Return to Sports and Activities after Arthroscopic Treatments for Rotator Cuff Lesions in Young Patients Less Than 45-Years-Old: A Systematic Review
Abstract
:1. Introduction
2. Material and Methods
2.1. Eligibility Criteria
2.2. Outcome Measures
2.3. Search Strategy
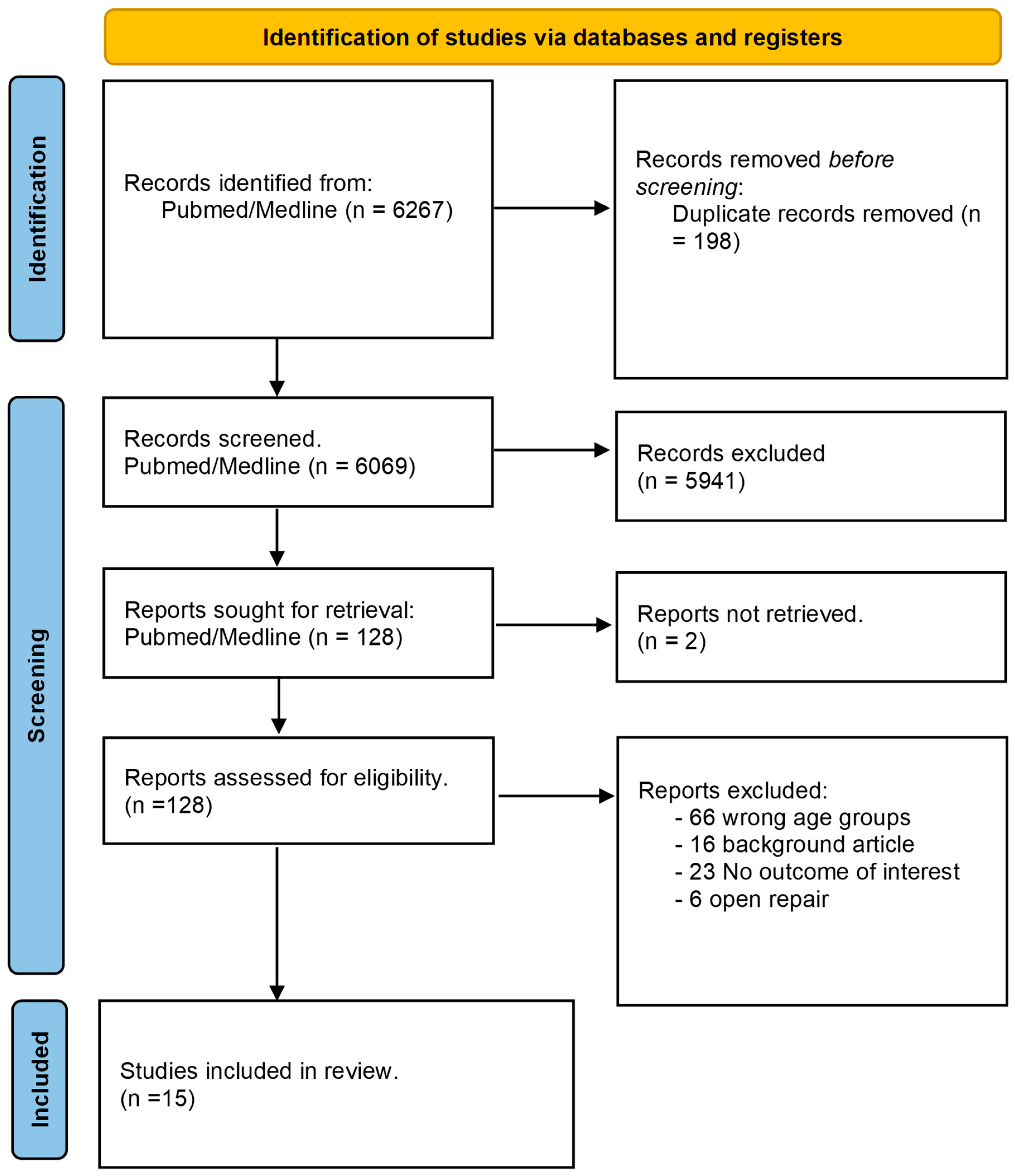
2.4. Study Selection
2.5. Data Extraction
2.6. Evaluation of the Quality of the Included Studies
2.7. Data Synthesis
3. Results
3.1. Included Studies
3.2. Study Characteristics and Quality (Table 1)
3.3. Patient Characteristics (Table 1)
3.4. Return to Sport (Table 2)
| Study | N | Loss to Follow-Up or Excluded | Type of Sport | Level of Sport | Rate of Return to Sport | Rate of Return to Same or Higher Level | Time to Return to Unrestricted Sport (months) | Time of Authorization of Return to Unrestricted Work as per Study Protocol |
|---|---|---|---|---|---|---|---|---|
| 2008, Krishnan et al. [12] | 23 | 0 | Worker compensation: 20. Professional athletes: 3 | Professional vs recreational | 23/23 (100%) | 21/23 (90%) | NR | Resistance exercises began at week 10. Activity progression was allowed as tolerated following this and full release to all activity and work (including sports) was allowed 6 months after surgery. |
| 2008, Reynolds et al. [13] | 82 | 15 | Professional elite overhead throwing athletes (Baseball pitchers) | Professional | 51/67 (76.1%) | 37/67 (55.2%) | 5.6 (SD = 2.6) | Early pain and inflammatory control phase, protection phase, gradual return of range of motion, strengthening, and gradual return to competition. |
| 2009, Tambe et al. [14] | 11 | 0 | Professional elite rugby players | Professional | 10/11 (90.9%) | 10/11 (90.9%) | 5.75 (SD = 2.42, range 3–11) | Accelerated rehabilitation program. Depending on the athletes’ progress, resistance exercises are introduced after approximately six weeks, along with skills training. Simulated tackling is started at about two to three months. Impact and tackle bag training is not started until the athletes have achieved satisfactory movement, strength, isokinetic and proprioceptive criteria. |
| 2012, Van Kleumen et al. [15] | 17 | 0 | Baseball, overhead-throwing sports | Interscholastic, Intercollegiate | 8/17 (47%) | 6/17 (35.2%) | NR | NR |
| 2013, Eisner et al. [16] | 30 | 17 | Adolescent overhead athletes | NR | 9/13 (69.2%) | 9/13 (69.2%) | NR | 6-week course of physical therapy, which consisted of rotator cuff stretching and strengthening, and scapular stabilizing exercises under the direction of licensed physical therapists before being offered surgical treatment. |
| 2018, Azzam et al. [17] | 32 | 5 | Athletes: Football, baseball, basketball, softball, wrestling, motocross, track, volleyball, bull riding, cross country, mixed martial arts | Athletes, NR otherwise | 25/27 (93%) | 17/27 (62.9%) | NR | Progression to sport-specific exercises began at 5 to 6 months, once the patient had obtained full motion and full strength. The patient was released to full activities when he or she had completed a sport-specific rehabilitation progression or interval training program, depending on the sport involved. |
| 2018, Merola et al. [18] | 38 | 0 | Professional overhead athletes. | Professional | 33/38 (87%) | 19/38 (50%) | 6 (SD = 0.7) months | Wearing a sling for the first 3 weeks, passive mobilization and active-assisted exercises in a pool in the pain-free range of motion (ROM) up to the 6th week, and thereafter active exercises with and without resistance. |
| 2018, Parness et al. [19] | 42 | 0 | Military | Recreational and military job athletes | 40/42 (95.2%) | 40/42 (95.2%) | 6 (SD = 0.7) months. | Return to full military job activity and contact sports was allowed 6 months after surgery. |
| 2018, Rossi et al. [20] | 70 * | 0 | NR for subgroup analysis | NR for subgroup analysis | NR for subgroup analysis | NR for subgroup analysis | 5.2 (SD = 2) months | Return to competition was allowed when the patient was pain free, full-shoulder ROM had been achieved, and shoulder strength was near the same as before the injury |
| 2019, Erickson et al. [21]—Debridement | 130 | 0 | Baseball (Major league) | Professional | Debridement: 75/130 (57.6%) | Debridement: 55/130 (42.3%), | NR | NR |
| 2019, Erickson et al. [21]—Repair (same study | 21 | 0 | Baseball (Major league) | Professional | Repair: 7/21 (33.3%) | Repair: 3/19 (14.3%) | NR | NR |
| 2021, Castagna et al. [23] | 3 | 0 | Professional soccer goalkeepers | Professional | 3/3 (100%) | 3/3 (100%) (Objective metrics: 96.7% ± 5.8) | 4.76 (SD = 0.97 months. (reported as 20.7 ± 4.2 weeks) | NR |
| 2021, Davey et al. [24] | 20 | 0 | 2 professional athletes(10.0%) 16 competitive athletes (80.0%) 2 recreational athletes (10.0%); there were 15 collision athletes (75.0%) | Professional athlete 10%. Competitive athlete 80%. Recreational athlete 10% | 17/20 (85%) for all 16/18 (88.9%) for professional and competitive | 10/20 (50%) | 5.8 (SD = 2.8) | A controlled return to contact in training was allowed after 12 weeks if comfortable, whereas a return to full contact and competition usually followed within the next 3 months. |
| 2022, Scanaliato et al. [25] | 42 | 5 | Military | military patients | 37/37 (100%) | NR | NR | Return to unrestricted active duty and contact sports were permitted 6 months postoperatively. |
3.5. Return to Work (Table 3)
| Study | N | Type of Work | Rate Of Return To Work | Time to Return to Work | Time of Authorization of Return to Unrestricted Work as by Study Protocol | Follow-Up (months) |
|---|---|---|---|---|---|---|
| 2008, Krishnan et al. [12] | 23 | Worker compensation: 20. Professional athletes: 3 | 21/23 (91.3%) | NR | 6 months | 26 (SD = NR, 24 to 29) |
| 2013, Lin et al. [7] | 53 | Work related: 23 | 47/53 (88.6%) | NR | 6 months | 37.8 (SD = 10.2, range 13.8 to 59.1) |
| 2018, Parness et al. [19] | 42 | Military | 40/42 (95.2%) | NR | 6 months | 41 (SD = NR, 24 to 66) |
| 2022, Scanaliato et al. [25] | 42 | Military | 37/42 (88.1%) | NR | 6 months | 104.51 (SD = 7.67, NR) |
| Total | 160 | Military: 84 Worker compensation: 20 Athletes: 3 | 145/160 (90.6%) | NR | 6 months |
3.6. Functional Scores
3.7. ASES Score (Table 4)
| Study | N | Pre Operative ASES | Post Operative ASES | p-Value |
|---|---|---|---|---|
| 2008, Krishnan et al. [12] | 23 | 42 (SD = NR, range 22 to 60). | 92 (SD = NR, range, 65 to 100) | <0.01 |
| 2013, Lin et al. [7] | 53 | NR | 84.6 (SD = 16.8, range, 21.6 to 100.0) | N/A |
| 2018, Azzam et al. [17] | 32 | NR | 93 (SD= 16.8, range, 21.6 to 100.0) | N/A |
| 2018, Parness et al. [19] | 42 | 38.97 (SD = 12.70) | 89.8 (SD = 14.26) | <0.01 |
| 2018, Rossi et al. [20] | Subgroup analysis n not available (N = 70 *) | 43.3 (SD = 1) | 88.4 (SD = 2) | NR |
| 2020, Kaptan et al. [22] | 151 | Partial + Full thickness: 23.8, (SD = NR, range, 8.3 to 36.6), Full thickness: 23.4 (SD = NR, range, 8.3 to 36.6) | Partial + Full thickness: 72.2 (SD = NR, range, 11.6 to 88.3) Full thickness: 72.3 (SD = NR, range, 11.6 to 88.3) | <0.01 |
| 2021, Davey et al. [24] | 20 | NR | 92.4 (SD = 4.6, range 83.3–100) | N/A |
| 2022, Scanaliato et al. [25] | 37 | 41.00 (SD = NR, range, 34.74 to 47.26) | Midterm: 90.84 (SD = NR, range, 85.78 to 95.90) Final follow up: 88.68 (SD = NR, range 82.69 to 94.66) | <0.001 |
| * Subgroup analysis available |
3.8. SANE Score (Table 5)
| SANE Score | N | Preoperative | Post Operative | p-Value |
|---|---|---|---|---|
| 2013, Eisner et al. [16] | 30 | NR | 80.6 (SD = 17.1) | N/A |
| 2013, Lin et al. [7] | 53 | NR | 80.8 (SD = 20, range, 10 to 100) | N/A |
| 2022, Scanaliato et al. [25] | 37 | 48.24 (SD = NR, range, 39.52 to 56.96) | Mid-term: 89.19 (SD = NR, range,82.81 to 95.57) Final follow up: 87.32 (SD = NR, range, 80.72 to 93.93) | <0.001 |
3.9. VAS Score (Table 6)
| VAS | N | Preoperative | Post Operative (Final Follow-Up) | p-Value |
|---|---|---|---|---|
| 2013, Lin et al. [7] | 53 | NR | 1.2 (SD = 2, range 0 to 10) | N/A |
| 2018, Parness et al. [19] | 42 | 8.09 (SD = 1.51) | 1.19 (SD = 1.85) | <0.01 |
| 2018, Rossi et al. [20] | 70 * | NR | 1.1 (SD = 2) | N/A |
| 2020, Kaptan et al. [22] | 50 | Partial + full thickness: 7.9 (SD = NR, range 5 to 10) Full thickness: 8.4 (SD = NR, range 6 to 10) | Partial + full thickness: 3.1 (SD = NR, range 1 to 10) Full thickness: 2.3 (SD = NR, range 1 to 4) | <0.01 <0.01 |
| 2021, Davey et al. [24] | 20 | NR | 0.7 (SD = NR, range 0 to 3) | N/A |
| 2022, Scanaliato et al. [25] | 37 | 8.03 (SD = NR, range 7.29 to 8.77) | Mid term: 1.14 (SD = NR, range, 0.43 to 1.85) Final follow up: 1.16 (SD = NR, range, 0.44 to 1.88) | <0.0001 <0.0001 |
3.10. Constant Score
3.11. SSV Score
3.12. KJOC Shoulder and Elbow Score
3.13. UCLA Score
3.14. WORC Score
3.15. Oxford Score
3.16. SST Score
3.17. QuickDash, Quickdash Sport
3.18. ASORS, SF-12, PSF, MSF
4. Discussion
5. RTS
6. Return to Work
7. Functional Scores
8. Limitation
9. Conclusions
Funding
Conflicts of Interest
Abbreviations
| RCT | Rotator cuff tear |
| RTS | Return to sport |
| PROMs | Patient-reported outcome measures |
| ASES | American Shoulder and Elbow Surgeons score |
| SANE | Single Assessment Numeric Evaluation score |
| VAS | Visual Analog Scale |
| Constant score | Constant–Murley Shoulder Outcome Score |
| SST | Simple Shoulder Test |
| WORC | Western Ontario Rotator Cuff Index |
| OSS | Oxford Shoulder Score |
| UCLA | University of California at Los Angeles Shoulder Rating Scale |
| DASH | Disabilities of the Arm, Shoulder, and Hand score |
| QuickDASH | Sports-specific module of the DASH score |
| ASORS | Athletic Shoulder Outcome Rating Scale |
| SF-12 | 12-Item Short Form Health Survey |
| PSF | Physical Component Summary |
| MSF | Mental Component Summary |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| MINORS | Methodological Index for Nonrandomized Studies |
| LOE | Level of evidence |
| SSV | Subjective Shoulder Value |
| SSP | Supraspinatus |
| ISP | Infraspinatus |
| SSC | Subscapularis |
| TM | Teres minor |
| SLAP | Superior labrum from anterior to posterior tear |
| KJOC | Kerlan–Jobe Orthopaedic Clinic Shoulder and Elbow score |
References
- Greenberg, D.L. Evaluation and Treatment of Shoulder Pain. Med. Clin. N. Am. 2014, 98, 487–504. [Google Scholar] [CrossRef] [PubMed]
- Sher, J.S.; Uribe, J.W.; Posada, A.; Murphy, B.J.; Zlatkin, M.B. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J. Bone Jt. Surg. 1995, 77, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Tashjian, R.Z. Epidemiology, Natural History, and Indications for Treatment of Rotator Cuff Tears. Clin. Sports Med. 2012, 31, 589–604. [Google Scholar] [CrossRef] [PubMed]
- Boileau, P. Arthroscopic Repair of Full-Thickness Tears of the Supraspinatus: Does the Tendon Really Heal? J. Bone Jt. Surg. Am. 2005, 87, 1229–1240. [Google Scholar] [CrossRef]
- Jensen, A.R.; Taylor, A.J.; Sanchez-Sotelo, J. Factors Influencing the Reparability and Healing Rates of Rotator Cuff Tears. Curr. Rev. Musculoskelet. Med. 2020, 13, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Lazarides, A.L.; Alentorn-Geli, E.; Choi, J.H.J.; Stuart, J.J.; Lo, I.K.Y.; Garrigues, G.E.; Taylor, D.C. Rotator cuff tears in young patients: A different disease than rotator cuff tears in elderly patients. J. Shoulder Elbow Surg. 2015, 24, 1834–1843. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.C.; Mall, N.A.; Dhawan, A.; Sherman, S.L.; McGill, K.C.; Provencher, M.T.; Nicholson, G.P.; Cole, B.J.; Solomon, D.J.; Verma, N.N.; et al. Arthroscopic Primary Rotator Cuff Repairs in Patients Aged Younger Than 45 Years. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Kelly, B.C.; Constantinescu, D.S.; Vap, A.R. Arthroscopic and Open or Mini-Open Rotator Cuff Repair Trends and Complication Rates Among American Board of Orthopaedic Surgeons Part II Examinees (2007–2017). Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 3019–3024. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument: Methodological index for non-randomized studies. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, S.G.; Harkins, D.C.; Schiffern, S.C.; Pennington, S.D.; Burkhead, W.Z. Arthroscopic Repair of Full-Thickness Tears of the Rotator Cuff in Patients Younger Than 40 Years. Arthrosc. J. Arthrosc. Relat. Surg. 2008, 24, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, S.B.; Dugas, J.R.; Cain, L.E.; McMichael, C.S.; Andrews, J.R. Débridement of Small Partial-thickness Rotator Cuff Tears in Elite Overhead Throwers. Clin. Orthop. 2008, 466, 614–621. [Google Scholar] [CrossRef]
- Tambe, A.; Badge, R.; Funk, L. Arthroscopic rotator cuff repair in elite rugby players. Int. J. Shoulder Surg. 2009, 3, 8. [Google Scholar] [CrossRef] [PubMed]
- Van Kleunen, J.P.; Tucker, S.A.; Field, L.D.; Savoie, F.H. Return to High-Level Throwing After Combination Infraspinatus Repair, SLAP Repair, and Release of Glenohumeral Internal Rotation Deficit. Am. J. Sports Med. 2012, 40, 2536–2541. [Google Scholar] [CrossRef] [PubMed]
- Eisner, E.A.; Roocroft, J.H.; Moor, M.A.; Edmonds, E.W. Partial Rotator Cuff Tears in Adolescents: Factors Affecting Outcomes. J. Pediatr. Orthop. 2013, 33, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Azzam, M.G.; Dugas, J.R.; Andrews, J.R.; Goldstein, S.R.; Emblom, B.A.; Cain, E.L. Rotator Cuff Repair in Adolescent Athletes. Am. J. Sports Med. 2018, 46, 1084–1090. [Google Scholar] [CrossRef] [PubMed]
- Merolla, G.; Paladini, P.; Porcellini, G. Assessment of return to play in professional overhead athletes subjected to arthroscopic repair of rotator cuff tears and associated labral injuries using the Italian version of the Kerlan-Jobe Orthopedic Clinic Shoulder and Elbow score. Musculoskelet. Surg. 2018, 102, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Parnes, N.; Bartoszewski, N.R.; Defranco, M.J. Arthroscopic Repair of Full-Thickness Rotator Cuff Tears in Active Patients Younger Than 40 Years: 2- to 5-Year Clinical Outcomes. Orthopedics 2018, 41, e52–e57. [Google Scholar] [CrossRef]
- Rossi, L.A.; Atala, N.; Bertona, A.; Tanoira, I.; Bongiovanni, S.; Maignon, G.; Ranalletta, M. Return to Sports After in Situ Arthroscopic Repair of Partial Rotator Cuff Tears. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 32–37. [Google Scholar] [CrossRef]
- Erickson, B.J.; Chalmers, P.N.; D’Angelo, J.; Ma, K.; Romeo, A.A. Performance and return to sport following rotator cuff surgery in professional baseball players. J. Shoulder Elbow Surg. 2019, 28, 2326–2333. [Google Scholar] [CrossRef] [PubMed]
- Kaptan, A.Y.; Ulucakoy, C.; Ozer, M.; Cetinkaya, M.; Ayanoglu, T.; Ataoğlu, M.B.; Kanatlı, U. Partial and full-thickness rotator cuff tears in patients younger than 45 years. Acta Orthop. Traumatol. Turc. 2020, 54, 478–482. [Google Scholar] [CrossRef] [PubMed]
- Castagna, A.; Ranieri, R.; Volpi, P.; Ceccarelli, E.; Garofalo, R.; Conti, M. Elite professional goalkeepers report high rate of sport resumption after shoulder surgery. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3943–3950. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.S.; Hurley, E.T.; Scanlon, J.P.; Gaafar, M.; Pauzenberger, L.; Mullett, H. Excellent Clinical Outcomes and Rates of Return to Play After Arthroscopic Rotator Cuff Repair for Traumatic Tears in Athletes Aged 30 Years or Less. Arthrosc. Sports Med. Rehabil. 2021, 3, e667–e672. [Google Scholar] [CrossRef] [PubMed]
- Scanaliato, J.P.; Eckhoff, M.D.; Dunn, J.C.; Czajkowski, H.; Fink, W.A.; Parnes, N. Long-term Results of Arthroscopic Repair of Full-Thickness Traumatic Rotator Cuff Tears in Active Duty Military Patients Under the Age of 40 Years. Am. J. Sports Med. 2022, 50, 2753–2760. [Google Scholar] [CrossRef]
- Migliorini, F.; Asparago, G.; Cuozzo, F.; Oliva, F.; Hildebrand, F.; Maffulli, N. Patient outcomes and return to play after arthroscopic rotator cuff repair in overhead athletes: A systematic review. J. Orthop. Traumatol. 2023, 24, 3. [Google Scholar] [CrossRef]
- Klouche, S.; Lefevre, N.; Herman, S.; Gerometta, A.; Bohu, Y. Return to Sport After Rotator Cuff Tear Repair: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2016, 44, 1877–1887. [Google Scholar] [CrossRef] [PubMed]
- Giberson-Chen, C.C.; Shaw, B.L.; Rudisill, S.S.; Carrier, R.E.; Farina, E.M.; Pearson, B.; Asnis, P.D.; O’Donnell, E.A. Return to Play After Shoulder Surgery in Professional Baseball Players: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2023, 11, 232596712211408. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.J.; Morin, W.D.; Bonutti, P.M. Surgical treatment of full-thickness rotator cuff tears in patients 40 years of age or younger. J. Shoulder Elbow Surg. 1999, 8, 259–265. [Google Scholar] [CrossRef]
- Mazoué, C.G.; Andrews, J.R. Repair of Full-Thickness Rotator Cuff Tears in Professional Baseball Players. Am. J. Sports Med. 2006, 34, 182–189. [Google Scholar] [CrossRef]
- Kholinne, E.; Singjie, L.C.; Marsetio, A.F.; Kwak, J.-M.; Jeon, I.-H. Return to physical activities after arthroscopic rotator cuff repair: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 2645–2654. [Google Scholar] [CrossRef] [PubMed]
- MacKechnie, M.A.K.; Chahal, J.; Wasserstein, D.; Theodoropoulos, J.S.; Henry, P.; Dwyer, T. Repair of Full-Thickness Rotator Cuff Tears in Patients Aged Younger Than 55 Years. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 1366–1371. [Google Scholar] [CrossRef] [PubMed]
- Altintas, B.; Anderson, N.L.; Pitta, R.; Buckley, P.S.; Bhatia, S.; Provencher, M.T.; Millett, P.J. Repair of Rotator Cuff Tears in the Elderly: Does It Make Sense? A Systematic Review. Am. J. Sports Med. 2020, 48, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.-C.; Kuo, L.-T.; Hsu, W.-H.; Tsai, Y.-H.; Peng, K.-T. Comparison of Outcomes after Arthroscopic Rotator Cuff Repair between Elderly and Younger Patient Groups: A Systematic Review and Meta-Analysis of Comparative Studies. Diagnostics 2023, 13, 1770. [Google Scholar] [CrossRef] [PubMed]
| Study | MINORS | Type of Study | LOE | Age: Mean (SD, Range) | Sex | n | Site (R/L or D/ND) | Tendon Involved | Partial versus Complete | Activity (Athletes, Worker) | Etiology | Mean Time before Surgery | Technique | Mean Follow Up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008, Krishnan et al. [12] | 10 | Case series | 4 | 37 (NR, 21–39) | M: 15, F: 8 | 23 | NR | SSP: 78%, SSP + ISP: 22% | Full thickness | Worker compensation: 20. Athletes: 3 | T: 22 (95%) | 6 (3–9) months | Double row repair | 26 (SD = NR, 24 to 29) |
| 2008, Reynolds et al. [13] | 6 | Retrospective study | 4 | 25.6 (5.5, NR) | M: 82 | 82 | 55 R, 27 L | SSP + ISP | Partial thickness | Elite overhead throwing athletes (Baseball pitchers) | Multifactorial related to overhead-throwing sports | <6-weeks: 6 >6-weeks: 76 | Debridement | 38 (SD = NR, 18 to 59) |
| 2009, Tambe et al. [14] | 8 | Retrospective study | 4 | 25.7 (NR, 19–31) | M: 11 | 11 | NR | SSP: 9 SSP + ISP: 1 SSP + SSC: 1 | Full thickness | Elite rugby players | T: 100% | 1.15 month | Simple or double row repair | 18 (SD = NR, 6 to 31) |
| 2012, Van Kleumen et al. [15] | 12 | Case series | 4 | 19.16 (NR, 16.08–22.92) | M: 17 | 17 | ISP + SLAP | Full thickness: 6, Partial thickness: 11 | Baseball, overhead-throwing sports | Multifactorial related to overhead-throwing sports | NR | Simple row or free PDS suture | 37.12 (SD = NR, 24 to 55) | |
| 2013, Eisner et al. [16] | 15 | Retrospective cohort | 3 | 15.5 (1.8, 8–18) | M: 16 F: 14 | 30 | R: 24 L: 6 | SSP | Partial thickness | Adolescent athletes | T: 30 (100%) | 5.8 month | Debridement or repair | 16.9 (SD = NR, 8 to 30) |
| 2013, Lin et al. [7] | 7 | Case series | 4 | 37.5 (16–45) | M: 40 D: 13 | 53 | D: 53% | All types | Full thickness | Work related: 23 (43%) | T: 32 (60%) | NR | 83% double-row suture, 17% single-row) | 37.8 (SD = 10.2, 13.8 to 59.1) |
| 2018, Azzam et al. [17] | 10 | Case series | 4 | 16.1 (1.3, 13.2–17.9) | M: 28 F: 4 | 32 | D: 26 ND: 6 | SSP: 21 SS: 6 SSP + ISP: 2 SSP+ SS: 1 ISP: 1 SSP + ISP + TM: 1 | Full thickness: 13 Partial thickness: 19 | Athletes: Football, baseball, basketball, softball, wrestling, motocross, track, volleyball, bull riding, cross country, mixed martial arts | T: 29 (90.6%) | NR | Simple or double row repair | 74.4 (SD = 31.2, 24–120) |
| 2018, Merola et al. [18] | 12 | Retrospective cohort | 3 | 27 (NR, 21–33) | M: 17 F:21 | 38 | R: 30 D: 30 | SSP: 28 (74%) SSP+ SLAP: 10 (26%) | Full thickness: 23 Partial: 15 | Professional overhead athletes. | Multifactorial related to overhead-throwing sports | 10.5 (6–18) | Tear: 1 or 2 triple-loaded, metal suture anchors (Threvo;ConMed, Largo FL, USA) SLAP: double-loaded nonmetallicsuture anchors (Lupine, DePuySynthes; Raynham, MA, USA and Y-knot, ConMed; Largo, FL, USA) | Minimum 24 months |
| 2018, Parness et al. [19] | Retrospective cohort | 3 | 32.7 (NA, 21–39 years) | M: 35 F: 7 | 42 | NR | SSP: 37 SSP + ISP: 2 SSP + ISP + S: 3 | Full thickness | Military | T: 24 (68.5%) NT: 18 (31.4%) | 23 months | Simple or double row repai | 41 (SD = NR, 24 to 66) | |
| 2018, Rossi et al. [20] | 16 | Case series | 4 | Subgroup analysis: 20–40 years | M: 37, F: 33 * | 70 * | D: 43, ND: 27 * | SSP * | Partial thickness (38 bursal, 32 articular) * | Non collision/non overhead = 35. High impact/collision sports = 20. Overhead sport = 15 * | T: 20 NT: 50 * | 5.8 * | Simple row repair For <1 cm: 1 anchor used. For >1 cm: 2 anchor used * | 54 (SD = NR, 24 to 113) * |
| 2019, Erickson et al. [21] | 8 | Case series | 4 | 24.6 (4.1) | M: 151 | 151 | D: 141 ND: 10 | SSP: 48 SSP + ISP: 68 ISP: 29 SS: 2 | Full thickness: 4%, Partial thickness: 96% | Baseball (Major league) | Trauma: 141 (100%) | NR | 130 debridement 21 repairs (6 single row, 5 double rows, 10 side to side) Anchors: 2.09 (1.1, range, 1–4) | Minimum 12 months |
| 2020, Kaptan et al. [22] | 14 | Case series | 4 | 41.4 (3.96, 31–45) | M: 24, F: 26 | 50 | NR | NR | Full thickness: 20, Partial thickness: 30 | NR | T: 39 (78%) NT: 11 (22%) | 1.38 | Double row repair | 42.4 (SD = 13.3, 24 to 95) |
| 2021, Castagna et al. [23] | 13 | Case series | 4 | 28 (6.2, NR) | M: 3 | 3 | D: 1/3, ND: 2/3 | NR | NR | Professional soccer goalkeepers | T: 3 (100%) | 2.53 (1.84–2.99) | NR | 57 (SD = NR, 140 to 130) |
| 2021, Davey et al. [24] | 10 | Case series | 4 | 25.5 (NR, 18–29) | M: 80%, F: 20% | 20 | NR | SSP: 18 SS: 2 | NR | Collision athlete 75% Overhead sport athlete 20%. Professional athlete 10%. Competitive athlete 80%. Recreational athlete 10% | T: 100% | <3 | Double-row repair with medial knots and knotless lateral anchor. Depending on the extent of the tear, 1 or 2 medial-row anchors and 1 or 2 lateral anchors were used | 31.8 (SD = 14.7, 15 to 56) |
| 2022, Scanaliato et al. [25] | 14 | Case series | 4 | 34.03 (NR, 24–39) | M: 33 (89.2%) | 37 | R: 67.6% (25) D: 75.7% (28) | NR | Full thickness | Military | T: 100% | 25.05 ± 28.13 (3–120) | Single-row technique utilized for C1 and C2 tears and a suture bridge double-row repair for C3 and C4 tears. | 104.51 (SD = 7.67, NR) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moussa, M.K.; Lang, E.; Gerometta, A.; Karam, K.; Chelli, M.; Grimaud, O.; Lefèvre, N.; Bou Raad, R.; Bohu, Y.; Khiami, F.; et al. Return to Sports and Activities after Arthroscopic Treatments for Rotator Cuff Lesions in Young Patients Less Than 45-Years-Old: A Systematic Review. J. Clin. Med. 2024, 13, 3703. https://doi.org/10.3390/jcm13133703
Moussa MK, Lang E, Gerometta A, Karam K, Chelli M, Grimaud O, Lefèvre N, Bou Raad R, Bohu Y, Khiami F, et al. Return to Sports and Activities after Arthroscopic Treatments for Rotator Cuff Lesions in Young Patients Less Than 45-Years-Old: A Systematic Review. Journal of Clinical Medicine. 2024; 13(13):3703. https://doi.org/10.3390/jcm13133703
Chicago/Turabian StyleMoussa, Mohamad K., Elena Lang, Antoine Gerometta, Karam Karam, Mickael Chelli, Olivier Grimaud, Nicolas Lefèvre, Ryan Bou Raad, Yoann Bohu, Frédéric Khiami, and et al. 2024. "Return to Sports and Activities after Arthroscopic Treatments for Rotator Cuff Lesions in Young Patients Less Than 45-Years-Old: A Systematic Review" Journal of Clinical Medicine 13, no. 13: 3703. https://doi.org/10.3390/jcm13133703
APA StyleMoussa, M. K., Lang, E., Gerometta, A., Karam, K., Chelli, M., Grimaud, O., Lefèvre, N., Bou Raad, R., Bohu, Y., Khiami, F., Khalaf, Z., Abadie, P., & Hardy, A. (2024). Return to Sports and Activities after Arthroscopic Treatments for Rotator Cuff Lesions in Young Patients Less Than 45-Years-Old: A Systematic Review. Journal of Clinical Medicine, 13(13), 3703. https://doi.org/10.3390/jcm13133703






