Antithrombotic Therapy in Patients Undergoing Transcatheter Aortic Valve Implantation
Abstract
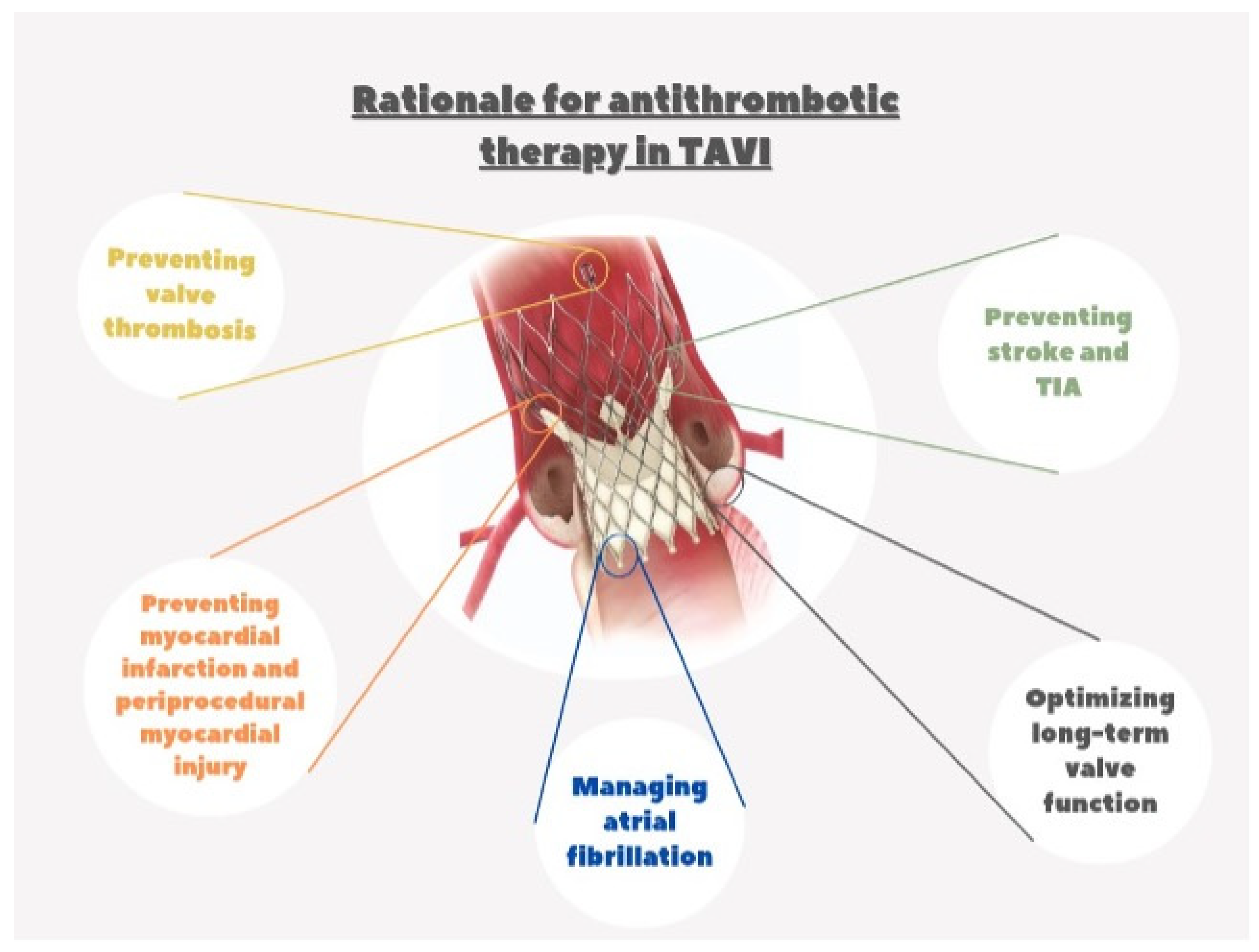
1. Rationale for Antithrombotic Therapy after TAVI
2. The Initial Experience in the Pivotal Randomized Trials of TAVI
3. Randomized Trials for Different Antithrombotic Therapy Regimens after TAVI
3.1. DAPT vs. SAPT
3.2. OAC vs. DAPT
3.2.1. Patients with a Clinical Indication for OAC
3.2.2. Patients without a Clinical Indication for OAC
3.3. No Antithrombotic Therapy
3.4. Personalized Treatment Based on Individual Patient Risk
3.5. Current Guideline Recommendations: ESC/EACTS and ACC/AHA Guidelines
3.6. Special Conditions: Patients Undergoing Concomitant Coronary Stent Implantation
3.7. Future Perspective on Optimization of Antithrombotic Therapy in TAVI Patients
3.8. Future Perspective on Optimization of Antithrombotic Therapy in TAVI Patients: New Drugs
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Grüntzig, A.R.; Senning, Å.; Siegenthaler, W.E. Nonoperative dilatation of coronary-artery stenosis: Percutaneous transluminal coronary angioplasty. N. Engl. J. Med. 1979, 301, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Schömig, A.; Neumann, F.-J.; Kastrati, A.; Schühlen, H.; Blasini, R.; Hadamitzky, M.; Walter, H.; Zitzmann-Roth, E.-M.; Richardt, G.; Alt, E.; et al. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N. Engl. J. Med. 1996, 334, 1084–1089. [Google Scholar] [CrossRef] [PubMed]
- Leon, M.B.; Baim, D.S.; Popma, J.J.; Gordon, P.C.; Cutlip, D.E.; Ho, K.K.L.; Giambartolomei, A.; Diver, D.J.; Lasorda, D.M.; Williams, D.O.; et al. A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting: Stent Anticoagulation Restenosis Study Investigators. N. Engl. J. Med. 1998, 339, 1665–1671. [Google Scholar] [CrossRef] [PubMed]
- Valgimigli, M.; Costa, F.; Byrne, R.; Haude, M.; Baumbach, A.; Windecker, S. Dual antiplatelet therapy duration after coronary stenting in clinical practice: Results of an EAPCI survey. EuroIntervent. J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2015, 11, 68–74. [Google Scholar] [CrossRef]
- Collet, J.-P.; Roffi, M.; Byrne, R.A.; Costa, F.; Valgimigli, M.; Bueno, H.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; et al. Case-based implementation of the 2017 ESC Focused Update on Dual Antiplatelet Therapy in Coronary Artery Disease. Eur. Heart J. 2018, 39, e1–e33. [Google Scholar] [CrossRef] [PubMed]
- Valgimigli, M.; Bueno, H.; Byrne, R.; Collet, J.-P.; Costa, F.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2018, 39, 213–260. [Google Scholar] [CrossRef]
- Task Force Members; Montalescot, G.; Sechtem, U.; Achenbach, S.; Andreotti, F.; Arden, C.; Budaj, A.; Bugiardini, R.; Crea, F.; Cuisset, T.; et al. 2013 ESC guidelines on the management of stable coronary artery disease: The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur. Heart J. 2013, 34, 2949–3003. [Google Scholar] [CrossRef]
- King, T.D.; Thompson, S.L.; Steiner, C.; Mills, N.L. Secundum atrial septal defect. Nonoperative closure during cardiac catheterization. JAMA 1976, 235, 2506–2509. [Google Scholar] [CrossRef] [PubMed]
- Bridges, N.D.; Hellenbrand, W.; Latson, L.; Filiano, J.; Newburger, J.W.; Lock, J.E. Transcatheter closure of patent foramen ovale after presumed paradoxical embolism. Circulation 1992, 86, 1902–1908. [Google Scholar] [CrossRef]
- Cribier, A.; Eltchaninoff, H.; Bash, A.; Borenstein, N.; Tron, C.; Bauer, F.; Derumeaux, G.; Anselme, F.; Laborde, F.; Leon, M.B.; et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: First human case description. Circulation 2002, 106, 3006–3008. [Google Scholar] [CrossRef]
- Kaneko, T.; Aranki, S.; Javed, Q.; McGurk, S.; Shekar, P.; Davidson, M.; Cohn, L. Mechanical versus bioprosthetic mitral valve replacement in patients <65 years old. J. Thorac. Cardiovasc. Surg. 2014, 147, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Rotman, O.M.; Bianchi, M.; Ghosh, R.P.; Kovarovic, B.; Bluestein, D. Principles of TAVR valve design, modelling, and testing. Expert Rev. Med. Devices 2018, 15, 771–791. [Google Scholar] [CrossRef] [PubMed]
- Anatomo-Pathological Analysis after CoreValve Revalving System Implantation—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/19577986/ (accessed on 19 February 2024).
- Tay, E.L.; Gurvitch, R.; Wijesinghe, N.; Nielispach, F.; Wood, D.; Cheung, A.; Ye, J.; Lichtenstein, S.V.; Carere, R.; Thompson, C.; et al. A high-risk period for cerebrovascular events exists after transcatheter aortic valve implantation. JACC Cardiovasc. Interv. 2011, 4, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Faroux, L.; Munoz-Garcia, E.; Serra, V.; Alperi, A.; Nombela-Franco, L.; Fischer, Q.; Veiga, G.; Donaint, P.; Asmarats, L.; Vilalta, V.; et al. Acute Coronary Syndrome Following Transcatheter Aortic Valve Replacement. Circ. Cardiovasc. Interv. 2020, 13, e008620. [Google Scholar] [CrossRef]
- Faroux, L.; Guimaraes, L.; Wintzer-Wehekind, J.; Junquera, L.; Ferreira-Neto, A.N.; del Val, D.; Muntané-Carol, G.; Mohammadi, S.; Paradis, J.-M.; Rodés-Cabau, J. Coronary Artery Disease and Transcatheter Aortic Valve Replacement: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 74, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Dey, T.; Sankaramangalam, K.; Alansari, S.A.R.; Williams, L.; Mick, S.; Krishnaswamy, A.; Svensson, L.G.; Kapadia, S. Prognostically Significant Myocardial Injury in Patients Undergoing Transcatheter Aortic Valve Replacement. J. Am. Heart Assoc. 2019, 8, e011889. [Google Scholar] [CrossRef]
- Koskinas, K.C.; Stortecky, S.; Franzone, A.; O’Sullivan, C.J.; Praz, F.; Zuk, K.; Räber, L.; Pilgrim, T.; Moschovitis, A.; Fiedler, G.M.; et al. Post-Procedural Troponin Elevation and Clinical Outcomes Following Transcatheter Aortic Valve Implantation. J. Am. Heart Assoc. 2016, 5, e002430. [Google Scholar] [CrossRef]
- Stundl, A.; Schulte, R.; Lucht, H.; Weber, M.; Sedaghat, A.; Shamekhi, J.; Zur, B.; Grube, E.; Mellert, F.; Welz, A.; et al. Periprocedural Myocardial Injury Depends on Transcatheter Heart Valve Type But Does Not Predict Mortality in Patients After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2017, 10, 1550–1560. [Google Scholar] [CrossRef] [PubMed]
- De Marzo, V.; Crimi, G.; Vercellino, M.; Benenati, S.; Pescetelli, F.; Della Bona, R.; Sarocchi, M.; Canepa, M.; Balbi, M.; Porto, I. Impact of bioprosthetic valve type on peri-procedural myocardial injury and mortality after transcatheter aortic valve replacement. Heart Vessel. 2021, 36, 1746–1755. [Google Scholar] [CrossRef]
- Dagan, M.; Dawson, L.P.; Stehli, J.; Koh, J.Q.S.; Quine, E.; Stub, D.; Htun, N.M.; Walton, A.; Duffy, S.J. Periprocedural Myocardial Injury and Coronary Artery Disease in Patients Undergoing Transcatheter Aortic Valve Replacement. Cardiovasc. Revascular. Med. 2022, 35, 8–15. [Google Scholar] [CrossRef]
- de Azevedo Filho, A.F.; Accorsi, T.A.; Ribeiro, H.B. Coronary Artery Disease in Patients with Aortic Stenosis and Transcatheter Aortic Valve Implantation: Implications for Management. Eur. Cardiol. Rev. 2021, 16, e49. [Google Scholar] [CrossRef] [PubMed]
- Sankaramangalam, K.; Banerjee, K.; Kandregula, K.; Mohananey, D.; Parashar, A.; Jones, B.M.; Jobanputra, Y.; Mick, S.; Krishnaswamy, A.; Svensson, L.G.; et al. Impact of Coronary Artery Disease on 30-Day and 1-Year Mortality in Patients Undergoing Transcatheter Aortic Valve Replacement: A Meta-Analysis. J. Am. Heart Assoc. 2017, 6, e006092. [Google Scholar] [CrossRef]
- Guedeney, P.; Chieffo, A.; Snyder, C.; Mehilli, J.; Petronio, A.S.; Claessen, B.E.; Sartori, S.; Lefèvre, T.; Presbitero, P.; Capranzano, P.; et al. Impact of Baseline Atrial Fibrillation on Outcomes Among Women Who Underwent Contemporary Transcatheter Aortic Valve Implantation (from the Win-TAVI Registry). Am. J. Cardiol. 2018, 122, 1909–1916. [Google Scholar] [CrossRef]
- Chakravarty, T.; Søndergaard, L.; Friedman, J.; De Backer, O.; Berman, D.; Kofoed, K.F.; Jilaihawi, H.; Shiota, T.; Abramowitz, Y.; Jørgensen, T.H.; et al. Subclinical leaflet thrombosis in surgical and transcatheter bioprosthetic aortic valves: An observational study. Lancet 2017, 389, 2383–2392. [Google Scholar] [CrossRef]
- Søndergaard, L. Subclinical leaflet thrombosis—A concern, but also an issue? EuroIntervent. J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2018, 13, e1738–e1740. [Google Scholar] [CrossRef] [PubMed]
- Renker, M.; Kim, W.-K. Choice of transcatheter heart valve: Should we select the device according to each patient’s characteristics or should it be “one valve fits all”? Ann. Transl. Med. 2020, 8, 961. [Google Scholar] [CrossRef] [PubMed]
- Kalogeropoulos, A.S.; Redwood, S.R.; Allen, C.J.; Hurrell, H.; Chehab, O.; Rajani, R.; Prendergast, B.; Patterson, T. A 20-year journey in transcatheter aortic valve implantation: Evolution to current eminence. Front. Cardiovasc. Med. 2022, 9, 971762. [Google Scholar] [CrossRef]
- Mangieri, A.; Montalto, C.; Poletti, E.; Sticchi, A.; Crimi, G.; Giannini, F.; Latib, A.; Capodanno, D.; Colombo, A. Thrombotic Versus Bleeding Risk After Transcatheter Aortic Valve Replacement: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 74, 2088–2101. [Google Scholar] [CrossRef]
- Gilard, M.; Eltchaninoff, H.; Donzeau-Gouge, P.; Chevreul, K.; Fajadet, J.; Leprince, P.; Leguerrier, A.; Lievre, M.; Prat, A.; Teiger, E.; et al. Late Outcomes of Transcatheter Aortic Valve Replacement in High-Risk Patients: The FRANCE-2 Registry. J. Am. Coll. Cardiol. 2016, 68, 1637–1647. [Google Scholar] [CrossRef]
- Adams, D.H.; Popma, J.J.; Reardon, M.J.; Yakubov, S.J.; Coselli, J.S.; Deeb, G.M.; Gleason, T.G.; Buchbinder, M.; Hermiller, J., Jr.; Kleiman, N.S.; et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N. Engl. J. Med. 2014, 370, 1790–1798. [Google Scholar] [CrossRef]
- Nikolayevska, O.; Conradi, L.; Schirmer, J.; Reichenspurner, H.; Deuschl, F.; Blankenberg, S.; Schäfer, U. Comparison of a novel self-expanding transcatheter heart valve with two established devices for treatment of degenerated surgical aortic bioprostheses. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2024, 113, 18–28. [Google Scholar] [CrossRef]
- Smith, C.R.; Leon, M.B.; Mack, M.J.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Makkar, R.R.; et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 2011, 364, 2187–2198. [Google Scholar] [CrossRef] [PubMed]
- Leon, M.B.; Smith, C.R.; Mack, M.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Makkar, R.R.; et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 2010, 363, 1597–1607. [Google Scholar] [CrossRef] [PubMed]
- Rodés-Cabau, J.; Dauerman, H.L.; Cohen, M.G.; Mehran, R.; Small, E.M.; Smyth, S.S.; Costa, M.A.; Mega, J.L.; O’Donoghue, M.L.; Ohman, E.M.; et al. Antithrombotic Treatment in Transcatheter Aortic Valve Implantation: Insights for Cerebrovascular and Bleeding Events. J. Am. Coll. Cardiol. 2013, 62, 2349–2359. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Y.; Howard, J.P.; Madhavan, M.V.; Leon, M.B.; Makkar, R.R. Single Versus Dual Antiplatelet Therapy After Transcatheter Aortic Valve Replacement: A Meta-Analysis of Randomized Clinical Trials. Cardiovasc. Revascular. Med. 2022, 34, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Rodés-Cabau, J.; Masson, J.-B.; Welsh, R.C.; del Blanco, B.G.; Pelletier, M.; Webb, J.G.; Al-Qoofi, F.; Généreux, P.; Maluenda, G.; Thoenes, M.; et al. Aspirin Versus Aspirin Plus Clopidogrel as Antithrombotic Treatment Following Transcatheter Aortic Valve Replacement with a Balloon-Expandable Valve: The ARTE (Aspirin Versus Aspirin + Clopidogrel Following Transcatheter Aortic Valve Implantation) Randomized Clinical Trial. JACC Cardiovasc. Interv. 2017, 10, 1357–1365. [Google Scholar] [CrossRef] [PubMed]
- Kappetein, A.P.; Head, S.J.; Généreux, P.; Piazza, N.; van Mieghem, N.M.; Blackstone, E.H.; Brott, T.G.; Cohen, D.J.; Cutlip, D.E.; van Es, G.-A.; et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document (VARC-2). Eur. J. Cardio-Thoracic Surg. 2012, 42, S45–S60. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, J.; Nijenhuis, V.J.; Delewi, R.; Hermanides, R.S.; Holvoet, W.; Dubois, C.L.; Frambach, P.; De Bruyne, B.; van Houwelingen, G.K.; Van Der Heyden, J.A.; et al. Aspirin with or without Clopidogrel after Transcatheter Aortic-Valve Implantation. N. Engl. J. Med. 2020, 383, 1447–1457. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, J.; Nijenhuis, V.J.; Rodés-Cabau, J.; Stabile, E.; Barbanti, M.; Costa, G.; Mahmoodi, B.K.; Berg, J.M.T. Aspirin Alone Versus Dual Antiplatelet Therapy After Transcatheter Aortic Valve Implantation: A Systematic Review and Patient-Level Meta-Analysis. J. Am. Heart Assoc. 2021, 10, e019604. [Google Scholar] [CrossRef]
- Shaul, A.A.; Kornowski, R.; Bental, T.; Vaknin-Assa, H.; Assali, A.; Golovchiner, G.; Kadmon, E.; Codner, P.; Orvin, K.; Strasberg, B.; et al. Type of Atrial Fibrillation and Clinical Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement. Ann. Noninvasive Electrocardiol. 2016, 21, 519–525. [Google Scholar] [CrossRef]
- Lee, S.Y.; Choi, K.H.; Park, T.K.; Kim, J.; Kim, E.K.; Park, S.-J.; Park, S.W.; Gwon, H.-C.; Chang, K.; Yu, C.W.; et al. Impact of Atrial Fibrillation on Patients Undergoing Transcatheter Aortic Valve Implantation (TAVI): The K-TAVI Registry. Yonsei Med. J. 2023, 64, 413–422. [Google Scholar] [CrossRef]
- Mentias, A.; Saad, M.; Girotra, S.; Desai, M.; Elbadawi, A.; Briasoulis, A.; Alvarez, P.; Alqasrawi, M.; Giudici, M.; Panaich, S.; et al. Impact of Pre-Existing and New-Onset Atrial Fibrillation on Outcomes After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2019, 12, 2119–2129. [Google Scholar] [CrossRef] [PubMed]
- Long, E.; Pitfield, A.F.; Kissoon, N. Anticoagulation therapy: Indications, monitoring, and complications. Pediatr. Emerg. Care 2011, 27, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef] [PubMed]
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1706–1715. [Google Scholar] [CrossRef] [PubMed]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef] [PubMed]
- Thyregod, H.G.H.; Steinbrüchel, D.A.; Ihlemann, N.; Nissen, H.; Kjeldsen, B.J.; Petursson, P.; Chang, Y.; Franzen, O.W.; Engstrøm, T.; Clemmensen, P.; et al. Transcatheter versus Surgical Aortic Valve Replacement in Patients with Severe Aortic Valve Stenosis: 1-Year Results From the All-Comers NOTION Randomized Clinical Trial. J. Am. Coll. Cardiol. 2015, 65, 2184–2194. [Google Scholar] [CrossRef]
- Reardon, M.J.; Van Mieghem, N.M.; Popma, J.J.; Kleiman, N.S.; Søndergaard, L.; Mumtaz, M.; Adams, D.H.; Deeb, G.M.; Maini, B.; Gada, H.; et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2017, 376, 1321–1331. [Google Scholar] [CrossRef]
- Vora, A.N.; Dai, D.; Matsuoka, R.; Harrison, J.K.; Hughes, G.C.; Sherwood, M.W.; Piccini, J.P.; Bhardwaj, B.; Lopes, R.D.; Cohen, D.; et al. Incidence, Management, and Associated Clinical Outcomes of New-Onset Atrial Fibrillation Following Transcatheter Aortic Valve Replacement: An Analysis From the STS/ACC TVT Registry. JACC Cardiovasc. Interv. 2018, 11, 1746–1756. [Google Scholar] [CrossRef]
- Siontis, G.C.M.; Overtchouk, P.; Cahill, T.J.; Modine, T.; Prendergast, B.; Praz, F.; Pilgrim, T.; Petrinic, T.; Nikolakopoulou, A.; Salanti, G.; et al. Transcatheter aortic valve implantation vs. surgical aortic valve replacement for treatment of symptomatic severe aortic stenosis: An updated meta-analysis. Eur. Heart J. 2019, 40, 3143–3153. [Google Scholar] [CrossRef]
- Indja, B.; Woldendorp, K.; Vallely, M.P.; Grieve, S.M. New Onset Atrial Fibrillation Following Transcatheter and Surgical Aortic Valve Replacement: A Systematic Review and Meta-Analysis. Heart Lung Circ. 2020, 29, 1542–1553. [Google Scholar] [CrossRef] [PubMed]
- Furuta, A.; Lellouche, N.; Mouillet, G.; Dhanjal, T.; Gilard, M.; Laskar, M.; Eltchaninoff, H.; Fajadet, J.; Iung, B.; Donzeau-Gouge, P.; et al. Prognostic value of new onset atrial fibrillation after transcatheter aortic valve implantation: A FRANCE 2 registry substudy. Int. J. Cardiol. 2016, 210, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Chopard, R.; Teiger, E.; Meneveau, N.; Chocron, S.; Gilard, M.; Laskar, M.; Eltchaninoff, H.; Iung, B.; Leprince, P.; Chevreul, K.; et al. Baseline Characteristics and Prognostic Implications of Pre-Existing and New-Onset Atrial Fibrillation After Transcatheter Aortic Valve Implantation: Results From the FRANCE-2 Registry. JACC Cardiovasc. Interv. 2015, 8, 1346–1355. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.-H.; Ahn, J.-M.; Kang, D.-Y.; Ko, E.; Lee, P.H.; Lee, S.-W.; Kim, H.J.; Kim, J.B.; Choo, S.J.; Park, D.-W.; et al. Incidence, Predictors, Management, and Clinical Significance of New-Onset Atrial Fibrillation After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2019, 123, 1127–1133. [Google Scholar] [CrossRef] [PubMed]
- Nijenhuis, V.J.; Brouwer, J.; Delewi, R.; Hermanides, R.S.; Holvoet, W.; Dubois, C.L.; Frambach, P.; De Bruyne, B.; Van Houwelingen, G.K.; Van Der Heyden, J.A.; et al. Anticoagulation with or without Clopidogrel after Transcatheter Aortic-Valve Implantation. N. Engl. J. Med. 2020, 382, 1696–1707. [Google Scholar] [CrossRef] [PubMed]
- Van Mieghem, N.M.; Unverdorben, M.; Valgimigli, M.; Mehran, R.; Boersma, E.; Baber, U.; Hengstenberg, C.; Shi, M.; Chen, C.; Saito, S.; et al. Edoxaban Versus standard of care and their effects on clinical outcomes in patients having undergone Transcatheter Aortic Valve Implantation in Atrial Fibrillation—Rationale and design of the ENVISAGE-TAVI AF trial. Am. Heart J. 2018, 205, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Van Belle, E.; Thiele, H.; Berti, S.; Lhermusier, T.; Manigold, T.; Neumann, F.J.; Gilard, M.; Attias, D.; Beygui, F.; et al. Apixaban vs. standard of care after transcatheter aortic valve implantation: The ATLANTIS trial. Eur. Heart J. 2022, 43, 2783–2797. [Google Scholar] [CrossRef]
- Makkar, R.R.; Fontana, G.; Jilaihawi, H.; Chakravarty, T.; Kofoed, K.F.; De Backer, O.; Asch, F.M.; Ruiz, C.E.; Olsen, N.T.; Trento, A.; et al. Possible Subclinical Leaflet Thrombosis in Bioprosthetic Aortic Valves. N. Engl. J. Med. 2015, 373, 2015–2024. [Google Scholar] [CrossRef] [PubMed]
- Dangas, G.D.; Tijssen, J.G.; Wöhrle, J.; Søndergaard, L.; Gilard, M.; Möllmann, H.; Makkar, R.R.; Herrmann, H.C.; Giustino, G.; Baldus, S.; et al. A Controlled Trial of Rivaroxaban after Transcatheter Aortic-Valve Replacement. N. Engl. J. Med. 2020, 382, 120–129. [Google Scholar] [CrossRef]
- De Backer, O.; Dangas, G.D.; Jilaihawi, H.; Leipsic, J.A.; Terkelsen, C.J.; Makkar, R.; Kini, A.S.; Veien, K.T.; Abdel-Wahab, M.; Kim, W.-K.; et al. Reduced Leaflet Motion after Transcatheter Aortic-Valve Replacement. N. Engl. J. Med. 2020, 382, 130–139. [Google Scholar] [CrossRef]
- Park, D.-W.; Ahn, J.-M.; Kang, D.-Y.; Kim, K.W.; Koo, H.J.; Yang, D.H.; Jung, S.C.; Kim, B.; Wong, Y.T.A.; Lam, C.C.S.; et al. Edoxaban Versus Dual Antiplatelet Therapy for Leaflet Thrombosis and Cerebral Thromboempolism After TAVR: The ADADT-TAVR Randomized Clinical Trial. Circulation 2022, 146, 466–479. [Google Scholar] [CrossRef] [PubMed]
- Giustino, G.; Genereux, P. Subclinical Thrombosis of Bioprosthetic Aortic Valves. J. Am. Coll. Cardiol. 2020, 75, 3016–3019. [Google Scholar] [CrossRef] [PubMed]
- Sondergaard, L.; De Backer, O.; Kofoed, K.F.; Jilaihawi, H.; Fuchs, A.; Chakravarty, T.; Kashif, M.; Kazuno, Y.; Kawamori, H.; Maeno, Y.; et al. Natural history of subclinical leaflet thrombosis affecting motion in bioprosthetic aortic valves. Eur. Heart J. 2017, 38, 2201–2207. [Google Scholar] [CrossRef]
- Kobari, Y.; Inohara, T.; Tsuruta, H.; Yashima, F.; Shimizu, H.; Fukuda, K.; Naganuma, T.; Mizutani, K.; Yamawaki, M.; Tada, N.; et al. No Antithrombotic Therapy After Transcatheter Aortic Valve Replacement: Insight From the OCEAN-TAVI Registry. JACC Cardiovasc. Interv. 2023, 16, 79–91. [Google Scholar] [CrossRef]
- Miyasaka, M.; Tada, N.; Taguri, M.; Kato, S.; Enta, Y.; Otomo, T.; Hata, M.; Watanabe, Y.; Naganuma, T.; Araki, M.; et al. Incidence, Predictors, and Clinical Impact of Prosthesis-Patient Mismatch Following Transcatheter Aortic Valve Replacement in Asian Patients: The OCEAN-TAVI Registry. JACC Cardiovasc. Interv. 2018, 11, 771–780. [Google Scholar] [CrossRef]
- Inohara, T.; Otsuka, T.; Watanabe, Y.; Shirai, S.; Tada, N.; Yamanaka, F.; Ueno, H.; Ohno, Y.; Tabata, M.; Suzuyama, H.; et al. Rationale and design of Non-antithrombotic Therapy After Transcatheter Aortic Valve Implantation (NAPT) Trial. Contemp. Clin. Trials 2023, 134, 107358. [Google Scholar] [CrossRef] [PubMed]
- Navarese, E.P.; Zhang, Z.; Kubica, J.; Andreotti, F.; Farinaccio, A.; Bartorelli, A.L.; Bedogni, F.; Rupji, M.; Tomai, F.; Giordano, A.; et al. Development and Validation of a Practical Model to Identify Patients at Risk of Bleeding after TAVR. JACC Cardiovasc. Interv. 2021, 14, 1196–1206. [Google Scholar] [CrossRef] [PubMed]
- Zembala-John, J.; Wilczek, K.; Tobota, Z.; Chodór, P.; Cieśla, D.; Jaźwiec, T.; Banasiak, W.; Stępińska, J.; Kalarus, Z.; Opolski, G.; et al. POL-TAVI—Polish Registry of Transcatheter Aortic Valve Implantation—Simple tool, great value, rationale and design. Kardiochirurgia Torakochirurgia Pol. Pol. J. Thorac. Cardiovasc. Surg. 2016, 13, 309–315. [Google Scholar] [CrossRef]
- De Luca, L.; Bolognese, L.; Rubboli, A.; Lucci, D.; Gabrielli, D.; Colivicchi, F.; Gulizia, M.M.; on behalf of the MATADOR-PCI Investigators. Could the PARIS Risk Scores Be Useful for the Choice of Triple versus Dual Antithrombotic Therapy in Patients with Atrial Fibrillation Undergoing Percutaneous Coronary Intervention? Cardiology 2022, 147, 133–136. [Google Scholar] [CrossRef]
- Gallego, P.; Roldán, V.; Torregrosa, J.M.; Gálvez, J.; Valdés, M.; Vicente, V.; Marín, F.; Lip, G.Y.H. Relation of the HAS-BLED bleeding risk score to major bleeding, cardiovascular events, and mortality in anticoagulated patients with atrial fibrillation. Circ. Arrhythmia Electrophysiol. 2012, 5, 312–318. [Google Scholar] [CrossRef]
- Jia, Y.; Luosang, G.; Li, Y.; Wang, J.; Li, P.; Xiong, T.; Li, Y.; Liao, Y.; Zhao, Z.; Peng, Y.; et al. Deep Learning in Prediction of Late Major Bleeding After Transcatheter Aortic Valve Replacement. Clin. Epidemiol. 2022, 14, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Sarker, I.H. Deep Learning: A Comprehensive Overview on Techniques, Taxonomy, Applications and Research Directions. SN Comput. Sci. 2021, 2, 420. [Google Scholar] [CrossRef] [PubMed]
- Garot, P.; Neylon, A.; Morice, M.-C.; Tamburino, C.; Bleiziffer, S.; Thiele, H.; Scholtz, S.; Schramm, R.; Cockburn, J.; Cunnington, M.; et al. Bleeding risk differences after TAVR according to the ARC-HBR criteria: Insights from SCOPE 2. EuroIntervent. J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2022, 18, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Tamburino, C.; Bleiziffer, S.; Thiele, H.; Scholtz, S.; Hildick-Smith, D.; Cunnington, M.; Wolf, A.; Barbanti, M.; Tchetché, D.; Garot, P.; et al. Comparison of Self-Expanding Bioprostheses for Transcatheter Aortic Valve Replacement in Patients with Symptomatic Severe Aortic Stenosis: The SCOPE 2 Randomized Clinical Trial. Circulation 2020, 142, 2431–2442. [Google Scholar] [CrossRef]
- Montalto, C.; Munafò, A.R.; Arzuffi, L.; Casula, M.; Mandurino-Mirizzi, A.; Costa, F.; Leonardi, S.; Visconti, L.O.; Ferlini, M. Validation of the ARC-HBR criteria in 68,874 patients undergoing PCI: A systematic review and meta-analysis. Hell. J. Cardiol. 2022, 66, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Coisne, A.; Lancellotti, P.; Habib, G.; Garbi, M.; Dahl, J.S.; Barbanti, M.; Vannan, M.A.; Vassiliou, V.S.; Dudek, D.; Chioncel, O.; et al. ACC/AHA and ESC/EACTS Guidelines for the Management of Valvular Heart Diseases: JACC Guideline Comparison. J. Am. Coll. Cardiol. 2023, 82, 721–734. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Otto, C.M.; Nishimura, R.A.; Nishimura, R.A.; Bonow, R.O.; Bonow, R.O.; Carabello, B.A.; Carabello, B.A.; Erwin, J.P.; Erwin, J.P.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, e35–e71. [Google Scholar] [CrossRef] [PubMed]
- van Ginkel, D.J.; Bor, W.L.; Veenstra, L.; van Hof, A.W.; Fabris, E. Evolving concepts in the management of antithrombotic therapy in patients undergoing transcatheter aortic valve implantation. Eur. J. Intern. Med. 2022, 101, 14–20. [Google Scholar] [CrossRef]
- Berg, J.T.; Sibbing, D.; Rocca, B.; Van Belle, E.; Chevalier, B.; Collet, J.-P.; Dudek, D.; Gilard, M.; Gorog, D.A.; Grapsa, J.; et al. Management of antithrombotic therapy in patients undergoing transcatheter aortic valve implantation: A consensus document of the ESC Working Group on Thrombosis and the European Association of Percutaneous Cardiovascular Interventions (EAPCI), in collaboration with the ESC Council on Valvular Heart Disease. Eur. Heart J. 2021, 42, 2265–2269. [Google Scholar] [CrossRef]
- Greco, A.; Laudani, C.; Spagnolo, M.; Agnello, F.; Faro, D.C.; Finocchiaro, S.; Legnazzi, M.; Mauro, M.S.; Mazzone, P.M.; Occhipinti, G.; et al. Pharmacology and Clinical Development of Factor XI Inhibitors. Circulation 2023, 147, 897–913. [Google Scholar] [CrossRef] [PubMed]
| Study Title | Patients Enrolled (n) | Target Population | Experimental Treatment | Control Treatment | Primary Endpoint (Experimental Group vs. Control Group) |
|---|---|---|---|---|---|
| ARTE | 222 | Patients undergoing TAVI without an indication for OAC | Aspirin + clopidogrel | Aspirin monotherapy | Composite of death, MI, stroke, TIA, or major/life-threatening bleed (at 90-day follow-up (15.3% vs. 7.2%) (OR 95% (CI) = 2.31 (0.95–5.62); p = 0.065) |
| POPular TAVI cohort A | 665 | Patients undergoing TAVI without an indication for OAC | Aspirin monotherapy | Aspirin + clopidogrel | Two primary endpoints: All bleeding (minor, major, life-threatening, or disabling) (15.1% vs. 26.6%) (risk ratio, 0.57; 95% (CI), 0.42 to 0.77; p = 0.001) Non-procedure-related bleeding (including bleeding at the puncture site) (15.1% vs. 24.9%) (risk ratio, 0.61; 95% (CI), 0.44 to 0.83; p = 0.005) |
| POPular TAVI cohort B | 313 | Patients undergoing TAVI with an indication for chronic OAC | VKA or DOAC | OAC + clopidogrel | Two primary endpoints: All bleeding (minor, major, life-threatening or disabling) (21.7% vs. 34.6%) (risk ratio, 0.63; 95% confidence interval (CI), 0.43 to 0.90; p = 0.01) No-procedure-related bleeding (including bleeding at the puncture site) (21.7% vs. 34.0%) (risk ratio, 0.64; 95% (CI), 0.44 to 0.92; p = 0.02) |
| ATLANTIS stratum 1 | 451 | Patients undergoing TAVI with an indication for chronic OAC | Apixaban | VKA | Composite of death, MI, stroke, or TIA, non–central nervous system embolism, pulmonary embolism, intracardiac or valve thrombosis, deep vein thrombosis, and life-threatening, disabling, or major bleeding (22.0% vs. 21.9%) (HR 1.02; 0.69–1.51; p = NS) |
| ENVISAGE-TAVI AF | 1426 | Patients undergoing TAVI with an indication for chronic OAC | Edoxaban | VKA | Composite of all-cause death, MI, ischemic stroke, systemic thromboembolism, valve thrombosis, or major bleeding (17.3% vs. 16.5%) (HR, 1.40; 95% (CI), 1.03 to 1.91; p = 0.93 for noninferiority) |
| GALILEO | 1644 | Patients undergoing TAVI without an indication for OAC | Rivaroxaban + aspirin | Clopidogrel + aspirin | Efficacy outcome: death or thromboembolic event (ie, stroke, MI, symptomatic valve thrombosis, non–central nervous system systemic embolism, pulmonary embolism, or deep vein thrombosis) (12.7% vs. 9.5%) (HR, 1.35; 95% (CI), 1.01 to 1.81; p = 0.04) Safety outcome: major, life-threatening, or disabling bleed (5.6% vs. 3.8%) (HR 1.50 (0.95 to 2.37); 95% (CI)) |
| GALILEO 4D | 231 | Patients undergoing TAVI either native or ViV | Rivaroxaban + aspirin | Clopidogrel + aspirin | ≥1 prosthetic leaflet with >50% RLM, detected on 4D-CT imaging (2.1% vs. 10.9%) (difference, −8.8 percentage points; 95% confidence interval (CI), −16.5 to −1.9; p = 0.01) |
| ADAPT-TAVR trial | 229 | Patients undergoing TAVI without an indication for OAC | Edoxaban | Aspirin + clopidogrel | Incidence of valve leaflet thrombosis detected on 4D-CT imaging (9.8% vs. 18.4%) (absolute difference, −8.5% 95% (CI), −17.8% to 0.8%; p = 0.076) |
| ATLANTIS stratum 2 | 1049 | Patients undergoing TAVI without an indication for OAC | Apixaban | Aspirin and/or clopidogrel | Composite of death, MI, stroke, TIA, non–central nervous system embolism, pulmonary embolism, intracardiac or valve thrombosis, deep vein thrombosis, life-threatening, disabling, or major bleeding (16.9% vs. 19.3%) (HR = 0.88; 95% (CI) (0.66, 1.17); p = 0.57) |
| Trial | N# | Test Arm | Control Arm | Duration | Primary Completion Date | Primary Endpoint |
|---|---|---|---|---|---|---|
| AVATAR (NCT02735902) | 170 | VKA or DOAC (apixaban or edoxaban) | ASA + VKA/DOAC | 12 months post-TAVI | 2024 | Composite of death, stroke, MI, valve thrombosis, and hemorrhage (as defined by VARC 2) |
| POPular PAUSE TAVI (NCT04437303) | 858 | Interruption of OAC | Continuation of OAC | 30 days post-TAVI | 2024 | Composite of cardiovascular mortality, stroke, MI, major vascular complications, and major, disabling, and life-threatening bleeding complications at 30 days post-TAVI, as defined by the VARC-2 criteria |
| POPular ATLANTIS (NCT06168370) | 2500 | (1) If subclinical valve thrombosis on 4D-CT, switch from SAPT to apixaban. (2) If no signs of subclinical valve thrombosis on 4D-CT, without another indication for antiplatelet therapy, stop their SAPT. (3) If no signs of subclinical valve thrombosis on 4D-CT, with another indication for antiplatelet therapy. continue lifelong SAPT | Lifelong SAPT after TAVI | 3 months post-TAVI | 2028 | Composite of cardiovascular death, ischemic stroke, TIA, MI, systemic embolism, and clinically significant valve thrombosis according to the VARC-3 criteria and composite of type 1-4 bleeding, according to the VARC-3 criteria |
| ACASA-TAVI (NCT05035277) | 360 | Apixaban, rivaroxaban, or edoxaban | Aspirin | From 12 months to 10 years | 2026 | (1) Hypo-attenuated leaflet thickening on cardiac CT after 12 months. (2) VARC-3 bleeding events, MI or stroke, all-cause mortality, cardiac death, aortic valve re-intervention, heart failure hospitalization, major, life-threatening, or disabling bleeding. |
| ACLO-TAVR (NCT05493657) | 230 | Clopidogrel | Aspirin | 3 months post-TAVI | 2024 | Incidence of leaflet thrombosis on cardiac CT |
| NAPT (NCT06007222) | 360 | Non-antithrombotic therapy | Aspirin | 1 year to 3 years post-TAVI | 2025 | Composite endpoint consisting of all-cause deaths, MI, stroke from any cause, and bleeding from randomization to end of study |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pallante, F.; Costa, F.; Garcia Ruiz, V.; Vizzari, G.; Iannello, P.; Teresi, L.; Carciotto, G.; Lo Giudice, S.; Iuvara, G.; Laterra, G.; et al. Antithrombotic Therapy in Patients Undergoing Transcatheter Aortic Valve Implantation. J. Clin. Med. 2024, 13, 3636. https://doi.org/10.3390/jcm13133636
Pallante F, Costa F, Garcia Ruiz V, Vizzari G, Iannello P, Teresi L, Carciotto G, Lo Giudice S, Iuvara G, Laterra G, et al. Antithrombotic Therapy in Patients Undergoing Transcatheter Aortic Valve Implantation. Journal of Clinical Medicine. 2024; 13(13):3636. https://doi.org/10.3390/jcm13133636
Chicago/Turabian StylePallante, Francesco, Francesco Costa, Victoria Garcia Ruiz, Giampiero Vizzari, Pietro Iannello, Lucio Teresi, Gabriele Carciotto, Stefania Lo Giudice, Giustina Iuvara, Giulia Laterra, and et al. 2024. "Antithrombotic Therapy in Patients Undergoing Transcatheter Aortic Valve Implantation" Journal of Clinical Medicine 13, no. 13: 3636. https://doi.org/10.3390/jcm13133636
APA StylePallante, F., Costa, F., Garcia Ruiz, V., Vizzari, G., Iannello, P., Teresi, L., Carciotto, G., Lo Giudice, S., Iuvara, G., Laterra, G., Regueiro, A., Giustino, G., Alonso Briales, J. H., Hernandez, J. M., Barbanti, M., Micari, A., & Patanè, F. (2024). Antithrombotic Therapy in Patients Undergoing Transcatheter Aortic Valve Implantation. Journal of Clinical Medicine, 13(13), 3636. https://doi.org/10.3390/jcm13133636







