Clean Intermittent Catheterization in Children under 12 Years Does Not Have a Negative Impact on Long-Term Graft Survival following Pediatric Kidney Transplantation
Abstract
1. Introduction
2. Materials and Methods
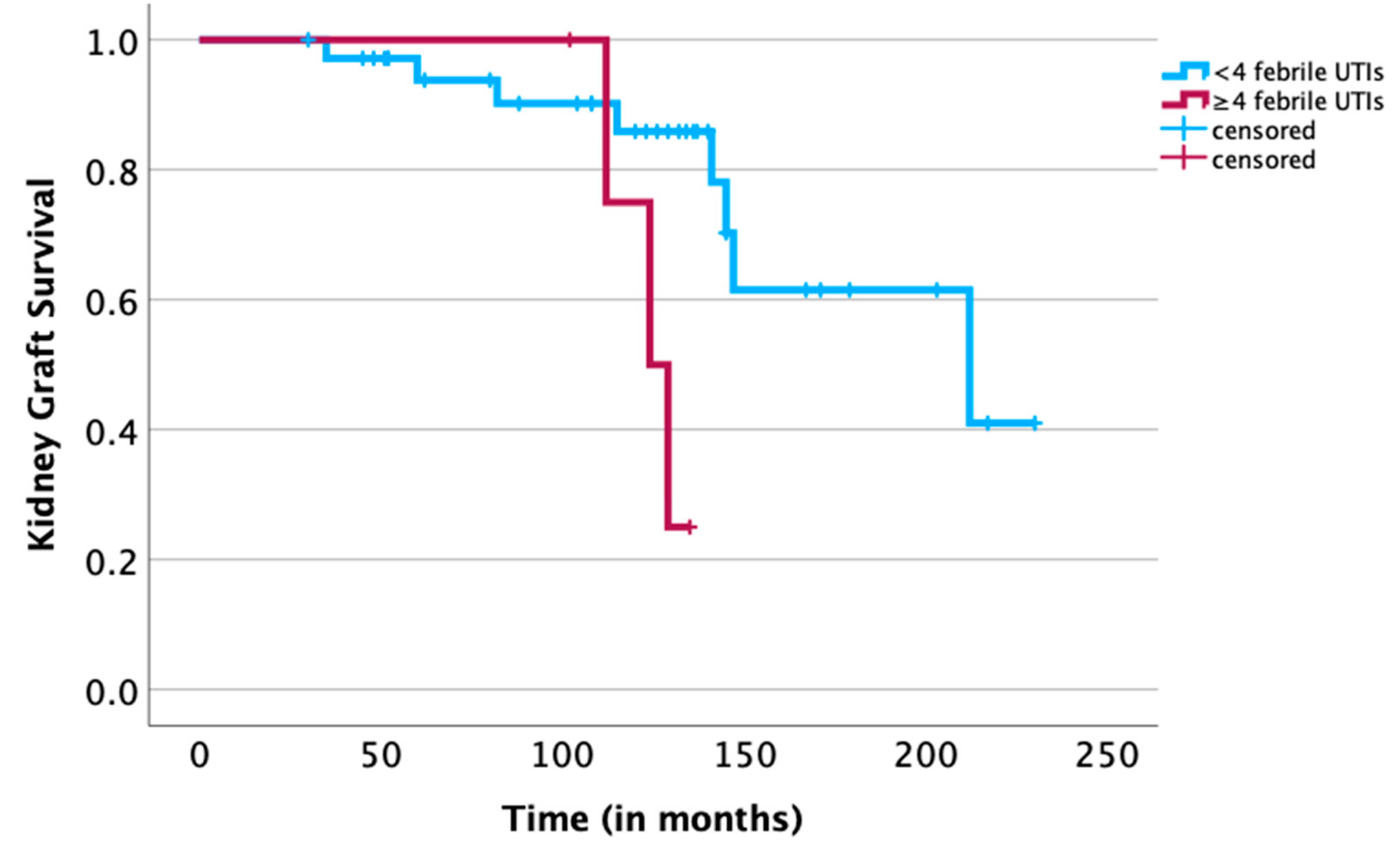
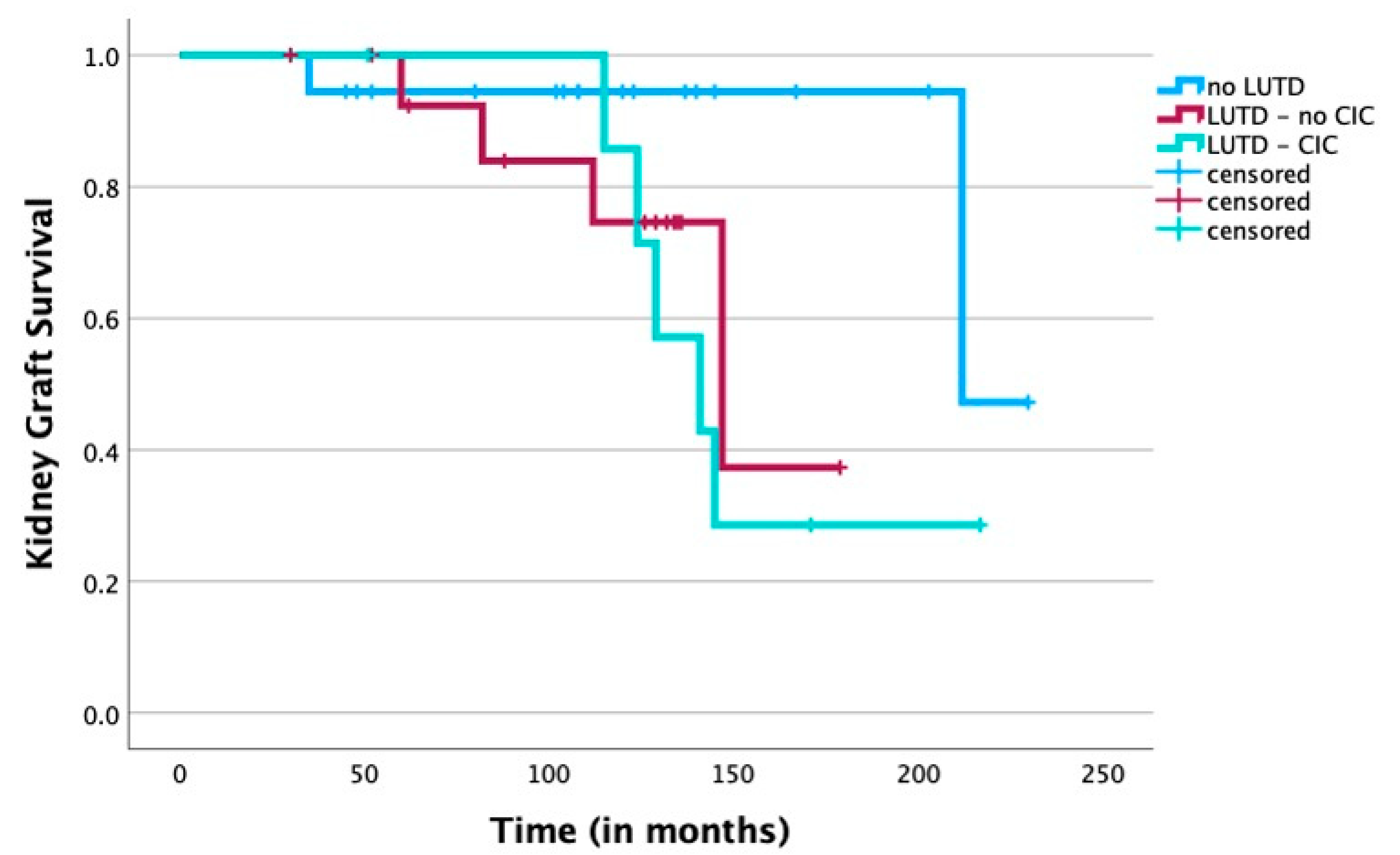
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dharnidharka, V.R.; Fiorina, P.; Harmon, W.E. Kidney transplantation in children. N. Engl. J. Med. 2014, 371, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Hussein, A.A.; Shoukry, A.I.; Fadel, F.; Morsi, H.A.; Hussein, H.A.; Sheba, M.; El-Khateeb, N.; Abou-El Ela, W.; El-Sheemy, M.; Daw, K.; et al. Outcome of pediatric renal transplantation in urological versus non-urological causes of end stage renal disease: Does it matter? J. Pediatr. Urol. 2018, 14, 166.e161–166.e167. [Google Scholar] [CrossRef] [PubMed]
- John, U.; Kemper, M.J. Urinary tract infections in children after renal transplantation. Pediatr. Nephrol. 2009, 24, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Saad, I.R.; Habib, E.; ElSheemy, M.S.; Abdel-Hakim, M.; Sheba, M.; Mosleh, A.; Salah, D.M.; Bazaraa, H.; Fadel, F.I.; Morsi, H.A.; et al. Outcomes of living donor renal transplantation in children with lower urinary tract dysfunction: A comparative retrospective study. BJU Int. 2016, 118, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Luke, P.P.; Herz, D.B.; Bellinger, M.F.; Chakrabarti, P.; Vivas, C.A.; Scantlebury, V.P.; Hakala, T.R.; Jevnikar, A.M.; Jain, A.; Shapiro, R.; et al. Long-term results of pediatric renal transplantation into a dysfunctional lower urinary tract. Transplantation 2003, 76, 1578–1582. [Google Scholar] [CrossRef] [PubMed]
- Holmdahl, G.; Sillen, U.; Hellström, A.L.; Sixt, R.; Sölsnes, E. Does treatment with clean intermittent catheterization in boys with posterior urethral valves affect bladder and renal function? J. Urol. 2003, 170, 1681–1685; discussion 1685. [Google Scholar] [CrossRef] [PubMed]
- Sager, C.; Burek, C.; Durán, V.; Corbetta, J.P.; Weller, S.; Paz, E.; López, J.C. Outcome of renal transplant in patients with abnormal urinary tract. Pediatr. Surg. Int. 2011, 27, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Riley, P.; Marks, S.D.; Desai, D.Y.; Mushtaq, I.; Koffman, G.; Mamode, N. Challenges facing renal transplantation in pediatric patients with lower urinary tract dysfunction. Transplantation 2010, 89, 1299–1307. [Google Scholar] [CrossRef]
- Kitta, T.; Mitsui, T.; Izumi, N. Diagnosis and Treatment of Japanese Children with Neurogenic Bladder: Analysis of Data from a National Health Insurance Database. J. Clin. Med. 2023, 12, 3191. [Google Scholar] [CrossRef]
- Groen, J.; Pannek, J.; Castro Diaz, D.; Del Popolo, G.; Gross, T.; Hamid, R.; Karsenty, G.; Kessler, T.M.; Schneider, M.; t Hoen, L.; et al. Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur. Urol. 2016, 69, 324–333. [Google Scholar] [CrossRef]
- Weld, K.J.; Dmochowski, R.R. Effect of bladder management on urological complications in spinal cord injured patients. J. Urol. 2000, 163, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Ben-David, R.; Carroll, F.; Kornitzer, E.; Dekalo, S.; Mano, R.; Ben-Chaim, J.; Cleper, R.; Bar-Yosef, Y. Asymptomatic bacteriuria and antibiotic resistance profile in children with neurogenic bladder who require clean intermittent catheterization. Spinal Cord. 2022, 60, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Salman, B.M.; Hassan, A.I.; Sultan, S.M.; Tophill, P.R.; Halawa, A.M. Renal Transplant in Patients With Abnormal Bladder: Impact of Causes on Graft Function and Survival. Exp. Clin. Transpl. 2017, 15, 609–614. [Google Scholar] [CrossRef][Green Version]
- González-Jorge, A.L.; Hernández-Plata, J.A.; Bracho-Blanchet, E.; Raya-Rivera, A.M.; Romero-Navarro, B.; Reyes-López, A.; Varela-Fascinetto, G. Should a complex uropathy be a contraindication for renal transplantation in children? Transpl. Proc. 2010, 42, 2365–2368. [Google Scholar] [CrossRef]
- Jahromi, M.S.; Velasquez, M.C.; Blachman-Braun, R.; Gosalbez, R.; Castellan, M.; Labbie, A.; Ciancio, G.; Chandar, J.; Alam, A. Pediatric Kidney Transplantation Outcomes in Children with Primary Urological Abnormalities Versus Nonurological Abnormalities: Long-Term Results. J. Urol. 2020, 203, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Marcou, M.; Galiano, M.; Tzschoppe, A.; Sauerstein, K.; Wach, S.; Taubert, H.; Wullich, B.; Hirsch-Koch, K.; Apel, H. Risk Factor Analysis for Long-Term Graft Survival Following Pediatric Kidney Transplantation: The Importance of Pretransplantation Time on Dialysis and Donor/Recipient Age Difference. J. Clin. Med. 2023, 12, 7014. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Enviironment for Statistical Computing; The R Project for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 1 October 2022).
- Lapides, J.; Diokno, A.C.; Silber, S.J.; Lowe, B.S. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J. Urol. 1972, 107, 458–461. [Google Scholar] [CrossRef]
- Van Savage, J.G.; Sackett, C.K.; Wilhelm, C.L.; Sessions, R.P.; Mesrobian, H.G. Indications for and outcomes of clean intermittent catheterization in children with normal genital sensation. J. Urol. 1997, 157, 1866–1868. [Google Scholar] [CrossRef]
- MacLellan, D.L. Management of pediatric neurogenic bladder. Curr. Opin. Urol. 2009, 19, 407–411. [Google Scholar] [CrossRef]
- Adams, J.; Mehls, O.; Wiesel, M. Pediatric renal transplantation and the dysfunctional bladder. Transpl. Int. 2004, 17, 596–602. [Google Scholar] [CrossRef]
- Bauer, S.B.; Saunders, R.A.; Masoom, S.N.; Choung, K.; Hayes, L.C.; Price, D.E.; Keays, M.; Sable, P.E.; Shimmel, A. The art of introducing clean intermittent catheterization: How families respond and adapt: A qualitative study. Neurourol. Urodyn. 2023, 42, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Vaidyananthan, S.; Soni, B.M.; Brown, E.; Sett, P.; Krishnan, K.R.; Bingley, J.; Markey, S. Effect of intermittent urethral catheterization and oxybutynin bladder instillation on urinary continence status and quality of life in a selected group of spinal cord injury patients with neuropathic bladder dysfunction. Spinal Cord. 1998, 36, 409–414. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bulut, I.K.; Taner, S.; Keskinoglu, A.; Sezer, T.O.; Kabasakal, C. Pediatric Kidney Transplantation in Patients with Urologic Anomalies. Transpl. Proc. 2019, 51, 2257–2261. [Google Scholar] [CrossRef] [PubMed]
- Hodges, S.J.; Patel, B.; McLorie, G.; Atala, A. Posterior urethral valves. Sci. World J. 2009, 9, 1119–1126. [Google Scholar] [CrossRef]
- Ferrari, P.; Lim, W.; Dent, H.; McDonald, S.P. Effect of donor-recipient age difference on graft function and survival in live-donor kidney transplantation. Nephrol. Dial. Transpl. 2011, 26, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Chang, J.H.; Choi, H.N.; Jung, J.Y.; Kim, Y.S.; Chung, W.K.; Park, Y.H.; Lee, H.H. Donor-recipient age difference and graft survival in living donor kidney transplantation. Transpl. Proc. 2012, 44, 270–272. [Google Scholar] [CrossRef] [PubMed]
- Tasaki, M.; Saito, K.; Nakagawa, Y.; Ikeda, M.; Imai, N.; Narita, I.; Takahashi, K. Effect of donor-recipient age difference on long-term graft survival in living kidney transplantation. Int. Urol. Nephrol. 2014, 46, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Kernig, K.; Albrecht, V.; Dräger, D.L.; Führer, A.; Mitzner, S.; Kundt, G.; Hakenberg, O.W. Predictors of Delayed Graft Function in Renal Transplantation. Urol. Int. 2022, 106, 512–517. [Google Scholar] [CrossRef]
- Van Arendonk, K.J.; Boyarsky, B.J.; Orandi, B.J.; James, N.T.; Smith, J.M.; Colombani, P.M.; Segev, D.L. National trends over 25 years in pediatric kidney transplant outcomes. Pediatrics 2014, 133, 594–601. [Google Scholar] [CrossRef]
- Dumbill, R.; Jaques, R.; Robb, M.; Johnson, R.; Ploeg, R.J.; Kaisar, M.E.; Sharples, E.J. Transplant and Recipient Factors in Prediction of Kidney Transplant Outcomes: A UK-Wide Paired Analysis. J. Clin. Med. 2022, 11, 2222. [Google Scholar] [CrossRef]
- Friedersdorff, F.; Koch, T.M.; Banuelos-Marco, B.; Gonzalez, R.; Fuller, T.F.; von Mechow, S.; Müller, D.; Lingnau, A. Long-Term Follow-Up after Paediatric Kidney Transplantation and Influence Factors on Graft Survival: A Single-Centre Experience of 16 years. Urol. Int. 2018, 100, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Peters-Sengers, H.; Houtzager, J.H.E.; Idu, M.M.; Heemskerk, M.B.A.; van Heurn, E.L.W.; Homan van der Heide, J.J.; Kers, J.; Berger, S.P.; van Gulik, T.M.; Bemelman, F.J. Impact of Cold Ischemia Time on Outcomes of Deceased Donor Kidney Transplantation: An Analysis of a National Registry. Transpl. Direct 2019, 5, e448. [Google Scholar] [CrossRef] [PubMed]
- van de Laar, S.C.; Lafranca, J.A.; Minnee, R.C.; Papalois, V.; Dor, F.J.M.F. The Impact of Cold Ischaemia Time on Outcomes of Living Donor Kidney Transplantation: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1620. [Google Scholar] [CrossRef] [PubMed]
- Jesus, L.E.; Pippi Salle, J.L. Pre-transplant management of valve bladder: A critical literature review. J. Pediatr. Urol. 2015, 11, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Reyblat, P.; Ginsberg, D.A. Augmentation cystoplasty: What are the indications? Curr. Urol. Rep. 2008, 9, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Rickard, M.; Chua, M.E.; Zu’bi, F.; Dos Santos, J.; Koyle, M.A.; Lorenzo, A.J.; Farhat, W.A. Comparative outcome analysis of pediatric kidney transplant in posterior urethral valves children with or without pretransplant Mitrofanoff procedure. Pediatr. Transpl. 2020, 24, e13798. [Google Scholar] [CrossRef]
- Lucas, E. Medical Management of Neurogenic Bladder for Children and Adults: A Review. Top. Spinal Cord. Inj. Rehabil. 2019, 25, 195–204. [Google Scholar] [CrossRef]
- Capizzi, A.; Zanon, G.F.; Zacchello, G.; Rigamonti, W. Kidney transplantation in children with reconstructed bladder. Transplantation 2004, 77, 1113–1116. [Google Scholar] [CrossRef]
- Herthelius, M.; Oborn, H. Urinary tract infections and bladder dysfunction after renal transplantation in children. J. Urol. 2007, 177, 1883–1886. [Google Scholar] [CrossRef]
- Weigel, F.; Lemke, A.; Tönshoff, B.; Pape, L.; Fehrenbach, H.; Henn, M.; Hoppe, B.; Jungraithmayr, T.; Konrad, M.; Laube, G.; et al. Febrile urinary tract infection after pediatric kidney transplantation: A multicenter, prospective observational study. Pediatr. Nephrol. 2016, 31, 1021–1028. [Google Scholar] [CrossRef]
- Reinberg, Y.; Gonzalez, R.; Fryd, D.; Mauer, S.M.; Najarian, J.S. The outcome of renal transplantation in children with posterior urethral valves. J. Urol. 1988, 140, 1491–1493. [Google Scholar] [CrossRef] [PubMed]
- Bryant, J.E.; Joseph, D.B.; Kohaut, E.C.; Diethelm, A.G. Renal transplantation in children with posterior urethral valves. J. Urol. 1991, 146, 1585–1587. [Google Scholar] [CrossRef] [PubMed]
- Morita, K.; Iwami, D.; Hotta, K.; Shimoda, N.; Miura, M.; Watarai, Y.; Hoshii, S.; Obikane, K.; Nakashima, T.; Sasaki, S.; et al. Pediatric kidney transplantation is safe and available for patients with urological anomalies as well as those with primary renal diseases. Pediatr. Transpl. 2009, 13, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Kamal, M.M.; El-Hefnawy, A.S.; Soliman, S.; Shokeir, A.A.; Ghoneim, M.A. Impact of posterior urethral valves on pediatric renal transplantation: A single-center comparative study of 297 cases. Pediatr. Transpl. 2011, 15, 482–487. [Google Scholar] [CrossRef]
- McKay, A.M.; Kim, S.; Kennedy, S.E. Long-term outcome of kidney transplantation in patients with congenital anomalies of the kidney and urinary tract. Pediatr. Nephrol. 2019, 34, 2409–2415. [Google Scholar] [CrossRef]
| Causes of ESRD in Children <12 Years Old in Our Center | n = 44 |
|---|---|
| Posterior urethral valves (PUVs) | 13 (29.5%) |
| Renal aplasia/hypoplasia/dysplasia | 7 (15.9%) |
| Reflux nephropathy | 6 (13.6%) |
| VACTERL association | 4 (9.0%) |
| Focal segmental glomerulosclerosis (FSGS) | 2 (4.5%) |
| Congenital nephrotic syndrome | 2 (4.5%) |
| Hemolytic uremic syndrome | 2 (4.5%) |
| Polycystic kidney disease | 2 (4.5%) |
| Other (cystinosis, bilateral nephrectomy, etc.) | 6 |
| Parameter | Control Group (No LUTD) n = 18 | LUTD CIC Group n = 8 | LUTD No CIC n = 15 | p |
|---|---|---|---|---|
| Organ donation | 0.013 | |||
| Living donation | 0 | 2 | 0 | |
| Postmortem donation | 18 | 6 | 15 | |
| Recipient sex | 0.036 | |||
| Male | 8 | 7 | 12 | |
| Female | 10 | 1 | 3 | |
| Age of the recipient (years; median (IQR)) | 7 (5–8) | 7 (4–10.5) | 6 (5–7) | 0.527 |
| Age of the donor (years; median (IQR)) | 32 (16–51) | 43 (35–53) | 34 (20–46) | 0.475 |
| BSA of the recipients at transplant (m2; median (IQR)) | 0.84 (0.72–0.93) | 0.89 (0.71–1.14) | 0.80 (0.70–0.83) | 0.492 |
| Pretransplant time of the recipient on dialysis (months; median (IQR)) | 24 (15–33) | 21 (11–34) | 41 (21–53) | 0.105 |
| HLA mismatches (n; median (IQR)) | 3 (2–3) | 3 (2–4) | 2 (2–3) | 0.652 |
| Cold ischemia time of the graft (h; median (IQR)) | 12 (10–16) | 14 (8–17) | 12 (11–15) | 0.930 |
| Urinary tract infections (n; median (IQR)) | 1 (0–2) | 2.5 (2–4) | 2 (0.5–3) | 0.045 |
| Follow-up of kidney grafts (months; median (IQR)) | 114 (86–144) | 135 (122–152) | 126 (72–135) | 0.420 |
| Parameter | HR (95% CI) | p |
|---|---|---|
| Organ donation | ||
| Living donation | 1 (Reference) | |
| Postmortem donation | 1.103 (0.132–9.235) | 0.928 |
| Recipient sex | ||
| Female | 1 (Reference) | |
| Male | 2.587 (0.551–12.160) | 0.229 |
| Age of the recipient (years; median (IQR)) | 0.928 (0.738–1.167) | 0.524 |
| Age of the donor (years; median (IQR)) | 1.063 (1.011–1.119) | 0.018 |
| BSA of the recipients at transplant (m2; median (IQR)) | 0.775 (0.021–28.18) | 0.889 |
| Pretransplant time of the recipient on dialysis (months; median (IQR)) | 1.011 (0.989–1.042) | 0.489 |
| HLA mismatches (n; median (IQR)) | 1.004 (0.503–1.901) | 0.990 |
| Cold ischemia time of the graft (h; median (IQR)) | 1.013 (0.909–1.130) | 0.813 |
| Urinary tract infections (n; median (IQR)) | 1.220 (1.024–1.454) | 0.026 |
| Grouping | ||
| Control (no LUTD) | 1 (Reference) | |
| LUTD CIC group | 4.091 (0.789–21.200) | 0.093 |
| LUTD no CIC | 3.197 (0.558–18.320) | 0.192 |
| Parameter | HR (95% CI) | p |
|---|---|---|
| Age of the donor (years; median (IQR)) | 1.066 (0.999–1.136) | 0.051 |
| Urinary tract infections (n; median (IQR)) | 1.192 (0.978–1.454) | 0.083 |
| Grouping | ||
| Control (no LUTD) | 1 (Reference) | |
| LUTD CIC group | 0.978 (0.125–7.659) | 0.983 |
| LUTD no CIC | 2.222 (0.357–13.834) | 0.392 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcou, M.; Galiano, M.; Tzschoppe, A.; Sauerstein, K.; Wach, S.; Taubert, H.; Wullich, B.; Hirsch-Koch, K.; Apel, H. Clean Intermittent Catheterization in Children under 12 Years Does Not Have a Negative Impact on Long-Term Graft Survival following Pediatric Kidney Transplantation. J. Clin. Med. 2024, 13, 33. https://doi.org/10.3390/jcm13010033
Marcou M, Galiano M, Tzschoppe A, Sauerstein K, Wach S, Taubert H, Wullich B, Hirsch-Koch K, Apel H. Clean Intermittent Catheterization in Children under 12 Years Does Not Have a Negative Impact on Long-Term Graft Survival following Pediatric Kidney Transplantation. Journal of Clinical Medicine. 2024; 13(1):33. https://doi.org/10.3390/jcm13010033
Chicago/Turabian StyleMarcou, Marios, Matthias Galiano, Anja Tzschoppe, Katja Sauerstein, Sven Wach, Helge Taubert, Bernd Wullich, Karin Hirsch-Koch, and Hendrik Apel. 2024. "Clean Intermittent Catheterization in Children under 12 Years Does Not Have a Negative Impact on Long-Term Graft Survival following Pediatric Kidney Transplantation" Journal of Clinical Medicine 13, no. 1: 33. https://doi.org/10.3390/jcm13010033
APA StyleMarcou, M., Galiano, M., Tzschoppe, A., Sauerstein, K., Wach, S., Taubert, H., Wullich, B., Hirsch-Koch, K., & Apel, H. (2024). Clean Intermittent Catheterization in Children under 12 Years Does Not Have a Negative Impact on Long-Term Graft Survival following Pediatric Kidney Transplantation. Journal of Clinical Medicine, 13(1), 33. https://doi.org/10.3390/jcm13010033









