Rapid and Precise Computation of Fractional Flow Reserve from Routine Two-Dimensional Coronary Angiograms Based on Fluid Mechanics: The Pilot FFR2D Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Population
2.2. Invasive FFR Measurement
2.3. Fluid Mechanics Framework
- Measuring the mean arterial pressure (MAP) in a coronary artery inlet and regressing a hyperemic MAP based on the literature (Pa).
- Acquiring a two-dimensional angiography image and delineating the vascular contours to compute the vessel geometric characteristics.
- Measuring the time taken for blood to flow across the interrogated vessel segment and calculating the volumetric flow rate of the blood vessel.
- Inferring a state of maximum hyperemia based on the regression of experimental data.
- Improving precision of computed Δp by k-fold cross-validation analysis of hyperemic and resting pressure measurements.
- Calculating fractional flow reserve FFR2D based on the simple formula of FFR2D = Pd/Pa.
2.4. Outcomes and Statistics
3. Results
3.1. Patient Cohort
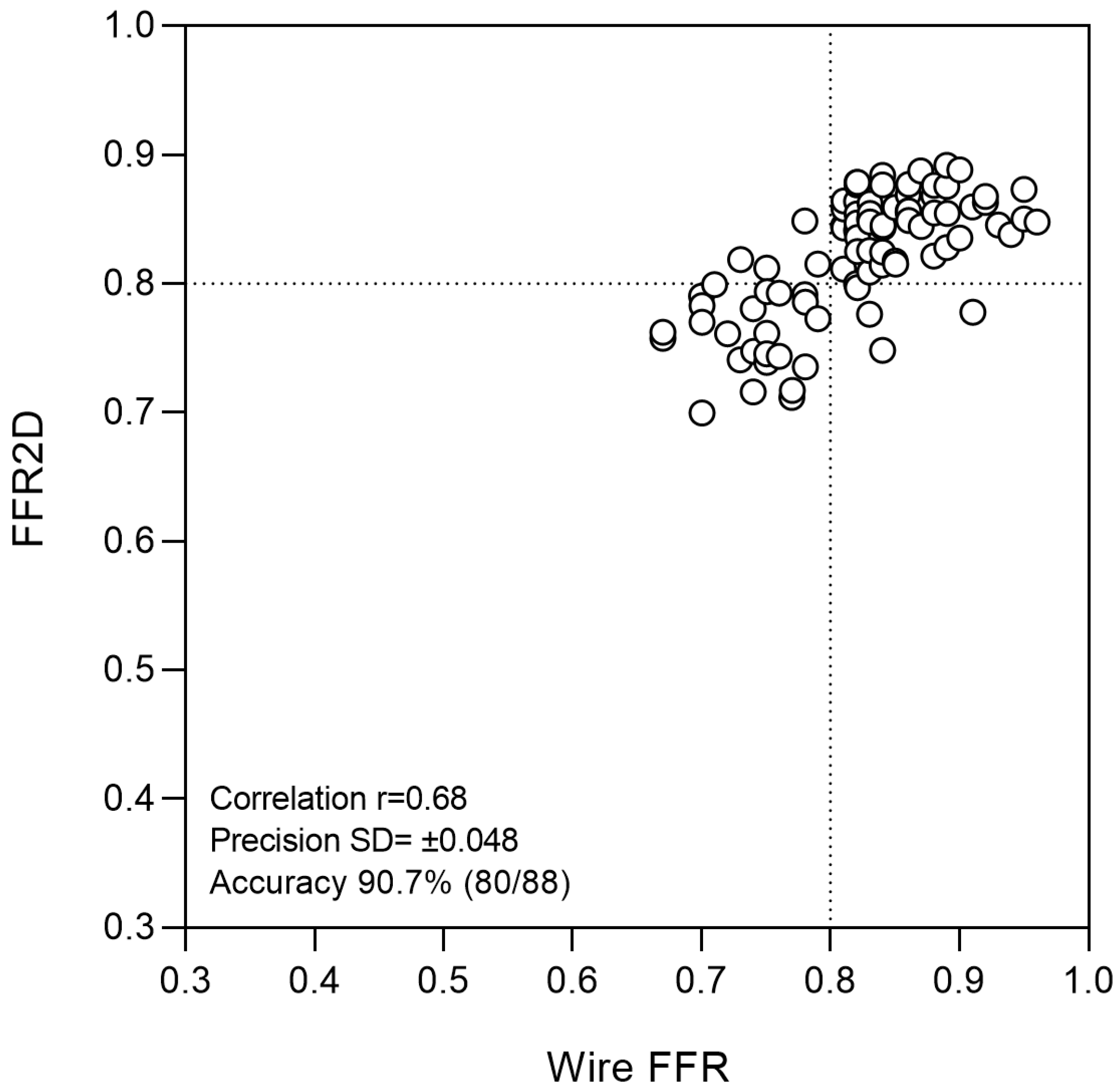
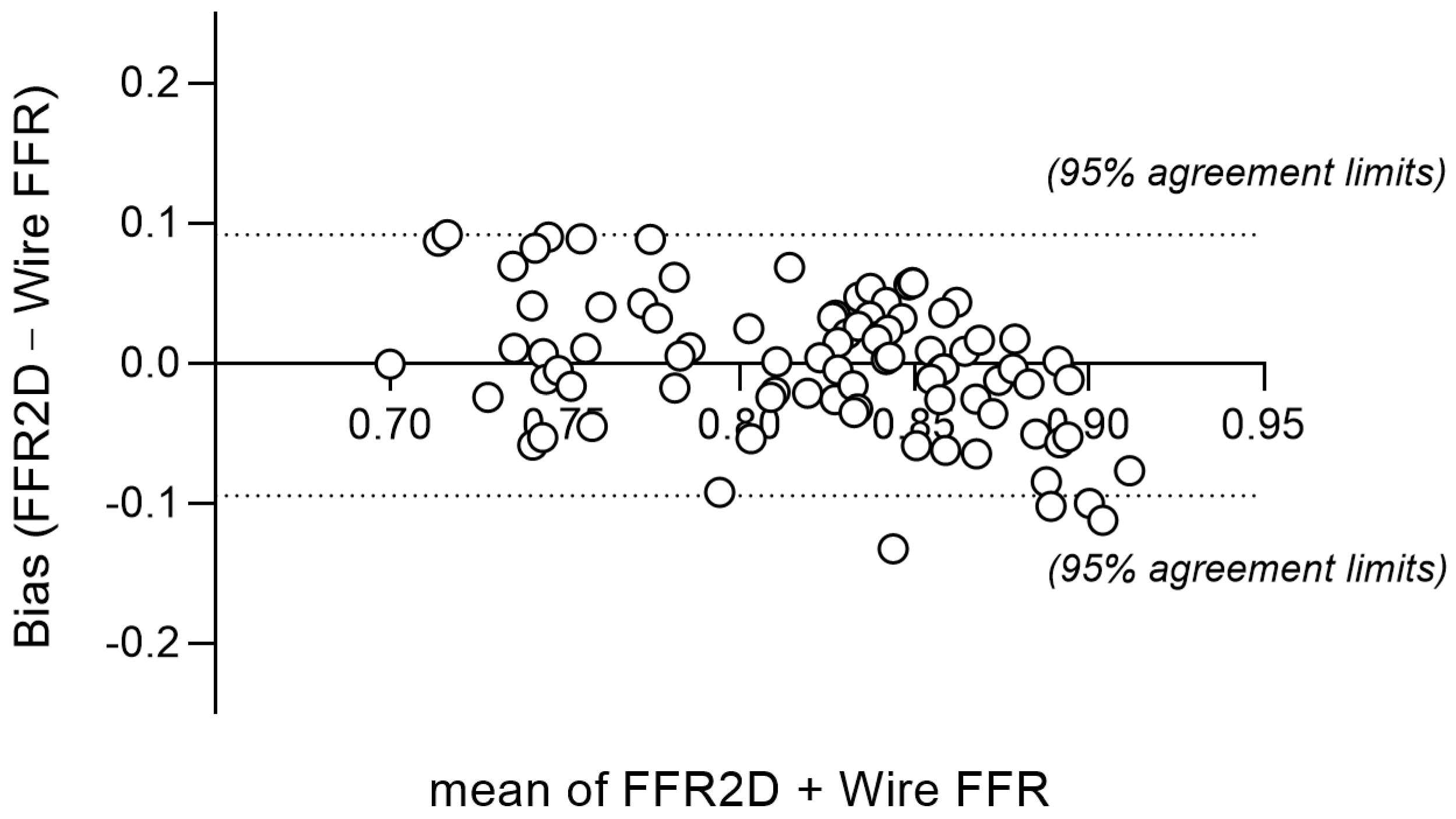
3.2. Diagnostic Performance
3.3. Subgroup Analyses
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Corcoran, D.; Hennigan, B.; Berry, C. Fractional flow reserve: A clinical perspective. Int. J. Cardiovasc. Imaging 2017, 33, 961–974. [Google Scholar] [CrossRef] [PubMed]
- van de Hoef, T.P.; Meuwissen, M.; Escaned, J.; Davies, J.E.; Siebes, M.; Spaan, J.A.; Piek, J.J. Fractional flow reserve as a surrogate for inducible myocardial ischaemia. Nat. Rev. Cardiol. 2013, 10, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, M.; Johnson, N.P.; Fearon, W.F.; Mintz, G.S.; Stone, G.W.; Oldroyd, K.G.; De Bruyne, B.; Pijls, N.H.J.; Maehara, A.; Jeremias, A. Accuracy of Fractional Flow Reserve Measurements in Clinical Practice: Observations From a Core Laboratory Analysis. JACC Cardiovasc. Interv. 2017, 10, 1392–1401. [Google Scholar] [CrossRef] [PubMed]
- Gotberg, M.; Cook, C.M.; Sen, S.; Nijjer, S.; Escaned, J.; Davies, J.E. The Evolving Future of Instantaneous Wave-Free Ratio and Fractional Flow Reserve. J. Am. Coll. Cardiol. 2017, 70, 1379–1402. [Google Scholar] [CrossRef]
- Blanco, P.J.; Bulant, C.A.; Muller, L.O.; Talou, G.D.M.; Bezerra, C.G.; Lemos, P.A.; Feijoo, R.A. Comparison of 1D and 3D Models for the Estimation of Fractional Flow Reserve. Sci. Rep. 2018, 8, 17275. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.; Zhang, J.M.; Su, B.; Tan, R.S.; Allen, J.C.; Kassab, G.S. Application of Patient-Specific Computational Fluid Dynamics in Coronary and Intra-Cardiac Flow Simulations: Challenges and Opportunities. Front. Physiol. 2018, 9, 742. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Lv, S.; Song, X.; Yuan, F.; Xu, F.; Zhang, M.; Yan, S.; Cao, X. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention: A meta-analysis. Heart 2015, 101, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Gould, K.L. Pressure-flow characteristics of coronary stenoses in unsedated dogs at rest and during coronary vasodilation. Circ. Res. 1978, 43, 242–253. [Google Scholar] [CrossRef]
- Young, D.F.; Cholvin, N.R.; Kirkeeide, R.L.; Roth, A.C. Hemodynamics of arterial stenoses at elevated flow rates. Circ. Res. 1977, 41, 99–107. [Google Scholar] [CrossRef]
- Gould, K.L.; Lipscomb, K.; Hamilton, G.W. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am. J. Cardiol. 1974, 33, 87–94. [Google Scholar] [CrossRef]
- Kirkeeide, R.L. Coronary obstructions, morphology and physiologic significance. Quant. Coron. Arter. 1991, 117, 229–244. [Google Scholar]
- Dodds, S.R. The haemodynamics of asymmetric stenoses. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2002, 24, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Young, D.F.; Tsai, F.Y. Flow characteristics in models of arterial stenoses. I. Steady flow. J. Biomech. 1973, 6, 395–410. [Google Scholar] [CrossRef]
- Young, D.F.; Tsai, F.Y. Flow characteristics in models of arterial stenoses. II. Unsteady flow. J. Biomech. 1973, 6, 547–559. [Google Scholar] [CrossRef]
- Gibson, C.M.; Cannon, C.P.; Daley, W.L.; Dodge, J.T., Jr.; Alexander, B., Jr.; Marble, S.J.; McCabe, C.H.; Raymond, L.; Fortin, T.; Poole, W.K.; et al. TIMI frame count: A quantitative method of assessing coronary artery flow. Circulation 1996, 93, 879–888. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Petraco, R.; Sen, S.; Nijjer, S.; Echavarria-Pinto, M.; Escaned, J.; Francis, D.P.; Davies, J.E. Fractional flow reserve-guided revascularization: Practical implications of a diagnostic gray zone and measurement variability on clinical decisions. JACC. Cardiovasc. Interv. 2013, 6, 222–225. [Google Scholar] [CrossRef] [PubMed]
- Pijls, N.H.; van Son, J.A.; Kirkeeide, R.L.; De Bruyne, B.; Gould, K.L. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation 1993, 87, 1354–1367. [Google Scholar] [CrossRef] [PubMed]
- Young, D.F.; Cholvin, N.R.; Roth, A.C. Pressure drop across artificially induced stenoses in the femoral arteries of dogs. Circ. Res. 1975, 36, 735–743. [Google Scholar] [CrossRef]
- Lee, J.M.; Choi, K.H.; Park, J.; Hwang, D.; Rhee, T.M.; Kim, J.; Park, J.; Kim, H.Y.; Jung, H.W.; Cho, Y.K.; et al. Physiological and Clinical Assessment of Resting Physiological Indexes. Circulation 2019, 139, 889–900. [Google Scholar] [CrossRef]
- Johnson, N.P.; Kirkeeide, R.L.; Asrress, K.N.; Fearon, W.F.; Lockie, T.; Marques, K.M.; Pyxaras, S.A.; Rolandi, M.C.; van’t Veer, M.; De Bruyne, B.; et al. Does the instantaneous wave-free ratio approximate the fractional flow reserve? J. Am. Coll. Cardiol. 2013, 61, 1428–1435. [Google Scholar] [CrossRef]
- Gonzalez, J.A.; Lipinski, M.J.; Flors, L.; Shaw, P.W.; Kramer, C.M.; Salerno, M. Meta-Analysis of Diagnostic Performance of Coronary Computed Tomography Angiography, Computed Tomography Perfusion, and Computed Tomography-Fractional Flow Reserve in Functional Myocardial Ischemia Assessment Versus Invasive Fractional Flow Reserve. Am. J. Cardiol. 2015, 116, 1469–1478. [Google Scholar] [CrossRef]
- Weir-McCall, J.R.; Fairbairn, T.A. Fractional Flow Reserve Derived from CT: The State of Play in 2020. Radiol. Cardiothorac. Imaging 2020, 2, e190153. [Google Scholar] [CrossRef]
- Norgaard, B.L.; Leipsic, J.; Gaur, S.; Seneviratne, S.; Ko, B.S.; Ito, H.; Jensen, J.M.; Mauri, L.; De Bruyne, B.; Bezerra, H.; et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J. Am. Coll. Cardiol. 2014, 63, 1145–1155. [Google Scholar] [CrossRef] [PubMed]
- Westra, J.; Tu, S.; Winther, S.; Nissen, L.; Vestergaard, M.B.; Andersen, B.K.; Holck, E.N.; Fox Maule, C.; Johansen, J.K.; Andreasen, L.N.; et al. Evaluation of Coronary Artery Stenosis by Quantitative Flow Ratio During Invasive Coronary Angiography: The WIFI II Study (Wire-Free Functional Imaging II). Circulation. Cardiovasc. Imaging 2018, 11, e007107. [Google Scholar] [CrossRef] [PubMed]
- Tu, S.; Westra, J.; Yang, J.; von Birgelen, C.; Ferrara, A.; Pellicano, M.; Nef, H.; Tebaldi, M.; Murasato, Y.; Lansky, A.; et al. Diagnostic Accuracy of Fast Computational Approaches to Derive Fractional Flow Reserve From Diagnostic Coronary Angiography: The International Multicenter FAVOR Pilot Study. JACC. Cardiovasc. Interv. 2016, 9, 2024–2035. [Google Scholar] [CrossRef] [PubMed]
- Westra, J.; Andersen, B.K.; Campo, G.; Matsuo, H.; Koltowski, L.; Eftekhari, A.; Liu, T.; Di Serafino, L.; Di Girolamo, D.; Escaned, J.; et al. Diagnostic Performance of In-Procedure Angiography-Derived Quantitative Flow Reserve Compared to Pressure-Derived Fractional Flow Reserve: The FAVOR II Europe-Japan Study. J. Am. Heart Assoc. 2018, 7, e009603. [Google Scholar] [CrossRef]
- Cortes, C.; Carrasco-Moraleja, M.; Aparisi, A.; Rodriguez-Gabella, T.; Campo, A.; Gutierrez, H.; Julca, F.; Gomez, I.; San Roman, J.A.; Amat-Santos, I.J. Quantitative flow ratio-Meta-analysis and systematic review. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2021, 97, 807–814. [Google Scholar] [CrossRef]
- Witberg, G.; De Bruyne, B.; Fearon, W.F.; Achenbach, S.; Engstrom, T.; Matsuo, H.; Kornowski, R. Diagnostic Performance of Angiogram-Derived Fractional Flow Reserve: A Pooled Analysis of 5 Prospective Cohort Studies. JACC. Cardiovasc. Interv. 2020, 13, 488–497. [Google Scholar] [CrossRef]
- Fearon, W.F.; Achenbach, S.; Engstrom, T.; Assali, A.; Shlofmitz, R.; Jeremias, A.; Fournier, S.; Kirtane, A.J.; Kornowski, R.; Greenberg, G.; et al. Accuracy of Fractional Flow Reserve Derived From Coronary Angiography. Circulation 2019, 139, 477–484. [Google Scholar] [CrossRef]
- Bech, G.J.; De Bruyne, B.; Pijls, N.H.; de Muinck, E.D.; Hoorntje, J.C.; Escaned, J.; Stella, P.R.; Boersma, E.; Bartunek, J.; Koolen, J.J.; et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: A randomized trial. Circulation 2001, 103, 2928–2934. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Hu, Y.; Xiang, P.; Sheng, X.; Leng, X.; Yang, X.; Dong, L.; Li, C.; Sun, Y.; Jiang, J.; et al. The diagnostic performance of AccuFFRangio for evaluating coronary artery stenosis under different computational conditions. Quant. Imaging Med. Surg. 2023, 13, 2496–2506. [Google Scholar] [CrossRef] [PubMed]


Inclusion Criteria:
|
| Baseline Variables | Sample n = 88 |
|---|---|
| Age (years) * | 65.8 ± 10.6 |
| Male gender | 66/88 (75.0%) |
| Hyperlipidemia | 68/88 (77.3%) |
| Smoking | 59/88 (67.0%) |
| Diabetes | 20/88 (22.7%) |
| Hypertension | 73/88 (83.0%) |
| Family CAD history | 13/88 (14.8%) |
| Previous PCI intervention | 28/88 (31.8%) |
| Previous CABG surgery | 0/88 (0.0%) |
| Asymptomatic positive stress test | 50/88 (56.8%) |
| Stable angina | 18/88 (20.5%) |
| Unstable angina | 20/88 (22.7%) |
| Ejection fraction (%) * | 53.2 ± 9.8 |
| Radial access | 88/88 (100%) |
| Adenosine intravenous | 88/88 (100%) |
| Vessel bifurcations | 27/88 (30.7%) |
| Vessel calcifications | 24/88 (27.3%) |
| Tandem lesions | 10/88 (11.4%) |
| Anatomy—index artery | |
| LAD | 74/88 (84.1%) |
| RCA | 9/88 (10.2%) |
| LCX | 5/88 (5.7%) |
| Minimum lumen diameter * | 1.76 ± 0.48 mm |
| Reference vessel diameter * | 3.25 ± 0.56 mm |
| Percent (%) diameter stenosis * | 45.7 ± 11.0% |
| Statistical Test | FFR2D (≤0.80) | 2D-QCA (50%DS) |
|---|---|---|
| Disease prevalence | 31.8 (22.3–42.6)% | 31.8 (22.3–42.6)% |
| Sensitivity | 85.7 (67.3–95.9)% | 57.1 (37.2–75.5)% |
| Specificity | 93.3 (83.8–98.2)% | 71.7 (58.6–82.6)% |
| Accuracy | 90.9 (82.9–96.0)% | 67.1 (56.2–76.7)% |
| Positive predictive value | 85.7 (69.7–94.0)% | 48.5 (30.8–66.5)% |
| Negative predictive value | 93.3 (84.9–97.2)% | 78.2 (64.9–88.2)% |
| Positive likelihood ratio | 13.0 (4.93–33.54) | 2.02 (1.21–3.37) |
| Negative likelihood ratio | 0.15 (0.06–0.38) | 0.60 (0.38–0.94) |
| ROC area under the curve | 0.95 (0.91–0.99) | 0.70 (0.59–0.82) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsigkas, G.G.; Bourantas, G.C.; Moulias, A.; Karamasis, G.V.; Bekiris, F.V.; Davlouros, P.; Katsanos, K. Rapid and Precise Computation of Fractional Flow Reserve from Routine Two-Dimensional Coronary Angiograms Based on Fluid Mechanics: The Pilot FFR2D Study. J. Clin. Med. 2024, 13, 3831. https://doi.org/10.3390/jcm13133831
Tsigkas GG, Bourantas GC, Moulias A, Karamasis GV, Bekiris FV, Davlouros P, Katsanos K. Rapid and Precise Computation of Fractional Flow Reserve from Routine Two-Dimensional Coronary Angiograms Based on Fluid Mechanics: The Pilot FFR2D Study. Journal of Clinical Medicine. 2024; 13(13):3831. https://doi.org/10.3390/jcm13133831
Chicago/Turabian StyleTsigkas, Grigorios G., George C. Bourantas, Athanasios Moulias, Grigorios V. Karamasis, Fivos V. Bekiris, Periklis Davlouros, and Konstantinos Katsanos. 2024. "Rapid and Precise Computation of Fractional Flow Reserve from Routine Two-Dimensional Coronary Angiograms Based on Fluid Mechanics: The Pilot FFR2D Study" Journal of Clinical Medicine 13, no. 13: 3831. https://doi.org/10.3390/jcm13133831
APA StyleTsigkas, G. G., Bourantas, G. C., Moulias, A., Karamasis, G. V., Bekiris, F. V., Davlouros, P., & Katsanos, K. (2024). Rapid and Precise Computation of Fractional Flow Reserve from Routine Two-Dimensional Coronary Angiograms Based on Fluid Mechanics: The Pilot FFR2D Study. Journal of Clinical Medicine, 13(13), 3831. https://doi.org/10.3390/jcm13133831







