ca/eng/1585323161648/1585323186650#s8-2-1 (accessed on 15 March 2024).
- Guest, J.F.; Helter, M.T.; Morga, A.; Stradling, J.R. Cost-effectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax 2008, 63, 860–865. [Google Scholar] [CrossRef]
- Nakamura, H.; Kanemura, T.; Takara, C.; Tsukayama, A.; Tohyama, K.; Matsumoto, T.; Iseki, K. A retrospective analysis of 4000 patients with obstructive sleep apnea in Okinawa, Japan. Sleep Biol. Rhythm. 2009, 7, 103–112. [Google Scholar] [CrossRef]
- Carberry, J.C.; Amatoury, J.; Eckert, D.J. Personalized management approach for OSA. Chest 2018, 153, 744–755. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhou, T.; Huang, W.; Zhang, J.; Zou, J.; Guan, J.; Yi, H.; Yin, S. Differences in physiological endotypes between non-positional and positional obstructive sleep apnea: Results from Shanghai Sleep Health Study cohort. Chest 2024, 166, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Hilbert, J.; Yaggi, H.K. Patient-centered care in obstructive sleep apnea: A vision for the future. Sleep Med. Rev. 2018, 37, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.W.; Powell, N.B.; Guilleminault, C. Obstructive sleep apnea syndrome: A surgical protocol for dynamic upper airway reconstruction. J. Oral Maxillofac. Surg. 1993, 51, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.Y.-C.; Awad, M.; Riley, R.; Capasso, R. The role of the revised stanford protocol in today’s precision medicine. Sleep Med. Clin. 2019, 14, 99–107. [Google Scholar] [CrossRef]
- Liu, S.Y.-C.; Riley, R.W.; Yu, M.S. Surgical algorithm for obstructive sleep apnea: An update. Clin. Exp. Otorhinolaryngol. 2020, 13, 215. [Google Scholar] [CrossRef]
- Li, H.-Y. Palatal surgery for obstructive sleep apnea: From ablation to reconstruction. Sleep Med. Clin. 2019, 14, 51–58. [Google Scholar] [CrossRef]
- Ruehland, W.R.; Rochford, P.D.; O’dOnoghue, F.J.; Pierce, R.J.; Singh, P.; Thornton, A.T. The new AASM criteria for scoring hypopneas: Impact on the apnea hypopnea index. Sleep 2009, 32, 150–157. [Google Scholar] [CrossRef]
- Gliklich, R.E.; Wang, P.-C. Validation of the snore outcomes survey for patients with sleep-disordered breathing. Arch. Otolaryngol.-Head Neck Surg. 2002, 128, 819–824. [Google Scholar] [CrossRef]
- Chen, N.; Li, H.; Gliklich, R.E.; Chu, C.; Liang, S.; Wang, P. Validation assessment of the Chinese version of the Snore Outcomes Survey. Qual. Life Res. 2002, 11, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.; Wang, J.; Huang, P.; Chien, Y.; Chiu, C.; Lin, C. Integrating domain knowledge with machine learning to detect obstructive sleep apnea: Snore as a significant bio-feature. J. Sleep Res. 2022, 31, e13487. [Google Scholar] [CrossRef] [PubMed]
- Thiese, M.S.; Ronna, B.; Ott, U. P value interpretations and considerations. J. Thorac. Dis. 2016, 8, E928–E931. [Google Scholar] [CrossRef] [PubMed]
- Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 2009, 5, 263–276. [Google Scholar] [CrossRef]
- He, M.; Yin, G.; Zhan, S.; Xu, J.; Cao, X.; Li, J.; Ye, J. Long-term efficacy of uvulopalatopharyngoplasty among adult patients with obstructive sleep apnea: A systematic review and meta-analysis. Otolaryngol.-Head Neck Surg. 2019, 161, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Sundman, J.; Browaldh, N.; Fehrm, J.; Friberg, D. Eight-Year Follow-up of Modified Uvulopalatopharyngoplasty in Patients With Obstructive Sleep Apnea. Laryngoscope 2021, 131, E307–E313. [Google Scholar] [CrossRef] [PubMed]
- Pinczel, A.J.; Woods, C.M.; Catcheside, P.G.; Woodman, R.J.; Carney, A.S.; Chai-Coetzer, C.L.; Chia, M.; Cistulli, P.A.; Hodge, J.-C.; Jones, A.; et al. Sleep apnea multi-level surgery trial: Long-term observational outcomes. Sleep 2024, 47, zsad218. [Google Scholar] [CrossRef] [PubMed]
- Caples, S.M.; Rowley, J.A.; Prinsell, J.R.; Pallanch, J.F.; Elamin, M.B.; Katz, S.G.; Harwick, J.D. Surgical modifications of the upper airway for obstructive sleep apnea in adults: A systematic review and meta-analysis. Sleep 2010, 33, 1396–1407. [Google Scholar] [CrossRef]
- Stuck, B.A.; Ravesloot, M.J.; Eschenhagen, T.; de Vet, H.; Sommer, J.U. Uvulopalatopharyngoplasty with or without tonsillectomy in the treatment of adult obstructive sleep apnea–A systematic review. Sleep Med. 2018, 50, 152–165. [Google Scholar] [CrossRef] [PubMed]
- Woods, C.M.; Gunawardena, I.; Chia, M.; Vowles, N.J.; Ullah, S.; Robinson, S.; Carney, A.S. Long-term quality-of-life outcomes following treatment for adult obstructive sleep apnoea: Comparison of upper airway surgery, continuous positive airway pressure and mandibular advancement splints. Clin. Otolaryngol. 2016, 41, 762–770. [Google Scholar] [CrossRef]
- Tschopp, S.; Tschopp, K. Tonsil size and outcome of uvulopalatopharyngoplasty with tonsillectomy in obstructive sleep apnea. Laryngoscope 2019, 129, E449–E454. [Google Scholar] [CrossRef]
- Koay, C.B.; Freeland, A.P.; Stradling, J.R. Short-and long-term outcomes of uvulopalatopharyngoplasty for snoring. Clin. Otolaryngol. Allied Sci. 1995, 20, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Levin, B.C.; Becker, G.D. Uvulopalatopharyngoplasty for snoring: Long-term results. Laryngoscope 1994, 104, 1150–1152. [Google Scholar] [CrossRef] [PubMed]
- Fairbanks, D.N. Snoring: Surgical vs. nonsurgical management. Laryngoscope 1984, 94, 1188–1192. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Tripuraneni, P.; Gulati, A.; Stephens, E.M.; Nguyen, D.; Durr, M.L.; Chang, J.L. Patient-defined goals for obstructive sleep apnea treatment. Otolaryngol.-Head Neck Surg. 2022, 167, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Case, S.M.; O’Leary, J.; Kim, N.; Tinetti, M.E.; Fried, T.R. Older adults’ recognition of trade-offs in healthcare decision-making. J. Am. Geriatr. Soc. 2015, 63, 1658–1662. [Google Scholar] [CrossRef] [PubMed]
- Renoux, C.; Azoulay, L.; Suissa, S. Biases in evaluating the safety and effectiveness of drugs for the treatment of COVID-19: Designing real-world evidence studies. Am. J. Epidemiol. 2021, 190, 1452–1456. [Google Scholar] [CrossRef]
- Duce, B.; Milosavljevic, J.; Hukins, C. The 2012 AASM respiratory event criteria increase the incidence of hypopneas in an adult sleep center population. J. Clin. Sleep Med. 2015, 11, 1425–1431. [Google Scholar] [CrossRef]
| UPPP Surgery a (N = 42) | Palatal Plus Nasal Surgery (N = 171) | CPAP b (N = 127) | No Intervention (N = 108) | p-Value | |
|---|---|---|---|---|---|
| Age (mean [SD]) †‡§¶# | 44.0 (9.7) | 46.3 (11.3) | 51.9 (12.2) | 50.8 (13.4) | <0.001 |
| Female (No. [%]) # | 9 (21) | 29 (17) | 12 (9) | 30 (27) | 0.003 |
| BMI (mean [SD]) *§# | 29.6 (5) | 26.9 (3.8) | 29.8 (5.5) | 28 (5.2) | <0.001 |
| BMI < 25 (No. [%]) §# | 9 (21) | 51 (30) | 24 (19) | 33 (31) | <0.001 |
| 25 ≤ BMI < 30 (No. [%]) | 16 (38) | 90 (53) | 51 (40) | 52 (48) | |
| BMI ≥ 30 (No. [%]) | 17 (41) | 30 (18) | 52 (41) | 23 (21) | |
| Comorbidities | |||||
| Hypertension § | 18 (43) | 58 (34) | 71 (56) | 46 (43) | 0.002 |
| Diabetes § | 4 (9) | 7 (4) | 23 (18) | 13 (12) | 0.001 |
| Myocardial infarction | 0 (0) | 4 (2) | 3 (2) | 3 (3) | 0.773 |
| GERD f | 0 (0) | 2 (1) | 3 (2) | 6 (6) | 0.388 |
| Objective evaluation | |||||
| AHI (per hour) c (mean [SD]) *†§# | 53.1 (25.0) | 39.1 (18.4) | 66.0 (20.9) | 44.0 (21.6) | <0.001 |
| Minimum SpO2 (%, mean [SD]) †§# | 72.9 (11.3) | 74.5 (11.5) | 66.7 (13.5) | 74.8 (11.7) | <0.001 |
| Sleep efficiency (%, mean [SD]) | 82.0 (12.6) | 85.6 (9.0) | 82.2 (12.0) | 82.1 (12.6) | 0.019 |
| Patient-reported outcomes | |||||
| Self-reported snoring (SOS d questionnaire, mean [SD]) ¶# | 43.9 (13.2) | 43.4 (13.7) | 45 (14.3) | 50.2 (15.0) | 0.001 |
| Hypersomnia (ESS e questionnaire, mean [SD]) | 9.9 (4.4) | 10.6 (4.3) | 10.8 (4.8) | 9.9 (5.1) | 0.394 |
| Objective Sleep Parameters | Subjective Sleep Parameters | ||||
|---|---|---|---|---|---|
| Fixed Effect a | AHI d | Minimum SpO2 | Sleep Efficiency | Self-Reported Snoring (SOS e Questionnaire) | Hypersomnia (ESS f Questionnaire) |
| Treatment (ref: no treatment) | |||||
| UPPP surgery b | −14.59 (−22.36, −6.82) *** | 3.87 (0.12, 7.62) * | 5.98 (1.28,10.69) * | 25.97 (19.18, 32.75) *** | −3.53 (−5.32, −1.74) *** |
| Palatal plus nasal surgery | −5.98 (−9.56, −2.40) ** | 3.38 (1.66, 5.09) *** | 1.61 (−0.58, 3.81) | 22.23 (19.05, 25.40) *** | −1.62 (−2.44, −0.79) *** |
| CPAP c use at home | −4.74 (−8.69, −0.79) * | 3.96 (2.08, 5.85) *** | 0.15 (−2.28, 2.58) | 13.39 (9.87, 16.92) *** | −1.29 (−2.20, −0.37) ** |
| Follow-up time (per month) | 0.02 (−0.11, 0.16) | 0.06 (−0.001, 0.13) | −0.004(−0.08,0.00) | 0.23 (0.11, 0.34) *** | −0.005 (−0.04, 0.03) |
| Interaction with post-treatment time g (per month) | |||||
| UPPP surgery | −0.03 (−0.76, 0.70) | 0.01 (−0.34, 0.36) | −0.25 (−0.70, 0.19) | −0.79 (−1.42, −0.15) * | 0.04 (−0.13, 0.21) |
| Palatal plus nasal surgery | −0.17 (−0.44, 0.11) | −0.10 (−0.23, 0.03) | −0.04 (−0.20, 0.13) | −0.58 (−0.82, −0.34) *** | 0.03 (−0.04, 0.09) |
| CPAP use at home | 0.12 (−0.10, 0.32) | −0.003 (−0.10, 0.10) | −0.10 (−0.23, 0.03) | −0.41 (−0.59, −0.22) *** | 0.03 (−0.02, 0.08) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, Y.-C.; Wang, J.-D.; Chang, S.-M.; Chiu, C.-J.; Chien, Y.-W.; Lin, C.-Y. Effectiveness of Treating Obstructive Sleep Apnea by Surgeries and Continuous Positive Airway Pressure: Evaluation Using Objective Sleep Parameters and Patient-Reported Outcomes. J. Clin. Med. 2024, 13, 5748. https://doi.org/10.3390/jcm13195748
Hsu Y-C, Wang J-D, Chang S-M, Chiu C-J, Chien Y-W, Lin C-Y. Effectiveness of Treating Obstructive Sleep Apnea by Surgeries and Continuous Positive Airway Pressure: Evaluation Using Objective Sleep Parameters and Patient-Reported Outcomes. Journal of Clinical Medicine. 2024; 13(19):5748. https://doi.org/10.3390/jcm13195748
Chicago/Turabian StyleHsu, Yu-Ching, Jung-Der Wang, Sheng-Mao Chang, Ching-Ju Chiu, Yu-Wen Chien, and Cheng-Yu Lin. 2024. "Effectiveness of Treating Obstructive Sleep Apnea by Surgeries and Continuous Positive Airway Pressure: Evaluation Using Objective Sleep Parameters and Patient-Reported Outcomes" Journal of Clinical Medicine 13, no. 19: 5748. https://doi.org/10.3390/jcm13195748
APA StyleHsu, Y.-C., Wang, J.-D., Chang, S.-M., Chiu, C.-J., Chien, Y.-W., & Lin, C.-Y. (2024). Effectiveness of Treating Obstructive Sleep Apnea by Surgeries and Continuous Positive Airway Pressure: Evaluation Using Objective Sleep Parameters and Patient-Reported Outcomes. Journal of Clinical Medicine, 13(19), 5748. https://doi.org/10.3390/jcm13195748







