Prognostic Evaluation of Disorders of Consciousness by Using Resting-State fMRI: A Systematic Review
Abstract
1. Introduction
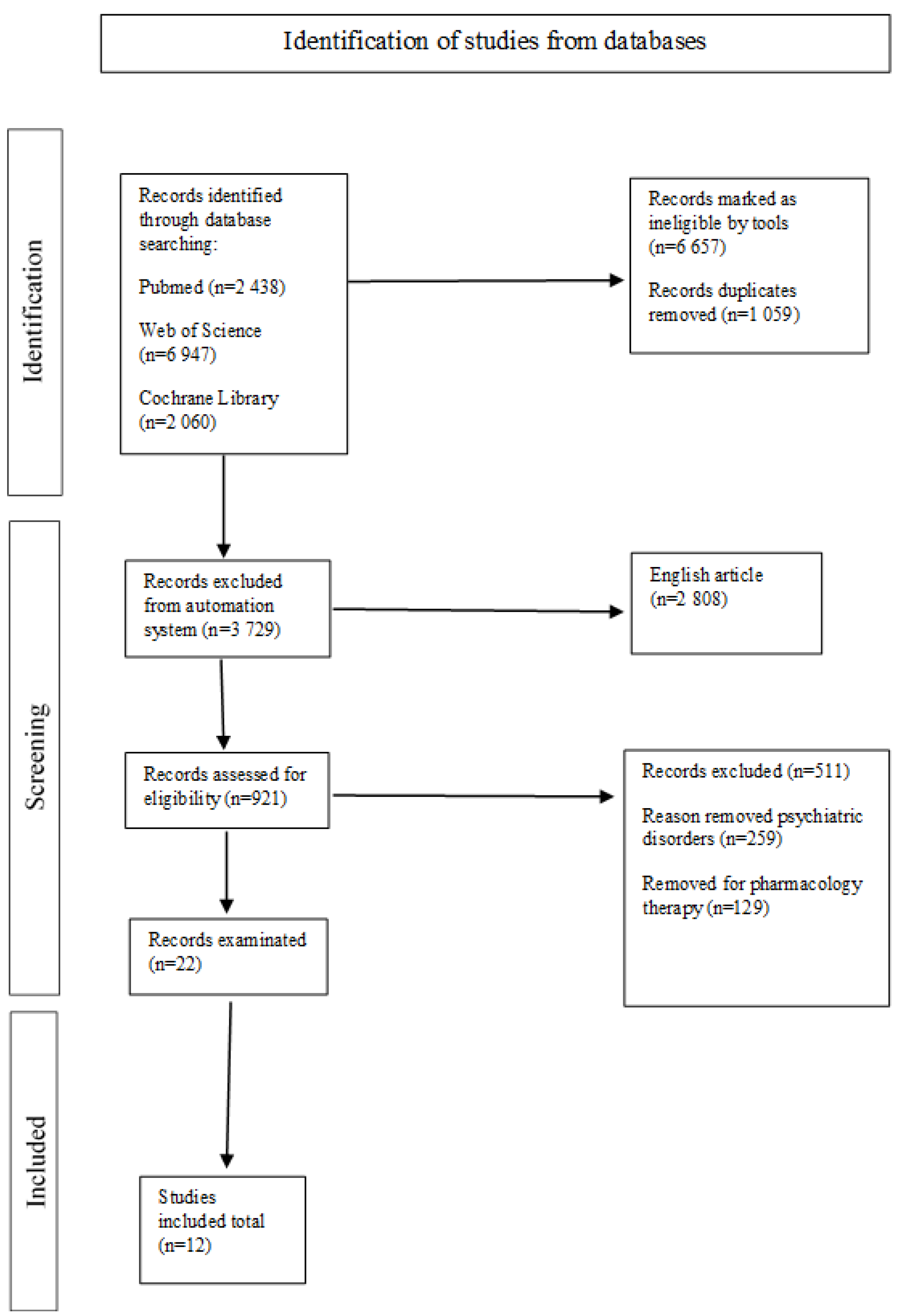
2. Materials and Methods
2.1. Information Sources and Search Approach
2.2. Selection and Data-Gathering Process
2.3. Data Elements
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MDPI | Multidisciplinary Digital Publishing Institute |
| DOAJ | Directory of open access journals |
| TLA | Three-letter acronym |
| LD | Linear dichroism |
References
- Giacino, J.T.; Ashwal, S.; Childs, N.; Cranford, R.; Jennett, B.; Katz, D.I.; Kelly, J.P.; Rosenberg, J.H.; Whyte, J.; Zafonte, R.D.; et al. The minimally conscious state: Definition and diagnostic criteria. Neurology 2002, 58, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T. The vegetative and minimally conscious states: Consensus-based criteria for establishing diagnosis and prognosis. NeuroRehabilitation 2004, 19, 393–398. [Google Scholar] [CrossRef]
- Eapen, B.C.; Georgekutty, J.; Subbarao, B.; Bavishi, S.; Cifu, D.X. Disorders of Consciousness. Phys. Med. Rehabil. Clin. 2017, 28, 245–258. [Google Scholar] [CrossRef]
- Giacino, J.T.; Katz, D.I.; Schiff, N.D.; Whyte, J.; Ashman, E.J.; Ashwal, S.; Barbano, R.; Hammond, F.M.; Laureys, S.; Ling, G.S.; et al. Practice guideline update recommendations summary: Disorders of consciousness. Neurology 2018, 91, 450–460. [Google Scholar] [CrossRef]
- Laureys, S.; Boly, M. What is it like to be vegetative or minimally conscious? Curr. Opin. Neurol. 2007, 20, 609–613. [Google Scholar] [CrossRef]
- Naccache, L. Minimally conscious state or cortically mediated state? Brain 2018, 141, 949–960. [Google Scholar] [CrossRef]
- Marino, S.; Bonanno, L.; Ciurleo, R.; Baglieri, A.; Morabito, R.; Guerrera, S.; Rifici, C.; Giorgio, A.; Bramanti, P.; De Stefano, N. Functional Evaluation of Awareness in Vegetative and Minimally Conscious State. Open Neuroimag J. 2017, 11, 17. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Montalcini, T.; Moraca, M.; Ferro, Y.; Romeo, S.; Serra, S.; Raso, M.G.; Rossi, F.; Sannita, W.G.; Dolce, G.; Pujia, A. Nutritional parameters predicting pressure ulcers and short-term mortality in patients with minimal conscious state as a result of traumatic and non-traumatic acquired brain injury. J. Transl. Med. 2015, 13, 305. [Google Scholar] [CrossRef]
- Mushkudiani, N.A.; Engel, D.C.; Steyerberg, E.W.; Butcher, I.; Lu, J.; Marmarou, A.; Slieker, F.; McHugh, G.S.; Murray, G.D.; Maas, A.I. Prognostic value of demographic characteristics in traumatic brain injury: Results from the IMPACT study. J. Neurotrauma 2007, 24, 259–269. [Google Scholar] [CrossRef]
- Pistoia, F.; Sacco, S.; Franceschini, M.; Sarà, M.; Pistarini, C.; Cazzulani, B.; Simonelli, I.; Pasqualetti, P.; Carolei, A. Comorbidities: A key issue in patients with disorders of consciousness. J. Neurotrauma 2015, 32, 682–688. [Google Scholar] [CrossRef]
- Soddu, A.; Vanhaudenhuyse, A.; Demertzi, A.; Bruno, M.A.; Tshibanda, L.; Di, H.; Mélanie, B.; Papa, M.; Laureys, S.; Noirhomme, Q. Resting state activity in patients with disorders of consciousness. Funct. Neurol. 2011, 26, 37–43. [Google Scholar] [PubMed]
- Laureys, S.; Schiff, N.D. Coma and consciousness: Paradigms (re)framed by neuroimaging. Neuroimage 2012, 61, 478–491. [Google Scholar] [CrossRef] [PubMed]
- Thibaut, A.; Schiff, N.; Giacino, J.; Laureys, S.; Gosseries, O. Therapeutic interventions in patients with prolonged disorders of consciousness. Lancet Neurol. 2019, 18, 600–614. [Google Scholar] [CrossRef]
- Raimondo, L.; Oliveira, Ĺ.A.F.; Heij, J.; Priovoulos, N.; Kundu, P.; Leoni, R.F.; van der Zwaag, W. Advances in resting state fMRI acquisitions for functional connectomics. Neuroimage 2021, 243, 118503. [Google Scholar] [CrossRef]
- Jackie, Y.; Suril, G.; Behroze, V. Current methods and new directions in resting state fMRI. Clin. Imaging 2020, 65, 47–53. [Google Scholar]
- Berlingeri, M.; Magnani, F.G.; Salvato, G.; Rosanova, M.; Bottini, G. Neuroimaging Studies on Disorders of Consciousness: A Meta-Analytic Evaluation. J. Clin. Med. 2019, 8, 516. [Google Scholar] [CrossRef]
- Kondziella, D.; Bender, A.; Diserens, K.; van Erp, W.; Estraneo, A.; Formisano, R.; Laureys, S.; Naccache, L.; Ozturk, S.; Rohaut, B.; et al. EAN Panel on Coma, Disorders of Consciousness. European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur. J. Neurol. 2020, 27, 741–756. [Google Scholar] [CrossRef]
- Cortese, M.D.; Riganello, F.; Arcuri, F.; Pugliese, M.E.; Lucca, L.F.; Dolce, G.; Sannita, W.G. Coma recovery scale-r: Variability in the disorder of consciousness. BMC Neurol. 2015, 15, 186. [Google Scholar] [CrossRef] [PubMed]
- Rossato, E.; Verzini, E.; Scandola, M.; Ferrari, F.; Bonadiman, S. Role of LCF scale as an outcome prognostic index in patients with traumatic brain injury. Neurol. Sci. 2021, 42, 2747–2752. [Google Scholar] [CrossRef]
- Wilson, L.; Boase, K.; Nelson, L.D.; Temkin, N.R.; Giacino, J.T.; Markowitz, A.J.; Maas, A.; Menon, D.K.; Teasdale, G.; Manley, G.T. A Manual for the Glasgow Outcome Scale-Extended Interview. J. Neurotrama 2021, 38, 2435–2446. [Google Scholar] [CrossRef]
- Bodien, Y.G.; Barra, A.; Temkin, N.R.; Barber, J.; Foreman, B.; Vassar, M.; Robertson, C.; Taylor, S.R.; Markowitz, A.J.; Manley, G.T.; et al. Diagnosing Level of Consciousness: The Limits of the Glasgow Coma Scale Total Score. J. Neurotrama 2021, 38, 3295–3305. [Google Scholar] [CrossRef]
- Green, S.M.; Haukoos, J.S.; Schriger, D.L. How to Measure the Glasgow Coma Scale. Ann. Emerg. Med. 2017, 70, 158–160. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Fins, J.J.; Laureys, S.; Schiff, N.D. Disorders of consciousness after acquired brain injury: The state of the science. Nat. Rev. Neurol. 2014, 10, 99–114. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Zasler, N.D.; Katz, D.I.; Kelly, J.P.; Rosenberg, J.H.; Filley, C.M. Development of practice guidelines for assessment and management of the vegetative and minimally conscious states. J. Head Trauma Rehabil. 1997, 12, 79–89. [Google Scholar] [CrossRef]
- Estraneo, A.; Moretta, P.; Loreto, V.; Santoro, L.; Trojano, L. Clinical and neuropsychological long-term outcomes after late recovery of responsiveness: A case series. Arch. Phys. Med. Rehabil. 2014, 95, 711–716. [Google Scholar] [CrossRef]
- Crone, J.S.; Ladurner, G.; Höller, Y.; Golaszewski, S.; Trinka, E.; Kronbichler, M. Deactivation of the default mode network as a marker of impaired consciousness: An fMRI study. PLoS ONE 2011, 6, e26373. [Google Scholar] [CrossRef]
- Kotchoubey, B.; Merz, S.; Lang, S.; Markl, A.; Müller, F.; Yu, T.; Schwarzbauer, C. Global functional connectivity reveals highly significant differences between the vegetative and the minimally conscious state. J. Neurol. 2013, 260, 975–983. [Google Scholar] [CrossRef]
- Silva, S.; De Pasquale, F.; Vuillaume, C.; Riu, B.; Loubinoux, I.; Geeraerts, T.; Seguin, T.; Bounes, V.; Fourcade, O.; Demonet, J.F.; et al. Disruption of posteromedial large-scale neural communication predicts recovery from coma. Neurology 2015, 85, 2036–2044. [Google Scholar] [CrossRef]
- Cao, B.; Guo, Y.; Xie, Q.; Chen, L.; Huang, H.; Yu, R.; Huang, R. Time-delay structure predicts clinical scores for patients with disorders of consciousness using resting-state fMRI. Neuroimage Clin. 2021, 32, 102797. [Google Scholar] [CrossRef]
- Medina, J.P.; Nigri, A.; Stanziano, M.; D’Incerti, L.; Sattin, D.; Ferraro, S.; Rossi, D.; Pinardi, C.; Marotta, G.; Leonardi, M.; et al. Resting-State fMRI in Chronic Patients with Disorders of Consciousness: The Role of Lower-Order Networks for Clinical Assessment. Brain Sci. 2022, 12, 355. [Google Scholar] [CrossRef]
- Di Perri, C.; Bahri, M.A.; Amico, E.; Thibaut, A.; Heine, L.; Antonopoulos, G.; Charland-Verville, V.; Wannez, S.; Gomez, F.; Hustinx, R.; et al. Neural correlates of consciousness in patients who have emerged from a minimally conscious state: A cross-sectional multimodal imaging study. Lancet Neurol. 2016, 15, 830–842. [Google Scholar] [CrossRef] [PubMed]
- Faugeras, F.; Rohaut, B.; Valente, M.; Sitt, J.; Demeret, S.; Bolgert, F.; Weiss, N.; Grinea, A.; Marois, C.; Quirins, M.; et al. Survival and consciousness recovery are better in the minimally conscious state than in the vegetative state. Brain Inj. 2018, 32, 72–77. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, S.; Xia, X.; Peng, Y.; Wu, B. Altered functional connectivity and regional brain activity in a triple-network model in minimally conscious state and vegetative-state/unresponsive wakefulness syndrome patients: A resting-state functional magnetic resonance imaging study. Front. Behav. Neurosci. 2022, 16, 1001519. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Meng, F.; Zhang, L.; Liu, X.; Wu, Y.; Chen, S.; Tan, X.; Li, X.; Kuang, S.; Sun, Y.; et al. A multi-domain prognostic model of disorder of consciousness using resting-state fMRI and laboratory parameters. Brain Imaging Behav. 2021, 15, 1966–1976. [Google Scholar] [CrossRef]
- Bodien, Y.G.; Giacino, J.T. Challenges and Pitfalls Associated with Diagnostic and Prognostic Applications of Functional Neuroimaging in Disorders of Consciousness. Open Neuroimag J. 2016, 10, 23. [Google Scholar] [CrossRef][Green Version]
- Edlow, B.L.; Claassen, J.; Schiff, N.D.; Greer, D.M. Recovery from disorders of consciousness: Mechanisms, prognosis and emerging therapies. Nat. Rev. Neurol. 2021, 17, 135–156. [Google Scholar] [CrossRef]
- Song, M.; Yang, Y.; He, J.; Yang, Z.; Yu, S.; Xie, Q.; Xia, X.; Dang, Y.; Zhang, Q.; Wu, X.; et al. Prognostication of chronic disorders of consciousness using brain functional networks and clinical characteristics. eLife 2018, 7, e36173. [Google Scholar] [CrossRef]
| Authors | Sample | Objective | Country | Diagnosis | Etiology | Time Since Diagnosis | Prognostic Factors | Data Acquisition | Treatment | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Estraneo, A. et al., 2014 [25] | 13 patients | Assessment of patients’ clinical condition and neuropsychological functioning. | Italy | 7 MCS 6 eMCS | 6 anoxia 6 closed head injury 1 hemorrhagic stroke | More than 12 months after onset in patients with head injury and more than 6 months post-onset in patients with non-TBI | Age, N20 cortical component preserved on one side | CRS-R Neuroimaging | NA | Assessment of the preserved N20 cortical component of somatosensory potentials evoked on at least one side revealed that 5 were still minimally conscious; 6 recovered some complex behavioral responses to the environment. |
| Crone, J.S. et al., 2011 [26] | 25 patients | To demonstrate DOCs that occurred in survivors of severe brain injury. Deactivation of the DMN is thought to reflect disruption of introspective processes. | Austria | 8 MCS 17 UWS | 12 traumatic 13 hypoxic | About 2 years | Correlation between the deactivation in the DMN and the level of consciousness. | CRS-R fMRI | Not applicable. | 17 patients (6 MCS patients; 11 UWS patients) showed no significant deactivation pattern. Deactivation in the medial regions of DMN was reduced in an MCS and absent in a UWS. |
| Kotchoubey, B. et al., 2013 [27] | 12 patients | In diagnosing disorders of consciousness, it is important to differentiate vegetative states from minimally conscious states. | Germany | 6 MCS 6 VS | 1 traumatic 7 anoxic 4 hemorrhagic | About 3 years | NA | CRS-R Functional connectivity | NA | Lack of connectivity between the posterior cingulate cortex and medial prefrontal cortex indicated that the patients had a loss of consciousness. |
| Stein, S. et al., 2015 [28] | 27 patients | The observation of a disruption in the long-range communication between neurons is a major deficit in DOCs when observing network impairment and correlation with clinical deficits. | France | 12 VS 11 MCS 4 other | 13 traumatic 15 anoxic | About 2 years | Specific pattern of connectivity from the pre-cuneus and posterior cingulate cortex | CRS-R fMRI | NA | Lack of connectivity between the posterior cingulate cortex and medial prefrontal cortex indicated that the patients had a loss of consciousness. |
| Cao, B. et al., 2021 [29] | 17 patients | Deficit structure predicts clinical outcomes in patients with disorders of consciousness using rs-fMRI in the resting state | China | 11 VS 6 MCS | 5 TBI 12 HIE | NA | Intrinsic brain activity imaging indicator | CRS-R fMRI | NA | DOC patients showed a time delay. Abnormalities in the precentral gyrus, pre-cuneus, middle cingulate cortex and postcentral gyrus. |
| Di Perri, C. et al., 2016 [31] | 58 patients | Study on DOCs to identify neural network dysfunction using imaging. | Belgium | 21 VS 24 MCS 13 eMCS | 29 TBI 14 anoxic 7 TBI/anoxic 8 other | About 5 years | NA | CRS-R Neuroimaging | NA | Resting-state neuroimaging suggests a specific brain organization that primarily involved the posterior cingulate cortex and adjacent pre-cuneus, as well as the anterior cingulate cortex and meso-frontal regions, which is known as the default mode network. |
| Medina, J.P. et al., 2022 [30] | 109 patients | Clarification of relevance to clinical evaluation | Italy | 34 MCS 65 VS 10 SD | 33 traumatic 39 vascular 37 anoxic | About 2 years | NA | CRS-R Neuroimaging techniques | NA | Correlative findings only suggest that visual networks could provide additional information about visual function in DOCs and may be functionally relevant to the patient’s level of consciousness. |
| Wang, Y. et al., 2022 [33] | 39 patients | Functional changes in regional brain connectivity and activity were examined in this study. | China | 14 MCS 25 VS | 14 TBI 15 ICH 10 others | NA | NA | CRS-R Resting-state fMRI | NA | The VS/UWS group showed reduced functional connectivity between the DMN and the SN, between the SN and the ECN, and within the SN compared with the MCS group. |
| Faugeras, F. et al., 2018 [32] | 67 patients | Determine whether patients diagnosed early on as minimally conscious (MCS) have a better prognosis. | France | 34 MCS 33 VS | 12 TBI 21 anoxia 14 ICH 20 other | About 5 years | Early diagnosis | CRS-R | NA | Early accurate clinical diagnosis of a VS/UWS or MCS had a strong prognostic value for survival and recovery of consciousness. |
| Yu, Y. 2020 [34] | 51 patients | To develop a prognostic model of DOC recovery using a combination of laboratory parameters and resting functional magnetic resonance imaging (fMRI). | China | 34 MCS 17 VS | TBI detail not specified | About 1 year | Information from neuroimaging and clinical parameters | CRS-R fMRI | NA | Combining information from the meso-frontoparietal cortex and the lower part of the brain may be a strategy to provide a more accurate prognosis. |
| Marino, S. et al., 2017 [7] | 50 patients | Differences in brain activation in a large sample of vegetative state (VS) and minimally conscious (MCS) patients using functional magnetic resonance imaging (fMRI). | Italy | 27 MCS 23 VS | 25 TBI 11 CVA 14 other | 4 to 7 months | fMRI could be a potentially reliable marker | CRS-R fMRI | NA | Significant bilateral brain activation in the primary auditory cortex during acoustic stimuli in patients with both VS and MCS. |
| Bodien, Y.G. et al., 2016 [35] | 54 patients | Accurate diagnosis of the patient’s level of consciousness is critical to determining the treatment objectives, access to rehabilitation services and the prognosis markers. | USA | 31 MCS 23 VS | TBI detail not specified | NA | NA | CRS-R fMRI | NA | The use of motor imagery to detect consciousness was not accurate. |
| Authors | Improvement | Differences in Activation Status |
|---|---|---|
| Estraneo, A., et al., 2014 [25] | Recovery of some behavioural responses to the environment. | |
| Stein, S.; et al., 2015 [28] | VS/MCS group showed improvements. | |
| Marino, S., et al., 2017 [7] | Ten patients with VS had a significant clinical improvement, evolving into MCS. | |
| Bodien, Y.G., et al., 2016 [35] | Presence of improvement from VS/MCS. | |
| Crone, J.S., et al., 2011 [26] | Deactivation of the network in default mode as an indicator of compromised Consciousness. | |
| Kotchoubey, B., et al., 2013 [27] | Activation status in different areas in VS/MCS. | |
| Cao, B., et al., 2021 [29] | Brain activity detection. | |
| Di Perri, C., et al., 2016 [31] | Neuronal correlation. | |
| Medina, J.P., et al., 2022 [30] | Exploring the residual functional activity of patients’ brains in relation to clinical data. | |
| Wang, Y., et al., 2022 [33] | Understanding the underlying neural mechanism of functional connectivity. | |
| Faugeras, F., et al., 2018 [32] | Importance of an early and strict distinction between VS/MCS. | |
| Yu, Y., 2020 [34] | Activity visualisation models. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le Cause, M.; Bonanno, L.; Alagna, A.; Bonanno, C.; De Caro, J.; Logiudice, A.L.; Pollicino, P.; Corallo, F.; De Salvo, S.; Rifici, C.; et al. Prognostic Evaluation of Disorders of Consciousness by Using Resting-State fMRI: A Systematic Review. J. Clin. Med. 2024, 13, 5704. https://doi.org/10.3390/jcm13195704
Le Cause M, Bonanno L, Alagna A, Bonanno C, De Caro J, Logiudice AL, Pollicino P, Corallo F, De Salvo S, Rifici C, et al. Prognostic Evaluation of Disorders of Consciousness by Using Resting-State fMRI: A Systematic Review. Journal of Clinical Medicine. 2024; 13(19):5704. https://doi.org/10.3390/jcm13195704
Chicago/Turabian StyleLe Cause, Maria, Lilla Bonanno, Antonella Alagna, Carmen Bonanno, Jolanda De Caro, Anna Lisa Logiudice, Patrizia Pollicino, Francesco Corallo, Simona De Salvo, Carmela Rifici, and et al. 2024. "Prognostic Evaluation of Disorders of Consciousness by Using Resting-State fMRI: A Systematic Review" Journal of Clinical Medicine 13, no. 19: 5704. https://doi.org/10.3390/jcm13195704
APA StyleLe Cause, M., Bonanno, L., Alagna, A., Bonanno, C., De Caro, J., Logiudice, A. L., Pollicino, P., Corallo, F., De Salvo, S., Rifici, C., Quartarone, A., & Marino, S. (2024). Prognostic Evaluation of Disorders of Consciousness by Using Resting-State fMRI: A Systematic Review. Journal of Clinical Medicine, 13(19), 5704. https://doi.org/10.3390/jcm13195704






