Human-in-the-Loop—A Deep Learning Strategy in Combination with a Patient-Specific Gaussian Mixture Model Leads to the Fast Characterization of Volumetric Ground-Glass Opacity and Consolidation in the Computed Tomography Scans of COVID-19 Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Datasets
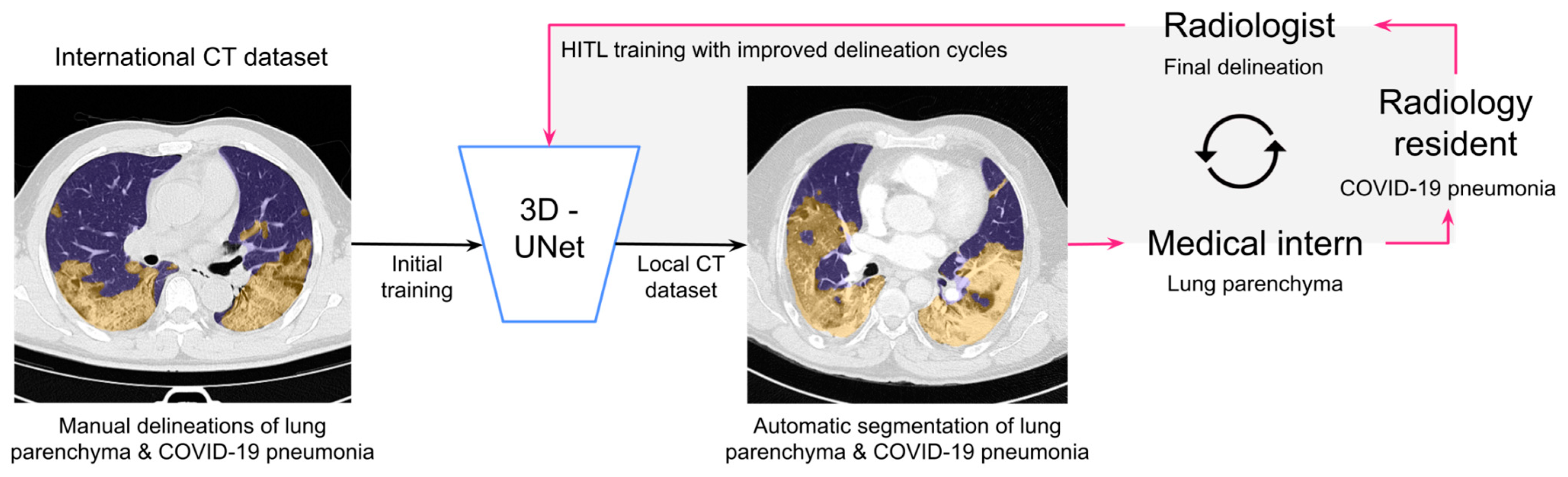
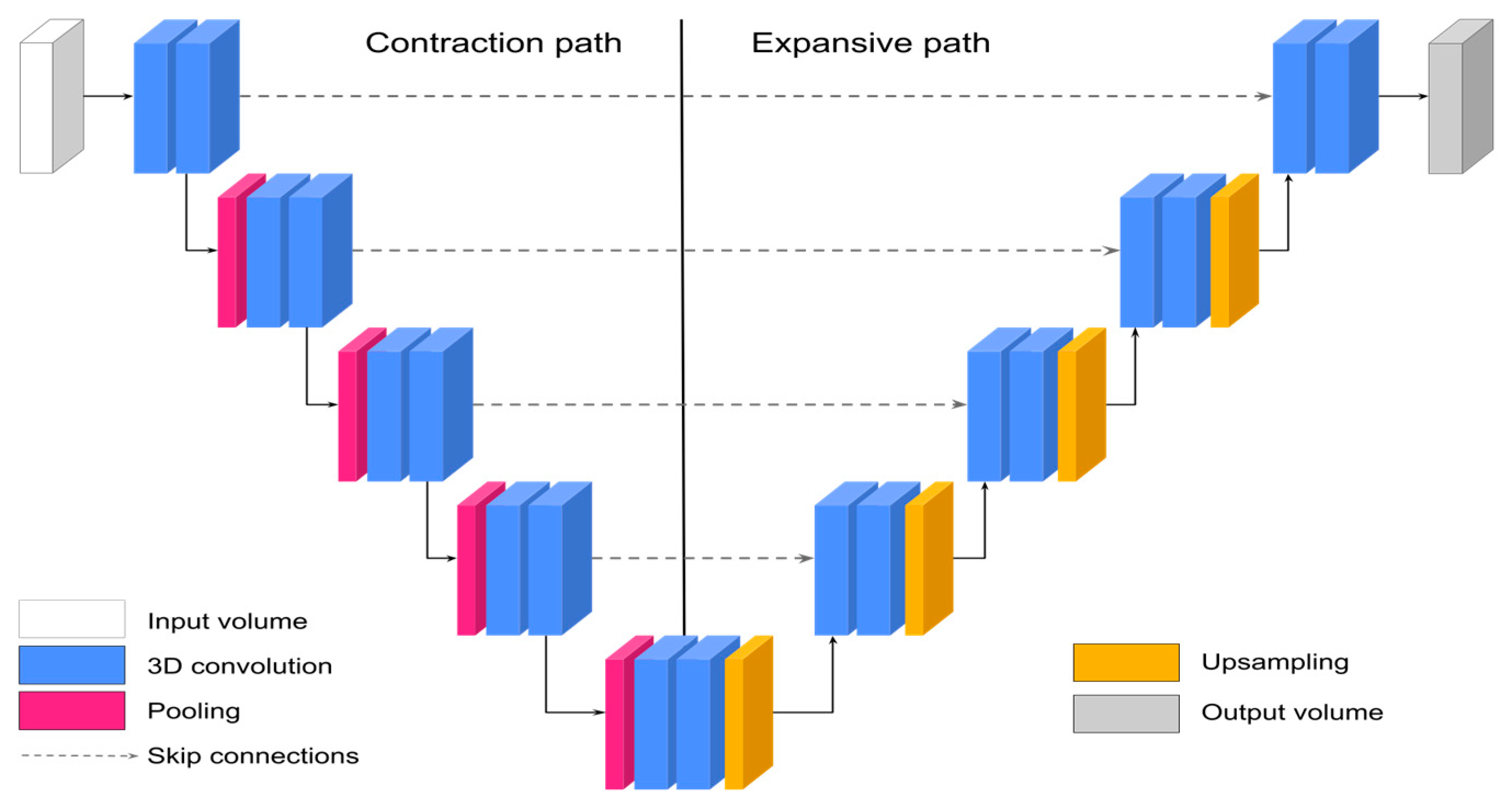
2.2. Segmentation of Normal Lung Parenchyma and COVID-19 Pneumonia with 3D-UNet
2.3. Human-in-the-Loop (HITL) Strategy for the Fast Optimization and Characterization of Normal Lung Parenchyma and COVID-19 Pneumonia
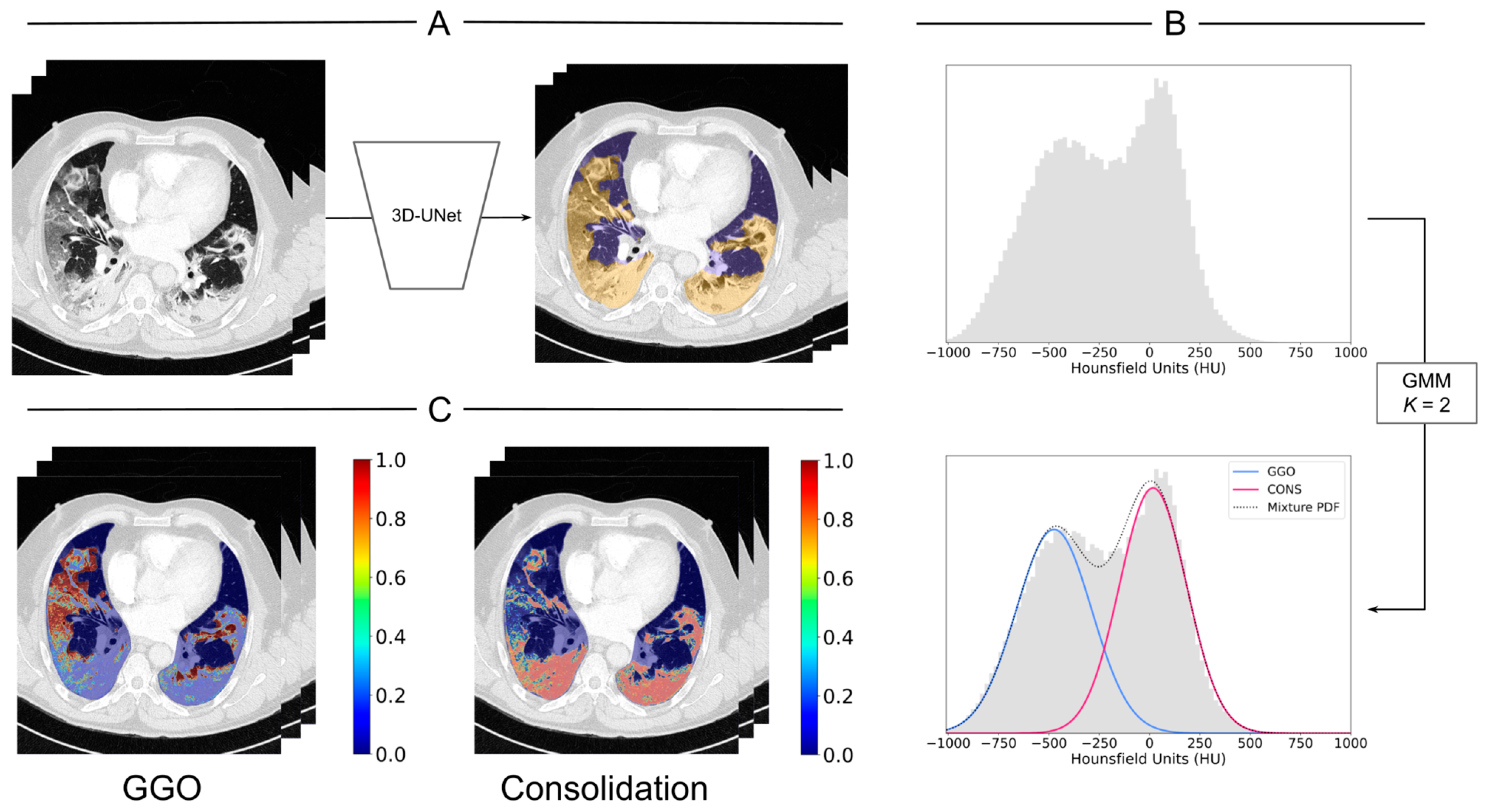
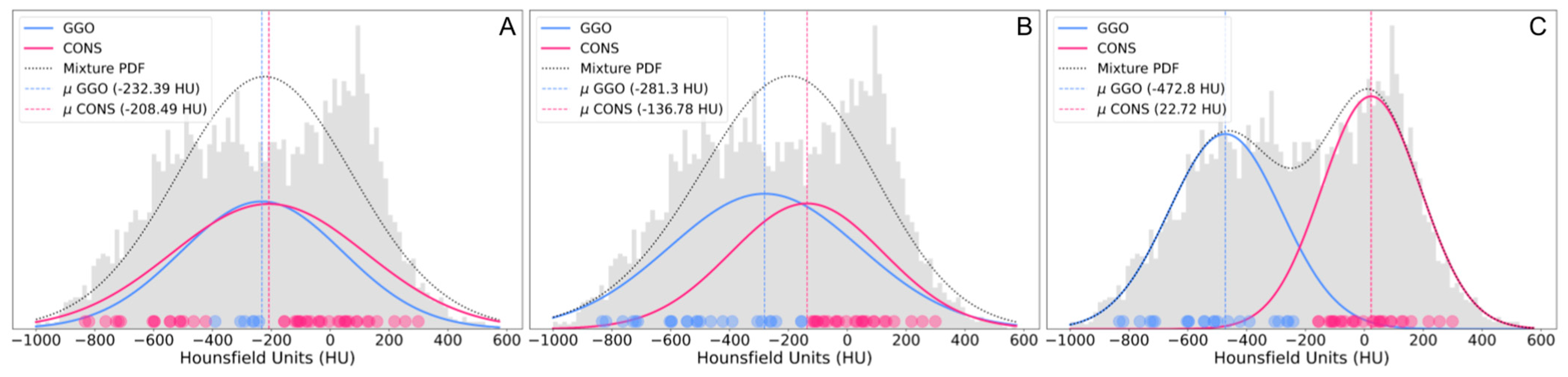
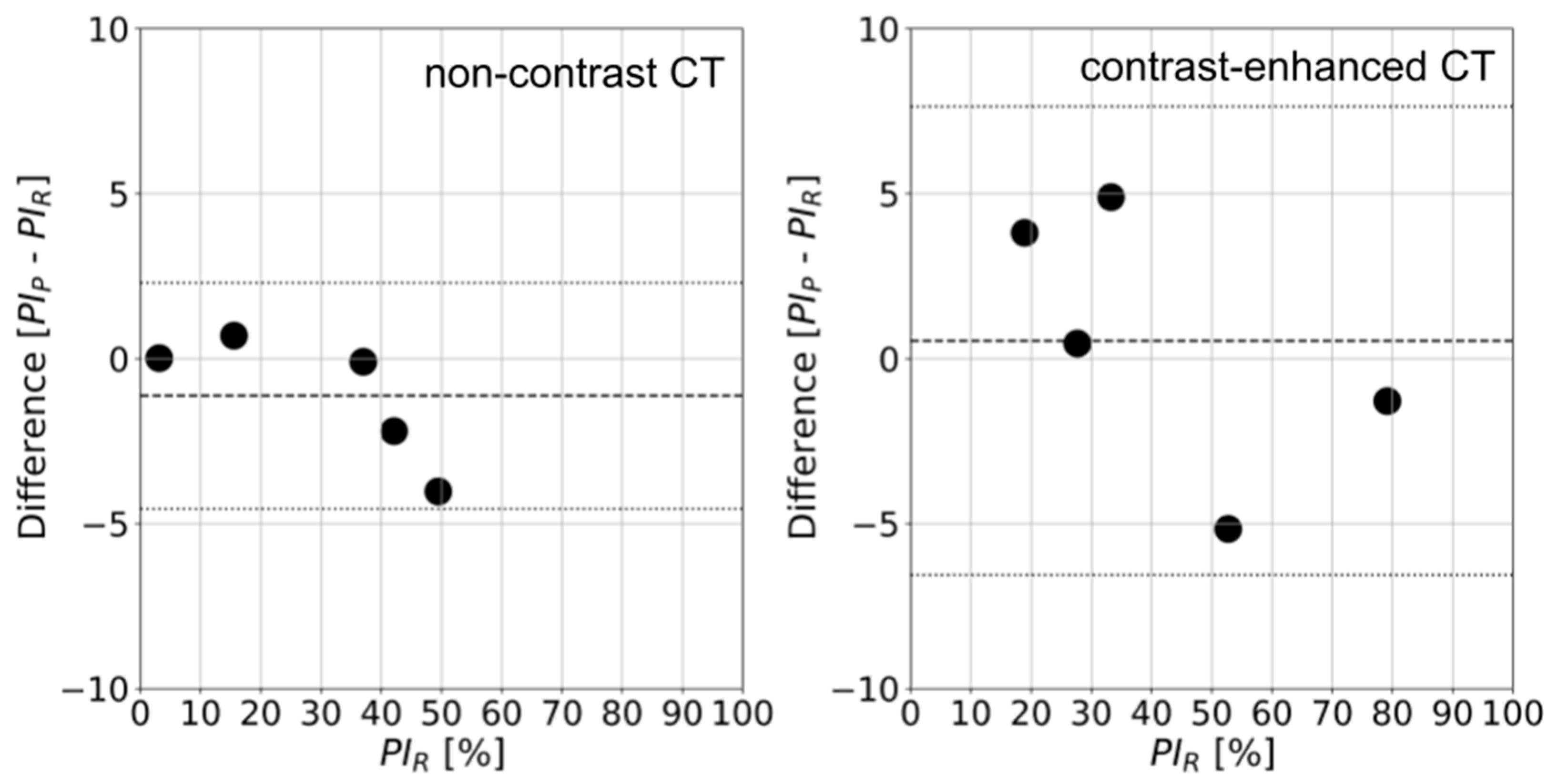
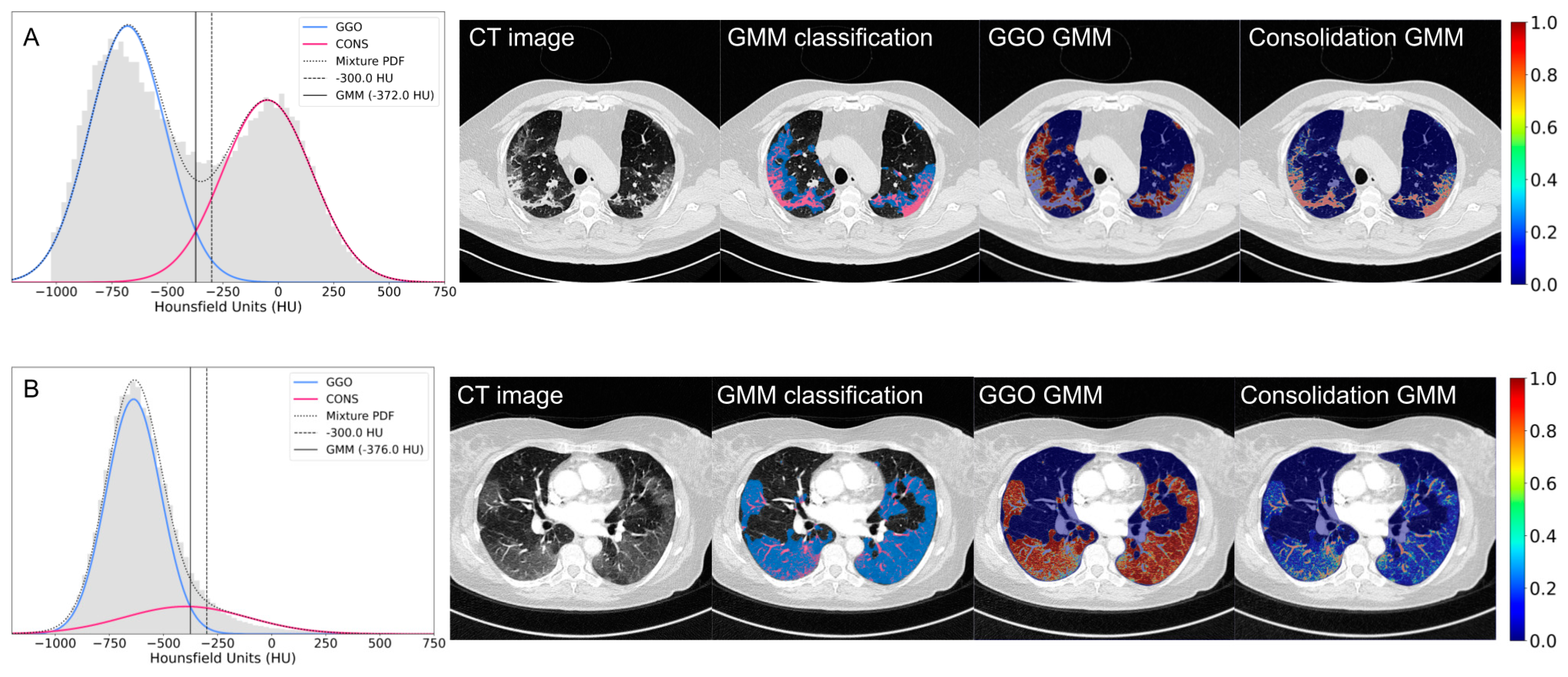
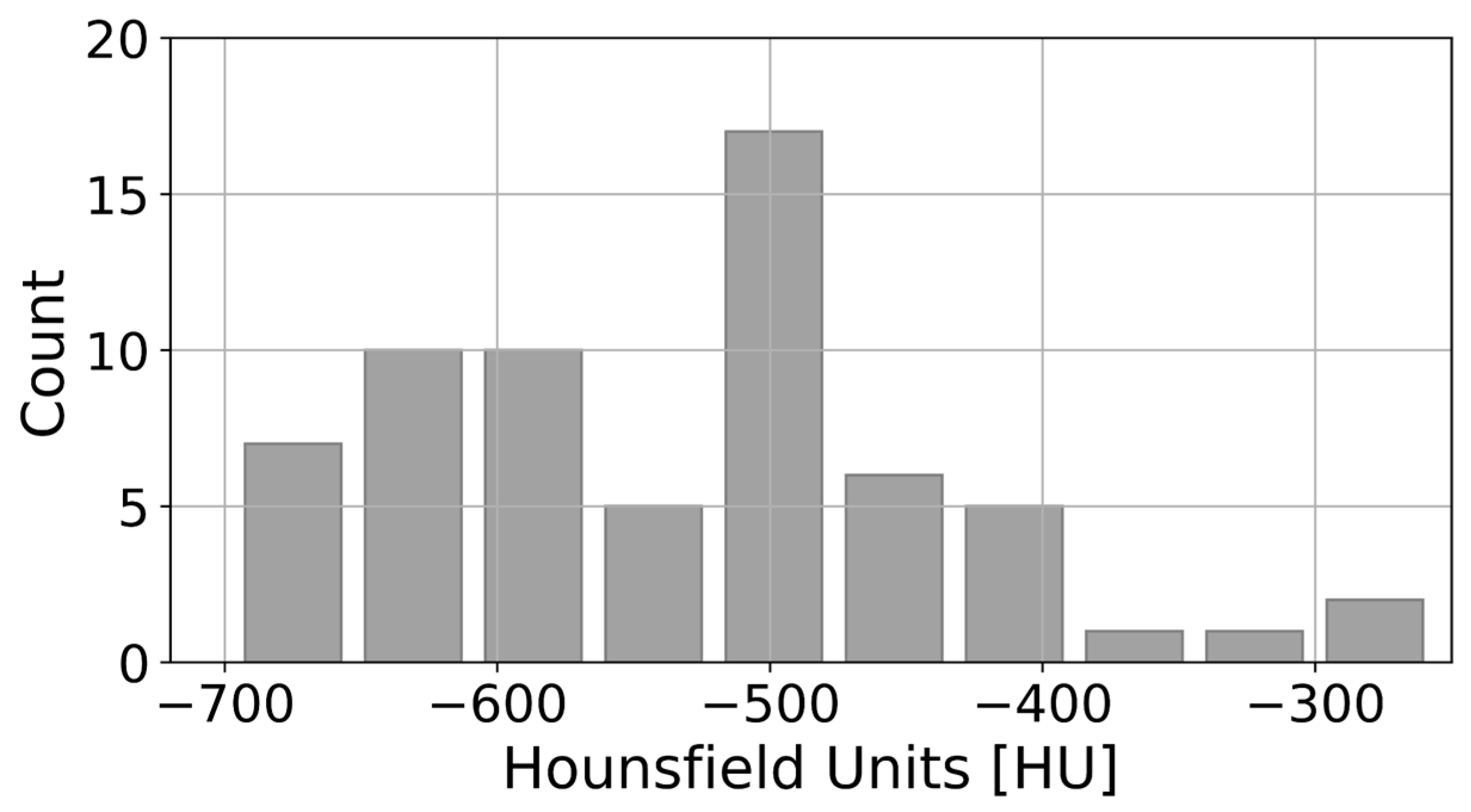
2.4. Gaussian Mixture Model (GMM) to Characterize Ground-Glass Opacity (GGO) and Consolidation
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yang, W.; Sirajuddin, A.; Zhang, X.; Liu, G.; Teng, Z.; Zhao, S.; Lu, M. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur. Radiol. 2020, 30, 4874–4882. [Google Scholar] [CrossRef]
- Cozzi, D.; Cavigli, E.; Moroni, C.; Smorchkova, O.; Zantonelli, G.; Pradella, S.; Miele, V. Ground-glass opacity (GGO): A review of the differential diagnosis in the era of COVID-19. Jpn. J. Radiol. 2021, 39, 721–732. [Google Scholar] [CrossRef]
- Mehrabi, S.; Fontana, S.; Mambrin, F.; Nguyen, H.Q.; Righi, E.; Tacconelli, E.; Mansueto, G. Pitfalls of computed tomography in the coronavirus 2019 (COVID-19) era: A new perspective on ground-glass opacities. Cureus 2020, 12, e8151. [Google Scholar] [CrossRef]
- Wang, Y.; Dong, C.; Hu, Y.; Li, C.; Ren, Q.; Zhang, X.; Shi, H.; Zhou, M. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: A longitudinal study. Radiology 2020, 296, E55–E64. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.; Wang, Y.; Zhou, S.; Zhang, N.; Xia, L. A comparative study of chest computed tomography features in young and older adults with coronavirus disease (COVID-19). J. Thorac. Imaging 2020, 35, W97. [Google Scholar] [CrossRef] [PubMed]
- Hansell, D.; Bankier, A.; MacMahon, H.; McLoud, T.; Muller, N.; Remy, J. Fleischner society: Glossary of terms for thoracic imaging. Radiology 2008, 246, 697–722. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Shang, K.; Bian, W.; He, L.; Fan, Y.; Ren, T.; Zhang, J. Prediction of disease progression in patients with COVID-19 by artificial intelligence assisted lesion quantification. Sci. Rep. 2020, 10, 22083. [Google Scholar] [CrossRef]
- Müller, N.L.; Staples, C.; Miller, R.; Vedal, S.; Thurlbeck, W.; Nostrow, D. Disease activity in idiopathic pulmonary fibrosis: CT and pathologic correlation. Radiology 1987, 165, 731–734. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, J.M.; Poon, L.L.; Lee, K.C.; Ng, W.F.; Lai, S.T.; Leung, C.Y.; Chu, C.M.; Hui, P.K.; Mak, K.L.; Lim, W.; et al. Lung pathology of fatal severe acute respiratory syndrome. Lancet 2003, 361, 1773–1778. [Google Scholar] [CrossRef]
- Jin, Y.-H.; Cai, L.; Cheng, Z.-S.; Cheng, H.; Deng, T.; Fan, Y.-P.; Fang, C.; Huang, D.; Huang, L.-Q.; Huang, Q.; et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil. Med. Res. 2020, 7, 4. [Google Scholar] [CrossRef]
- Sapienza, L.; Nasra, K.; Calsavara, V.; Little, T.; Narayana, V.; Abu-Isa, E. Risk of in-hospital death associated with COVID-19 lung consolidations on chest computed tomography–a novel translational approach using a radiation oncology contour software. Eur. J. Radiol. Open 2021, 8, 100322. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Wang, Y.; Huang, S.; Liu, S.; Zhou, Z.; Zhang, S.; Zhao, Z.; Yu, Y.; Yang, Y.; Ju, S. Multicenter cohort study demonstrates more consolidation in upper lungs on initial CT increases the risk of adverse clinical outcome in COVID-19 patients. Theranostics 2020, 10, 5641–5648. [Google Scholar] [CrossRef] [PubMed]
- Fan, D.-P.; Zhou, T.; Ji, G.-P.; Zhou, Y.; Chen, G.; Fu, H.; Shen, J.; Shao, L. Inf-Net: Automatic COVID-19 Lung Infection Segmentation from CT Images. IEEE Trans. Med. Imaging 2020, 39, 2626–2637. [Google Scholar] [CrossRef]
- Enshaei, N.; Oikonomou, A.; Rafiee, M.J.; Afshar, P.; Heidarian, S.; Mohammadi, A.; Plataniotis, K.N.; Naderkhani, F. COVID-rate: An automated framework for segmentation of COVID-19 lesions from chest CT images. Sci. Rep. 2022, 12, 3212. [Google Scholar] [CrossRef]
- Müller, D.; Soto-Rey, I.; Kramer, F. Robust chest CT image segmentation of COVID-19 lung infection based on limited data. Inform. Med. Unlocked 2021, 25, 100681. [Google Scholar] [CrossRef] [PubMed]
- Oulefki, A.; Agaian, S.; Trongtirakul, T.; Laouar, A. Automatic COVID-19 lung infected region segmentation and measurement using CT-scans images. Pattern Recognit. 2021, 114, 107747. [Google Scholar] [CrossRef]
- Bougourzi, F.; Distante, C.; Dornaika, F.; Taleb-Ahmed, A. PDAtt-Unet: Pyramid Dual-Decoder Attention Unet for COVID-19 infection segmentation from CT-scans. Med. Image Anal. 2023, 86, 102797. [Google Scholar] [CrossRef]
- Mosqueira-Rey, E.; Hernández-Pereira, E.; Alonso-Ríos, D.; Bobes-Bascarán, J.; Fernández-Leal, Á. Human-in-the-loop machine learning: A state of the art. Artif. Intell. Rev. 2023, 56, 3005–3054. [Google Scholar] [CrossRef]
- Budd, S.; Robinson, E.C.; Kainz, B. A survey on active learning and human-in-the-loop deep learning for medical image analysis. Med. Image Anal. 2021, 71, 102062. [Google Scholar] [CrossRef]
- Qu, C.; Zhang, T.; Qiao, H.; Tang, Y.; Yuille, A.L.; Zhou, Z. Abdomenatlas-8k: Annotating 8,000 CT volumes for multi-organ segmentation in three weeks. Adv. Neural Inf. Process. Syst. 2024, 36. [Google Scholar] [CrossRef]
- Rajamani, K.; Siebert, H.; Heinrich, M. Dynamic deformable attention network (DDANet) for COVID-19 lesions semantic segmentation. J. Biomed. Inform. 2021, 119, 103816. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Zhu, Y.; Qin, X.; Xin, Y.; Yang, D.; Xu, T. A multi-class COVID-19 segmentation network with pyramid attention and edge loss in CT images. IET Image Process 2021, 15, 2604–2613. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.T.; Zhang, J.S.; Zhang, H.H.; Nan, Y.D.; Zhao, Y.; Fu, E.Q.; Xie, Y.H.; Liu, W.; Li, W.P.; Zhang, H.J.; et al. Automated detection and quantification of COVID-19 pneumonia: CT imaging analysis by a deep learning-based software. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 2525–2532. [Google Scholar] [CrossRef] [PubMed]
- Grassi, R.; Cappabianca, S.; Urraro, F.; Granata, V.; Giacobbe, G.; Magliocchetti, S.; Cozzi, D.; Fusco, R.; Galdiero, R.; Picone, C.; et al. Evolution of CT findings and lung residue in patients with COVID-19 pneumonia: Quantitative analysis of the disease with a computer automatic tool. J. Pers. Med. 2021, 11, 641. [Google Scholar] [CrossRef]
- Lu, W.; Wei, J.; Xu, T.; Ding, M.; Li, X.; He, M.; Chen, K.; Yang, X.; She, H.; Huang, B. Quantitative CT for detecting COVID-19 pneumonia in suspected cases. BMC Infect Dis. 2021, 21, 836. [Google Scholar] [CrossRef]
- Grassi, R.; Belfiore, M.P.; Montanelli, A.; Patelli, G.; Urraro, F.; Giacobbe, G.; Fusco, R.; Granata, V.; Petrillo, A.; Sacco, P.; et al. COVID-19 pneumonia: Computer-aided quantification of healthy lung parenchyma, emphysema, ground glass and consolidation on chest computed tomography (CT). Radiol. Med. 2021, 126, 553–560. [Google Scholar] [CrossRef]
- Shan, F.; Gao, Y.; Wang, J.; Shi, W.; Shi, N.; Han, M.; Xue, Z.; Shen, D.; Shi, Y. Abnormal lung quantification in chest CT images of COVID-19 patients with deep learning and its application to severity prediction. Med. Phys. 2021, 48, 1633–1645. [Google Scholar] [CrossRef]
- Biebau, C.; Dubbeldam, A.; Cockmartin, L.; Coudyzer, W.; Coolen, J.; Verschakelen, J.; De Wever, W. Comparing Visual Scoring of Lung Injury with a Quantifying AI-Based Scoring in Patients with COVID-19. J. Belg. Soc. Radiol. 2021, 105, 16. [Google Scholar] [CrossRef]
- Fang, X.; Kruger, U.; Homayounieh, F.; Chao, H.; Zhang, J.; Digumarthy, S.R.; Arru, C.D.; Kalra, M.K.; Yan, P. Association of AI quantified COVID-19 chest CT and patient outcome. Int. J. Comput. Assist. Radiol. Surg. 2021, 16, 435–445. [Google Scholar] [CrossRef]
- Mader, C.; Bernatz, S.; Michalik, S.; Koch, V.; Martin, S.S.; Mahmoudi, S.; Basten, L.; Grünewald, L.D.; Bucher, A.; Albrecht, M.H.; et al. Quantification of COVID-19 opacities on chest CT—Evaluation of a fully automatic AI-approach to non invasively differentiate critical versus noncritical patients. Acad. Radiol. 2021, 28, 10048–11057. [Google Scholar] [CrossRef]
- Biondi, R.; Curti, N.; Coppola, F.; Giampieri, E.; Vara, G.; Bartoletti, M.; Cattabriga, A.; Cocozza, M.A.; Ciccarese, F.; De Benedittis, C.; et al. Classification performance for COVID patient prognosis from automatic AI segmentation—A single-center study. Appl. Sci. 2021, 11, 5438. [Google Scholar] [CrossRef]
- Zheng, T.; Oda, M.; Wang, C.; Moriya, T.; Hayashi, Y.; Otake, Y.; Hashimoto, M.; Akashi, T.; Mori, M.; Takabatake, H.; et al. Unsupervised segmentation of COVID-19 infected lung clinical CT volumes using image inpainting and representation learning. In Medical Imaging 2021: Image Processing; SPIE: St Bellingham, WA, USA, 2021; Volume 11596, pp. 931–936. [Google Scholar]
- Çiçek, Ö.; Abdulkadir, A.; Lienkamp, S.; Brox, T.; Ronneberger, O. 3D U-Net: Learning dense volumetric segmentation from sparse annotation. In Medical Image Computing and Computer-Assisted Intervention–MICCAI 2016: 19th International Conference, Athens, Greece, 17-21 October 2016; Springer International Publishing: Berlin/Heidelberg, Germany, 2016; pp. 424–432. [Google Scholar]
- Bishop, C. Pattern Recognition and Machine Learning; Springer: Berlin/Heidelberg, Germany, 2006. [Google Scholar]
- Mongan, J.; Moy, L.; Kahn, C.E. Checklist for Artificial Intelligence in Medical Imaging (CLAIM): A Guide for Authors and Reviewers. Radiol. Artif. Intell. 2020, 2, e200029. [Google Scholar] [CrossRef] [PubMed]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD Statement. BMC Med. 2015, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Jun, M.; Cheng, G.; Yixin, W.; Xingle, A.; Jiantao, G.; Ziqi, Y.; Minqing, Z.; Xin, L.; Xueyuan, D.; Shucheng, C.; et al. COVID-19 CT Lung and Infection Segmentation Dataset. 2020. Available online: https://zenodo.org/records/3757476 (accessed on 5 March 2020).
- Müller, D.; Kramer, F. MIScnn: A framework for medical image segmentation with convolutional neural networks and deep learning. BMC Med. Imaging 2021, 21, 12. [Google Scholar] [CrossRef]
- Seyed, S.S.M.; Erdogmus, D.; Gholipour, A.; Salehi, S.S.M.; Erdogmus, D.; Gholipour, A. Lecture notes in computer science. In Tversky Loss Function for Image Segmentation Using 3D Fully Convolutional Deep Networks; Springer: Berlin/Heidelberg, Germany, 2017; pp. 379–387. [Google Scholar]
- Kingma, D.P.; Ba, J. Adam: A method for stochastic optimization. arXiv 2014, arXiv:1412.6980. [Google Scholar]
- Dice, L.R. Measures of the amount of ecologic association between species. Ecology 1945, 26, 297–302. [Google Scholar] [CrossRef]
- Giavarina, D. Understanding Bland Altman analysis. Biochem. Med. 2015, 25, 141–151. [Google Scholar] [CrossRef] [PubMed]
- DenOtter, T.D.; Schubert, J. Hounsfield Unit. [Updated 2023 Mar 6]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: www.ncbi.nlm.nih.gov/books/NBK547721 (accessed on 5 March 2024).
- Yuan, R.; Janzen, I.; Devnath, L.; Khattra, S.; Myers, R.; Lam, S.; MacAulay, C. MA19.11 Predicting Future Lung Cancer Risk with Low-Dose Screening CT Using an Artificial Intelligence Model. J. Thorac. Oncol. 2023, 18, S174. [Google Scholar] [CrossRef]
- Wang, H.; Wang, L.; Lee, E.H.; Zheng, J.; Zhang, W.; Halabi, S.; Liu, C.; Deng, K.; Song, J.; Yeom, K.W. Decoding COVID-19 pneumonia: Comparison of deep learning and radiomics CT image signatures. Eur. J. Nucl. Med. 2020, 48, 1478–1486. [Google Scholar] [CrossRef]
- Homayounieh, F.; Ebrahimian, S.; Babaei, R.; Mobin, H.K.; Zhang, E.; Bizzo, B.C.; Mohseni, I.; Digumarthy, S.R.; Kalra, M.K. CT Radiomics, Radiologists, and Clinical Information in Predicting Outcome of Patients with COVID-19 Pneumonia. Radiol. Cardiothorac. Imaging 2020, 2, e200322. [Google Scholar] [CrossRef]
| Parameters | Non-Contrast CT | Contrast-Enhanced CT |
|---|---|---|
| Voltage [kV] | 120 | 80 |
| Rotation time [s] | 0.5 | 0.33 |
| Slice thickness [mm] | 1.5 | 1.5 |
| Collimation [mm] | 0.6 | 0.6 |
| Image resolution | 512 × 512 | 512 × 512 |
| Slides reconstruction | 1.5 × 1 | 1.5 × 1 |
| Algorithm | 70f | I70f |
| Variable | n (%) |
|---|---|
| Male | 46 (71.9) |
| No symptoms * | 0 (0) |
| Fever * | 29 (45.3) |
| Cough * | 47 (73.4) |
| Expectoration * | 13 (20.3) |
| Dyspnea * | 54 (84.4) |
| Diabetes mellitus | 11 (17.2) |
| Hypertension | 26 (40.6) |
| Chronic obstructive pulmonary disease | 0 (0) |
| Cardiovascular disease | 5 (7.8) |
| Hospitalization | 56 (87.5) |
| Intensive care unit admission | 36 (56.3) |
| Death | 11 (17.2) |
| Hospitalization days ** | 20.5 [0, 84] |
| Intensive care unit days ** | 13.6 [0, 73] |
| DSC (μ ± σ) 3D-UNet (Initial Training) | DSC (μ ± σ) 3D-UNet (3 HITL Cycles) | DSC (μ ± σ) Expert Teams | |||
|---|---|---|---|---|---|
| Non-Contrast CT | Contrast-Enhanced CT | Non-Contrast CT | Contrast-Enhanced CT | Non-Contrast CT | |
| Normal lung parenchyma | 0.77 ± 0.15 | 0.84 ± 0.03 | 0.97 ± 0.02 | 0.97 ± 0.03 | 0.98 ± 0.01 |
| COVID-19 pneumonia | 0.31 ± 0.19 | 0.41 ± 0.14 | 0.82 ± 0.12 | 0.90 ± 0.11 | 0.86 ± 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vásquez-Venegas, C.; Sotomayor, C.G.; Ramos, B.; Castañeda, V.; Pereira, G.; Cabrera-Vives, G.; Härtel, S. Human-in-the-Loop—A Deep Learning Strategy in Combination with a Patient-Specific Gaussian Mixture Model Leads to the Fast Characterization of Volumetric Ground-Glass Opacity and Consolidation in the Computed Tomography Scans of COVID-19 Patients. J. Clin. Med. 2024, 13, 5231. https://doi.org/10.3390/jcm13175231
Vásquez-Venegas C, Sotomayor CG, Ramos B, Castañeda V, Pereira G, Cabrera-Vives G, Härtel S. Human-in-the-Loop—A Deep Learning Strategy in Combination with a Patient-Specific Gaussian Mixture Model Leads to the Fast Characterization of Volumetric Ground-Glass Opacity and Consolidation in the Computed Tomography Scans of COVID-19 Patients. Journal of Clinical Medicine. 2024; 13(17):5231. https://doi.org/10.3390/jcm13175231
Chicago/Turabian StyleVásquez-Venegas, Constanza, Camilo G. Sotomayor, Baltasar Ramos, Víctor Castañeda, Gonzalo Pereira, Guillermo Cabrera-Vives, and Steffen Härtel. 2024. "Human-in-the-Loop—A Deep Learning Strategy in Combination with a Patient-Specific Gaussian Mixture Model Leads to the Fast Characterization of Volumetric Ground-Glass Opacity and Consolidation in the Computed Tomography Scans of COVID-19 Patients" Journal of Clinical Medicine 13, no. 17: 5231. https://doi.org/10.3390/jcm13175231
APA StyleVásquez-Venegas, C., Sotomayor, C. G., Ramos, B., Castañeda, V., Pereira, G., Cabrera-Vives, G., & Härtel, S. (2024). Human-in-the-Loop—A Deep Learning Strategy in Combination with a Patient-Specific Gaussian Mixture Model Leads to the Fast Characterization of Volumetric Ground-Glass Opacity and Consolidation in the Computed Tomography Scans of COVID-19 Patients. Journal of Clinical Medicine, 13(17), 5231. https://doi.org/10.3390/jcm13175231






