Mechanical versus Biological Valve Prostheses for Infective Endocarditis Presenting with Stroke
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Patients and Clinical Data
2.3. Study Outcomes
2.4. Statistical Analysis
3. Results
- Baseline characteristics
- Detected pathogens in the blood culture
- Neurological and radiological characteristics
- Operative characteristics
- Postoperative in-hospital adverse events
- Antithrombotic therapy
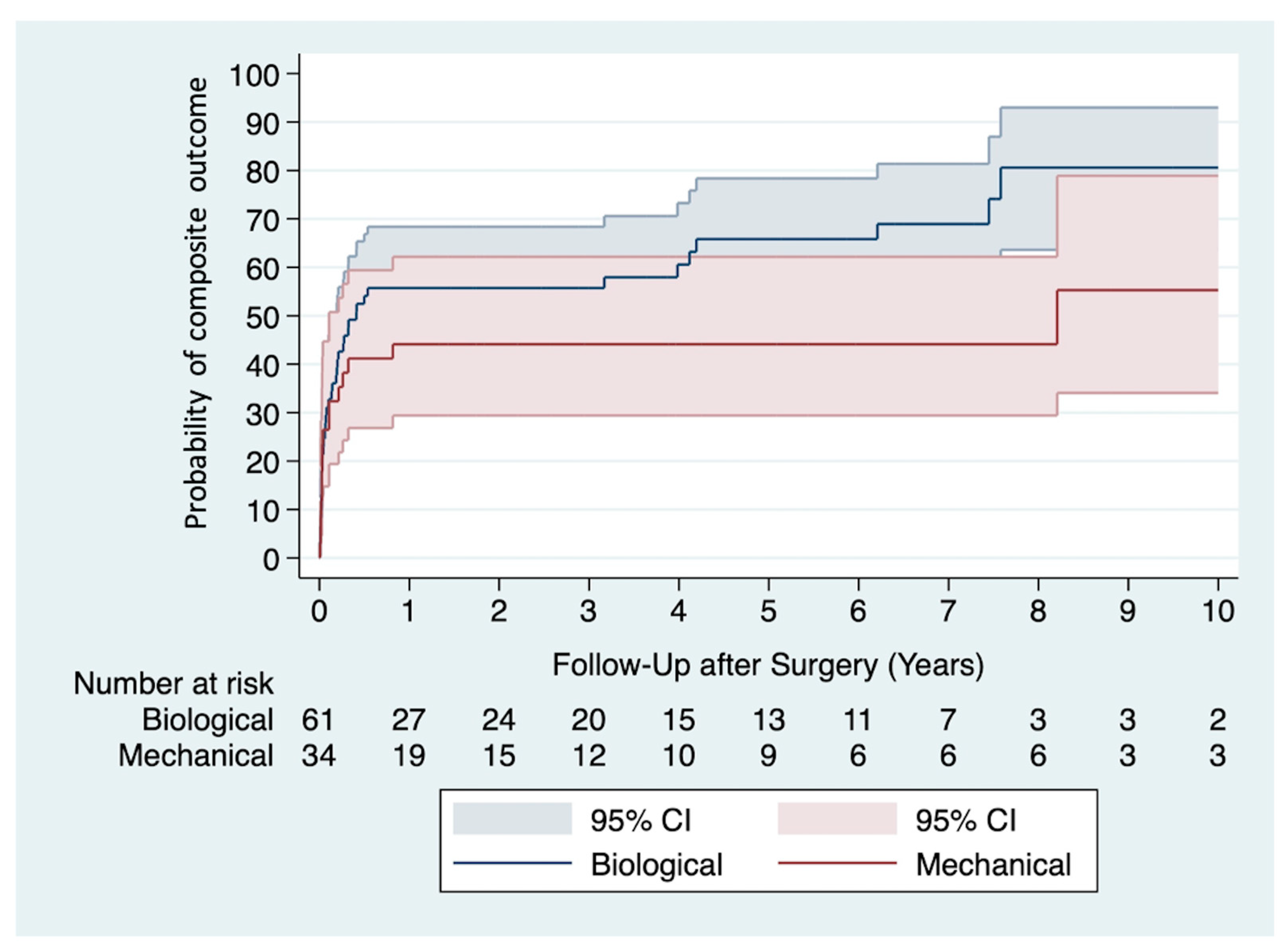
- Primary study outcome—Composite outcome
- Secondary study outcomes
- Causes of death
4. Discussion
5. Study Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AVR | Aortic valve replacement |
| CABG | Coronary artery bypass grafting |
| CI | Confidence interval |
| CPB | Cardiopulmonary bypass |
| ECMO | Extracorporeal Membrane Oxygenation |
| Euro SCORE II | European System for Cardiac Operative Risk Evaluation II |
| HR | Hazard ratio |
| IE | Infective endocarditis |
| IQR | Interquartile range |
| mRS | modified Rankin Scale |
| MVR | Mitral valve replacement |
| OR | Odds Ratio |
References
- Thuny, F.; Avierinos, J.-F.; Tribouilloy, C.; Giorgi, R.; Casalta, J.-P.; Milandre, L.; Brahim, A.; Nadji, G.; Riberi, A.; Collart, F.; et al. Impact of cerebrovascular complications on mortality and neurologic outcome during infective endocarditis: A prospective multicentre study. Eur. Heart J. 2007, 28, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Barsic, B.; Dickerman, S.; Krajinovic, V.; Pappas, P.; Altclas, J.; Carosi, G.; Casabé, J.H.; Chu, V.H.; Delahaye, F.; Edathodu, J.; et al. Influence of the Timing of Cardiac Surgery on the Outcome of Patients with Infective Endocarditis and Stroke. Clin. Infect. Dis. 2013, 56, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Delgado, V.; Marsan, N.A.; de Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. 2023 ESC Guidelines for the management of endocarditis. Eur. Heart J. 2023, 44, 3948–4042. [Google Scholar] [CrossRef] [PubMed]
- AATS Surgical Treatment of Infective Endocarditis Consensus Guidelines Writing Committee Chairs; Pettersson, G.B.; Coselli, J.S.; Hussain, S.T.; Griffin, B.; Blackstone, E.H.; Gordon, S.M.; LeMaire, S.A.; Woc-Colburn, L.E. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: Surgical treatment of infective endocarditis: Executive summary. J. Thorac. Cardiovasc. Surg. 2017, 153, 1241–1258.e29. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 60, 727–800. [Google Scholar] [CrossRef]
- Klein, C.F.; Gørtz, S.; Wohlfahrt, J.; Munch, T.N.; Melbye, M.; Bundgaard, H.; Iversen, K.K. Long-term Risk of Hemorrhagic Stroke in Patients with Infective Endocarditis: A Danish Nationwide Cohort Study. Clin. Infect. Dis. 2019, 68, 668–675. [Google Scholar] [CrossRef]
- García-Cabrera, E.; Fernández-Hidalgo, N.; Almirante, B.; Ivanova-Georgieva, R.; Noureddine, M.; Plata, A.; Lomas, J.M.; Gálvez-Acebal, J.; Hidalgo-Tenorio, C.; Ruíz-Morales, J.; et al. Neurological complications of infective endocarditis: Risk factors, outcome, and impact of cardiac surgery: A multicenter observational study. Circulation 2013, 127, 2272–2284. [Google Scholar] [CrossRef]
- Friberg, L.; Rosenqvist, M.; Lip, G.Y. Net clinical benefit of warfarin in patients with atrial fibrillation: A report from the Swedish atrial fibrillation cohort study. Circulation 2012, 125, 2298–2307. [Google Scholar] [CrossRef]
- Xian, Y.; Wu, J.; O’brien, E.C.; Fonarow, G.C.; Olson, D.M.; Schwamm, L.H.; Bhatt, D.L.; E Smith, E.; E Suter, R.; Hannah, D.; et al. Real world effectiveness of warfarin among ischemic stroke patients with atrial fibrillation: Observational analysis from Patient-Centered Research into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) study. BMJ 2015, 351, h3786. [Google Scholar] [CrossRef]
- Kleindorfer, D.O.; Towfighi, A.; Chaturvedi, S.; Cockroft, K.M.; Gutierrez, J.; Lombardi-Hill, D.; Kamel, H.; Kernan, W.N.; Kittner, S.J.; Leira, E.C.; et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke 2021, 52, e364–e467. [Google Scholar] [CrossRef]
- Biffi, A.; Kuramatsu, J.B.; Leasure, A.; Kamel, H.; Kourkoulis, C.; Schwab, K.; Ayres, A.M.; Elm, J.; Gurol, M.E.; Greenberg, S.M.; et al. Oral Anticoagulation and Functional Outcome after Intracerebral Hemorrhage. Ann. Neurol. 2017, 82, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Dvir, D.; Bourguignon, T.; Otto, C.M.; Hahn, R.T.; Rosenhek, R.; Webb, J.G.; Treede, H.; Sarano, M.E.; Feldman, T.; Wijeysundera, H.C.; et al. Standardized Definition of Structural Valve Degeneration for Surgical and Transcatheter Bioprosthetic Aortic Valves. Circulation 2018, 137, 388–399. [Google Scholar] [CrossRef] [PubMed]
- Li, J.S.; Sexton, D.J.; Mick, N.; Nettles, R.; Fowler, V.G., Jr.; Ryan, T.; Bashore, T.; Corey, G.R. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin. Infect. Dis. 2000, 30, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Caplan, L.R.; Connors, J.J.; Culebras, A.; Elkind, M.S.; George, M.G.; Hamdan, A.D.; Higashida, R.T.; et al. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 2064–2089. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.L.; Marotta, C.A. Outcomes validity and reliability of the modified Rankin scale: Implications for stroke clinical trials: A literature review and synthesis. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef]
- Sorabella, R.A.; Han, S.M.; Grbic, M.; Wu, Y.S.; Takyama, H.; Kurlansky, P.; Borger, M.A.; Argenziano, M.; Gordon, R.; George, I. Early Operation for Endocarditis Complicated by Preoperative Cerebral Emboli Is Not Associated With Worsened Outcomes. Ann. Thorac. Surg. 2015, 100, 501–508. [Google Scholar] [CrossRef]
- Samura, T.; Yoshioka, D.; Toda, K.; Sakaniwa, R.; Yokoyama, J.; Suzuki, K.; Miyagawa, S.; Yoshikawa, Y.; Hata, H.; Takano, H.; et al. Emergency valve surgery improves clinical results in patients with infective endocarditis complicated with acute cerebral infarction: Analysis using propensity score matching. Eur. J. Cardiothorac. Surg. 2019, 56, 942–949. [Google Scholar] [CrossRef]
- Bonaros, N.; Czerny, M.; Pfausler, B.; Müller, S.; Bartel, T.; Thielmann, M.; Shehada, S.-E.; Folliguet, T.; Obadia, J.-F.; Holfeld, J.; et al. Infective endocarditis and neurologic events: Indications and timing for surgical interventions. Eur. Heart J. Suppl. 2020, 22, M19–M25. [Google Scholar] [CrossRef]
- Ruttmann, E.; Abfalterer, H.; Wagner, J.; Grimm, M.; Müller, L.; Bates, K.; Ulmer, H.; Bonaros, N. Endocarditis-related stroke is not a contraindication for early cardiac surgery: An investigation among 440 patients with left-sided endocarditis. Eur. J. Cardiothorac. Surg. 2020, 58, 1161–1167. [Google Scholar] [CrossRef]
- Murai, R.; Kaji, S.; Kitai, T.; Kim, K.; Ota, M.; Koyama, T.; Furukawa, Y. The Clinical Significance of Cerebral Microbleeds in Infective Endocarditis Patients. Semin. Thorac. Cardiovasc. Surg. 2019, 31, 51–58. [Google Scholar] [CrossRef]
- Kume, Y.; Fujita, T.; Fukushima, S.; Shimahara, Y.; Matsumoto, Y.; Yamashita, K.; Kawamoto, N.; Kobayashi, J. Intracranial mycotic aneurysm is associated with cerebral bleeding post-valve surgery for infective endocarditis. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Salaun, E.; Touil, A.; Hubert, S.; Casalta, J.-P.; Gouriet, F.; Robinet-Borgomano, E.; Doche, E.; Laksiri, N.; Rey, C.; Lavoute, C.; et al. Intracranial haemorrhage in infective endocarditis. Arch. Cardiovasc. Dis. 2018, 111, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Okita, Y.; Minakata, K.; Yasuno, S.; Uozumi, R.; Sato, T.; Ueshima, K.; Konishi, H.; Morita, N.; Harada, M.; Kobayashi, J.; et al. Optimal timing of surgery for active infective endocarditis with cerebral complications: A Japanese multicentre study. Eur. J. Cardiothorac. Surg. 2016, 50, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Goldstone, A.B.; Chiu, P.; Baiocchi, M.; Lingala, B.; Patrick, W.L.; Fischbein, M.P.; Woo, Y.J. Mechanical or Biologic Prostheses for Aortic-Valve and Mitral-Valve Replacement. N. Engl. J. Med. 2017, 377, 1847–1857. [Google Scholar] [CrossRef] [PubMed]
- Glaser, N.; Jackson, V.; Holzmann, M.J.; Franco-Cereceda, A.; Sartipy, U. Aortic valve replacement with mechanical vs. biological prostheses in patients aged 50–69 years. Eur. Heart J. 2016, 37, 2658–2667. [Google Scholar] [CrossRef]
- Cannegieter, S.C.; Rosendaal, F.R.; Briët, E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 1994, 89, 635–641. [Google Scholar] [CrossRef]
- Chan, W.S.; Anand, S.; Ginsberg, J.S. Anticoagulation of pregnant women with mechanical heart valves: A systematic review of the literature. Arch. Intern. Med. 2000, 160, 191–196. [Google Scholar] [CrossRef]
- Kernan, W.N.; Ovbiagele, B.; Black, H.R.; Bravata, D.M.; Chimowitz, M.I.; Ezekowitz, M.D.; Fang, M.C.; Fisher, M.; Furie, K.L.; Heck, D.V.; et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45, 2160–2236. [Google Scholar] [CrossRef]
- Murai, R.; Funakoshi, S.; Kaji, S.; Kitai, T.; Kim, K.; Koyama, T.; Furukawa, Y. Outcomes of early surgery for infective endocarditis with moderate cerebral complications. J. Thorac. Cardiovasc. Surg. 2017, 153, 831–840.e8. [Google Scholar] [CrossRef]
- Diab, M.; Musleh, R.; Lehmann, T.; Sponholz, C.; Pletz, M.W.; Franz, M.; Schulze, P.C.; Witte, O.W.; Kirchhof, K.; Doenst, T.; et al. Risk of postoperative neurological exacerbation in patients with infective endocarditis and intracranial haemorrhage. Eur. J. Cardiothorac. Surg. 2021, 59, 426–433. [Google Scholar] [CrossRef]
- Said, S.M.; Abdelsattar, Z.M.; Schaff, H.V.; Greason, K.L.; Daly, R.C.; Pochettino, A.; Joyce, L.D.; Dearani, J.A. Outcomes of surgery for infective endocarditis: A single-centre experience of 801 patients. Eur. J. Cardiothorac. Surg. 2018, 53, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.T.; Delahaye, F.; Obadia, J.-F.; Duval, X.; Selton-Suty, C.; Carteaux, J.-P.; Hoen, B.; Alla, F.; for the AEPEI Study Group. Aortic valve replacement for active infective endocarditis: 5-year survival comparison of bioprostheses, homografts and mechanical prostheses. Eur. J. Cardiothorac. Surg. 2010, 37, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Musci, M.; Hübler, M.; Amiri, A.; Stein, J.; Kosky, S.; Meyer, R.; Weng, Y.; Hetzer, R. Surgical treatment for active infective prosthetic valve endocarditis: 22-year single-centre experience. Eur. J. Cardiothorac. Surg. 2010, 38, 528–538. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kahrovic, A.; Angleitner, P.; Herkner, H.; Kocher, A.; Ehrlich, M.; Laufer, G.; Andreas, M. Mechanical versus biological valve prostheses for left-sided infective endocarditis. Eur. J. Cardiothorac. Surg. 2022, 62, ezac056. [Google Scholar] [CrossRef]
- Anantha-Narayanan, M.; Reddy, Y.N.V.; Sundaram, V.; Murad, M.H.; Erwin, P.J.; Baddour, L.M.; Schaff, H.V.; A Nishimura, R. Endocarditis risk with bioprosthetic and mechanical valves: Systematic review and meta-analysis. Heart 2020, 106, 1413–1419. [Google Scholar] [CrossRef]
- Tao, E.; Wan, L.; Wang, W.; Luo, Y.; Zeng, J.; Wu, X. The prognosis of infective endocarditis treated with biological valves versus mechanical valves: A meta-analysis. PLoS ONE 2017, 12, e0174519. [Google Scholar] [CrossRef]
- Lee, H.-A.; Wu, V.C.-C.; Chan, Y.-S.; Cheng, Y.-T.; Lee, J.-K.; Chu, P.-H.; Chen, S.-W. Infective endocarditis after surgical aortic or mitral valve replacement: A nationwide population-based study. J. Thorac. Cardiovasc. Surg. 2023, 166, 1056–1068.e7. [Google Scholar] [CrossRef]
- Østergaard, L.; Valeur, N.; Ihlemann, N.; Smerup, M.H.; Bundgaard, H.; Gislason, G.; Torp-Pedersen, C.; Bruun, N.E.; Køber, L.; Fosbøl, E.L. Incidence and factors associated with infective endocarditis in patients undergoing left-sided heart valve replacement. Eur. Heart J. 2018, 39, 2668–2675. [Google Scholar] [CrossRef]
- Pizzino, F.; Paradossi, U.; Trimarchi, G.; Benedetti, G.; Marchi, F.; Chiappino, S.; Conti, M.; Di Bella, G.; Murzi, M.; Di Sibio, S.; et al. Clinical Features and Patient Outcomes in Infective Endocarditis with Surgical Indication: A Single-Centre Experience. J. Cardiovasc. Dev. Dis. 2024, 11, 138. [Google Scholar] [CrossRef]
- Piani, F.; Tossetta, G.; Cara-Fuentes, G.; Agnoletti, D.; Marzioni, D.; Borghi, C. Diagnostic and Prognostic Role of CD93 in Cardiovascular Disease: A Systematic Review. Biomolecules 2023, 13, 910. [Google Scholar] [CrossRef]
| Variables | Mechanical n = 34 (35.8%) | Biological n = 61 (64.2%) | p-Value |
|---|---|---|---|
| Age (years) (25th–75th interval) | 47.4 (41.6–56.7) | 65.1 (55.3–71.5) | <0.001 |
| Age > 55 years (%) | 10 (29.4) | 45 (73.8) | <0.001 |
| Female (%) | 10 (29.4) | 20 (32.8) | 0.734 |
| EuroSCORE II (25th–75th interval) | 7.5 (2.4–18.1) | 10.3 (5.2–24.6) | 0.073 |
| Ejection fraction > 60% (%) | 27 (79.4) | 49 (80.3) | 0.915 |
| Atrial fibrillation (%) | 10 (29.4) | 14 (23.0) | 0.487 |
| Hypertension (%) | 14 (41.2) | 42 (68.9) | 0.009 |
| Diabetes mellitus (%) | 3 (8.8) | 18 (29.5) | 0.020 |
| Dialysis (%) | 2 (5.9) | 7 (11.5) | 0.372 |
| Prosthetic valve endocarditis (%) | 6 (17.7) | 14 (23.0) | 0.543 |
| Positive blood culture (%) | 32 (94.1) | 59 (96.7) | 0.545 |
| Laboratory data (25th–75th interval) | |||
| C-reactive protein (mg/dL) | 6.0 (2.9–9.0) | 6.7 (3.8–14.1) | 0.244 |
| White blood cell count (G/L) | 8.5 (6.7–12.4) | 9.0 (7.1–12.7) | 0.650 |
| Lactate value (mmol/L) | 1.0 (0.7–1.5) | 1.0 (0.8–1.3) | 0.941 |
| Positive echocardiography findings | |||
| Vegetation (%) | 34 (100) | 52 (85.3) | 0.019 |
| Annular abscess (%) | 8 (23.5) | 17 (27.9) | 0.645 |
| Pseudoaneurysm (%) | 2 (5.9) | 1 (1.6) | 0.257 |
| Fistula (%) | 1 (2.9) | 1 (1.6) | 0.672 |
| Peripheral embolism (%) | 16 (47.1) | 37 (60.7) | 0.201 |
| Main indication for surgery | |||
| Heart failure (%) | 14 (41.2) | 16 (26.2) | 0.133 |
| Uncontrolled infection (%) | 10 (29.4) | 23 (37.7) | 0.416 |
| High embolic risk (%) | 10 (29.4) | 22 (36.1) | 0.511 |
| Preoperative antibiotic treatment (d) (25th–75th interval) | 14.0 (6.6–24.8) | 10.3 (6.4–22.4) | 0.342 |
| Variables | Mechanical n = 34 (35.8%) | Biological n = 61 (64.2%) | p-Value |
|---|---|---|---|
| Stroke prior to surgery | |||
| Ischemic (%) | 27 (79.4) | 49 (80.3) | 0.915 |
| Hemorrhagic (%) | 1 (2.9) | 4 (6.6) | 0.449 |
| Mixed lesion (%) | 6 (17.7) | 8 (13.1) | 0.550 |
| Time from stroke to surgery (d) (25th–75th interval) | 13.5 (3.4–29.4) | 10.0 (5.8–17.7) | 0.470 |
| Neurologic presentation at admission | |||
| mRS score ≥ 4 (%) | 16 (47.1) | 29 (47.5) | 0.964 |
| Motor control impairment (%) | 14 (41.2) | 28 (45.9) | 0.657 |
| Impaired consciousness (%) | 4 (11.8) | 17 (27.9) | 0.070 |
| Asymptomatic (%) | 7 (20.6) | 6 (9.8) | 0.144 |
| Brain area affected | |||
| Middle cerebral artery (%) | 11 (32.4) | 13 (21.3) | 0.235 |
| Multiple site (%) | 12 (35.3) | 20 (32.8) | 0.804 |
| Frontoparietal (%) | 7 (20.6) | 12 (19.7) | 0.915 |
| Temporal (%) | 3 (8.8) | 5 (8.2) | 0.916 |
| Occipital (%) | 4 (11.8) | 7 (11.5) | 0.966 |
| Cerebellum (%) | 0 (0.0) | 8 (13.1) | 0.027 |
| Brain Stem (%) | 2 (5.9) | 1 (1.6) | 0.257 |
| Basal ganglia (%) | 1 (2.9) | 9 (14.8) | 0.072 |
| Variables | Mechanical n = 34 (35.8%) | Biological n = 61 (64.2%) | p-Value |
|---|---|---|---|
| Urgency status | |||
| Urgent (%) | 28 (82.4) | 46 (75.4) | 0.434 |
| Emergent (%) | 6 (17.6) | 13 (21.3) | 0.669 |
| Salvage (%) | 0 (0.0) | 2 (3.3) | 0.056 |
| AVR (%) | 12 (35.3) | 25 (41.0) | 0.586 |
| MVR (%) | 18 (52.9) | 26 (42.6) | 0.334 |
| Combined AVR and MVR (%) | 4 (11.8) | 10 (16.4) | 0.542 |
| Right side involvement (%) | 2 (5.9) | 3 (4.9) | 0.840 |
| CABG (%) | 3 (8.8) | 12 (19.7) | 0.164 |
| Annular abscess exclusion (%) | 6 (17.6) | 18 (29.5) | 0.202 |
| Commando procedure (%) | 2 (5.9) | 0 (0.0) | 0.056 |
| Ventricular septal defect closure (%) | 1 (2.9) | 1 (1.6) | 0.672 |
| Aortic root enlargement (%) | 5 (14.7) | 2 (3.3) | 0.041 |
| Aortic root replacement (%) | 4 (11.8) | 2 (3.3) | 0.103 |
| CPB time (min) (25th–75th interval) | 148 (95–221) | 145 (108–192) | 0.951 |
| Cross-clamp time (min) (25th–75th interval) | 103 (63–164) | 103 (71–129) | 0.816 |
| Variables | HR | 95% CI | p-Value |
|---|---|---|---|
| Mechanical valve prosthesis a | 0.46 | 0.22–0.96 | 0.037 |
| Age > 55 years | 0.42 | 0.19–0.94 | 0.035 |
| EuroSCORE II (log-transformed) | 1.49 | 1.07–2.06 | 0.017 |
| Time from stroke to surgery (days) | 0.98 | 0.96–1.00 | 0.078 |
| Atrial fibrillation | 1.74 | 0.88–3.46 | 0.112 |
| Intravenous drug abuse | 0.99 | 0.40–2.43 | 0.984 |
| Prosthetic valve endocarditis | 0.82 | 0.40–1.67 | 0.579 |
| Annular abscess | 1.32 | 0.69–2.52 | 0.398 |
| Cross-clamp time (min) | 1.00 | 1.00–1.01 | 0.417 |
| Variables | Multivariable Relative Effects | p-Value |
|---|---|---|
| Ischemic stroke a | ||
| Mechanical valve prosthesis | 0.74 (0.24–2.24) | 0.590 |
| Hemorrhagic stroke a | ||
| Mechanical valve prosthesis | 0.31 (0.08–1.11) | 0.073 |
| Re-endocarditis a | ||
| Mechanical valve prosthesis | 0.15 (0.06–0.77) | 0.026 |
| All-cause mortality a | ||
| Mechanical valve prosthesis | 0.48 (0.21–1.09) | 0.081 |
| mRS deterioration during follow-up b | ||
| Mechanical valve prosthesis | 0.22 (0.05–1.02) | 0.053 |
| Variables | Mechanical n = 34 (35.8%) | Biological n = 61 (64.2%) | p-Value |
|---|---|---|---|
| Cardiac (%) | 4 (11.8) | 7 (11.5) | 0.966 |
| Infection (%) | 3 (8.8) | 10 (16.4) | 0.303 |
| Multi-organ failure (%) | 2 (5.9) | 3 (4.9) | 0.840 |
| Neurological (%) | 1 (2.9) | 4 (6.6) | 0.449 |
| Cancer (%) | 0 (0.0) | 3 (4.9) | 0.286 |
| Other (%) | 1 (2.9) | 3 (4.9) | 0.647 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kahrovic, A.; Angleitner, P.; Herkner, H.; Werner, P.; Andreeva, A.; Poschner, T.; Laengle, S.; Kocher, A.; Laufer, G.; Andreas, M. Mechanical versus Biological Valve Prostheses for Infective Endocarditis Presenting with Stroke. J. Clin. Med. 2024, 13, 5712. https://doi.org/10.3390/jcm13195712
Kahrovic A, Angleitner P, Herkner H, Werner P, Andreeva A, Poschner T, Laengle S, Kocher A, Laufer G, Andreas M. Mechanical versus Biological Valve Prostheses for Infective Endocarditis Presenting with Stroke. Journal of Clinical Medicine. 2024; 13(19):5712. https://doi.org/10.3390/jcm13195712
Chicago/Turabian StyleKahrovic, Amila, Philipp Angleitner, Harald Herkner, Paul Werner, Alexandra Andreeva, Thomas Poschner, Severin Laengle, Alfred Kocher, Guenther Laufer, and Martin Andreas. 2024. "Mechanical versus Biological Valve Prostheses for Infective Endocarditis Presenting with Stroke" Journal of Clinical Medicine 13, no. 19: 5712. https://doi.org/10.3390/jcm13195712
APA StyleKahrovic, A., Angleitner, P., Herkner, H., Werner, P., Andreeva, A., Poschner, T., Laengle, S., Kocher, A., Laufer, G., & Andreas, M. (2024). Mechanical versus Biological Valve Prostheses for Infective Endocarditis Presenting with Stroke. Journal of Clinical Medicine, 13(19), 5712. https://doi.org/10.3390/jcm13195712







