Type 4 Tibial Tuberosity Avulsion Fractures: Surgical Treatment Early Outcomes and a Presentation of the Distal Cortical Fixation
Abstract
1. Introduction
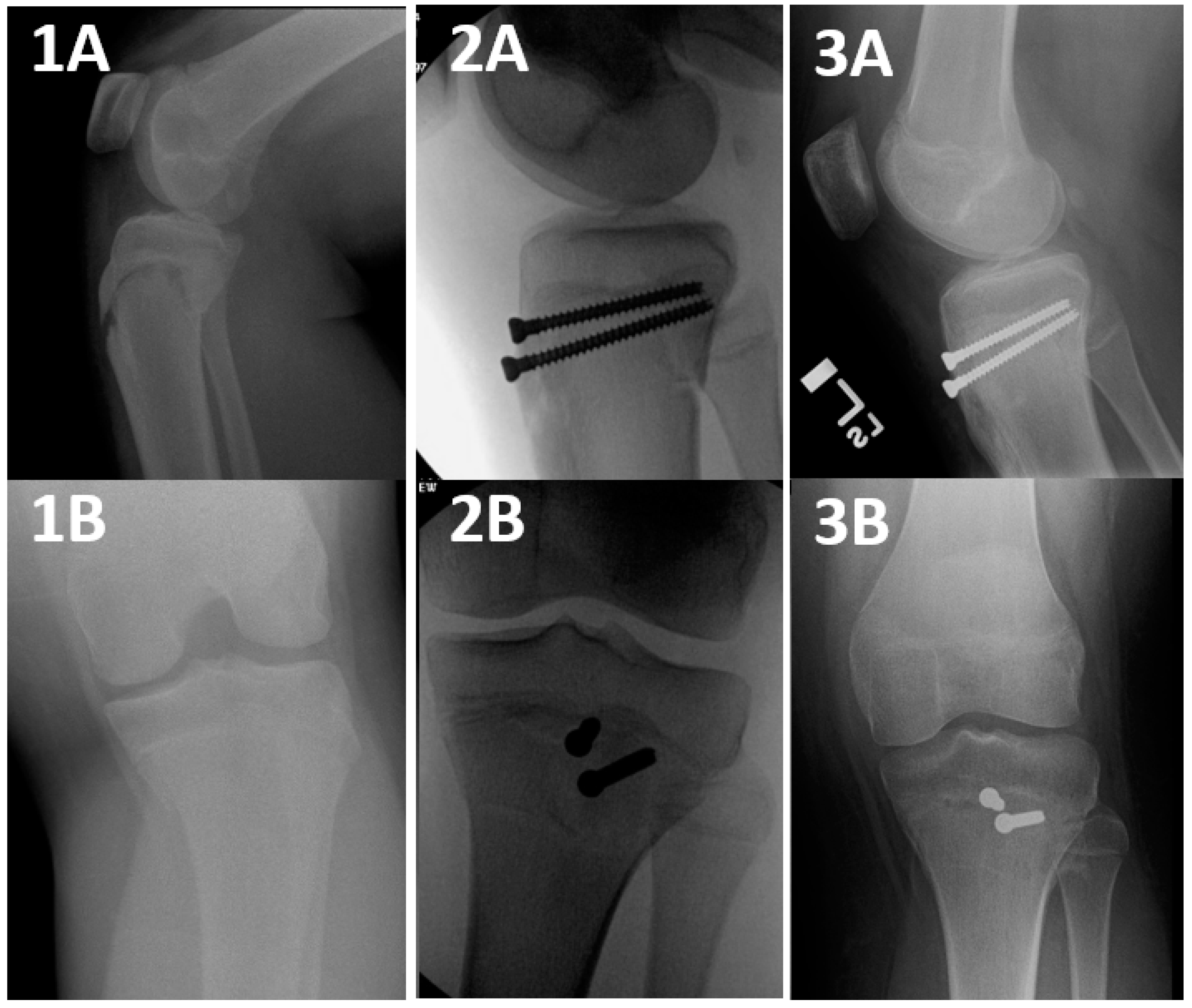
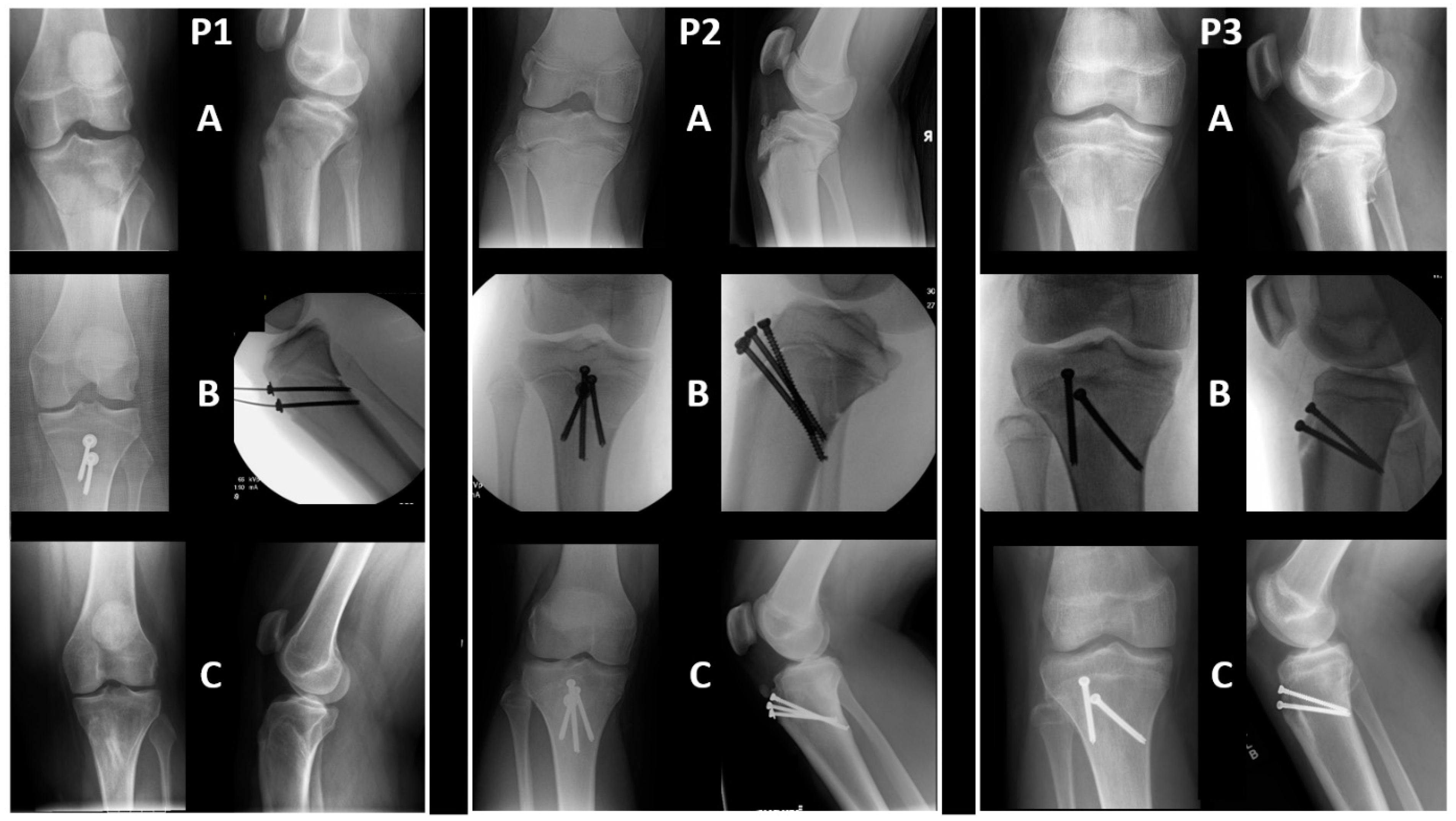
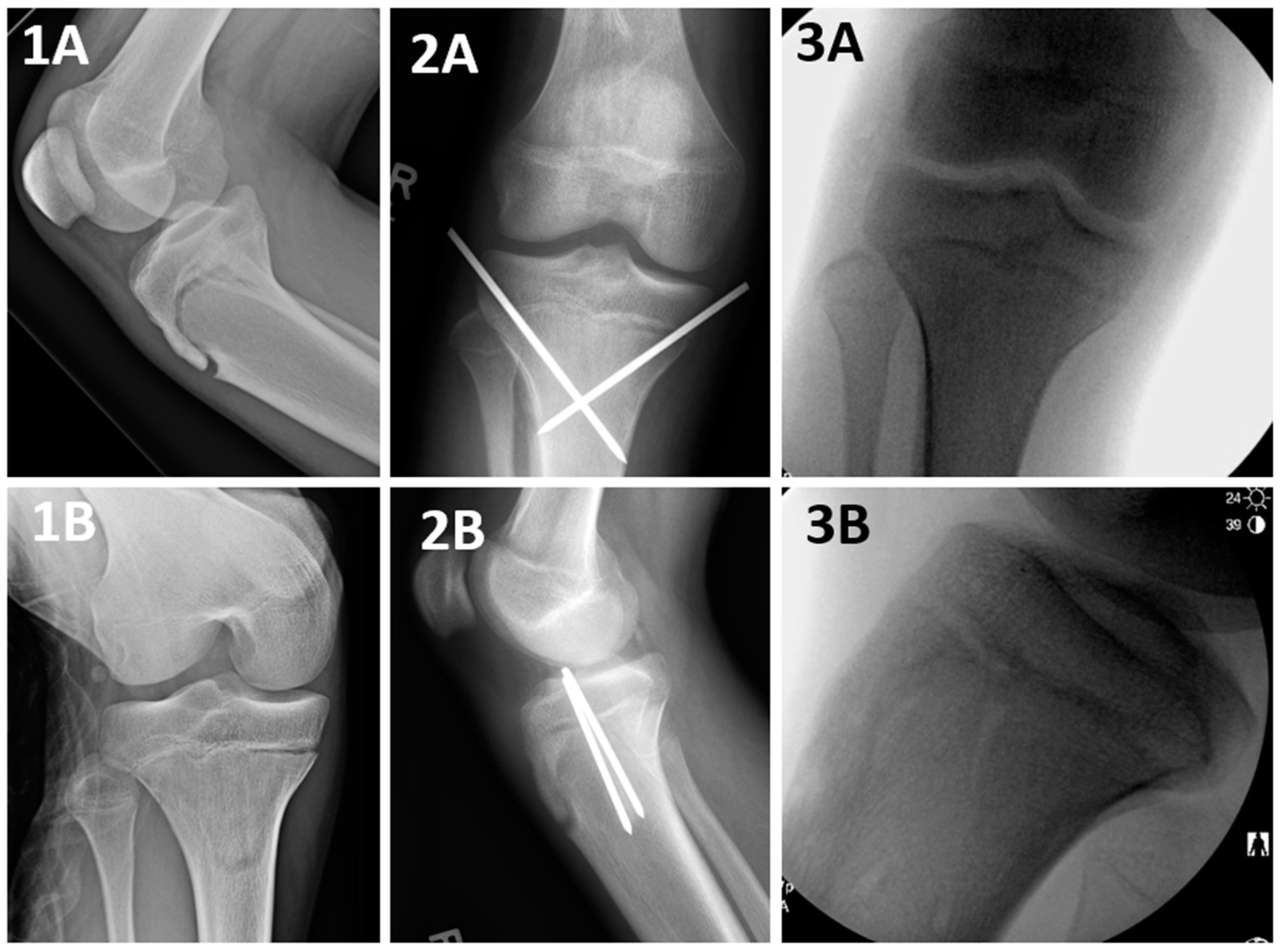
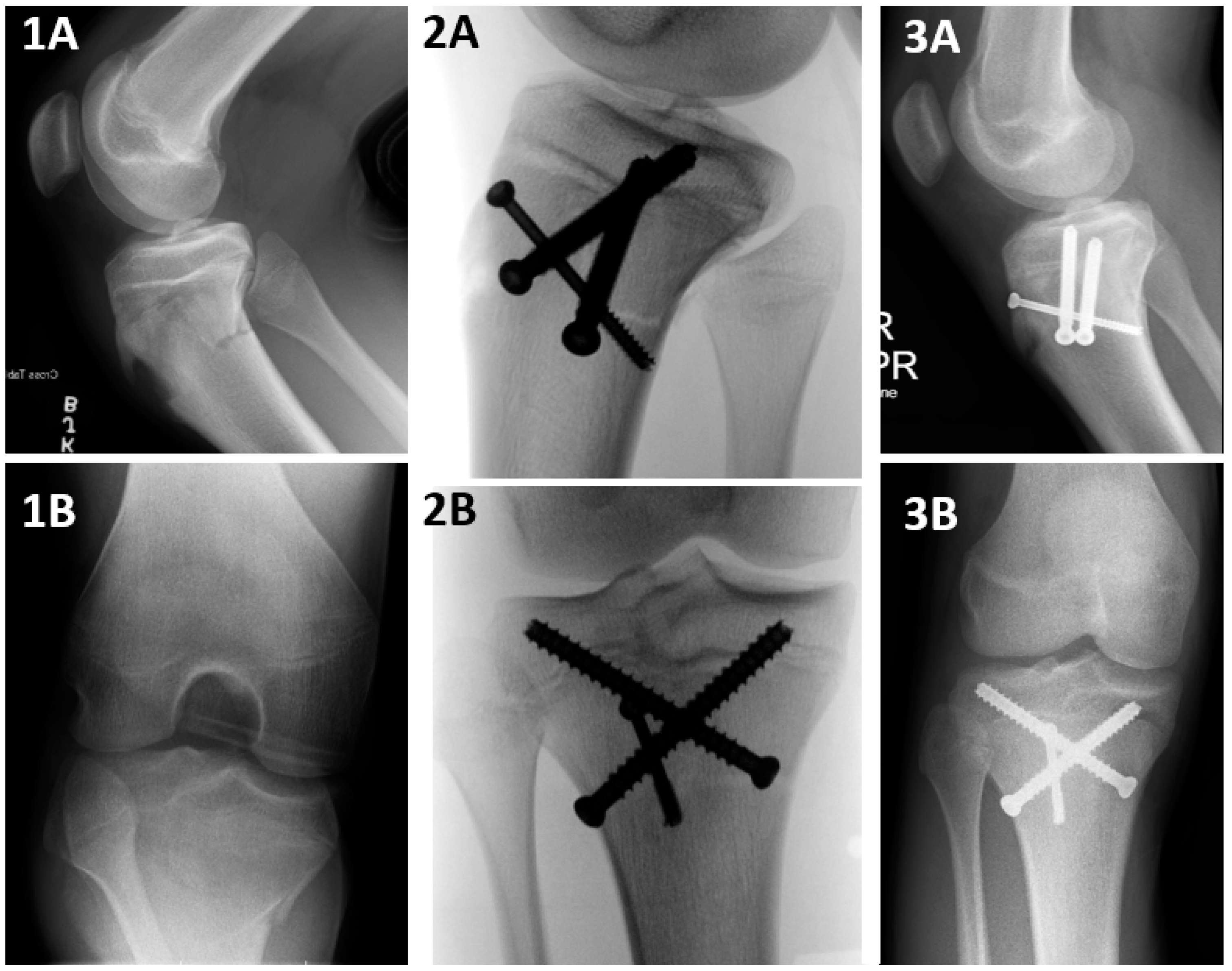
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McKoy, B.E.; Stanitski, C.L. Acute tibial tubercle avulsion fractures. Orthop. Clin. N. Am. 2003, 34, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.A.; Tross, R.B.; Murphy, M.J. Fractures of the tibial tuberosity in adolescents. J. Bone Joint Surg. Am. 1980, 62, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Pretell-Mazzini, J.; Kelly, D.M.; Sawyer, J.R.; Esteban, E.M.; Spence, D.D.; Warner, W.C., Jr.; Beaty, J.H. Outcomes and Complications of Tibial Tubercle Fractures in Pediatric Patients: A Systematic Review of the Literature. J. Pediatr. Orthop. 2016, 36, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Cole, W.W., 3rd; Brown, S.M.; Vopat, B.; Heard, W.M.R.; Mulcahey, M.K. Epidemiology, Diagnosis, and Management of Tibial Tubercle Avulsion Fractures in Adolescents. JBJS Rev. 2020, 8, e0186. [Google Scholar] [CrossRef] [PubMed]
- Watson-Jones, R. Fractures and Joint Injuries; Williams & Wilkins: Philadelphia, PA, USA, 1955. [Google Scholar]
- Ryu, R.K.; Debenham, J.O. An unusual avulsion fracture of the proximal tibial epiphysis. Case report and proposed addition to the Watson-Jones classification. Clin. Orthop. Relat. Res. 1985, 181–184. [Google Scholar]
- Brey, J.M.; Conoley, J.; Canale, S.T.; Beaty, J.H.; Warner, W.C., Jr.; Kelly, D.M.; Sawyer, J.R. Tibial tuberosity fractures in adolescents: Is a posterior metaphyseal fracture component a predictor of complications? J. Pediatr. Orthop. 2012, 32, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, I.; Sepúlveda, M.; Birrer, E.; Tuca, M.J. Fracture of the anterior tibial tuberosity in children. EFORT Open Rev. 2020, 5, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Bae, K.; Park, S.-S.; Kang, M.S. Ogden Type IV Tibial Tuberosity Fractures in Healthy Adolescents: Preoperative Magnetic Resonance Imaging and 2-Year Clinical Follow-up Study. Clin. Orthop. Surg. 2023, 15, 499. [Google Scholar] [CrossRef] [PubMed]
- Pace, J.L.; McCulloch, P.C.; Momoh, E.O.; Nasreddine, A.Y.; Kocher, M.S. Operatively treated type IV tibial tubercle apophyseal fractures. J. Pediatr. Orthop. 2013, 33, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Arkader, A.; Schur, M.; Refakis, C.; Capraro, A.; Woon, R.; Choi, P. Unicortical Fixation is Sufficient for Surgical Treatment of Tibial Tubercle Avulsion Fractures in Children. J. Pediatr. Orthop. 2019, 39, e18–e22. [Google Scholar] [CrossRef] [PubMed]
- Formiconi, F.; D’Amato, R.D.; Voto, A.; Panuccio, E.; Memeo, A. Outcomes of surgical treatment of the tibial tuberosity fractures in skeletally immature patients: An update. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Haber, D.B.; Tepolt, F.A.; McClincy, M.P.; Hussain, Z.B.; Kalish, L.A.; Kocher, M.S. Tibial tubercle fractures in children and adolescents: A large retrospective case series. J. Pediatr. Orthop. B. 2021, 30, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Rickert, K.D.; Hedequist, D.; Bomar, J.D. Screw Fixation of Pediatric Tibial Tubercle Fractures. JBJS Essent. Surg. Tech. 2021, 11, e19. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://int.aofoundation.org/trauma/-/media/project/aocd/aotrauma/documents/competency-based-education/handout_screws_english_high.pdf (accessed on 1 September 2024).
- Coders AAoP. American Academy of Professional Coders. 2023. Online Resource. Available online: https://www.aapc.com/codes/cpt-codes/27540 (accessed on 15 April 2024).
- Mun, F.; Suresh, S.J.; Marrache, M.; Suresh, K.V.; Ikwuezunma, I.; Lee, R.J. Minimizing the Risk of Vascular Injury: Anatomy of the Popliteal Artery in the Pediatric Knee. J. Pediatr. Orthop. 2022, 42, e847–e851. [Google Scholar] [CrossRef] [PubMed]


| Materials and Methods | Results | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Technique Group | Sex | Age | Side | Injury Setting/Mechanism | Follow-Up Duration | NWB (Weeks) | Immobilization Duration (Weeks) | Wound Complications | Change in Coronal Alignment (Degrees) | Change in Sagittal Alignment (Degrees) | |
| 1 | DCF | F | 13.98 | L | Running in soccer | 89 | 5 | 5 | None | −0.60 | 1.80 |
| 2 | DCF | F | 13.87 | R | fall | 24 | 3 | 3 | None | 2.60 | 0.90 |
| 3 | DCF | F | 13.84 | L | Jumping in gymnastics | 74 | 6 | 6 | None | −0.50 | 1.40 |
| 4 | DCF | M | 17.23 | L | Foot caught | 449 | 6 | 6 | None | −1.00 | 0.80 |
| 5 | DCF | M | 14.01 | L | Trampoline | 33 | 4 | 6 | None | 0.00 | 0.30 |
| 6 | DCF | M | 15.20 | L | Basketball, hit knee on a pole | 605 | 7 | 7 | None | 2.00 | 0.70 |
| 7 | DCF | M | 14.66 | L | Jumping in basketball | 140 | 5 | 5 | None | 0.50 | −0.80 |
| 8 | DCF | M | 15.51 | R | Football, while Running | 89 | 5 | 5 | None | 3.10 | 1.40 |
| 9 | DCF | M | 15.83 | L | Kicked in leg playing soccer | 209 | 4 | 4 | None | −2.10 | −3.00 |
| 10 | DCF | M | 12.44 | L | Ran and felt a “pop” | 60 | 4 | 4 | None | 0.80 | −5.10 |
| 11 | DCF | M | 15.59 | L | Jumping in basketball | 15 | 2 | no sufficient follow-up | None | 0.80 | −0.70 |
| 12 | DCF | M | 18.16 | L | Playing basketball | 36 | 5 | 5 | None | 1.00 | −1.70 |
| 13 | DCF | M | 14.37 | r | Jumping at basketball | 775 | 2 | 4 | Serous drainage 2 years after surgery | −3.00 | −3.10 |
| 14 | DCF | M | 13.72 | L | Running in soccer | 179 | 0 | 3 | None | −3.40 | −4.30 |
| 15 | DCF | M | 15.22 | R | Felt a “pop” while running | 583 | 6 | 4 | None | 0.50 | 1.50 |
| 16 | DCF | M | 15.23 | L | Running in basketball | 78 | 4 | 4 | None | −0.10 | 0.20 |
| 17 | DCF | M | 15.66 | R | Jumping in basketball | 155 | 0 | 4 | None | −1.60 | −0.50 |
| 18 | DCF | M | 14.04 | L | Playing bsketball | 289 | 5 | 5 | None | 1.20 | 3.20 |
| 19 | DCF | M | 14.68 | L | Abrupt stop while running | 31 | 6 | 4 | None | 4.10 | −2.20 |
| 20 | DCF | M | 16.24 | L | Jumping in basketball | 391 | 7 | 7 | None | 1.50 | −1.50 |
| 21 | DCF | M | 12.97 | L | Running in dodgeball, head a “pop” | 836 | 4 | 3 | None | 3.00 | −9.30 |
| 22 | PST | M | 14.12 | R | Jumping at basketball | 157 | 4 | 4 | None | −4.30 | −3.30 |
| 23 | PST | M | 14.64 | L | Jumping rope | 194 | 4 | 4 | None | 1.60 | 0.10 |
| 24 | PST | M | 13.91 | L | Trampoline park | 240 | 4 | 4 | None | 1.50 | −10.40 |
| 25 | PST | M | 12.72 | Bil | Slipped on water playing basketball | 366 | 6 | 6 | wound dehiscence | 1.60 | −2.40 |
| 26 | PST | M | 15.68 | L | Jumping hurdles | 117 | 6 | 6 | None | 1.70 | 3.10 |
| 27 | PST | M | 12.87 | R | Trampoline | 41 | 7 | 3 | None | −1.00 | unmeasurable |
| 28 | PST | M | 15.59 | L | 72 | 7 | 7 | None | −0.10 | 1.10 | |
| 29 | PST | M | 14.76 | R | Running/“roughhousing” | 468 | 2 | 8 | None | 2.70 | 1.40 |
| 30 | Crossed | M | 15.50 | R | Jumping in basketball | 97 | 4 | 4 | None | 2.60 | 2.80 |
| 31 | Crossed lateral and medial | M | 14.09 | L | Soccer | 98 | 2 | 7 | None | 1.70 | −4.10 |
| 32 | Crossed lateral and medial | M | 16.35 | R | Jumping on trampoline | 141 | 4 | 4 | None | −1.30 | 8.60 |
| 33 | Crossed lateral and medial | M | 15.85 | R | Stepped wrong on ladder, fell, and hit his knee | 26 | 6 | 3.5 | None | 2.60 | 3.10 |
| 34 | Crossed lateral and medial | M | 15.50 | R | Jumping in basketball | 103 | 4 | 2 | None | 0.10 | 2.20 |
| 35 | Multiple | M | 15.30 | R | Jumping over fence | 366 | 0 | 6 | None | −1.50 | 0.20 |
| 36 | Multiple | M | 15.84 | R | Jumping in basketball | 358 | 6 | 6 | None | −1.60 | 1.00 |
| 37 | Multiple | M | 13.79 | L | Fell while running in baseball | 343 | 4 | 4 | None | −0.20 | −2.60 |
| Variable | DCF (n = 21, 56.75%) | PST (n = 8, 21.62%) | Crossed/Other (n = 8, 21.62%) | Total (n = 37, 100%) | p Value |
|---|---|---|---|---|---|
| Materials and Methods | |||||
| Sex (Male) | 18 (85.7%) | 8 (100%) | 8 (100%) | 34 (91.9%) | 0.395 |
| Age (Years) | 14.88 ± 1.35 | 14.28 ± 1.11 | 15.28 ± 0.88 | 14.83 ± 1.23 | 0.263 |
| Side (Left) | 16 (76.2%) | 5 (62.5%) | 2 (25%) | 23 (62.2%) | 0.059 |
| Ethnicity | 0.644 | ||||
| Black | 9 (42.9%) | 4 (50%) | 5 (62.5%) | 18 (48.6%) | |
| White | 9 (42.9%) | 2 (25%) | 3 (37.5%) | 14 (37.8%) | |
| Hispanic/Asian/other | 3 (14.3%) | 2 (25%) | 0 (0%) | 5 (13.5%) | |
| Weight (kg) | 78.73 ± 20.35 | 75.42 ± 17.63 | 74.43 ± 19.42 | 77.09 ± 19.17 | 0.888 |
| Weight percentile | 84.34 ± 19.96 | 95.76 ± 4.79 | 76.26 ± 24.9 | 84.77 ± 19.91 | 0.14 |
| Time from presentation to surgery | 1.57 ± 2.29 | 2.75 ± 3.41 | 1.13 ± 0.354 | 1.73 ± 2.29 | 0.679 |
| Number of patients who underwent additional imaging studies | 0.004 | ||||
| CT | 1 (4.8%) | 3 (37.5%) | 4 (50%) | 8 (21.6%) | |
| MRI | 0 (0%) | 1 (12.5%) | 0 (0%) | 1 (2.7%) | |
| Duration of surgery (minutes) | 80.05 ± 26.13 | 68.88 ± 28.59 | 57.25 ± 11.89 | 72.5 ± 25.59 | 0.102 |
| Closed reduction (vs. open reduction) | 10 (47.6%) | 4 (50%) | 6 (75%) | 20 (54.1%) | 0.45 |
| Number of screws per surgery * | 0.014 | ||||
| 1 | 2 (9.5%) | 1 (12.5%) | 0 (0%) | 3 (8.1%) | |
| 2 | 14 (66.7%) | 5 (62.5%) | 1 (12.5%) | 20 (54.1%) | |
| 3 | 5 (23.8%) | 2 (25%) | 3 (37.5%) | 10 (27%) | |
| 4 | 0 (0%) | 0 (0%) | 1 (12.5%) | 1 (2.7%) | |
| K wires | 0 (0%) | 0 (0%) | 3 (37.5%) | 3 (8.1%) | |
| Screw size | 0.006 | ||||
| 4.0 | 3 (14.3%) | 0 (0%) | 0 (0%) | ||
| 4.5 | 15 (71.4%) | 5 (62.5%) | 1 (12.5%) | ||
| 6.5 | 2 (9.5%) | 2 (25%) | 2 (25%) | ||
| Mixed | 1 (4.8%) | 1 (12.5%) | 2 (25%) | ||
| K wires | 0 (0%) | 0 (0%) | 3 (37.5%) | ||
| Washer (yes) | 12 (57.1%) | 4 (50%) | 1 (12.5%) | 17 (45.9%) | 0.115 |
| Biocortical purchase | 13 (61.9%) * | 8 (100%) | 8 (100%) | 29 (78.4%) | 0.021 |
| Fasciotomy | 0.814 | ||||
| Surgical | 2 (9.5%) | 2 (25%) | 0 (0%) | 4 (10.8%) | |
| Traumatic (documented) | 5 (23.8%) | 1 (12.5%) | 1 (12.5%) | 7 (18.9%) | |
| Both | 1 (4.8%) | 0 (0%) | 0 (0%) | 1 (2.7%) | |
| Follow-up duration (weeks) | 35.17 ± 36.79 | 30.03 ± 20.84 | 28 ± 19.58 | 32.51 ± 30.34 | 0.883 |
| Duration of complete immobilization at full extension (weeks) | 4.7 ± 1.22 | 5.25 ± 1.75 | 4.56 ± 1.63 | 4.79 ± 1.42 | 0.707 |
| Duration of non-weight-bearing restriction (weeks) | 4.29 ± 1.98 | 5 ± 1.77 | 3.75 ± 1.98 | 4.32 ± 1.93 | 0.435 |
| Referral to physical therapy | 21 (100%) | 8 (100%) | 7 (87.5%) | 36 (97.3%) | 0.432 |
| Results | |||||
| Documented pain after 3 months | 0.517 | ||||
| Yes | 4 (19%) | 2 (25%) | 0 (0%) | 6 (16.2%) | |
| No | 13 (61.9%) | 6 (75%) | 7 (87.5%) | 26 (70.3%) | |
| Lacking sufficient follow-up | 4 (19%) | 0 (0%) | 1 (12.5%) | 5 (13.5%) | |
| Wound complications | 0 (0%) | 1 (4.8%) | 1 (12.5%) | 2 (5.4%) | 0.685 |
| Full range of motion on last follow-up | 0.761 | ||||
| Yes | 15 (71.4%) | 7 (87.5%) | 6 (75%) | 28 (75.7%) | |
| No | 3 (14.3%) | 0 (0%) | 0 (0%) | 3 (8.1%) | |
| Lacking sufficient follow-up | 3 (14.3%) | 1 (12.5) | 2 (25%) | 6 (16.2%) | |
| Variable | DCF (n = 21, 56.75%) | PST (n = 8, 21.62%) | Crossed/Other (n = 8, 21.62%) | Total (n = 37, 100%) | p Value |
|---|---|---|---|---|---|
| Coronal alignment (degrees) | |||||
| Immediate postoperative | 88.2 ± 1.86 | 86.96 ± 2.08 | 86.47 ± 1.41 | 87.56 ± 1.93 | |
| Last documented (fused fracture) | 87.78 ± 1.57 | 86.5 ± 1.48 | 86.17 ± 2.6 | 87.16 ± 1.91 | |
| Difference | 0.41 ± 1.97 | 0.46 ± 2.24 | 0.3 ± 1.78 | 0.4 ± 1.94 | 0.872 |
| Sagittal alignment (degrees) | |||||
| Immediate postoperative | 9.7 ± 4.95 | 9.91 ± 7.84 | 8.85 ± 4.68 | 9.55 ± 4.94 | |
| Last documented (fused fracture) | 8.75 ± 3.58 | 8.11 ± 5.01 | 10.25 ± 4.18 | 8.93 ± 3.99 | |
| Difference | 0.95 ± 2.86 | 1.48 ± 4.52 | −1.4 ± 3.87 | 0.53 ± 3.51 | 0.296 |
| Refs. | mWJ4 Cases (n) | Relevant Findings and Conclusions |
|---|---|---|
| Pace et al. [9] | 24 | The authors’ perception was that longer bi-cortical screws were necessary to stabilize the posterior fracture fragment. Accordingly, they stated that a screw purchase in this fragment should be achieved whenever possible. In their series, 4 patients required a supplemental plate fixation. |
| Haber et al. [12] | 26 | In all, 79% of the mWJ4/5 fractures were treated operatively. The authors did not separate types 4 and 5 in their analysis. Although they did not elaborate on the technique in the text, the image provided by the authors presented a PST as their surgical method. |
| Arkader et al. [10] | 13 | A total of 12 cases were operated with uni-cortical fixation, while only 1 case was treated with a mixed uni- and bi-cortical fixation. The authors concluded that a uni-cortical fixation might be suitable in mWJ4 fractures. |
| Park et al. [14] | 10 | All fractures were fixated by a PST construct utilizing 2 (in a few cases) or 3 (in most cases) screws, most commonly 6.5 mm cancellous. The entry points were medial and lateral to the tibial tuberosity without violating the tibial apophysis. |
| Formicini et al. [11] | 5 | The authors used 4.5 mm cannulated screws and pointed out that while mWJ 1–3 could be treated with uni-cortical screws, mWJ4 fractures required greater stability, especially for the posterior component. For this reason, they used bi-cortical screws that engaged this component to form a construct regarded by them to be more effective. |
| Rodriguez et al. [7] | review | The authors presented a review of tibial tuberosity fractures. In their review, they did not discuss the specifications of the screw trajectory but did provide an image that represented their concept of a proper screw position for fixating mWJ4 fractures. In that image, the posterior component was captured with a PST, with two fully threaded screws that were inserted through the tibial tuberosity midline. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Segal, D.; Dillenkofer, M.; Wall, E.J.; Tamai, J. Type 4 Tibial Tuberosity Avulsion Fractures: Surgical Treatment Early Outcomes and a Presentation of the Distal Cortical Fixation. J. Clin. Med. 2024, 13, 5695. https://doi.org/10.3390/jcm13195695
Segal D, Dillenkofer M, Wall EJ, Tamai J. Type 4 Tibial Tuberosity Avulsion Fractures: Surgical Treatment Early Outcomes and a Presentation of the Distal Cortical Fixation. Journal of Clinical Medicine. 2024; 13(19):5695. https://doi.org/10.3390/jcm13195695
Chicago/Turabian StyleSegal, David, Michael Dillenkofer, Eric J. Wall, and Junichi Tamai. 2024. "Type 4 Tibial Tuberosity Avulsion Fractures: Surgical Treatment Early Outcomes and a Presentation of the Distal Cortical Fixation" Journal of Clinical Medicine 13, no. 19: 5695. https://doi.org/10.3390/jcm13195695
APA StyleSegal, D., Dillenkofer, M., Wall, E. J., & Tamai, J. (2024). Type 4 Tibial Tuberosity Avulsion Fractures: Surgical Treatment Early Outcomes and a Presentation of the Distal Cortical Fixation. Journal of Clinical Medicine, 13(19), 5695. https://doi.org/10.3390/jcm13195695






