Myocardial Mechanics and Associated Valvular and Vascular Abnormalities in Left Ventricular Noncompaction Cardiomyopathy
Abstract
1. Noncompaction Cardiomyopathy
2. Cardiovascular Imaging and Criteria
- -
- Chin’s criterion is the earliest and simplest criterion: The distance between the epicardial surface and the trough of the trabeculation divided by the distance between the epicardial surface and the peak of the trabeculum measured at the apex of the LV in parasternal short-axis and apical views is ≤0.5 [3].
- -
- Jenni’s criterion is more complicated and takes into account a number of other factors: (I) the presence of a two-layer myocardial structure with a thin compacted and a thicker noncompacted myocardium, (II) the ratio of noncompacted to compacted myocardium > 2 at the end-systole, (III) the absence of coexisting cardiac structural abnormalities, and (IV) excessive prominent trabeculations and deep intertrabecular recesses filled with intraventricular blood with color Doppler imaging. Parameters are measured in parasternal short-axis views [4].
- -
- Stollberger’s criterion is a simplified criterion that is closer to the clinical routine: (I) the presence of >3 trabeculations located apically to the papillary muscles in parasternal short-axis and apical views, within a distinct two-layered myocardium in the end-systole, and (II) perfusion of intertrabecular recesses with either color Doppler or echocardiographic contrast imaging in the end-diastole [10].
- -
- Petersen’s criterion is simple, as it aims to assess the noncompacted/compacted myocardial ratio, ideally with a ratio > 2.3 in the end-diastole, excluding the LV apex from the measurement, as the compacted myocardium is physiologically thinner [11].
- -
- Jacquier’s criterion aims to assess trabecular LV mass, and a value > 20% of global LV mass in the end-diastole is diagnostic [12].
- -
- Grothoff’s criterion is more complicated: (I) LV myocardial mass index of the noncompacted tissue (‘a’) >15 g/m2, (II) ‘a’ as a percentage of total LV myocardial mass index >25%, and (III) increased trabeculation in LV basal segments and a noncompacted/compacted ratio ≥3:1 measured in the end-diastole on the short axis [13].
3. The Left Heart and the Aorta
3.1. Left Ventricle
3.1.1. Under Healthy Circumstances
3.1.2. In Noncompaction Cardiomyopathy
LV Structure, Volumes, and Function
LV Strains
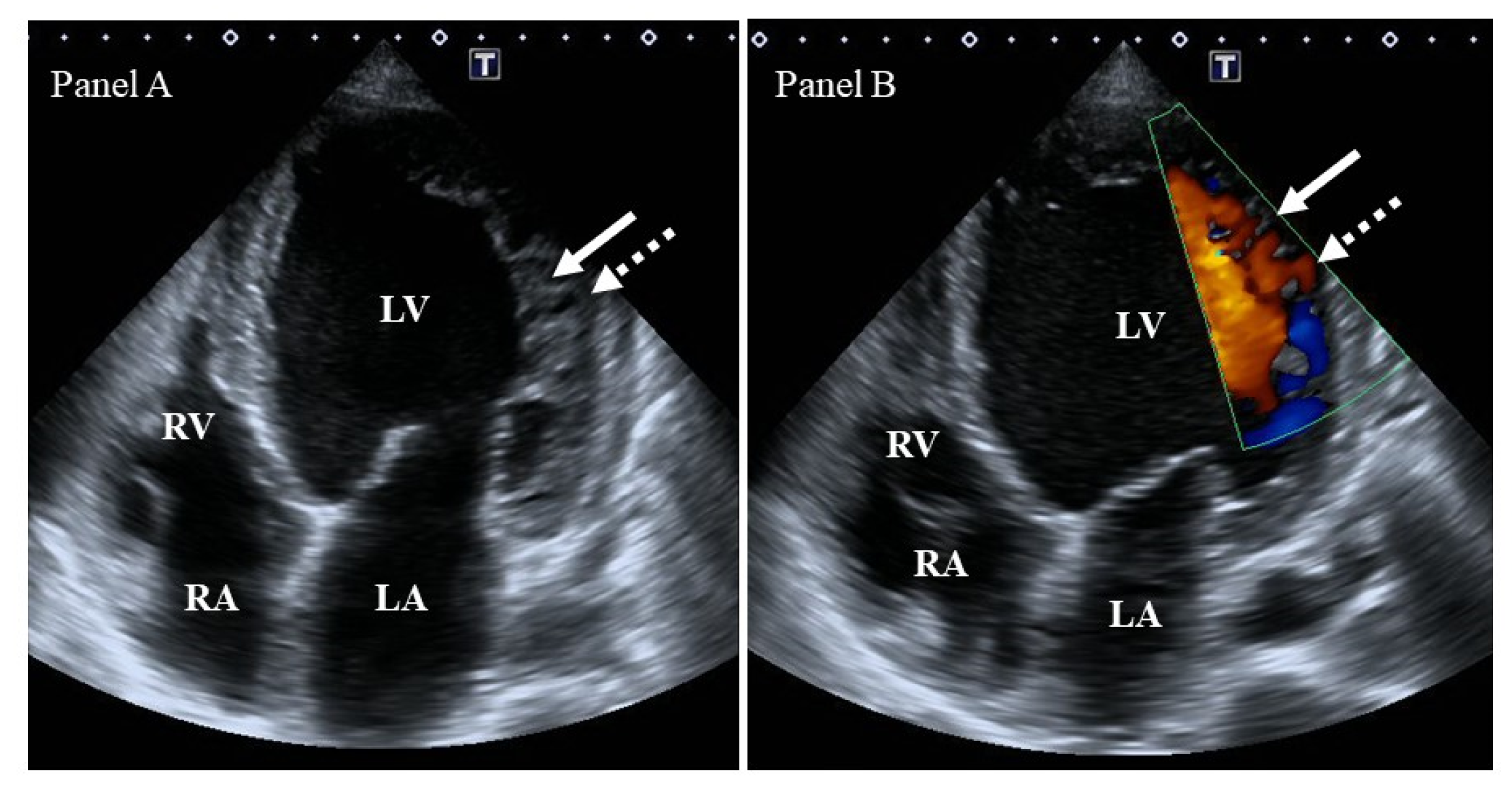
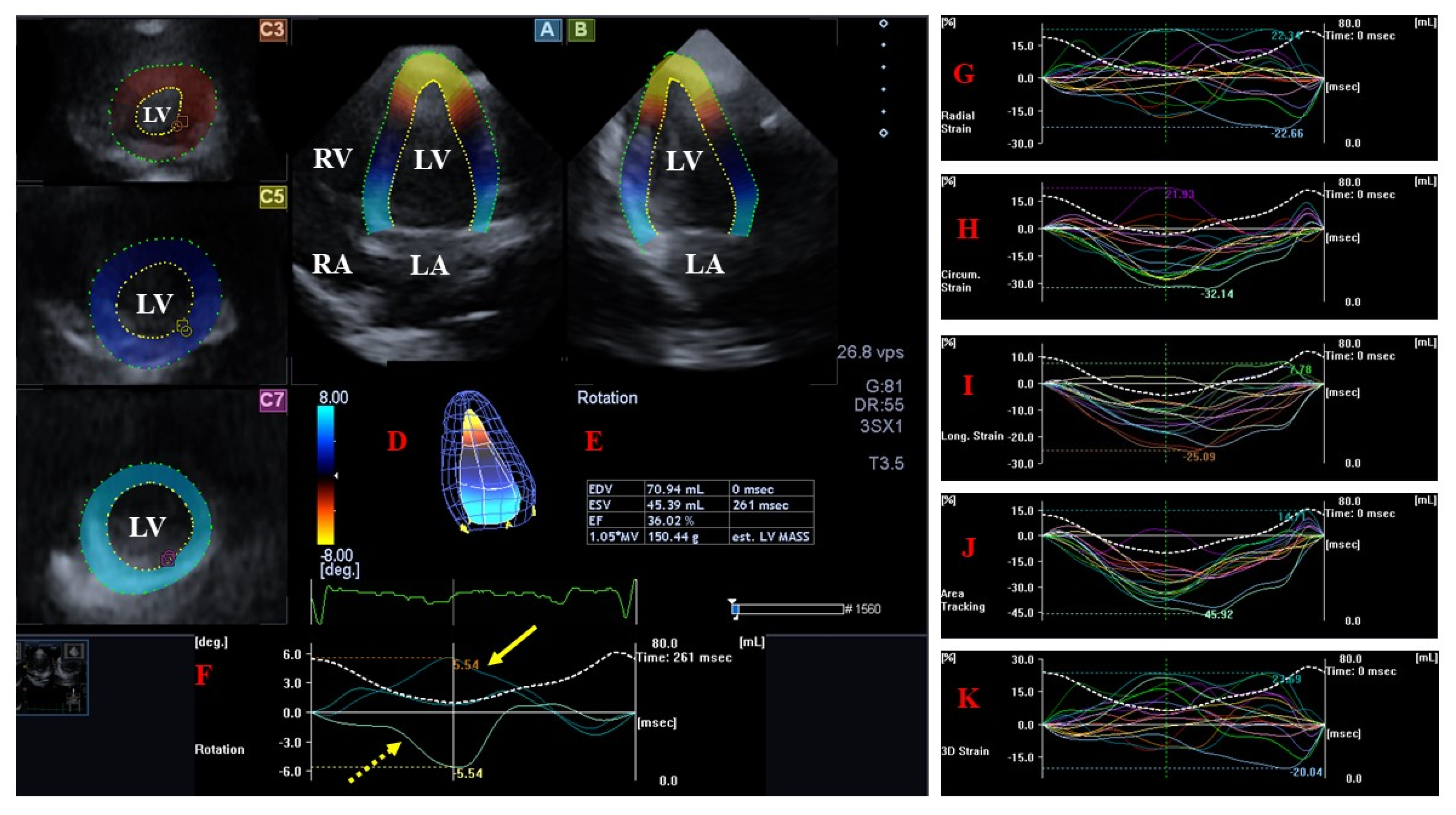
LV Rotational Mechanics
LV Rigid Body Rotation
3.2. Left Atrium
3.2.1. Under Healthy Circumstances
3.2.2. In Noncompaction Cardiomyopathy
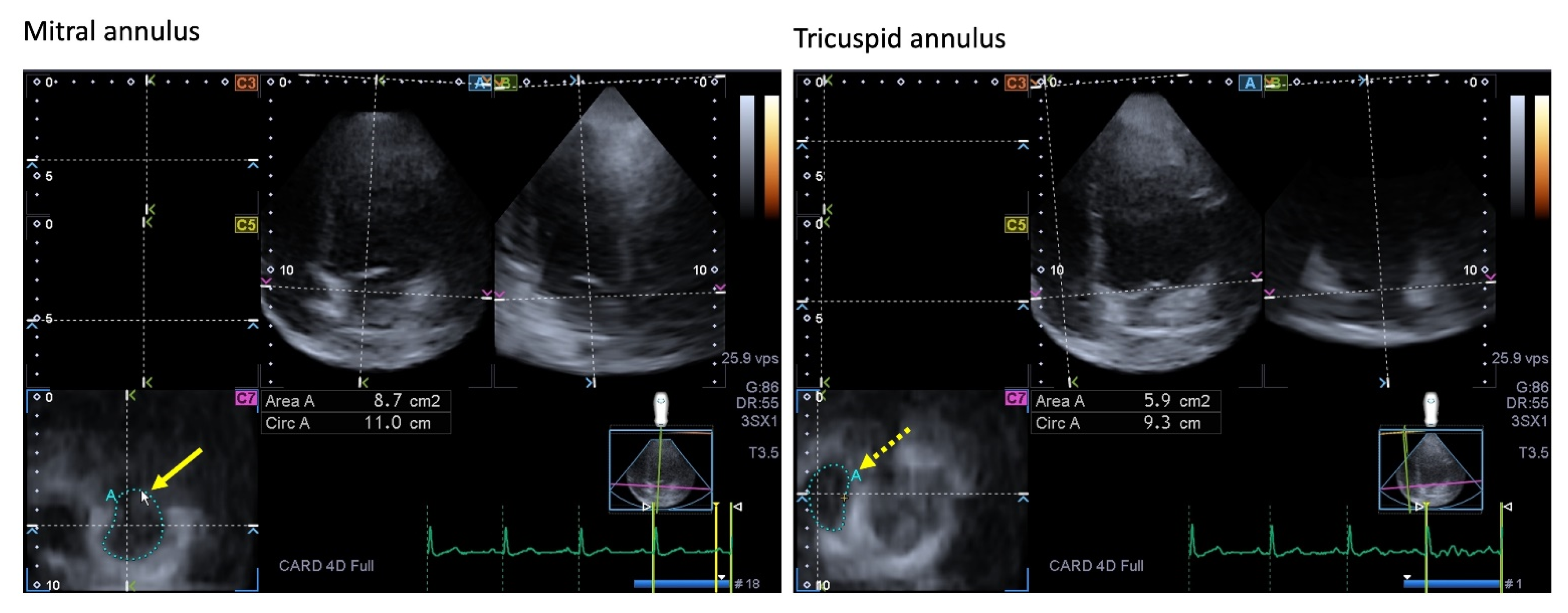
3.3. Mitral Valve
3.3.1. Under Healthy Circumstances
3.3.2. In Noncompaction Cardiomyopathy
3.4. Aortic Valve
3.4.1. Under Healthy Circumstances
3.4.2. In Noncompaction Cardiomyopathy
3.5. Aorta
3.5.1. Under Healthy Circumstances
3.5.2. In Noncompaction Cardiomyopathy
4. The Right Heart and the Pulmonary Artery
4.1. Right Ventricle
4.1.1. Under Healthy Circumstances
4.1.2. In Noncompaction Cardiomyopathy
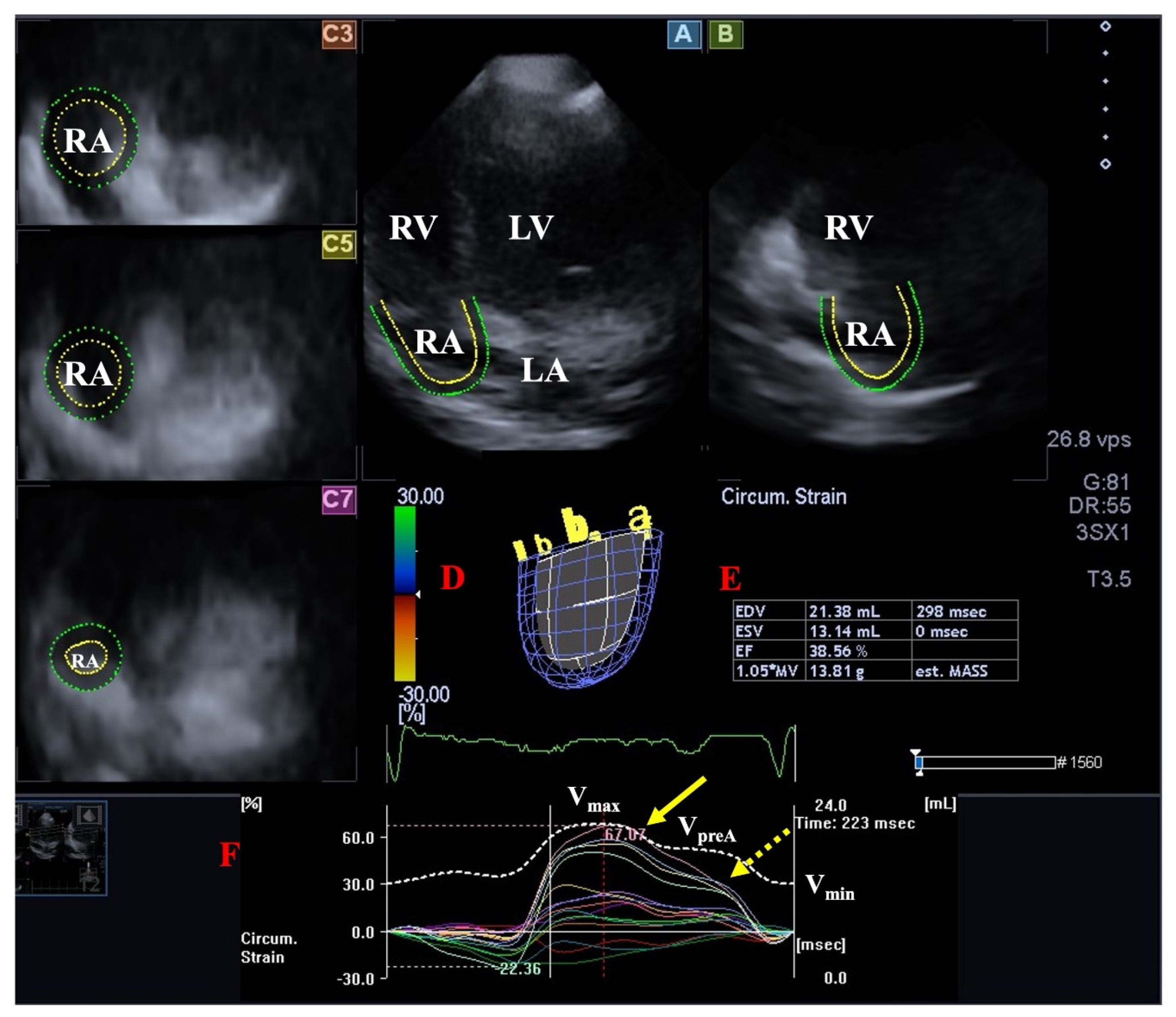
4.2. Right Atrium
4.2.1. Under Healthy Circumstances
4.2.2. In Noncompaction Cardiomyopathy
4.3. Tricuspid Valve
4.3.1. Under Healthy Circumstances
4.3.2. In Noncompaction Cardiomyopathy
4.4. Pulmonary Valve
4.4.1. Under Healthy Circumstances
4.4.2. In Noncompaction Cardiomyopathy
4.5. Pulmonary Artery
4.5.1. Under Healthy Circumstances
4.5.2. In Noncompaction Cardiomyopathy
5. Pathophysiologic Background
6. Clinical Implications
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, M. Mechanisms of Trabecular Formation and Specification During Cardiogenesis. Pediatr. Cardiol. 2018, 39, 1082–1089. [Google Scholar] [CrossRef]
- Engberding, R.; Bender, F. Identification of a rare congenital anomaly of the myocardium by two-dimensional echocardiography: Persistence of isolated myocardial sinusoids. Am. J. Cardiol. 1984, 53, 1733–1734. [Google Scholar] [CrossRef]
- Chin, T.K.; Perloff, J.K.; Williams, R.G.; Jue, K.; Mohrmann, R. Isolated noncompaction of left ventricular myocardium. A study of eight cases. Circulation 1990, 82, 507–513. [Google Scholar] [CrossRef]
- Jenni, R.; Oechslin, E.; Schneider, J.; Attenhofer Jost, C.; Kaufmann, P.A. Echocardiographic and pathoanatomical characteristics of isolated left ventricular noncompaction: A step towards classification as a distinct cardiomyopathy. Heart 2001, 86, 666–671. [Google Scholar] [CrossRef]
- Almeida, A.G.; Pinto, F.J. Non-compaction cardiomyopathy. Heart 2013, 99, 1535–1542. [Google Scholar] [CrossRef]
- Gomathi, S.B.; Makadia, N.; Ajit, S.M. An unusual case of isolated non-compacted right ventricular myocardium. Eur. J. Echocardiogr. 2008, 9, 424–425. [Google Scholar] [CrossRef]
- Vaikhanskaya, T.G.; Sivitskaya, L.N.; Kurushko, T.V.; Nizhnikava, O.G.; Levdanskiy, O.D.; Danilenko, N.G. Left ventricular noncompaction: A distinct cardiomyopathy or a composite anatomical syndrome? Kardiologiia 2018, 58, 33–45. [Google Scholar] [CrossRef]
- Zhu, X.; Ya, Y.; Hu, G. Left ventricular noncompaction in patients with coronary artery disease: Preliminary analysis of echocardiographic findings. J. Clin. Ultrasound 2018, 46, 475–479. [Google Scholar] [CrossRef]
- Rao, K.; Bhaskaran, A.; Choudhary, P.; Tan, T.C. The role of multimodality imaging in the diagnosis of left ventricular noncompaction. Eur. J. Clin. Investig. 2020, 50, e13254. [Google Scholar] [CrossRef]
- Stollberger, C.; Gerecke, B.; Finsterer, J.; Engberding, R. Refinement of echocardiographic criteria for left ventricular noncompaction. Int. J. Cardiol. 2013, 165, 463–467. [Google Scholar] [CrossRef]
- Petersen, S.E.; Selvanayagam, J.B.; Wiesmann, F.; Robson, M.D.; Francis, J.M.; Anderson, R.H.; Watkins, H.; Naubauer, S. Left ventricular non-compaction: Insights from cardiovascular magnetic resonance imaging. J. Am. Coll. Cardiol. 2005, 46, 101–105. [Google Scholar] [CrossRef]
- Jacquier, A.; Thuny, F.; Jop, B.; Giorgi, R.; Cohen, F.; Gaubert, J.Y.; Vidal, V.; Bartoli, J.M.; Habib, G.; Moulin, G. Measurement of trabeculated left ventricular mass using cardiac magnetic resonance imaging in the diagnosis of left ventricular non-compaction. Eur. Heart J. 2010, 31, 1098–1104. [Google Scholar] [CrossRef]
- Grothoff, M.; Pachowsky, M.; Hoffmann, J.; Posch, M.; Klaassen, S.; Lehmkuhl, L.; Gutberlet, M. Value of cardiovascular MR in diagnosing left ventricular non-compaction cardiomyopathy and in discriminating between other cardiomyopathies. Eur. Radiol. 2012, 22, 2699–2709. [Google Scholar] [CrossRef]
- Ammar, K.A.; Paterick, T.E.; Khandheria, B.K.; Jan, M.F.; Kramer, C.; Umland, M.M.; Tercius, A.J.; Baratta, L.; Tajik, A.J. Myocardial mechanics: Understanding and applying three-dimensional speckle tracking echocardiography in clinical practice. Echocardiography 2012, 97, 861–872. [Google Scholar] [CrossRef]
- Urbano-Moral, J.A.; Patel, A.R.; Maron, M.S.; Arias-Godinez, J.A.; Pandian, N.G. Three-dimensional speckle-tracking echocardiography: Methodological aspects and clinical potential. Echocardiography 2012, 29, 997–1010. [Google Scholar] [CrossRef]
- Muraru, D.; Niero, A.; Rodriguez-Zanella, H.; Cherata, D.; Badano, L. Three-dimensional speckle-tracking echocardiography: Benefits and limitations of integrating myocardial mechanics with three-dimensional imaging. Cardiovasc. Diagn. Ther. 2018, 8, 101–117. [Google Scholar] [CrossRef]
- Gao, L.; Lin, Y.; Ji, M.; Wu, W.; Li, H.; Qian, M.; Zhang, L.; Xie, M.; Li, Y. Clinical Utility of Three-Dimensional Speckle-Tracking Echocardiography in Heart Failure. J. Clin. Med. 2022, 11, 6307. [Google Scholar] [CrossRef]
- Nemes, A.; Rácz, G.; Kormányos, Á. Tricuspid Annular Abnormalities in Isolated Left Ventricular Non-compaction-Insights From the Three-dimensional Speckle-Tracking Echocardiographic MAGYAR-Path Study. Front. Cardiovasc. Med. 2022, 9, 694616. [Google Scholar] [CrossRef]
- Nemes, A.; Domsik, P.; Kalapos, A.; Gavallér, H.; Oszlánczi, M.; Forster, T. Right atrial deformation analysis in isolated left ventricular noncompaction–insights from the three-dimensional speckle tracking echocardiographic MAGYAR-Path Study. Rev. Port. Cardiol. 2016, 35, 515–521. [Google Scholar] [CrossRef]
- Nemes, A.; Piros, G.Á.; Domsik, P.; Kalapos, A.; Forster, T. Left Atrial Volumetric and Strain Analysis by Three-Dimensional Speckle-Tracking Echocardiography in Noncompaction Cardiomyopathy: Results from the MAGYAR-Path Study. Hell. J. Cardiol. 2016, 57, 23–29. [Google Scholar] [CrossRef]
- Nemes, A.; Hausinger, P.; Kalapos, A.; Domsik, P.; Forster, T. Alternative ways to assess left atrial function in noncompaction cardiomyopathy by three-dimensional speckle-tracking echocardiography: (a case from the MAGYAR-Path study). Int. J. Cardiol. 2012, 158, 105–107. [Google Scholar] [CrossRef]
- Kalapos, A.; Domsik, P.; Forster, T.; Nemes, A. Left ventricular strain reduction is not confined to the noncompacted segments in noncompaction cardiomyopathy-insights from the three-dimensional speckle tracking echocardiographic MAGYAR-Path Study. Echocardiography 2014, 31, 638–643. [Google Scholar] [CrossRef]
- Narang, A.; Addetia, K. An introduction to left ventricular strain. Curr. Opin. Cardiol. 2018, 33, 455–463. [Google Scholar] [CrossRef]
- Nakatani, S. Left ventricular rotation and twist: Why should we learn? J. Cardiovasc. Ultrasound 2011, 19, 1–6. [Google Scholar] [CrossRef]
- Sengupta, P.P.; Tajik, A.J.; Chandrasekaran, K.; Khandheria, B.K. Twist mechanics of the left ventricle: Principles and application. JACC Cardiovasc. Imaging. 2008, 1, 366–376. [Google Scholar] [CrossRef]
- He, T.; Zeng, H.S.; Le, W.B.; Li, X.H.; Lu, Z.Y. Clinical characterization and outcome of patients with noncompaction of ventricular myocardium. Zhonghua Xin Xue Guan Bing Za Zhi 2007, 35, 548–551. [Google Scholar]
- Tian, T.; Liu, Y.; Gao, L.; Wang, J.; Sun, K.; Zou, Y.; Wang, L.; Zhang, L.; Li, Y.; Xiao, Y.; et al. Isolated left ventricular noncompaction: Clinical profile and prognosis in 106 adult patients. Heart Vessel. 2014, 29, 645–652. [Google Scholar] [CrossRef]
- Peters, F.; Khandheria, B.K.; dos Santos, C.; Matioda, H.; Maharaj, N.; Libhaber, E.; Mamdoo, F.; Essop, M.R. Isolated left ventricular noncompaction in sub-Saharan Africa: A clinical and echocardiographic perspective. Circ. Cardiovasc. Imaging. 2012, 5, 187–193. [Google Scholar] [CrossRef]
- Oechslin, E.N.; Attenhofer Jost, C.H.; Rojas, J.R.; Kaufmann, P.A.; Jenni, R. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: A distinct cardiomyopathy with poor prognosis. J. Am. Coll. Cardiol. 2000, 36, 493–500. [Google Scholar] [CrossRef]
- Jenni, R.; Wyss, C.A.; Oechslin, E.N.; Kaufmann, P.A. Isolated ventricular noncompaction is associated with coronary microcirculatory dysfunction. J. Am. Coll. Cardiol. 2002, 39, 450–454. [Google Scholar] [CrossRef]
- Sengupta, P.P.; Mohan, J.C.; Mehta, V.; Jain, V.; Arora, R.; Pandian, N.G.; Khandheria, B.K. Comparison of echocardiographic features of noncompaction of the left ventricle in adults versus idiopathic dilated cardiomyopathy in adults. Am. J. Cardiol. 2004, 94, 389–391. [Google Scholar] [CrossRef]
- Nemes, A.; Caliskan, K.; Geleijnse, M.L.; Soliman, O.I.I.; Vletter, W.B.; ten Cate, F.J. Reduced regional systolic function is not confined to the noncompacted segments in noncompaction cardiomyopathy. Int. J. Cardiol. 2009, 134, 366–370. [Google Scholar] [CrossRef]
- Yousef, Z.R.; Foley, P.W.X.; Khadjooi, K.; Chalil, S.; Sandman, H.; Mohammed, N.U.H.; Leyva, F. Left ventricular non-compaction: Clinical features and cardiovascular magnetic resonance imaging. BMC Cardiovasc. Disord. 2009, 9, 37. [Google Scholar] [CrossRef]
- Lofiego, C.; Biagini, E.; Ferlito, M.; Pasquale, F.; Rocchi, G.; Perugini, E.; Leone, O.; Bracchetti, G.; Caliskan, K.; Branzi, A.; et al. Paradoxical contributions of non-compacted and compacted segments to global left ventricular dysfunction in isolated left ventricular noncompaction. Am. J. Cardiol. 2006, 97, 738–741. [Google Scholar] [CrossRef]
- Fazio, G.; Pipitone, S.; Iacona, M.A.; Marchì, S.; Mongiovì, M.; Zito, R.; Sutera, L.; Novo, G.; Novo, S. Evaluation of diastolic function by the tissue Doppler in children affected by non-compaction. Int. J. Cardiol. 2007, 116, 60–62. [Google Scholar] [CrossRef]
- Caliskan, K.; Soliman, O.I.; Nemes, A.; van Domburg, R.T.; Simoons, M.L.; Geleijnse, M.L. No relationship between left ventricular radial wall motion and longitudinal velocity and the extent and severity of noncompaction cardiomyopathy. Cardiovasc. Ultrasound 2012, 10, 9. [Google Scholar] [CrossRef]
- Guigui, S.A.; Horvath, S.A.; Arenas, I.A.; Mihos, C.G. Cardiac geometry, function and mechanics in left ventricular non-compaction cardiomyopathy with preserved ejection fraction. J. Echocardiogr. 2022, 20, 144–150. [Google Scholar] [CrossRef]
- Łuczak-Woźniak, K.; Werner, B. Left Ventricular Noncompaction-A Systematic Review of Risk Factors in the Pediatric Population. J. Clin. Med. 2021, 16, 1232. [Google Scholar] [CrossRef]
- Liu, J.; Li, Y.; Cui, Y.; Cao, Y.; Yao, S.; Zhou, X.; Wetzl, J.; Zeng, W.; Shi, H. Quantification of myocardial strain in patients with isolated left ventricular non-compaction and healthy subjects using deformable registration algorithm: Comparison with feature tracking. BMC Cardiovasc. Disord. 2020, 20, 400. [Google Scholar] [CrossRef]
- Yu, S.; Chen, X.; Yang, K.; Wang, J.; Zhao, K.; Dong, W.; Yan, W.; Su, G.; Zhano, S. Correlation between left ventricular fractal dimension and impaired strain assessed by cardiac MRI feature tracking in patients with left ventricular noncompaction and normal left ventricular ejection fraction. Eur. Radiol. 2022, 32, 2594–2603. [Google Scholar] [CrossRef]
- Cortés, M.; Oliva, M.R.; Orejas, M.; Navas, M.A.; Rábago, R.M.; Martínez, M.E.; Taibo, M.; Palfy, J.; Rey, M.; Farré, J. Usefulness of speckle myocardial imaging modalities for differential diagnosis of left ventricular noncompaction of the myocardium. Int. J. Cardiol. 2016, 223, 813–818. [Google Scholar] [CrossRef]
- Bellavia, D.; Michelena, H.I.; Martinez, M.; Pellikka, P.A.; Bruce, C.J.; Connolly, H.M.; Villarraga, H.R.; Veress, G.; Oh, J.K.; Miller, F.A. Speckle myocardial imaging modalities for early detection of myocardial impairment in isolated left ventricular non-compaction. Heart 2010, 96, 440–447. [Google Scholar] [CrossRef]
- Arenas, I.A.; Mihos, C.G.; DeFaria Yeh, D.; Yucel, E.; Elmahdy, H.M.; Santana, O. Echocardiographic and clinical markers of left ventricular ejection fraction and moderate or greater systolic dysfunction in left ventricular noncompaction cardiomyopathy. Echocardiography 2018, 35, 941–948. [Google Scholar] [CrossRef]
- Anwer, S.; Heiniger, P.S.; Rogler, S.; Erhart, L.; Cassani, D.; Kuzo, N.; Rebellius, L.; Schoenenberger-Berzins, R.; Schmid, D.; Nussbaum, S.; et al. Left ventricular mechanics and cardiovascular outcomes in non-compaction phenotype. Int. J. Cardiol. 2021, 336, 73–80. [Google Scholar] [CrossRef]
- Zhang, J.; Jiang, M.; Zheng, C.; Liu, H.; Guo, Y.; Yie, X.; Zhou, Z.; Zhou, X.; Xia, L.; Luo, M.; et al. Evaluation of isolated left ventricular noncompaction using cardiac magnetic resonance tissue tracking in global, regional and layer-specific strains. Sci. Rep. 2021, 11, 7183. [Google Scholar] [CrossRef]
- Visoiu, I.S.; Rimbas, R.C.; Nicula, A.I.; Mihaila-Baldea, S.; Magda, S.L.; Mihalcea, D.J.; Hayat, M.; Luchian, M.L.; Chitroceanu, A.M.; Vinereanu, D. Multimodality Imaging and Biomarker Approach to Characterize the Pathophysiology of Heart Failure in Left Ventricular Non-Compaction with Preserved Ejection Fraction. J. Clin. Med. 2023, 12, 3632. [Google Scholar] [CrossRef]
- Szűcs, A.; Kiss, A.R.; Gregor, Z.; Horváth, M.; Tóth, A.; Dohy, Z.; Szabó, L.E.; Suhai, F.I.; Merkely, B.; Vágó, H. Changes in strain parameters at different deterioration levels of left ventricular function: A cardiac magnetic resonance feature-tracking study of patients with left ventricular noncompaction. Int. J. Cardiol. 2021, 331, 124–130. [Google Scholar] [CrossRef]
- Qiu, Q.; Chen, Y.X.; Mai, J.T.; Yuan, W.L.; Wei, Y.L.; Liu, Y.M.; Yang, L.; Wang, J.F. Effects of cardiac resynchronization therapy on left ventricular remodeling and dyssynchrony in patients with left ventricular noncompaction and heart failure. Int. J. Cardiovasc. Imaging 2015, 31, 329–337. [Google Scholar] [CrossRef]
- Cerar, A.; Jaklic, M.; Frljak, S.; Poglajen, G.; Zemljic, G.; Salobir, B.G.; Novak, M.D.; Stalc, M.; Zbacnik, R.; Kozelj, M. Impairment of myocardial perfusion correlates with heart failure severity in patients with non-compaction cardiomyopathy. ESC Heart Fail. 2020, 7, 1161–1167. [Google Scholar] [CrossRef]
- Bogunovic, N.; Farr, M.; Pirl, L.; Faber, L.; van Buuren, F.; Rudolph, V.; Roder, F. Systolic longitudinal global and segmental myocardial mechanics in symptomatic isolated left ventricular non-compaction cardiomyopathy. Echocardiography 2021, 38, 555–567. [Google Scholar] [CrossRef]
- Gastl, M.; Gotschy, A.; Polacin, M.; Vishnevskiy, V.; Meyer, D.; Sokolska, J.; Tanner, F.C.; Alkadhi, H.; Kozerke, S.; Manka, R. Determinants of myocardial function characterized by CMR-derived strain parameters in left ventricular non-compaction cardiomyopathy. Sci. Rep. 2019, 9, 15882. [Google Scholar] [CrossRef] [PubMed]
- Huttin, O.; Venner, C.; Frikha, Z.; Voilliot, D.; Marie, P.Y.; Aliot, E.; Sadoul, N.; Juillière, Y.; Brembilla-Perrot, B.; Selton-Suty, C. Myocardial deformation pattern in left ventricular non-compaction: Comparison with dilated cardiomyopathy. Int. J. Cardiol. Heart Vasc. 2014, 5, 9–14. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Akhan, O.; Demir, E.; Dogdus, M.; Cakan, F.O.; Nalbantgil, S. Speckle tracking echocardiography and left ventricular twist mechanics: Predictive capabilities for noncompaction cardiomyopathy in the first degree relatives. Int. J. Cardiovasc. Imaging 2021, 37, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Li, S.; Sirajuddin, A.; Wu, W.; Huang, J.; Sun, X.; Zhao, S.; Pu, J.; Lu, M. CMR Characteristics, gene variants and long-term outcome in patients with left ventricular non-compaction cardiomyopathy. Insights Imaging 2021, 12, 184. [Google Scholar] [CrossRef] [PubMed]
- Kiss, A.R.; Gregor, Z.; Furák, A.; Tóth, A.; Horváth, M.; Szabó, L.; Czimbalmos, C.; Dohy, Z.; Merkely, B.; Vágó, H.; et al. Left ventricular characteristics of noncompaction phenotype patients with good ejection fraction measured with cardiac magnetic resonance. Anatol. J. Cardiol. 2021, 25, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Sarnecki, J.; Paszkowska, A.; Petryka-Mazurkiewicz, J.; Kubik, A.; Feber, J.; Jurkiewicz, E.; Ziółkowska, E. Left and Right Ventricular Morphology, Function and Myocardial Deformation in Children with Left Ventricular Non-Compaction Cardiomyopathy: A Case-Control Cardiovascular Magnetic Resonance Study. J. Clin. Med. 2022, 11, 1104. [Google Scholar] [CrossRef]
- Koh, C.; Hong, W.J.; Wong, S.J.; Cheung, Y.F. Systolic-diastolic coupling of myocardial deformation of the left ventricle in children with left ventricular noncompaction. Heart Vessels 2010, 25, 493–499. [Google Scholar] [CrossRef]
- Ari, M.E.; Cetin, I.I.; Kocabas, A.; Ekici, F.; Ceylan, O.; Surucu, M. Decreased Deformation in Asymptomatic Children with Isolated Left Ventricular Non-compaction and Normal Ejection Fraction. Pediatr. Cardiol. 2016, 37, 201–207. [Google Scholar] [CrossRef]
- Yubbu, P.; Nawaytou, H.M.; Calderon-Anyosa, R.; Banerjee, A. Diagnostic value of myocardial deformation pattern in children with noncompaction cardiomyopathy. Int. J. Cardiovasc. Imaging 2018, 34, 1529–1539. [Google Scholar] [CrossRef]
- Nucifora, G.; Raman, K.S.; Muser, D.; Shah, R.; Perry, R.; Ramli, K.A.A.; Selvanayagam, J.B. Cardiac magnetic resonance evaluation of left ventricular functional, morphological, and structural features in children and adolescents vs. young adults with isolated left ventricular non-compaction. Int. J. Cardiol. 2017, 246, 68–73. [Google Scholar] [CrossRef]
- Arunamata, A.; Stringer, J.; Balasubramanian, S.; Tacy, T.A.; Silverman, N.H.; Punn, R. Cardiac Segmental Strain Analysis in Pediatric Left Ventricular Noncompaction Cardiomyopathy. J. Am. Soc. Echocardiogr. 2019, 32, 763–773.e1. [Google Scholar] [CrossRef] [PubMed]
- Zheng, T.; Ma, X.; Li, S.; Ueda, T.; Wang, Z.; Lu, A.; Zhou, W.; Zou, H.; Zhao, L.; Gong, L. Value of Cardiac Magnetic Resonance Fractal Analysis Combined with Myocardial Strain in Discriminating Isolated Left Ventricular Noncompaction and Dilated Cardiomyopathy. J. Magn. Reson. Imaging 2019, 50, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Tarando, F.; Coisne, D.; Galli, E.; Rousseau, C.; Viera, F.; Bosseau, C.; Habib, G.; Lederlin, M.; Schnell, F.; Donal, E. Left ventricular non-compaction and idiopathic dilated cardiomyopathy: The significant diagnostic value of longitudinal strain. Int. J. Cardiovasc. Imaging 2017, 33, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Niemann, M.; Liu, D.; Hu, K.; Cikes, M.; Beer, M.; Herrmann, S.; Gaudron, P.D.; Hillenbrand, H.; Voelker, W.; Ertl, G.; et al. Echocardiographic quantification of regional deformation helps to distinguish isolated left ventricular non-compaction from dilated cardiomyopathy. Eur. J. Heart Fail. 2012, 14, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Gregor, Z.; Kiss, A.R.; Grebur, K.; Szabó, L.E.; Merkely, B.; Vágó, H.; Szűcs, A. MR-specific characteristics of left ventricular noncompaction and dilated cardiomyopathy. Int. J. Cardiol. 2022, 359, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Wu, J.; Hao, X.; Li, X. Value of cardiac magnetic resonance feature tracking technology in the differential diagnosis of isolated left ventricular noncompaction and dilated cardiomyopathy. Quant. Imaging Med. Surg. 2023, 13, 1453–1463. [Google Scholar] [CrossRef] [PubMed]
- Haland, T.F.; Saberniak, J.; Leren, I.S.; Edvardsen, T.; Haugaa, K.H. Echocardiographic comparison between left ventricular non-compaction and hypertrophic cardiomyopathy. Int. J. Cardiol. 2017, 228, 900–905. [Google Scholar] [CrossRef]
- Ashwal, A.J.; Mugula, S.R.; Samanth, J.; Paramasivam, G.; Nayak, K.; Padmakumar, R. Role of deformation imaging in left ventricular non-compaction and hypertrophic cardiomyopathy: An Indian perspective. Egypt. Heart J. 2020, 72, 6. [Google Scholar] [CrossRef]
- Zou, Q.; Xu, R.; Li, X.; Yu, H.Y.; Yang, Z.G.; Wang, Y.N.; Fan, H.M.; Guo, Y.K. The mitral regurgitation effects of cardiac structure and function in left ventricular noncompaction. Sci. Rep. 2021, 11, 4616. [Google Scholar] [CrossRef]
- Wang, J.X.; Li, X.; Xu, R.; Hou, R.L.; Yang, Z.G.; Zhou, Z.Q.; Wang, Y.N.; Guo, Y.K. Comparison of cardiovascular magnetic resonance features and clinical consequences in patients with left ventricular non-compaction with and without mitral regurgitation-a multi-institutional study of the retrospective cohort study. Cardiovasc. Diagn. Ther. 2022, 12, 241–252. [Google Scholar] [CrossRef]
- Dorobantu, D.M.; Radulescu, C.R.; Riding, N.; McClean, G.; de la Garza, M.S.; Abuli-LLuch, M.; Duarte, N.; Adamuz, M.C.; Ryding, D.; Perry, D.; et al. The use of 2-D speckle tracking echocardiography in assessing adolescent athletes with left ventricular hypertrabeculation meeting the criteria for left ventricular non-compaction cardiomyopathy. Int. J. Cardiol. 2023, 371, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Sabatino, J.; Di Salvo, G.; Krupickova, S.; Fraisse, A.; Prota, C.; Bucciarelli, V.; Josen, M.; Paredes, J.; Sirico, D.; Voges, I.; et al. Left Ventricular Twist Mechanics to Identify Left Ventricular Noncompaction in Childhood. Circ. Cardiovasc. Imaging 2019, 12, e007805. [Google Scholar] [CrossRef] [PubMed]
- Peters, F.; Khandheria, B.K.; Libhaber, E.; Maharaj, N.; Dos Santos, C.; Matioda, H.; Essop, M.R. Left ventricular twist in left ventricular noncompaction. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Van Dalen, B.M.; Caliskan, K.; Soliman, O.I.I.; Nemes, A.; Vletter, W.B.; Ten Cate, F.J.; Geleijnse, M.L. Left ventricular solid body rotation in non-compaction cardiomyopathy: A potential new objective and quantitative functional diagnostic criterion? Eur. J. Heart Fail. 2008, 10, 1088–1093. [Google Scholar] [CrossRef] [PubMed]
- Van Dalen, B.M.; Caliskan, K.; Soliman, O.I.I.; Kauer, F.; van der Zwaan, H.B.; Vletter, W.B.; van Kark, L.C.; Ten Cate, F.J.; Geleijnse, M.L. Diagnostic Value of Rigid Body Rotation in Noncompaction Cardiomyopathy. J. Am. Soc. Echocardiogr. 2011, 24, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Nawaytou, H.M.; Montero, A.E.; Yubbu, P.; Calderón-Anyosa, R.J.C.; Sato, T.; O’Connor, M.J.; Miller, K.D.; Ursell, P.C.; Hoffman, J.I.E.; Banerjee, A. A Preliminary Study of Left Ventricular Rotational Mechanics in Children with Noncompaction Cardiomyopathy: Do They Influence Ventricular Function? J. Am. Soc. Echocardiogr. 2018, 31, 951–961. [Google Scholar] [CrossRef] [PubMed]
- Peters, F.; Khandheria, B.K.; dos Santos, C.; Govender, S.; Botha, F.; Essop, M.R. Peripartum Cardiomyopathy Associated with Left Ventricular Noncompaction Phenotype and Reversible Rigid Body Rotation. Circ. Heart Fail. 2013, 6, e62–e63. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–270. [Google Scholar] [CrossRef]
- Hoit, B.D. Left atrial size and function: Role in prognosis. J. Am. Coll. Cardiol. 2014, 63, 493–505. [Google Scholar] [CrossRef]
- Badano, L.P.; Nour, A.; Muraru, D. Left atrium as a dynamic three-dimensional entity: Implications for echocardiographic assessment. Rev. Esp. Cardiol. 2013, 66, 1–4. [Google Scholar] [CrossRef]
- Xu, W.; Yang, Y.; Zhu, J.; Tan, J.; Wang, J.; Wang, L. Left Atrial Diameter and the Risk of Thromboembolism in Patients with Left Ventricular Noncompaction. J. Cardiovasc. Dev. Dis. 2022, 9, 426. [Google Scholar] [CrossRef]
- Nemes, A.; Anwar, A.M.; Caliskan, K.; Soliman, O.I.I.; van Dalen, B.M.; Geleijnse, M.L.; ten Cate, F.J. Evaluation of left atrial systolic function in noncompaction cardiomyopathy by real-time three-dimensional echocardiography. Int. J. Cardiovasc. Imaging 2008, 24, 237–242. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Han, P.L.; Shen, M.T.; Jiang, Y.; Jiang, Z.K.; Li, K.; Yang, Z.G. Prognostic Value of Left Atrial Reservoir Strain in Left Ventricular Myocardial Noncompaction: A 3.0 T Cardiac Magnetic Resonance Feature Tracking Study. J. Magn. Reson. Imaging 2023, 57, 559–575. [Google Scholar] [CrossRef] [PubMed]
- Dal-Bianco, J.P.; Levine, R.A. Anatomy of the mitral valve apparatus: Role of 2D and 3D echocardiography. Cardiol. Clin. 2013, 31, 151–164. [Google Scholar] [CrossRef] [PubMed]
- Silbiger, J.J.; Bazaz, R. The anatomic substrate of mitral annular contraction. Int. J. Cardiol. 2020, 306, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Mihaila, S.; Muraru, D.; Miglioranza, M.H.; Piasentini, E.; Peluso, D.; Cucchini, U.; Iliceto, S.; Vinereanu, D.; Badano, L.P. Normal mitral annulus dynamics and its relationships with left ventricular and left atrial function. Int. J. Cardiovasc. Imaging 2015, 31, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Nemes, A.; Anwar, A.M.; Caliskan, K.; Soliman, O.I.I.; van Dalen, B.M.; Geleijnse, M.L.; ten Cate, F.J. Non-compaction cardiomyopathy is associated with mitral annulus enlargement and functional impairment: A real-time three-dimensional echocardiographic study. J. Heart Valve Dis. 2008, 17, 31–35. [Google Scholar]
- Li, Q.; Miao, L.; Xia, L.; Abdelnasser, H.Y.; Zhang, F.; Lu, Y.; Nusrat, A.; Tabassum, M.; Li, J.; Wu, M. Left Ventricular Noncompaction Is Associated with Valvular Regurgitation and a Variety of Arrhythmias. J. Cardiovasc. Dev. Dis. 2022, 9, 49. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Zhang, D.; Lu, Y.T.; Zhou, Z.M.; Hu, Y.X.; Liu, X.C.; Qu, Y.; Liu, Y.X.; Liu, Y.X.; Zhou, X.L. Clinical characteristics and management of coexistent cardiomyopathy in patients with bicuspid aortic valve. J. Geriatr. Cardiol. 2023, 20, 205–213. [Google Scholar] [CrossRef]
- Jeong, H.; Shim, C.Y.; Kim, D.; Choi, J.Y.; Choi, K.U.; Lee, S.Y.; Hong, G.R.; Ha, J.W. Prevalence, Characteristics, and Clinical Significance of Concomitant Cardiomyopathies in Subjects with Bicuspid Aortic Valves. Yonsei Med. J. 2019, 60, 816–823. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Khandheria, B.K.; Paterick, T.E.; Treiber, S.C.; Bush, M.; Tajik, A.J. Left ventricular noncompaction in patients with bicuspid aortic valve. J. Am. Soc. Echocardiogr. 2013, 26, 1306–1313. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Capoulade, R.; Tastet, L.; Guzzetti, E.; Clavel, M.A.; Salaun, E.; Bédard, É.; Arsenault, M.; Chetaille, P.; Tizón-Marcos, H.; et al. Prevalence of left ventricle non-compaction criteria in adult patients with bicuspid aortic valve versus healthy control subjects. Open Heart 2018, 5, e000869. [Google Scholar] [CrossRef] [PubMed]
- Shim, C.Y. Arterial-cardiac interaction: The concept and implications. J. Cardiovasc. Ultrasound 2011, 19, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Belz, G.G. Elastic properties and Windkessel function of the human aorta. Cardiovasc. Drugs Ther. 1995, 9, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Tukker, M.; Leening, M.J.G.; Mohamedhoesein, S.; Vanmaele, A.L.A.; Caliskan, K. Prevalence and clinical correlates of ascending aortic dilatation in patients with noncompaction cardiomyopathy. Int. J. Cardiovasc. Imaging 2023, 39, 1687–1695. [Google Scholar] [CrossRef] [PubMed]
- Nemes, A.; Caliskan, K.; Geleijnse, M.L.; Soliman, O.I.I.; Anwar, A.M.; ten Cate, F.J. Alterations in aortic elasticity in noncompaction cardiomyopathy. Int. J. Cardiovasc. Imaging 2008, 24, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Foale, R.; Nihoyannopoulos, P.; McKenna, W.; Kleinebenne, A.; Nadazdin, A.; Rowland, E.; Smith, G. Echocardiographic measurement of the normal adult right ventricle. Br. Heart J. 1986, 56, 33–44. [Google Scholar] [CrossRef]
- Ho, S.Y.; Nihoyannopoulos, P. Anatomy, echocardiography, and normal right ventricular dimensions. Heart 2006, 92 (Suppl. 1), i2–i13. [Google Scholar] [CrossRef]
- Haddad, F.; Hunt, S.A.; Rosenthal, D.N.; Murphy, D.J. Right ventricular function in cardiovascular disease, Part I. Anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation 2008, 117, 1436–1448. [Google Scholar] [CrossRef]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar] [PubMed]
- Stacey, R.B.; Andersen, M.; Haag, J.; Hall, M.E.; McLeod, G.; Upadhya, B.; Hundley, W.G.; Thohan, V. Right ventricular morphology and systolic function in left ventricular noncompaction cardiomyopathy. Am. J. Cardiol. 2014, 113, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Nucifora, G.; Aquaro, G.D.; Masci, P.G.; Pingitore, A.; Lombardi, M. Magnetic resonance assessment of prevalence and correlates of right ventricular abnormalities in isolated left ventricular noncompaction. Am. J. Cardiol. 2014, 113, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Stämpfli, S.F.; Gotschy, A.; Kiarostami, P.; Özkartal, T.; Gruner, C.; Niemann, M.; Manka, R.; Tanner, F.C. Right ventricular involvement in left ventricular non-compaction cardiomyopathy. Cardiol. J. 2022, 29, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Gregor, Z.; Kiss, A.R.; Grebur, K.; Dohy, Z.; Kovács, A.; Merkely, B.; Vágó, H.; Szűcs, A. Characteristics of the right ventricle in left ventricular noncompaction with reduced ejection fraction in the light of dilated cardiomyopathy. PLoS ONE 2023, 18, e0290981. [Google Scholar] [CrossRef] [PubMed]
- Kiss, A.R.; Gregor, Z.; Popovics, A.; Grebur, K.; Szabó, L.E.; Dohy, Z.; Kovács, A.; Lakatos, B.K.; Merkely, B.; Vágó, H.; et al. Impact of Right Ventricular Trabeculation on Right Ventricular Function in Patients with Left Ventricular Non-compaction Phenotype. Front. Cardiovasc. Med. 2022, 9, 843952. [Google Scholar] [CrossRef] [PubMed]
- Leung, S.W.; Elayi, C.S.; Charnigo Jr, R.J.; Syed, M.A. Clinical significance of right ventricular dysfunction in left ventricular non-compaction cardiomyopathy. Int. J. Cardiovasc. Imaging 2012, 28, 1123–1131. [Google Scholar] [CrossRef]
- Wang, W.; Chen, W.; Lin, X.; Fang, L. Influence of Right Ventricular Dysfunction on Outcomes of Left Ventricular Non-compaction Cardiomyopathy. Front. Cardiovasc. Med. 2022, 9, 816404. [Google Scholar] [CrossRef]
- Tadic, M. The right atrium, a forgotten cardiac chamber: An updated review of multimodality imaging. J. Clin. Ultrasound 2015, 43, 335–345. [Google Scholar] [CrossRef]
- Dahou, A.; Levin, D.; Reisman, M.; Hahn, R.T. Anatomy and physiology of the tricuspid valve. JACC Cardiovasc. Imaging 2019, 12, 458–468. [Google Scholar] [CrossRef]
- Kivelitz, D.E.; Dohmen, P.M.; Lembcke, A.; Kroencke, T.J.; Klingebiel, R.; Hamm, B.; Konertz, W.; Taupitz, M. Visualization of the pulmonary valve using cine MR imaging. Acta Radiol. 2003, 44, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Hirono, K.; Ichida, F. Left ventricular noncompaction: A disorder with genotypic and phenotypic heterogeneity-a narrative review. Cardiovasc. Diagn. Ther. 2022, 12, 495–515. [Google Scholar] [CrossRef] [PubMed]
- van Waning, J.I.; Moesker, J.; Heijsman, D.; Boersma, E.; Majoor-Krakauer, D. Systematic Review of Genotype-Phenotype Correlations in Noncompaction Cardiomyopathy. J. Am. Heart. Assoc. 2019, 8, e012993. [Google Scholar] [CrossRef] [PubMed]
- Marakhonov, A.V.; Brodehl, A.; Myasnikov, R.P.; Sparber, P.A.; Kiseleva, A.V.; Kulikova, O.V.; Meshkov, A.N.; Zharikova, A.A.; Koretsky, S.N.; Kharlap, M.S.; et al. Noncompaction cardiomyopathy is caused by a novel in-frame desmin (DES) deletion mutation within the 1A coiled-coil rod segment leading to a severe filament assembly defect. Hum. Mutat. 2019, 40, 734–741. [Google Scholar] [CrossRef]
- Kulikova, O.; Brodehl, A.; Kiseleva, A.; Myasnikov, R.; Meshkov, A.; Stanasiuk, C.; Gärtner, A.; Divashuk, M.; Sotnikova, E.; Koretskiy, S.; et al. The Desmin (DES) Mutation p.A337P Is Associated with Left-Ventricular Non-Compaction Cardiomyopathy. Genes 2021, 12, 121. [Google Scholar] [CrossRef]
- My, I.; Di Pasquale, E. Genetic Cardiomyopathies: The Lesson Learned from hiPSCs. J. Clin. Med. 2021, 10, 1149. [Google Scholar] [CrossRef]
- Purevjav, E.; Chintanaphol, M.; Orgil, B.O.; Alberson, N.R.; Towbin, J.A. Left ventricular noncompaction cardiomyopathy: From clinical features to animal modeling. In Preclinical Animal Modeling in Medicine, 1st ed.; Purevjav, E., Pierre, J.F., Lu, L., Eds.; IntechOpen: London, UK, 2022. [Google Scholar]

| Reference Number | Number of LVNC/NCCM pts in the Current Study | ||
|---|---|---|---|
| LEFT HEART | |||
| Left ventricle | Hypokinesis was observed in both noncompacted and compacted segments. | [26] | 18 |
| Most patients had systolic dysfunction, which is a predictor of outcome. | [27] | 106 | |
| Common sites of noncompaction were the apical, midinferior, and midlateral LV regions. | [28] | 54 | |
| The wall motion score index was markedly abnormal in the compacted LV segments and significantly less abnormal compared to the noncompacted segments. | [32] | 17 | |
| Noncompacted and compacted LV segments had comparable increased regional volumes and reduced systolic function: Systolic LV dysfunction was not confined to the noncompacted LV segments. | [32] | 17 | |
| All LV strains were decreased in all segments and LV-RS and LV-3DS showed further reduction in noncompacted segments compared to compacted segments. | [22] * | 9 | |
| Compared with controls, patients with preserved LV-EF had a larger mass, more abnormal LV geometry, and decreased global LV-LS. | [37] | 17 | |
| Global LV-LS was reduced regardless of LV-EF. | [41] | 28 | |
| Myocardial strain reduction was more significant in patients with focal myocardial fibrosis. | [45] | 63 | |
| Carriers of multiple genetic variants had a lower LV-EF and cardiac index, increased LV fibrosis, and reduced global LV-CS. | [54] | 28 | |
| Several strain abnormalities were seen even in children with LVNC. | [56] | 16 | |
| Certain strain parameters differed between LVNC and other cardiomyopathies. | [62] | 35 | |
| LV twist was reduced. | [72] | 47 | |
| There was a decreasing pattern in LV rotation values in patients’ relatives. | [53] | 32 pts and 30 relatives | |
| There was no difference in the LV rotational pattern between dilated cardiomyopathy and LVNC. | [65] | 42 | |
| LV-RBR had high specificity and sensitivity in differentiating NCCM from LV hypertrabeculation. | [75] | 52 pts with hypertrabeculation from which 34 proved to be NCCM | |
| Patients with LV-RBR showed worse NYHA functional status. | [73] | 60 | |
| Patients with lower LV-EF had higher rates of LV-RBR. | [47] | 31 | |
| Patients with clockwise LV-RBR had lower LV-LS but similar LV-EF. | [76] | 28 | |
| LV-RBR was present in 26–100% of patients and in most cases was oriented clockwise. | [74] | 10 | |
| Left atrium | There were signs of LA remodeling. | [37] | 17 |
| LA dimensions and volumes were larger. | [81] | 320 | |
| LA ejection force was increased. | [82] | 17 | |
| LA emptying fractions were smaller and certain peak global LA strains were reduced. | [20] * | 12 | |
| LA reservoir strain was an independent predictor of events. | [83] | 95 | |
| In the presence of a positive genotype, LA parameters were worse. | [54] | 28 | |
| Mitral valve | MA was dilated and functionally impaired. | [87] | 20 |
| The prevalence and grades of MV regurgitation were higher. | [88] | 45 | |
| Aortic valve | Patients with bicuspid aortic valve did not harbour more LVNC and there was no evidence that they are at higher risk for the development of LVNC. | [93] | 8, 49, 43 |
| Patients showed a higher ratio of AV regurgitation. | [88] | 45 | |
| Aorta | The prevalence of ascending aortic dilation was low. | [96] | 109 |
| Aortic stiffness was increased with no dilation but there was a reduced pulsatile change in diameter. | [97] | 20 | |
| RIGHT HEART | |||
| Right ventricle | RV apical trabecular thickness was greater. | [102] | 105 |
| RV systolic dysfunction | [103] | 56 | |
| RV myocardium displayed more trabeculations. | [104] | 20 | |
| Subclinical impairment of RV myocardial deformation | [56] | 16 | |
| Right atrium | RA volumes and certain stroke volumes were increased without RA strain abnormalities. | [19] * | 13 |
| Tricuspid valve | TA was dilated, with preserved sphincter-like function. | [18] * | 21 |
| The prevalence and grade of TV regurgitation were higher. | [88] | 45 | |
| Pulmonary valve | A low rate of patients showed pulmonary regurgitation. | [88] | 45 |
| Pulmonary artery | A high rate of patients had pulmonary hypertension. | [28] | 54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nemes, A. Myocardial Mechanics and Associated Valvular and Vascular Abnormalities in Left Ventricular Noncompaction Cardiomyopathy. J. Clin. Med. 2024, 13, 78. https://doi.org/10.3390/jcm13010078
Nemes A. Myocardial Mechanics and Associated Valvular and Vascular Abnormalities in Left Ventricular Noncompaction Cardiomyopathy. Journal of Clinical Medicine. 2024; 13(1):78. https://doi.org/10.3390/jcm13010078
Chicago/Turabian StyleNemes, Attila. 2024. "Myocardial Mechanics and Associated Valvular and Vascular Abnormalities in Left Ventricular Noncompaction Cardiomyopathy" Journal of Clinical Medicine 13, no. 1: 78. https://doi.org/10.3390/jcm13010078
APA StyleNemes, A. (2024). Myocardial Mechanics and Associated Valvular and Vascular Abnormalities in Left Ventricular Noncompaction Cardiomyopathy. Journal of Clinical Medicine, 13(1), 78. https://doi.org/10.3390/jcm13010078







