Impact of Guideline-Directed Drug Therapy after ST-Elevation Myocardial Infarction on Outcome in Young Patients—Age and Sex-Specific Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Missing Data
2.2. Endpoints
2.3. Ethic Statement and Data Accessibility Statement
2.3.1. Ethic Statement
2.3.2. Data Accessibility Statement
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Mortality and Predictors for 30- and 90-Day Mortality after STEMI
3.3. Clinical Effect of Guideline-Directed Drug Therapy on Mortality
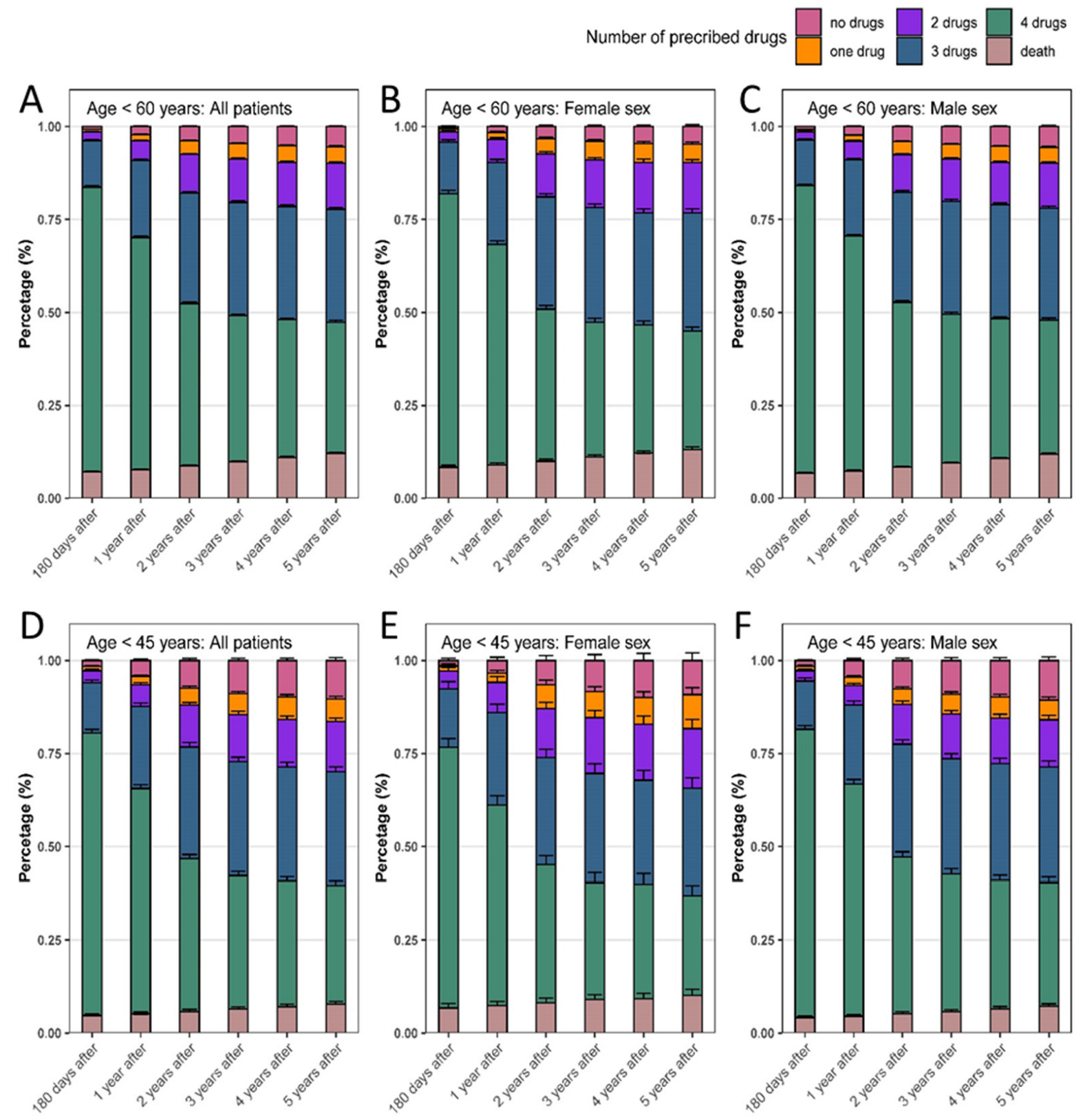
3.4. Guideline-Directed Drug Therapy after STEMI
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bortnick, A.E.; Shahid, M.; Shitole, S.G.; Park, M.; Broder, A.; Rodriguez, C.J.; Scheuer, J.; Faillace, R.; Kizer, J.R. Outcomes of ST-elevation myocardial infarction by age and sex in a low-income urban community: The Montefiore STEMI Registry. Clin. Cardiol. 2020, 43, 1100–1109. [Google Scholar] [CrossRef] [PubMed]
- Kytö, V.; Sipilä, J.; Rautava, P. Gender and in-hospital mortality of ST-segment elevation myocardial infarction (from a multihospital nationwide registry study of 31,689 patients). Am. J. Cardiol. 2015, 115, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Zasada, W.; Bobrowska, B.; Plens, K.; Dziewierz, A.; Siudak, Z.; Surdacki, A.; Dudek, D.; Bartuś, S. Acute myocardial infarction in young patients. Kardiol. Pol. 2021, 79, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Otten, A.M.; Maas, A.H.; Ottervanger, J.P.; Kloosterman, A.; van ‘t Hof, A.W.; Dambrink, J.H.; Gosselink, A.T.; Hoorntje, J.C.; Suryapranata, H.; de Boer, M.J. Is the difference in outcome between men and women treated by primary percutaneous coronary intervention age dependent? Gender difference in STEMI stratified on age. Eur. Heart J. Acute Cardiovasc. Care 2013, 2, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.J.; Feld, J.; Makowski, L.; Engelbertz, C.; Kühnemund, L.; Günster, C.; Dröge, P.; Ruhnke, T.; Gerß, J.; Freisinger, E.; et al. ST-Elevation Myocardial Infarction as a First Event. Dtsch. Arztebl. Int. 2022, 119, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Kuehnemund, L.; Koeppe, J.; Feld, J.; Wiederhold, A.; Illner, J.; Makowski, L.; Gerß, J.; Reinecke, H.; Freisinger, E. Gender differences in acute myocardial infarction—A nationwide German real-life analysis from 2014 to 2017. Clin. Cardiol. 2021, 44, 890–898. [Google Scholar] [CrossRef] [PubMed]
- Kuehnemund, L.; Lange, S.A.; Feld, J.; Padberg, J.S.; Fischer, A.J.; Makowski, L.; Engelbertz, C.; Dröge, P.; Ruhnke, T.; Guenster, C.; et al. Sex disparities in guideline-recommended therapies and outcomes after ST-elevation myocardial infarction in a contemporary nationwide cohort of patients over an eight-year period. Atherosclerosis 2023, 375, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, H.R.; Srichai, M.B.; Iqbal, S.N.; Slater, J.N.; Mancini, G.B.; Feit, F.; Pena-Sing, I.; Axel, L.; Attubato, M.J.; Yatskar, L.; et al. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation 2011, 124, 1414–1425. [Google Scholar] [CrossRef] [PubMed]
- Yahagi, K.; Davis, H.R.; Arbustini, E.; Virmani, R. Sex differences in coronary artery disease: Pathological observations. Atherosclerosis 2015, 239, 260–267. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Bugiardini, R.; Cenko, E.; Ricci, B.; Vasiljevic, Z.; Dorobantu, M.; Kedev, S.; Vavlukis, M.; Kalpak, O.; Puddu, P.E.; Gustiene, O.; et al. Comparison of Early Versus Delayed Oral β Blockers in Acute Coronary Syndromes and Effect on Outcomes. Am. J. Cardiol. 2016, 117, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G.G.; Olsson, A.G.; Ezekowitz, M.D.; Ganz, P.; Oliver, M.F.; Waters, D.; Zeiher, A.; Chaitman, B.R.; Leslie, S.; Stern, T. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial. JAMA 2001, 285, 1711–1718. [Google Scholar] [CrossRef]
- Indications for ACE inhibitors in the early treatment of acute myocardial infarction: Systematic overview of individual data from 100,000 patients in randomized trials. ACE Inhibitor Myocardial Infarction Collaborative Group. Circulation 1998, 97, 2202–2212. [CrossRef] [PubMed]
- Kannel, W.B.; Dawber, T.R.; Kagan, A.; Revotskie, N.; Stokes, J. 3rd. Factors of risk in the development of coronary heart disease--six year follow-up experience. The Framingham Study. Ann. Intern. Med. 1961, 55, 33–50. [Google Scholar] [CrossRef] [PubMed]
- Boyer, N.M.; Laskey, W.K.; Cox, M.; Hernandez, A.F.; Peterson, E.D.; Bhatt, D.L.; Cannon, C.P.; Fonarow, G.C. Trends in clinical, demographic, and biochemical characteristics of patients with acute myocardial infarction from 2003 to 2008: A report from the american heart association get with the guidelines coronary artery disease program. J. Am. Heart Assoc. 2012, 1, e001206. [Google Scholar] [CrossRef] [PubMed]
- Rahhal, A.; Mahfouz, A.; Khir, F.; Okleh, N.; Aljundi, A.H.; AlKhalaila, O.; Hamid, Y.; Al-Amri, M.; Al-Yafei, S.A.; Al Suwaidi, J.; et al. Medications adherence post-primary percutaneous coronary intervention in acute myocardial infarction: A population-based cohort study. J. Clin. Pharm. Ther. 2021, 46, 772–779. [Google Scholar] [CrossRef]
- Schwalm, J.D.; Ivers, N.M.; Natarajan, M.K.; Taljaard, M.; Rao-Melacini, P.; Witteman, H.O.; Zwarenstein, M.; Grimshaw, J.M. Cluster randomized controlled trial of Delayed Educational Reminders for Long-term Medication Adherence in ST-Elevation Myocardial Infarction (DERLA-STEMI). Am. Heart J. 2015, 170, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Faridi, K.F.; Peterson, E.D.; McCoy, L.A.; Thomas, L.; Enriquez, J.; Wang, T.Y. Timing of First Postdischarge Follow-up and Medication Adherence After Acute Myocardial Infarction. JAMA Cardiol. 2016, 1, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Castellano, J.M.; Sanz, G.; Peñalvo, J.L.; Bansilal, S.; Fernández-Ortiz, A.; Alvarez, L.; Guzmán, L.; Linares, J.C.; García, F.; D’Aniello, F.; et al. A polypill strategy to improve adherence: Results from the FOCUS project. J. Am. Coll. Cardiol. 2014, 64, 2071–2082. [Google Scholar] [CrossRef]
- Tung, B.W.; Ng, Z.Y.; Kristanto, W.; Saw, K.W.; Chan, S.P.; Sia, W.; Chan, K.H.; Chan, M.; Kong, W.; Lee, R.; et al. Characteristics and outcomes of young patients with ST segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: Retrospective analysis in a multiethnic Asian population. Open Heart 2021, 8, e001437. [Google Scholar] [CrossRef]
- Schmidt, M.; Szépligeti, S.; Horváth-Puhó, E.; Pedersen, L.; Bøtker, H.E.; Sørensen, H.T. Long-Term Survival Among Patients With Myocardial Infarction Before Age 50 Compared With the General Population. Circ. Cardiovasc. Qual. Outcomes 2016, 9, 523–531. [Google Scholar] [CrossRef]
- Champney, K.P.; Frederick, P.D.; Bueno, H.; Parashar, S.; Foody, J.; Merz, C.N.; Canto, J.G.; Lichtman, J.H.; Vaccarino, V. The joint contribution of sex, age and type of myocardial infarction on hospital mortality following acute myocardial infarction. Heart 2009, 95, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Vaccarino, V.; Parsons, L.; Every, N.R.; Barron, H.V.; Krumholz, H.M. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N. Engl. J. Med. 1999, 341, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.H.; Eurich, D.T.; Majumdar, S.R.; Padwal, R.S.; Tsuyuki, R.T.; Varney, J.; Johnson, J.A. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006, 333, 15. [Google Scholar] [CrossRef] [PubMed]
- Bramlage, P.; Messer, C.; Bitterlich, N.; Pohlmann, C.; Cuneo, A.; Stammwitz, E.; Tebbenjohanns, J.; Gohlke, H.; Senges, J.; Tebbe, U. The effect of optimal medical therapy on 1-year mortality after acute myocardial infarction. Heart 2010, 96, 604–609. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Larsen, A.I.; Tomey, M.I.; Mehran, R.; Nilsen, D.W.; Kirtane, A.J.; Witzenbichler, B.; Guagliumi, G.; Brener, S.J.; Généreux, P.; Kornowski, R.; et al. Comparison of outcomes in patients with ST-segment elevation myocardial infarction discharged on versus not on statin therapy (from the Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction Trial). Am. J. Cardiol. 2014, 113, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Angeli, F.; Ricci, F.; Moscucci, F.; Sciomer, S.; Bucciarelli, V.; Bianco, F.; Mattioli, A.V.; Pizzi, C.; Gallina, S. Sex- and gender-related disparities in chest pain syndromes: The feminine mystique of chest pain. Curr. Probl. Cardiol. 2024, 49, 102457. [Google Scholar] [CrossRef]
- Senst, B.L.; Achusim, L.E.; Genest, R.P.; Cosentino, L.A.; Ford, C.C.; Little, J.A.; Raybon, S.J.; Bates, D.W. Practical approach to determining costs and frequency of adverse drug events in a health care network. Am. J. Health Syst. Pharm. 2001, 58, 1126–1132. [Google Scholar] [CrossRef]
- Naderi, S.H.; Bestwick, J.P.; Wald, D.S. Adherence to drugs that prevent cardiovascular disease: Meta-analysis on 376,162 patients. Am. J. Med. 2012, 125, 882–887.e1. [Google Scholar] [CrossRef]
- Freisinger, E.; Koeppe, J.; Gerss, J.; Goerlich, D.; Malyar, N.M.; Marschall, U.; Faldum, A.; Reinecke, H. Mortality after use of paclitaxel-based devices in peripheral arteries: A real-world safety analysis. Eur. Heart J. 2020, 41, 3732–3739. [Google Scholar] [CrossRef]



| (A) | Age < 45 Years | ||
|---|---|---|---|
| All | Women | Men | |
| Patients—n (%) | 7927 | 1635 (20.6) | 6292 (79.4) |
| Median age—years (IQR) | 41 (38, 43) | 41 (37, 43) | 41 (38, 43) |
| Number of involved coronary vessels—n (%) | |||
| Unknown | 769 (9.7) | 189 (11.6) | 580 (9.2) |
| 1 | 4295 (54.2) | 1023 (62.6) | 3272 (52.0) |
| 2 | 1696 (21.4) | 270 (16.5) | 1426 (22.7) |
| 3 | 1167 (14.7) | 153 (9.4) | 1014 (16.1) |
| Arterial hypertension—n (%) | 4759 (60.0) | 981 (60.0) | 3777 (60.0) |
| Atrial fibrillation and/or flutter—n (%) | 247 (3.1) | 51 (3.1) | 196 (3.1) |
| Cancer—n (%) | 219 (2.8) | 62 (3.8) | 157 (2.5) |
| Cerebrovascular disease—n (%) | 95 (1.2) | 24 (1.5) | 71 (1.1) |
| CHF, all—n (%) | 2134 (26.9) | 460 (28.1) | 1674 (26.6) |
| Chronic kidney disease—n (%) | 406 (5.1) | 108 (6.6) | 298 (4.7) |
| Coronary artery disease—n (%) | 2406 (30.4) | 517 (31.6) | 1899 (30.2) |
| Diabetes mellitus, unspecified—n (%) | 1266 (16.0) | 347 (21.2) | 919 (14.6) |
| Dialysis | 32 (0.4) | 13 (0.8) | 19 (0.3) |
| Dyslipidemia—n (%) | 5172 (65.2) | 980 (59.9) | 4192 (66.6) |
| Ischemic cerebral insult—n (%) | 100 (1.3) | 33 (2.0) | 67 (1.1) |
| Left ventricular congestive heart failure (CHF)—n (%) | |||
| No CHF | 5980 (79.4) | 1208 (73.9) | 4772 (75.8) |
| NYHA I | 286 (3.6) | 48 (2.9) | 238 (3.8) |
| NYHA II | 631 (8.0) | 150 (9.2) | 481 (7.6) |
| NYHA III | 519 (6.5) | 105 (6.4) | 414 (6.6) |
| NYHA IV | 511 (6.4) | 124 (7.6) | 387 (6.2) |
| Nicotine abuse—n (%) | 3729 (47.8) | 757 (46.3) | 2972 (47.2) |
| Obesity—n (%) | 2138 (27.0) | 627 (38.4) | 1511 (24.0) |
| Peripheral artery disease (PAD)—n (%) | |||
| No PAD | 7825 (98.7) | 1607 (98.3) | 6218 (98.8) |
| PAD 1–3 | 69 (0.9) | 12 (0.7) | 57 (0.9) |
| PAD 4–6 | 33 (0.4) | 16 (1.0) | 17 (0.3) |
| Previous acute myocardial infarction—n (%) | 460 (5.8) | 90 (5.5) | 370 (5.9) |
| Previous coronary artery bypass graft—n (%) | *** | *** | |
| Previous percutaneous coronary intervention—n (%) | 129 (1.6) | 22 (1.4) | 107 (1.7) |
| Previous valve implantation—n (%) | *** | *** | |
| Right ventricular heart failure—n (%) | 166 (2.1) | 41 (2.5) | 125 (2.0) |
| ACE- inhibitors/ Angiotensin II receptor blockers—n (%) | 1326 (16.7) | 300 (18.4) | 1026 (16.3) |
| Beta blockers—n (%) | 970 (12.2) | 258 (15.8) | 712 (11.3) |
| OAC and/or PAI—n (%) | 446 (5.6) | 86 (5.3) | 360 (5.7) |
| Oral anticoagulants (OAC)—n (%) | 85 (1.1) | 29 (1.8) | 56 (0.9) |
| Platelet activation inhibitor (PAI)—n (%) | 368 (4.6) | 58 (3.6) | 310 (4.9) |
| Statins—n (%) | 600 (7.6) | 113 (6.9) | 487 (7.7) |
| All drugs—n (%) | 159 (2.0) | 27 (1.7) | 132 (2.1) |
| (B) | Total—Age < 60 Years | ||
| All | Women | Men | |
| Patients—n (%) | 59,401 | 11,453 (19.3) | 47,948 (80.7) |
| Median age—years (IQR) | 52 (48, 56) | 53 (48, 56) | 52 (48, 56) |
| Number of involved coronary vessels—n (%) | |||
| Unknown | 4524 (7.6) | 1098 (9.6) | 3426 (7.2) |
| 1 | 23,246 (39.1) | 5327 (46.5) | 17,919 (37.4) |
| 2 | 16,271 (27.4) | 2795 (24.4) | 13,476 (28.1) |
| 3 | 15,360 (25.9) | 2233 (19.5) | 13,127 (27.4) |
| Arterial hypertension—n (%) | 43,474 (73.2) | 8703 (76.0) | 34,771 (72.5) |
| Atrial fibrillation and/or flutter—n (%) | 3585 (6.0) | 645 (5.6) | 2940 (6.1) |
| Cancer—n (%) | 3282 (5.5) | 929 (8.1) | 2353 (4.9) |
| Cerebrovascular disease—n (%) | 2063 (3.5) | 442 (3.9) | 1611 (3.4) |
| CHF, all—n (%) | 19,057 (32.1) | 3679 (32.1) | 15,378 (32.1) |
| Chronic kidney disease—n (%) | 4776 (8.0) | 1049 (9.2) | 3727 (7.8) |
| Coronary artery disease—n (%) | 22,737 (38.3) | 4531 (39.6) | 18,206 (38.0) |
| Diabetes mellitus, unspecified—n (%) | 14,255 (24.0) | 3086 (26.9) | 11,169 (23.3) |
| Dialysis | 201 (0.3) | 56 (0.5) | 145 (0.3) |
| Dyslipidemia—n (%) | 42,413 (71.4) | 7992 (69.8) | 34,421 (71.8) |
| Ischemic cerebral insult—n (%) | 1891 (3.2) | 420 (3.7) | 1471 (3.1) |
| Left ventricular congestive heart failure (CHF)—n (%) | |||
| No CHF | 42,310 (71.2) | 8148 (71.1) | 34,162 (71.3) |
| NYHA I | 2157 (3.6) | 356 (3.1) | 1801 (3.8) |
| NYHA II | 5038 (8.5) | 959 (8.4) | 4079 (8.5) |
| NYHA III | 4706 (7.9) | 881 (7.7) | 3825 (8.0) |
| NYHA IV | 5190 (8.7) | 1109 (9.7) | 4081 (8.5) |
| Nicotine abuse—n (%) | 26,584 (44.8) | 5264 (46.0) | 21,320 (44.6) |
| Obesity—n (%) | 15,250 (25.7) | 3963 (34.6) | 11,287 (23.5) |
| Peripheral artery disease (PAD)—n (%) | |||
| No PAD | 56,841 (95.7) | 10,967 (95.8) | 45,874 (95.7) |
| PAD 1–3 | 1825 (3.1) | 328 (2.9) | 1497 (3.1) |
| PAD 4–6 | 735 (1.2) | 158 (1.4) | 577 (1.2) |
| Previous acute myocardial infarction—n (%) | 4449 (7.5) | 812 (7.1) | 3637 (7.6) |
| Previous coronary artery bypass graft—n (%) | 976 (1.6) | 132 (1.2) | 844 (1.8) |
| Previous percutaneous coronary intervention—n (%) | 1432 (2.4) | 203 (1.8) | 1229 (2.6) |
| Previous valve implantation—n (%) | 105 (0.2) | 23 (0.2) | 82 (0.2) |
| Right ventricular heart failure—n (%) | 1964 (3.3) | 396 (3.5) | 1568 (3.3) |
| Medication at Admission—n (%) | |||
| ACE- inhibitors/ Angiotensin II receptor blockers—n (%) | 16,738 (28.1) | 3574 (31.2) | 13,144 (27.4) |
| Beta blockers—n (%) | 12,327 (20.8) | 3024 (26.4) | 9303 (19.4) |
| OAC and/or PAI—n (%) | 5608 (9.4) | 946 (8.3) | 4662 (9.7) |
| Oral anticoagulants (OAC)—n (%) | 795 (1.3) | 168 (1.5) | 627 (1.3) |
| Platelet activation inhibitor (PAI)—n (%) | 4937 (8.3) | 805 (7.0) | 4132 (8.6) |
| Statins—n (%) | 8174 (13.8) | 1462 (12.8) | 6712 (14.0) |
| All drugs—n (%) | 2196 (3.7) | 312 (2.7) | 1884 (3.9) |
| Age < 45 Years | Total—Age < 60 Years | |||||
|---|---|---|---|---|---|---|
| All | Women | Men | All | Women | Men | |
| Mean length of hospital stay, years (±SD) | 9.8 (±13.3) | 11.1 (±17.3) | 9.4 (±12.1) | 10.2 (±13.2) | 10.4 (±13.1) | 10.2 (±13.2) |
| Mean costs, Euro (±SD) | 8470.20 (±16,969) | 9512.12 (±20,707) | 8199.45 (±15,845) | 9120.30 (±17,630) | 8978.14 (±16,931) | 9154.25 (±17,793) |
| Acute kidney failure and/or renal replacement therapy, n (%) | 241 (3.0) | 66 (4.0) | 175 (2.8) | 2475 (4.2) | 494 (4.3) | 1981 (4.1) |
| Acute kidney failure, n (%) | 201 (2.5) | 57 (3.5) | 144 (2.3) | 2083 (3.5) | 406 (3.5) | 1677 (3.5) |
| Bare metal stent only, n (%) | 1178 (14.9) | 221 (13.5) | 957 (15.2) | 8954 (15.1) | 1562 (13.6) | 7392 (15.4) |
| Bleeding, n (%) | 441 (5.6) | 107 (6.5) | 334 (5.3) | 3487 (5.9) | 910 (8.0) | 2577 (5.4) |
| Blood transfusion and/or bleeding, n (%) | 702 (8.9) | 209 (12.8) | 493 (7.8) | 6085 (10.5) | 1618 (14.1) | 4467 (9.3) |
| Blood transfusion, n (%) | 362 (4.6) | 137 (8.4) | 225 (3.6) | 3491 (5.9) | 982 (8.6) | 2509 (5.2) |
| Circulatory support device (Impella), n (%) | 37 (0.5) | 10 (0.6) | 27 (0.4) | 271 (0.5) | 52 (0.5) | 219 (0.5) |
| Coronary angiography, n (%) | 7588 (95.7) | 1555 (95.1) | 6033 (95.9) | 56,272 (95.2) | 10,876 (95.0) | 45,696 (95.3) |
| Coronary artery bypass grafting, n (%) | 168 (2.1) | 27 (1.7) | 141 (2.2) | 2192 (3.8) | 320 (2.8) | 1872 (3.9) |
| Drug eluting stent, n (%) | 5605 (70.7) | 1108 (67.8) | 4497 (71.5) | 42,625 (71.8) | 8138 (71.1) | 34,487 (71.9) |
| Extracorporeal membrane oxygenation, n (%) | 95 (1.2) | 20 (1.2) | 75 (1.2) | 760 (1.3) | 159 (1.4) | 601 (1.3) |
| GpIIb/IIIa-inhibitor, n (%) | 2311 (29.2) | 477 (29.2) | 1834 (29.2) | 16,374 (27.6) | 2920 (25.5) | 13,454 (28.1) |
| Hemorrhagic stroke, n (%) | *** | *** | *** | 144 (0.2) | 36 (0.3) | 89 (0.2) |
| Impella and/or intra-aortic balloon pump and/or extracorporeal membrane oxygenation or shock, n (%) | 725 (9.1) | 193 (11.8) | 532 (8.5) | 6423 (10.8) | 1354 (11.8) | 5069 (10.6) |
| In-hospital resuscitation, n (%) | 591 (7.5) | 161 (9.9) | 430 (6.8) | 4840 (8.1) | 1063 (9.3) | 3777 (7.9) |
| Intervention and/or thrombolysis, n (%) | 7689 (97.0) | 1583 (96.8) | 6106 (97.0) | 57,330 (96.5) | 11,038 (96.4) | 46,292 (96.6) |
| Intra-aortic balloon pump, n (%) | 168 (2.1) | 50 (3.1) | 118 (1.9) | 1475 (2.5) | 291 (2.5) | 1184 (2.5) |
| Percutaneous coronary intervention, n (%) | 7216 (91.0) | 1454 (88.9) | 5762 (91.6) | 54,253 (91.3) | 10,282 (89.8) | 43,971 (91.7) |
| Renal replacement therapy, n (%) | 144 (1.8) | 34 (2.1) | 110 (1.8) | 1312 (2.2) | 257 (2.2) | 1055 (2.2) |
| Sepsis, n (%) | 111 (1.4) | 30 (1.8) | 81 (1.3) | 1090 (1.8) | 208 (1.8) | 882 (1.8) |
| Shock, n (%) | 663 (8.4) | 175 (10.7) | 488 (7.8) | 5801 (9.8) | 1230 (10.7) | 4571 (9.5) |
| Stroke, n (%) | 53 (0.7) | 13 (0.8) | 40 (0.6) | 508 (0.2) | 122 (1.1) | 386 (0.8) |
| Thrombolysis, n (%) | 145 (1.8) | 35 (2.1) | 110 (1.8) | 904 (1.5) | 195 (1.7) | 709 (1.5) |
| Ventilation, n (%) | 989 (12.5) | 255 (15.6) | 734 (11.7) | 8564 (14.4) | 1778 (15.5) | 6786 (14.2) |
| Median duration—h (IQR) | 77 (198) | 69 (226) | 81.5 (193) | 72 (195) | 57 (180) | 76 (197) |
| In-hospital death, n (%) | 336 (4.2) | 101 (6.2) | 235 (3.7) | 3588 (6.0) | 829 (7.2) | 2759 (5.8) |
| 30 days mortality, n (%) | 331 (4.2) | 94 (5.8) | 237 (3.8) | 3591 (6.0) | 823 (7.2) | 2768 (5.8) |
| 90 days mortality, n (%) | 357 (4.5) | 103 (6.4) | 254 (4.1) | 3950 (6.6) | 898 (7.9) | 3052 (6.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fischer, A.J.; Feld, J.; Lange, S.A.; Günster, C.; Dröge, P.; Engelbertz, C.; Ruhnke, T.; Gerß, J.; Reinecke, H.; Köppe, J. Impact of Guideline-Directed Drug Therapy after ST-Elevation Myocardial Infarction on Outcome in Young Patients—Age and Sex-Specific Factors. J. Clin. Med. 2024, 13, 3788. https://doi.org/10.3390/jcm13133788
Fischer AJ, Feld J, Lange SA, Günster C, Dröge P, Engelbertz C, Ruhnke T, Gerß J, Reinecke H, Köppe J. Impact of Guideline-Directed Drug Therapy after ST-Elevation Myocardial Infarction on Outcome in Young Patients—Age and Sex-Specific Factors. Journal of Clinical Medicine. 2024; 13(13):3788. https://doi.org/10.3390/jcm13133788
Chicago/Turabian StyleFischer, Alicia Jeanette, Jannik Feld, Stefan A. Lange, Christian Günster, Patrik Dröge, Christiane Engelbertz, Thomas Ruhnke, Joachim Gerß, Holger Reinecke, and Jeanette Köppe. 2024. "Impact of Guideline-Directed Drug Therapy after ST-Elevation Myocardial Infarction on Outcome in Young Patients—Age and Sex-Specific Factors" Journal of Clinical Medicine 13, no. 13: 3788. https://doi.org/10.3390/jcm13133788
APA StyleFischer, A. J., Feld, J., Lange, S. A., Günster, C., Dröge, P., Engelbertz, C., Ruhnke, T., Gerß, J., Reinecke, H., & Köppe, J. (2024). Impact of Guideline-Directed Drug Therapy after ST-Elevation Myocardial Infarction on Outcome in Young Patients—Age and Sex-Specific Factors. Journal of Clinical Medicine, 13(13), 3788. https://doi.org/10.3390/jcm13133788





