Virtual Care in Nephrology: An In-Depth Retrospective Analysis of Outcomes Using the Reset Kidney Health Model
Abstract
:1. Introduction
1.1. Background and Rationale
1.2. The Reset Kidney Health Model
2. Materials and Methods
2.1. Study Design
2.2. Error Margin and Interpretation
- Variability in Serum Creatinine: Serum creatinine levels may vary in individuals due to factors such as muscle mass, diet, and hydration status.
- Laboratory Measurement Variations: Different laboratories may use distinct methods or equipment to measure serum creatinine, leading to slight variations in serum creatinine results.
- Limitations of the Formulas: The formulas used to calculate eGFR (like the MDRD Study equation or the CKD-EPI equation) are based on population averages and may not be accurate for individual patients, especially those who are very young, very old, extremely overweight or underweight, or have unusual muscle mass.
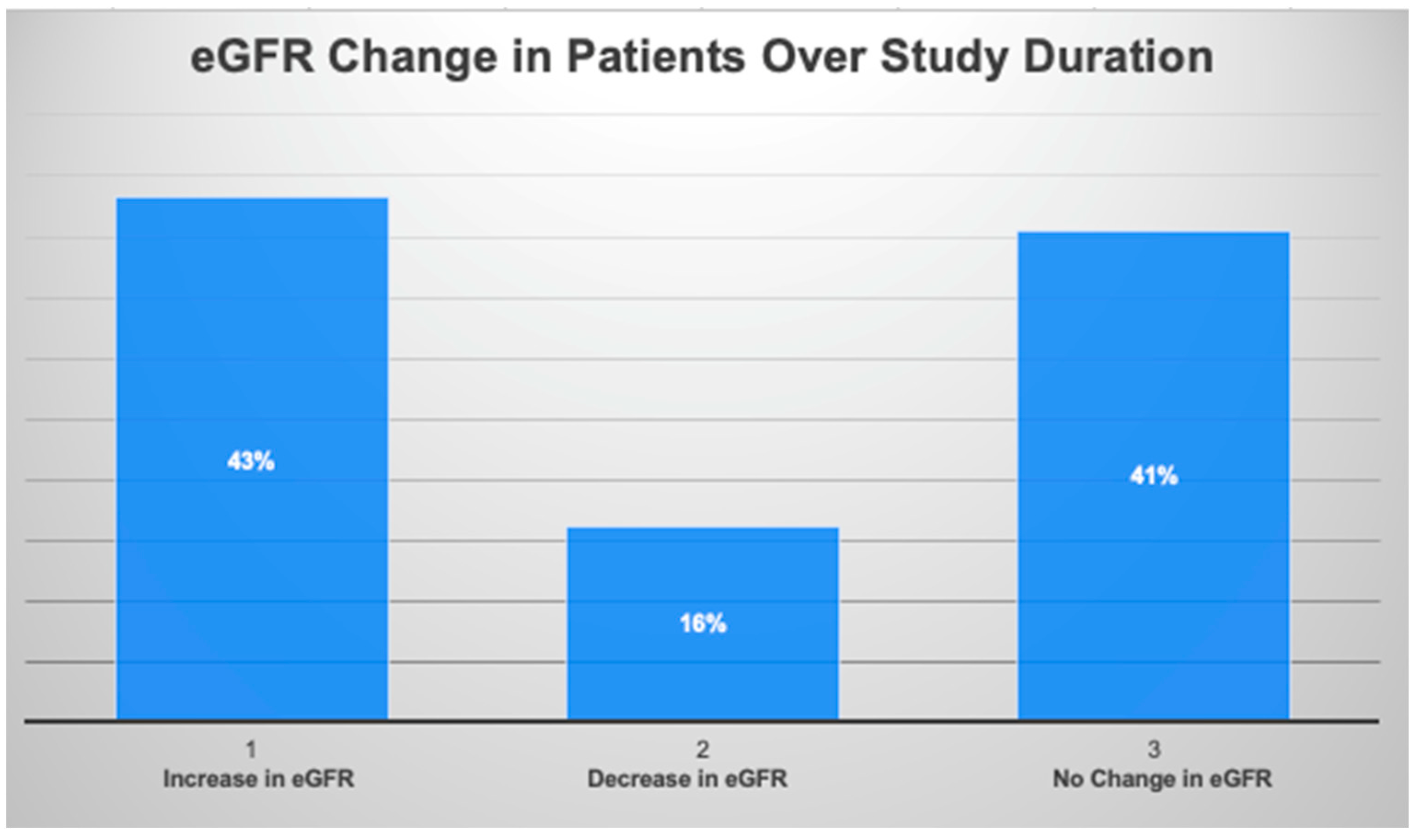
2.3. Categories of Estimated Glomerular Filtration Rate (eGFR) Changes
2.4. Intervention Framework
3. Results
4. Discussion
4.1. Reset Kidney Health Model
4.2. Positive Trends
4.3. Summary and Implications
4.4. Clinical Implications
4.5. Limitations and Future Research
4.6. Plans for Continued Study
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.-M.; Yang, C.-W. Chronic kidney disease: Global dimension and perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, B.W.; Morgenstern, H.; Hedgeman, E.; Tilea, A.; Scholz, N.; Shearon, T.; Burrows, N.R.; Shahinian, V.B.; Yee, J.; Plantinga, L.; et al. Nephrology care prior to end-stage renal disease and outcomes among new ESRD patients in the USA. Clin. Kidney J. 2015, 8, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Hassan, R.; Akbari, A.; Brown, P.A.; Hiremath, S.; Brimble, K.S.; Molnar, A.O. Risk Factors for Unplanned Dialysis Initiation: A Systematic Review of the Literature. Can. J. Kidney Health Dis. 2019, 6, 2054358119831684. [Google Scholar] [CrossRef] [PubMed]
- Rettig, R.; Vargas, R.; Norris, K.; Nissenson, A. A “Quiet Revolution” in Nephrology: Challenges and Opportunities for Advancing the Treatment of Chronic Kidney Disease; Rand Corporation: Santa Monica, CA, USA, 2010; pp. 1–4. [Google Scholar]
- Agrawal, V.; Jaar, B.G.; Frisby, X.Y.; Chen, S.-C.; Qiu, Y.; Li, S.; Whaley-Connell, A.T.; McCullough, P.A.; Bomback, A.S. Access to Health Care Among Adults Evaluated for CKD: Findings from the Kidney Early Evaluation Program (KEEP). Am. J. Kidney Dis. 2012, 59, S5–S15. [Google Scholar] [CrossRef] [PubMed]
- Golestaneh, L.; Alvarez, P.J.; Reaven, N.L.; Funk, S.E.; McGaughey, K.J.; Romero, A.; Brenner, M.S.; Onuigbo, M. All-Cause costs Increase Exponentially with Increased Chronic Kidney Disease Stage. Am. J. Manag. Care 2017, 23 (Suppl. S10), S163–S172. [Google Scholar] [PubMed]
- Trivedi, H.S.; Pang, M.M.; Campbell, A.; Saab, P. Slowing the progression of chronic renal failure: Economic benefits and patients’ perspectives. Am. J. Kidney Dis. 2002, 39, 721–729. [Google Scholar] [CrossRef] [PubMed]
- Naber, T.; Purohit, S. Chronic Kidney Disease: Role of Diet for a Reduction in the Severity of the Disease. Nutrients 2021, 13, 3277. [Google Scholar] [CrossRef] [PubMed]
- Rowe, C.; Sitch, A.J.; Barratt, J.; Brettell, E.A.; Cockwell, P.; Dalton, R.N.; Deeks, J.J.; Eaglestone, G.; Pellatt-Higgins, T.; Kalra, P.A.; et al. Biological variation of measured and estimated glomerular filtration rate in patients with chronic kidney disease. Kidney Int. 2019, 96, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Inker, L.A.; Heerspink, H.J.L.; Tighiouart, H.; Levey, A.S.; Coresh, J.; Gansevoort, R.T.; Simon, A.L.; Ying, J.; Beck, G.J.; Wanner, C.; et al. GFR Slope as a Surrogate End Point for Kidney Disease Progression in Clinical Trials: A Meta-Analysis of Treatment Effects of Randomized Controlled Trials. J. Am. Soc. Nephrol. 2019, 30, 1735–1745. [Google Scholar] [CrossRef] [PubMed]
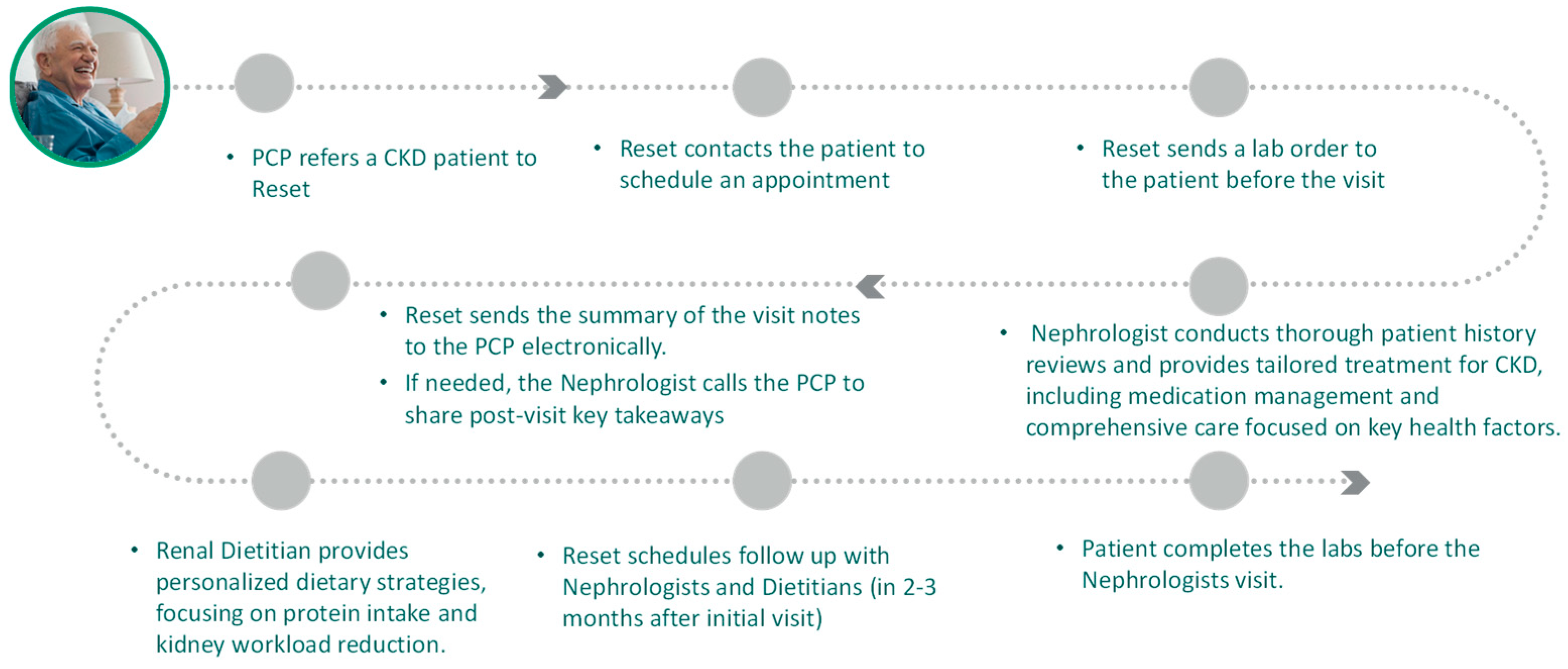
| Key Features | Overview |
|---|---|
| Provides patients with the ability to secure a virtual appointment with a nephrologist within 5–10 business days. |
| Patients are offered supplemental care from a renal dietitian, focusing on the adoption of a kidney-friendly diet. |
| Reset’s nephrologists adhere to a comprehensive checklist that aligns with evidence-based clinical protocols. To slow CKD progression, the patient is prescribed SGLT 2 inhibitors, ACE inhibitor/ARBs, and Finerenone as indicated. The Reset Kidney Health care model also focuses on blood pressure monitoring, glycemic control, statin therapy, and NSAID avoidance. |
| Reset Kidney Health care providers are dedicated to establishing early and trusted relationships with their patients through empathy and shared decision-making. Reset Kidney Health fosters robust patient engagement, ensuring that each patient is confident in their understanding of their disease and the care they can provide. |
| Reset collaborates closely with the patient’s PCP to ensure seamless, comprehensive care. |
| Stable eGFR | If a subsequent estimated Glomerular Filtration Rate (eGFR) measurement falls within the range established by the baseline (±2 mL/min/1.73 m²), it is classified as a stable GFR. For example, if the baseline eGFR is 24 mL/min/1.73 m² (range of 22 to 26 mL/min/1.73 m²), and a subsequent eGFR measurement is 25 mL/min/1.73 m², that value would be evaluated against the initial value with a standard error range of ±2 mL/min/1.73 m². Because 25 mL/min/1.73 m² falls between 22 and 26 mL/min/1.73 m², the patient’s eGFR would be considered stable between the two visits. |
| Increase in eGFR: | Any rise in the eGFR value by more than 2 mL/min/1.73 m² beyond the baseline range’s upper limit is considered an eGFR increase. |
| Reduction in eGFR: | Conversely, any decline in eGFR value by more than 2 mL/min/1.73 m² below the lower limit of the baseline range will be interpreted as a reduction in eGFR. |
| Factors | Intervention Group (n = 37) |
|---|---|
| Mean Age | 70 years |
| Gender | |
| 78% |
| 22% |
| Race Breakdown | |
| 14% |
| 3% |
| 84% |
| Dietician Recommendation Accepted | 23 |
| Mean Length of Treatment | 114 days |
| Factors | Intervention Group (n = 37) |
|---|---|
| The baseline mean of eGFR | 37.69 |
| Mean eGFR at Q3 | 40.79 |
| Mean eGFR difference from baseline | +3.09 |
| Baseline CKD Stage | |
| 9 |
| 19 |
| 9 |
| 0 |
| Last Observable CKD Staging | |
| 3 |
| 11 |
| 16 |
| 7 |
| 0 |
| Changes in CKD Stage | |
| 11 |
| 1 |
| 25 |
| Mean BP/S | |
| 135.0 |
| 136.2 |
| 133.9 |
| Mean BP/D | |
| 76.4 |
| 75.2 |
| 77.7 |
| Average A1C | |
| 6.6 |
| 6.6 |
| 6.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fritz, B.A. Virtual Care in Nephrology: An In-Depth Retrospective Analysis of Outcomes Using the Reset Kidney Health Model. J. Clin. Med. 2024, 13, 66. https://doi.org/10.3390/jcm13010066
Fritz BA. Virtual Care in Nephrology: An In-Depth Retrospective Analysis of Outcomes Using the Reset Kidney Health Model. Journal of Clinical Medicine. 2024; 13(1):66. https://doi.org/10.3390/jcm13010066
Chicago/Turabian StyleFritz, Benjamin A. 2024. "Virtual Care in Nephrology: An In-Depth Retrospective Analysis of Outcomes Using the Reset Kidney Health Model" Journal of Clinical Medicine 13, no. 1: 66. https://doi.org/10.3390/jcm13010066
APA StyleFritz, B. A. (2024). Virtual Care in Nephrology: An In-Depth Retrospective Analysis of Outcomes Using the Reset Kidney Health Model. Journal of Clinical Medicine, 13(1), 66. https://doi.org/10.3390/jcm13010066




