Effects of the Severity of Stenosis on Clinical Outcomes of Indirect Decompression Using Oblique Lumbar Interbody Fusion
Abstract
1. Introduction
2. Materials and Methods
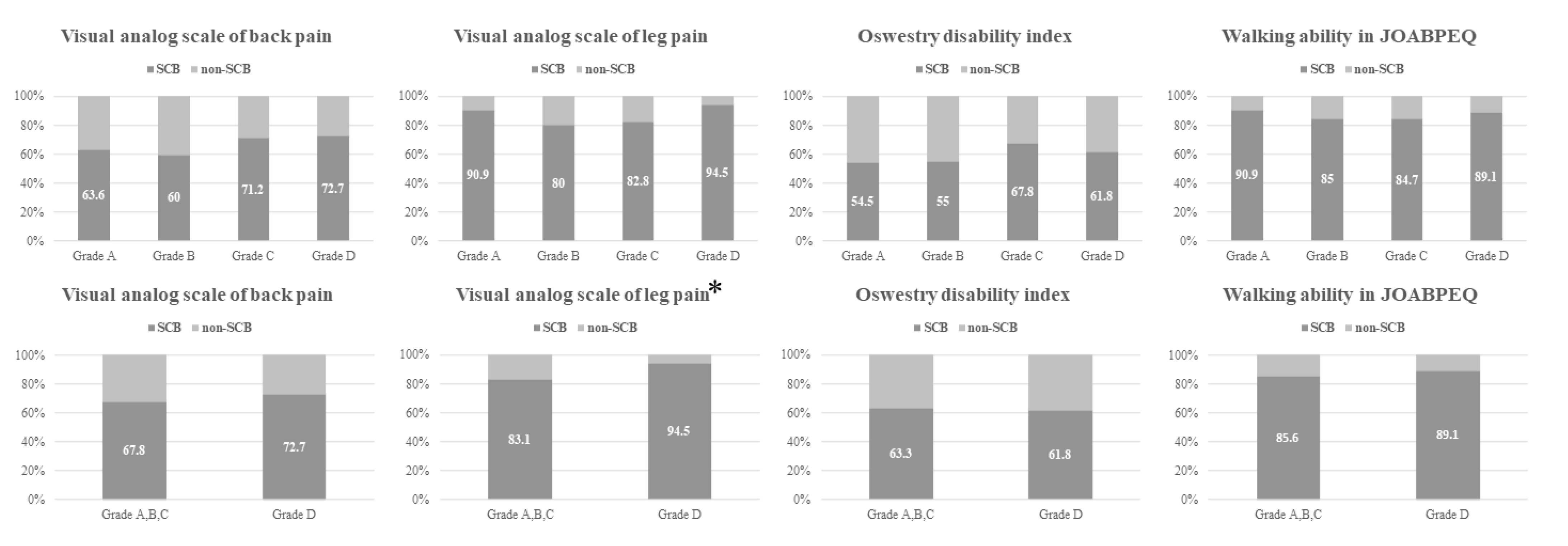
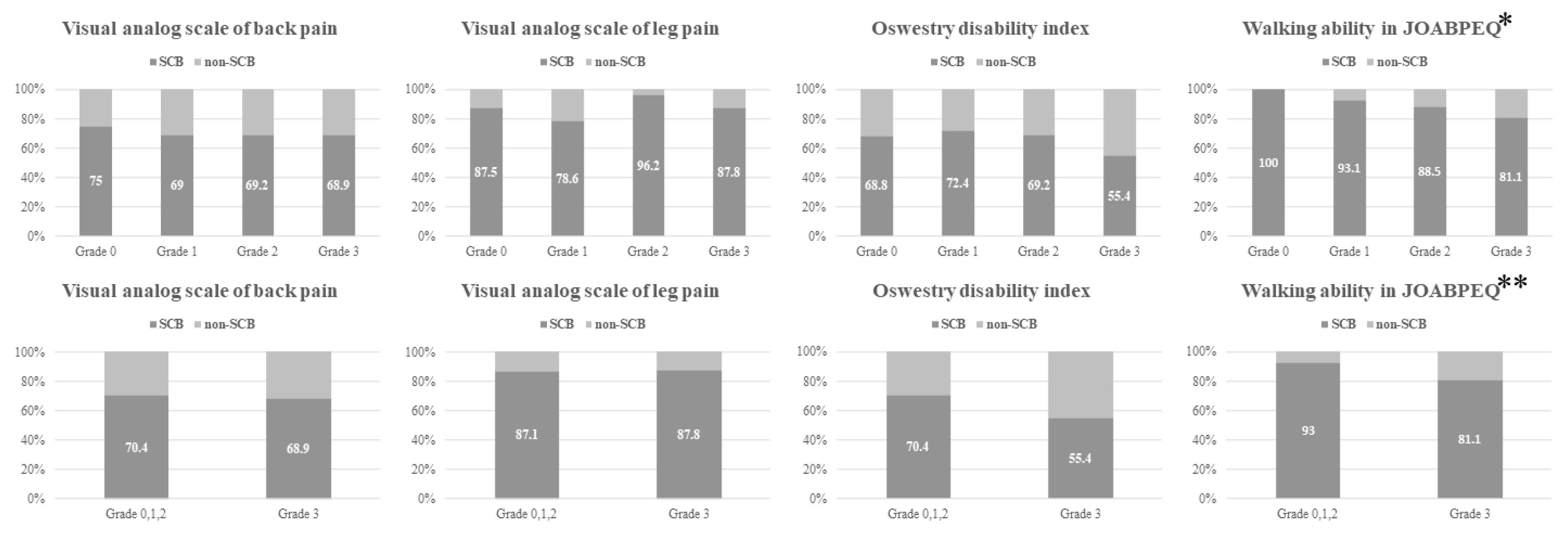
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kwon, J.W.; Moon, S.H.; Park, S.Y.; Park, S.J.; Park, S.R.; Suk, K.S.; Kim, H.S.; Lee, B.H. Lumbar Spinal Stenosis: Review Update 2022. Asian Spine J. 2022, 16, 789–798. [Google Scholar] [CrossRef]
- Lee, B.H.; Moon, S.H.; Suk, K.S.; Kim, H.S.; Yang, J.H.; Lee, H.M. Lumbar spinal stenosis: Pathophysiology and treatment principle: A narrative review. Asian Spine J. 2020, 14, 682–693. [Google Scholar] [CrossRef] [PubMed]
- Melancia, J.L.; Francisco, A.F.; Antunes, J.L. Spinal stenosis. Handb. Clin. Neurol. 2014, 119, 541–549. [Google Scholar] [CrossRef]
- Fujibayashi, S.; Hynes, R.A.; Otsuki, B.; Kimura, H.; Takemoto, M.; Matsuda, S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine 2015, 40, E175–E182. [Google Scholar] [CrossRef]
- Kim, H.; Chang, B.S.; Chang, S.Y. Pearls and pitfalls of oblique lateral interbody fusion: A comprehensive narrative review. Neurospine 2022, 19, 163–176. [Google Scholar] [CrossRef]
- Choi, J.Y.; Park, S.M.; Kim, H.J.; Yeom, J.S. Recent Updates on Minimally Invasive Spine Surgery: Techniques, Technologies, and Indications. Asian Spine J. 2022, 16, 1013–1021. [Google Scholar] [CrossRef]
- Chang, S.Y.; Nam, Y.; Lee, J.; Chang, B.S.; Lee, C.K.; Kim, H. Clinical significance of radiologic improvement following single-level oblique lateral interbody fusion with percutaneous pedicle screw fixation. Orthopedics 2020, 43, e283–e290. [Google Scholar] [CrossRef] [PubMed]
- Sato, J.; Ohtori, S.; Orita, S.; Yamauchi, K.; Eguchi, Y.; Ochiai, N.; Kuniyoshi, K.; Aoki, Y.; Nakamura, J.; Miyagi, M.; et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur. Spine J. 2017, 26, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Mahatthanatrakul, A.; Kim, H.S.; Lin, G.X.; Kim, J.S. Decreasing thickness and remodeling of ligamentum flavum after oblique lumbar interbody fusion. Neuroradiology 2020, 62, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, H.; Zhang, N.; Wang, Z.-W.; Zhao, T.-F.; Chen, L.-W.; Chen, G.; Chen, Q.-X.; Li, F.-C. Radiographic and clinical outcome of lateral lumbar interbody fusion for extreme lumbar spinal stenosis of Schizas grade D: A retrospective study. BMC Musculoskelet. Disord. 2020, 21, 259. [Google Scholar] [CrossRef]
- Formica, M.; Quarto, E.; Zanirato, A.; Mosconi, L.; Vallerga, D.; Zotta, I.; Baracchini, M.L.; Formica, C.; Felli, L. Lateral lumbar interbody fusion: What is the evidence of indirect neural decompression? A systematic review of the literature. HSS J. 2020, 16, 143–154. [Google Scholar] [CrossRef]
- Buckland, A.J.; Ashayeri, K.; Leon, C.; Cheng, I.; Thomas, J.A.; Braly, B.; Kwon, B.; Eisen, L. Anterior column reconstruction of the lumbar spine in the lateral decubitus position: Anatomical and patient-related considerations for ALIF, anterior-to-psoas, and transpsoas LLIF approaches. Eur. Spine J. 2022, 31, 2175–2187. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Xu, T.Z.; Zhang, N.; Chen, Q.X.; Li, F.C. Predictors for second-stage posterior direct decompression after lateral lumbar interbody fusion: A review of five hundred fifty-seven patients in the past five years. Int. Orthop. 2022, 46, 1101–1109. [Google Scholar] [CrossRef]
- Takahashi, Y.; Funao, H.; Yoshida, K.; Sasao, Y.; Nishiyama, M.; Isogai, N.; Ishii, K. Sequential MRI changes after lateral lumbar interbody fusion in spondylolisthesis with mild and severe lumbar spinal stenosis. World Neurosurg. 2021, 152, e289–e296. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, A.; Katoh, H.; Sakai, D.; Sato, M.; Watanabe, M. Radiographic and clinical evaluation of single-level lateral interbody fusion in patients with severe stenosis analyzed using cluster analysis. Medicine 2021, 100, e27775. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Fujibayashi, S.; Otsuki, B.; Murata, K.; Matsuda, S. Indirect decompression with lateral interbody fusion for severe degenerative lumbar spinal stenosis: Minimum 1-year MRI follow-up. J. Neurosurg. Spine 2020, 33, 27–34. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry disability index. Spine 2000, 25, 2940–2952; discussion 2952. [Google Scholar] [CrossRef] [PubMed]
- Fukui, M.; Chiba, K.; Kawakami, M.; Kikuchi, S.; Konno, S.; Miyamoto, M.; Seichi, A.; Shimamura, T.; Shirado, O.; Taguchi, T.; et al. JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) The report on the development of revised versions April 16, 2007: The subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on low back pain and cervical myelopathy evaluation. J. Orthop. Sci. Rev. Version 2009, 14, 348–365. [Google Scholar] [CrossRef]
- Glassman, S.D.; Copay, A.G.; Berven, S.H.; Polly, D.W.; Subach, B.R.; Carreon, L.Y. Defining substantial clinical benefit following lumbar spine arthrodesis. J. Bone Jt. Surg. Am. 2008, 90, 1839–1847. [Google Scholar] [CrossRef]
- Kasai, Y.; Fukui, M.; Takahashi, K.; Ohtori, S.; Takeuchi, D.; Hashizume, H.; Kanamori, M.; Hosono, N.; Kanchiku, T.; Wada, E.; et al. Verification of the sensitivity of functional scores for treatment results—Substantial clinical benefit thresholds for the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ). J. Orthop. Sci. 2017, 22, 665–669. [Google Scholar] [CrossRef]
- Schizas, C.; Kulik, G. Decision-making in lumbar spinal stenosis: A survey on the influence of the morphology of the dural sac. J. Bone Jt. Surg. Br. 2012, 94, 98–101. [Google Scholar] [CrossRef]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.-J.; Kim, H.-J.; Chung, S.K.; Kang, H.S. A practical MRI grading system for lumbar foraminal stenosis. AJR Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.; Marchi, L.; Coutinho, E.; Pimenta, L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine 2010, 35, S331–S337. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.T.; Xu, D.S.; Cole, T.S.; Alhilali, L.M.; Godzik, J.; Estrada, S.A.; Giraldo, J.P.; Wewel, J.T.; Morgan, C.D.; Zhou, J.J.; et al. Predictors of indirect neural decompression in minimally invasive transpsoas lateral lumbar interbody fusion. J. Neurosurg. Spine 2021, 35, 80–90. [Google Scholar] [CrossRef]
- Choi, K.-C.; Ahn, Y.; Kang, B.-U.; Jang, J.-H.; Kim, K.-K.; Shin, Y.H.; Choi, J.-O.; Lee, S.-H. Failed anterior lumbar interbody fusion due to incomplete foraminal decompression. Acta Neurochir. 2011, 153, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Rentenberger, C.; Okano, I.; Salzmann, S.N.; Winter, F.; Plais, N.; Burkhard, M.D.; Shue, J.; Sama, A.A.; Cammisa, F.P.; Girardi, F.P.; et al. Perioperative risk factors for early revisions in stand-alone lateral lumbar interbody fusion. World Neurosurg. 2020, 134, e657–e663. [Google Scholar] [CrossRef] [PubMed]
- Mahatthanatrakul, A.; Kotheeranurak, V.; Lin, G.-X.; Hur, J.-W.; Chung, H.-J.; Lokanath, Y.K.; Pakdeenit, B.; Kim, J.-S. Do obliquity and position of the oblique lumbar interbody fusion cage influence the degree of indirect decompression of foraminal stenosis? J. Korean Neurosurg. Soc. 2022, 65, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Malham, G.M.; Parker, R.M.; Goss, B.; Blecher, C.M.; Ballok, Z.E. Indirect foraminal decompression is independent of metabolically active facet arthropathy in extreme lateral interbody fusion. Spine 2014, 39, E1303–E1310. [Google Scholar] [CrossRef] [PubMed]
- Koike, Y.; Kotani, Y.; Terao, H.; Iwasaki, N. Comparison of outcomes of oblique lateral interbody fusion with percutaneous posterior fixation in lateral position and minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis. Asian Spine J. 2021, 15, 97–106. [Google Scholar] [CrossRef]
- Takaoka, H.; Inage, K.; Eguchi, Y.; Shiga, Y.; Furuya, T.; Maki, S.; Aoki, Y.; Inoue, M.; Fujiyoshi, T.; Miyamoto, T.; et al. Comparison between intervertebral oblique lumbar interbody fusion and transforaminal lumbar interbody fusion: A multicenter study. Sci. Rep. 2021, 11, 16673. [Google Scholar] [CrossRef]
- Zhang, Q.Y.; Tan, J.; Huang, K.; Xie, H.Q. Minimally invasive transforaminal lumbar interbody fusion versus oblique lateral interbody fusion for lumbar degenerative disease: A meta-analysis. BMC Musculoskelet. Disord. 2021, 22, 802. [Google Scholar] [CrossRef] [PubMed]
- Malham, G.M.; Parker, R.M.; Goss, B.; Blecher, C.M. Clinical results and limitations of indirect decompression in spinal stenosis with laterally implanted interbody cages: Results from a prospective cohort study. Eur. Spine J. 2015, 24 (Suppl. S3), 339–345. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Ramirez, R.; Lang, G.; Moriguchi, Y.; Elowitz, E.; Corredor, J.A.; Avila, M.J.; Gotfryd, A.; Alimi, M.; Gandevia, L.; Härtl, R. Are locked facets a contraindication for extreme lateral interbody fusion? World Neurosurg. 2017, 100, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.Y.; Chae, I.S.; Mok, S.; Park, S.C.; Chang, B.S.; Kim, H. Can Indirect Decompression Reduce Adjacent Segment Degeneration and the Associated Reoperation Rate after Lumbar Interbody Fusion? A Systemic Review and Meta-analysis. World Neurosurg. 2021, 153, e435–e445. [Google Scholar] [CrossRef]



| Grade A | Grade B | Grade C | Grade D | |
|---|---|---|---|---|
| Central lesion [21] | Mild stenosis and visible CSF | Moderate stenosis and visible rootlets | Severe stenosis and invisible rootlets | Extreme stenosis, invisible rootlets, and no epidural fat |
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | |
| Foraminal lesion [22] | Normal | Perineural fat obliteration in the two opposing directions | Perineural fat obliteration in the four directions | Nerve root collapse or morphologic changes |
| Index | Maximum Grade of Central Stenosis | ||||
|---|---|---|---|---|---|
| A (n = 11) | B (n=20) | C (n = 59) | D (n = 55) | p-Value | |
| Age (mean ± SD, years) | 66.27 ± 9.96 | 69.15 ± 6.92 | 67.53 ± 8.09 | 70.89 ± 6.77 | 0.076 |
| Sex, M:F (n) | 3:8 | 4:16 | 22:37 | 16:39 | 0.496 |
| BMI (mean ± SD, kg/m2) | 24.88 ± 7.39 | 22.23 ± 4.96 | 25.83 ± 6.74 | 24.74 ± 6.37 | 0.201 |
| Indexes | Maximum Grade of Foraminal Stenosis | ||||
| 0 (n = 16) | 1 (n = 29) | 2 (n = 26) | 3 (n = 74) | p-Value | |
| Age (mean ± SD, years) | 67.06 ± 7.8 | 66.59 ± 9.42 | 70.5 ± 7.39 | 69.7 ± 6.91 | 0.142 |
| Sex, M:F (n) | 4:12 | 7:22 | 11:15 | 23:51 | 0.482 |
| BMI (mean ± SD, kg/m2) | 23.33 ± 7.8 | 25.97 ± 6.76 | 25.54 ± 7.44 | 24.49 ± 5.69 | 0.522 |
| Characteristics | OR (95% CI) | p-Value |
|---|---|---|
| Age (years) | 0.92 (0.88–0.98) | 0.004 |
| Preoperative diagnosis | 0.040 | |
| Degenerative spondylolisthesis * | 2.68 (1.23–5.84) | 0.013 |
| Adjacent segment disease * | 1.15 (0.25–5.40) | 0.856 |
| Previous operation history in index surgical level | 0.240 | |
| Open posterior fusion | 0.124 | |
| The number of surgical levels | 0.307 | |
| Severe foraminal stenosis | 0.547 | |
| Foraminal osteophytes of SAP | 0.20 (0.05–0.81) | 0.024 |
| Instability | 0.420 |
| Characteristics | OR (95% CI) | p-Value |
|---|---|---|
| Previous operation history in index surgical level | 0.15 (0.05–0.45) | 0.001 |
| Open posterior fusion | 0.344 | |
| Maximum grade of foraminal stenosis | 0.478 | |
| Severe foraminal stenosis | 0.415 | |
| Foraminal osteophytes of SAP | 0.22 (0.06–0.86) | 0.030 |
| Facet cyst | 0.115 | |
| Cage subsidence | 0.191 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, D.-H.; Baek, J.; Chang, B.-S.; Kim, H.; Hong, S.H.; Chang, S.Y. Effects of the Severity of Stenosis on Clinical Outcomes of Indirect Decompression Using Oblique Lumbar Interbody Fusion. J. Clin. Med. 2024, 13, 4421. https://doi.org/10.3390/jcm13154421
Kang D-H, Baek J, Chang B-S, Kim H, Hong SH, Chang SY. Effects of the Severity of Stenosis on Clinical Outcomes of Indirect Decompression Using Oblique Lumbar Interbody Fusion. Journal of Clinical Medicine. 2024; 13(15):4421. https://doi.org/10.3390/jcm13154421
Chicago/Turabian StyleKang, Dong-Ho, Jonghyuk Baek, Bong-Soon Chang, Hyoungmin Kim, Seong Hwa Hong, and Sam Yeol Chang. 2024. "Effects of the Severity of Stenosis on Clinical Outcomes of Indirect Decompression Using Oblique Lumbar Interbody Fusion" Journal of Clinical Medicine 13, no. 15: 4421. https://doi.org/10.3390/jcm13154421
APA StyleKang, D.-H., Baek, J., Chang, B.-S., Kim, H., Hong, S. H., & Chang, S. Y. (2024). Effects of the Severity of Stenosis on Clinical Outcomes of Indirect Decompression Using Oblique Lumbar Interbody Fusion. Journal of Clinical Medicine, 13(15), 4421. https://doi.org/10.3390/jcm13154421







