Electrochemical Skin Conductance by Sudoscan in Non-Dialysis Chronic Kidney Disease Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Data Collection
2.3. Biochemical Investigations
2.4. Sudomotor Function Assessment
2.5. Clinical Neuropathy Scores
2.6. Statistical Analyses
3. Results
3.1. Clinical and Biochemical Characteristics of the Study Population Stratified by CKD Stages
3.2. Correlation between Sudoscan Score and Clinical and Biochemical Characteristics
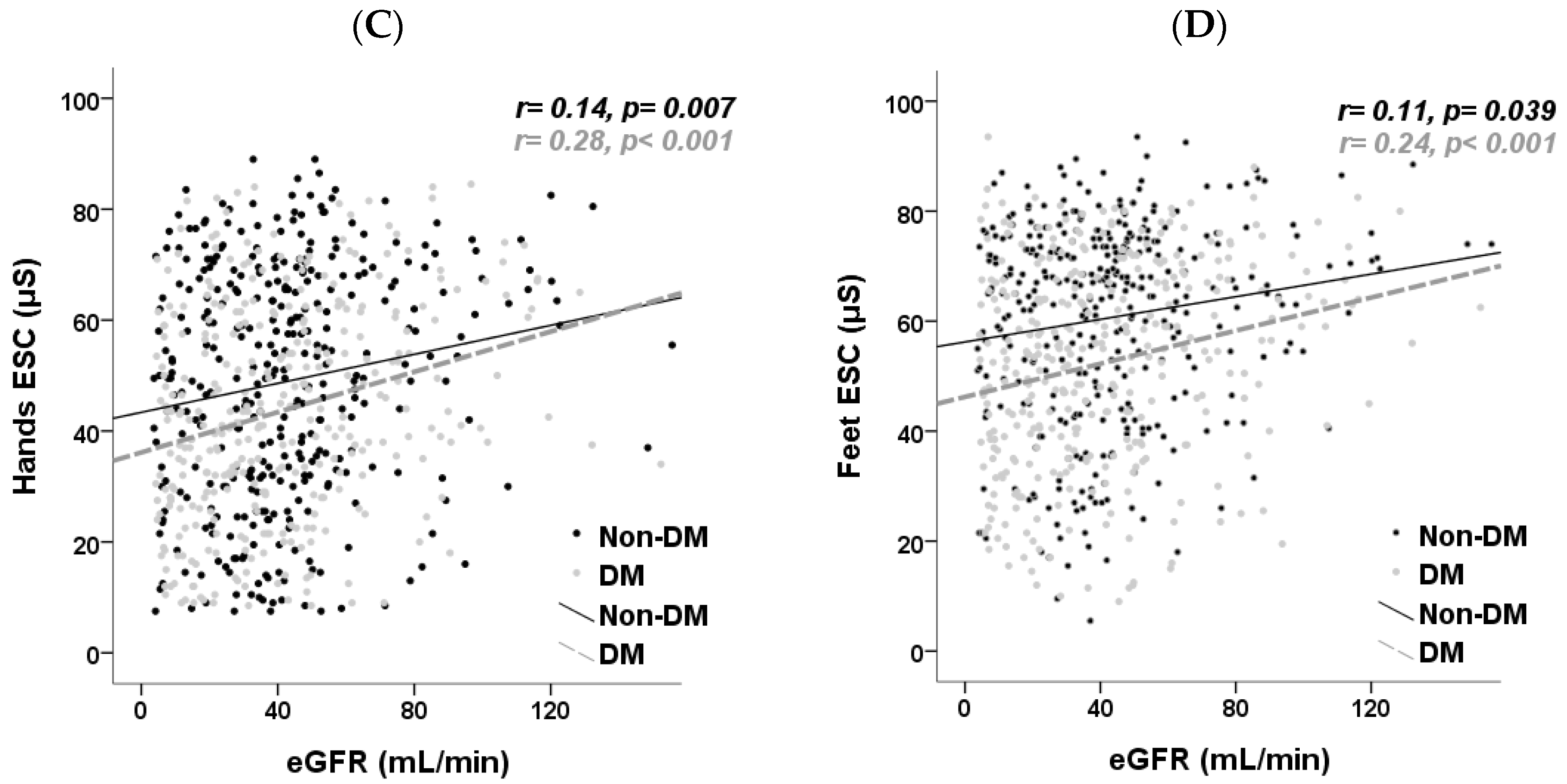
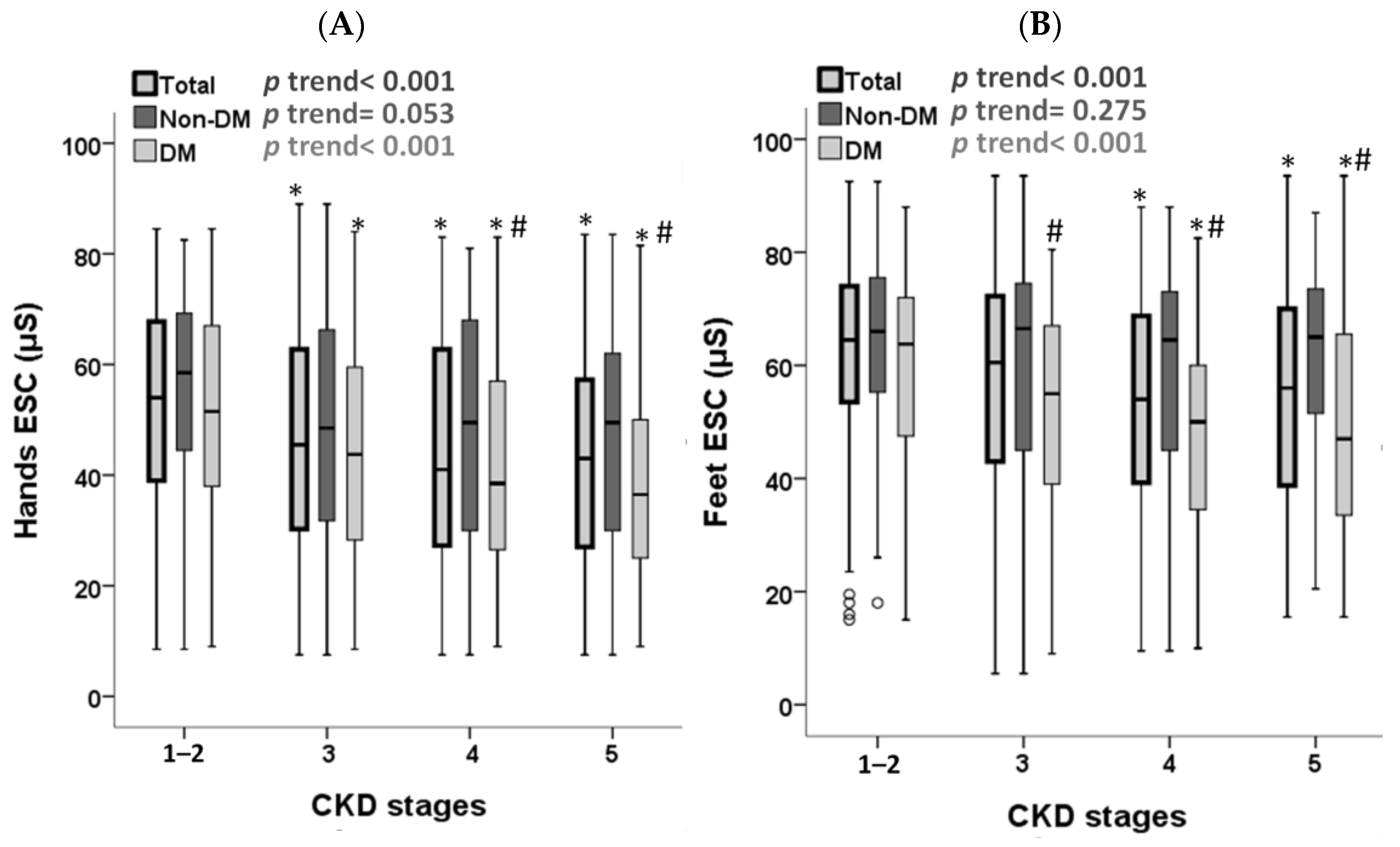
3.3. The Association between Sudoscan Score and CKD, Stratified by DM Status
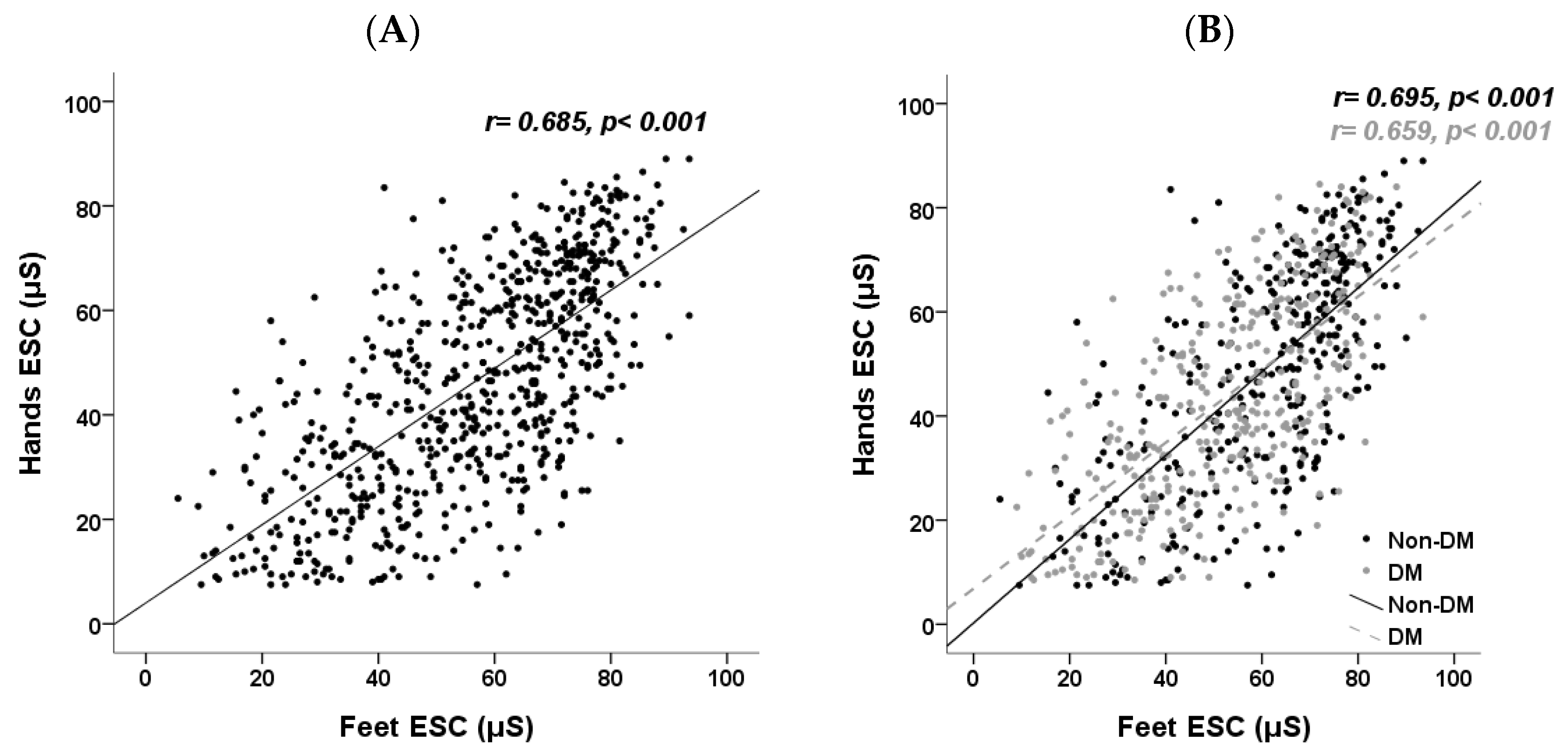
3.4. The Association between Hands and Feet Sudoscan Score, Stratified by DM Status
3.5. The Relationship between Sudomotor Function and Clinical Neuropathy Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raskin, N.H.; Fishman, R.A. Neurologic disorders in renal failure (second of two parts). N. Engl. J. Med. 1976, 294, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.V.; Kiernan, M.C. Uremic neuropathy: Clinical features and new pathophysiological insights. Muscle Nerve 2007, 35, 273–290. [Google Scholar] [CrossRef] [PubMed]
- Brouns, R.; De Deyn, P.P. Neurological complications in renal failure: A review. Clin. Neurol. Neurosurg. 2004, 107, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Kaminski, M.R.; Raspovic, A.; McMahon, L.P.; Strippoli, G.F.; Palmer, S.C.; Ruospo, M.; Dallimore, S.; Landorf, K.B. Risk factors for foot ulceration and lower extremity amputation in adults with end-stage renal disease on dialysis: A systematic review and meta-analysis. Nephrol. Dial. Transpl. 2015, 30, 1747–1766. [Google Scholar] [CrossRef] [PubMed]
- Laaksonen, S.; Metsarinne, K.; Voipio-Pulkki, L.M.; Falck, B. Neurophysiologic parameters and symptoms in chronic renal failure. Muscle Nerve 2002, 25, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Bolton, C.F. Peripheral neuropathies associated with chronic renal failure. Can. J. Neurol. Sci. 1980, 7, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Arnold, R.; Pianta, T.J.; Issar, T.; Kirby, A.; Scales, C.M.K.; Kwai, N.C.G.; Endre, Z.; Krishnan, A.V. Peripheral neuropathy: An important contributor to physical limitation and morbidity in stages 3 and 4 chronic kidney disease. Nephrol. Dial. Transpl. 2022, 37, 713–719. [Google Scholar] [CrossRef]
- Aggarwal, H.K.; Sood, S.; Jain, D.; Kaverappa, V.; Yadav, S. Evaluation of spectrum of peripheral neuropathy in predialysis patients with chronic kidney disease. Ren. Fail. 2013, 35, 1323–1329. [Google Scholar] [CrossRef]
- Jasti, D.B.; Mallipeddi, S.; Apparao, A.; Vengamma, B.; Sivakumar, V.; Kolli, S. A Clinical and Electrophysiological Study of Peripheral Neuropathies in Predialysis Chronic Kidney Disease Patients and Relation of Severity of Peripheral Neuropathy with Degree of Renal Failure. J. Neurosci. Rural. Pract. 2017, 8, 516–524. [Google Scholar] [CrossRef][Green Version]
- Smith, A.G.; Lessard, M.; Reyna, S.; Doudova, M.; Singleton, J.R. The diagnostic utility of Sudoscan for distal symmetric peripheral neuropathy. J. Diabetes Complicat. 2014, 28, 511–516. [Google Scholar] [CrossRef]
- Tesfaye, S.; Boulton, A.J.; Dyck, P.J.; Freeman, R.; Horowitz, M.; Kempler, P.; Lauria, G.; Malik, R.A.; Spallone, V.; Vinik, A.; et al. Diabetic neuropathies: Update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 2010, 33, 2285–2293. [Google Scholar] [CrossRef] [PubMed]
- Casellini, C.M.; Parson, H.K.; Richardson, M.S.; Nevoret, M.L.; Vinik, A.I. Sudoscan, a noninvasive tool for detecting diabetic small fiber neuropathy and autonomic dysfunction. Diabetes Technol. Ther. 2013, 15, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Freedman, B.I.; Bowden, D.W.; Smith, S.C.; Xu, J.; Divers, J. Relationships between electrochemical skin conductance and kidney disease in Type 2 diabetes. J. Diabetes Complicat. 2014, 28, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Luk, A.O.; Fu, W.C.; Li, X.; Ozaki, R.; Chung, H.H.; Wong, R.Y.; So, W.Y.; Chow, F.C.; Chan, J.C. The Clinical Utility of SUDOSCAN in Chronic Kidney Disease in Chinese Patients with Type 2 Diabetes. PLoS ONE 2015, 10, e0134981. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Yajnik, C.S.; Kantikar, V.; Pande, A.; Deslypere, J.P.; Dupin, J.; Calvet, J.H.; Bauduceau, B. Screening of cardiovascular autonomic neuropathy in patients with diabetes using non-invasive quick and simple assessment of sudomotor function. Diabetes Metab. 2013, 39, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Vinik, A.I.; Nevoret, M.L.; Casellini, C. The New Age of Sudomotor Function Testing: A Sensitive and Specific Biomarker for Diagnosis, Estimation of Severity, Monitoring Progression, and Regression in Response to Intervention. Front Endocrinol 2015, 6, 94. [Google Scholar] [CrossRef]
- Reach, P.; Touzot, M.; Lombardi, Y.; Maheas, C.; Sacco, E.; Fels, A.; Beaussier, H.; Urena-Torres, P.; Chatellier, G.; Ridel, C.; et al. Electrochemical skin conductance by Sudoscan(R): A new tool to predict intradialytic hypotension. Nephrol. Dial. Transplant. 2021, 36, 1511–1518. [Google Scholar] [CrossRef]
- Feldman, E.L.; Stevens, M.J.; Thomas, P.K.; Brown, M.B.; Canal, N.; Greene, D.A. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care 1994, 17, 1281–1289. [Google Scholar] [CrossRef]
- Mambelli, E.; Barrella, M.; Facchini, M.G.; Mancini, E.; Sicuso, C.; Bainotti, S.; Formica, M.; Santoro, A. The prevalence of peripheral neuropathy in hemodialysis patients. Clin. Nephrol. 2012, 77, 468–475. [Google Scholar] [CrossRef]
- Bouhassira, D.; Attal, N.; Alchaar, H.; Boureau, F.; Brochet, B.; Bruxelle, J.; Cunin, G.; Fermanian, J.; Ginies, P.; Grun-Overdyking, A.; et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005, 114, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Oh, T.J.; Song, Y.; Jang, H.C.; Choi, S.H. SUDOSCAN in Combination with the Michigan Neuropathy Screening Instrument Is an Effective Tool for Screening Diabetic Peripheral Neuropathy. Diabetes Metab. J. 2022, 46, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Selvarajah, D.; Cash, T.; Davies, J.; Sankar, A.; Rao, G.; Grieg, M.; Pallai, S.; Gandhi, R.; Wilkinson, I.D.; Tesfaye, S. SUDOSCAN: A Simple, Rapid, and Objective Method with Potential for Screening for Diabetic Peripheral Neuropathy. PLoS ONE 2015, 10, e0138224. [Google Scholar] [CrossRef] [PubMed]
- Lindblom, U.; Tegner, R. Thermal sensitivity in uremic neuropathy. Acta Neurol. Scand. 1985, 71, 290–294. [Google Scholar] [CrossRef]
- Chao, C.C.; Wu, V.C.; Tan, C.H.; Wang, Y.M.; Tseng, M.T.; Wu, P.C.; Lin, Y.H.; Lin, W.M.; Wu, K.D.; Hsieh, S.T. Skin denervation and its clinical significance in late-stage chronic kidney disease. Arch. Neurol. 2011, 68, 200–206. [Google Scholar] [CrossRef]
- Issar, T.; Walker, S.; Arnold, R.; Poynten, A.M.; Endre, Z.H.; Krishnan, A.V. Peripheral nerve morphology and intraneural blood flow in chronic kidney disease with and without diabetes. Muscle Nerve 2022, 65, 603–607. [Google Scholar] [CrossRef]
- Li, L.; Liu, B.; Lu, J.; Jiang, L.; Zhang, Y.; Shen, Y.; Wang, C.; Jia, W. Serum albumin is associated with peripheral nerve function in patients with type 2 diabetes. Endocrine 2015, 50, 397–404. [Google Scholar] [CrossRef]
- Wu, F.; Jing, Y.; Tang, X.; Li, D.; Gong, L.; Zhao, H.; He, L.; Li, Q.; Li, R. Anemia: An independent risk factor of diabetic peripheral neuropathy in type 2 diabetic patients. Acta Diabetol. 2017, 54, 925–931. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, J.; Zeng, S.; Chen, M.; Zou, G.; Li, Y.; Zhu, L.; Xu, J. Association Between Serum Albumin Levels and Diabetic Peripheral Neuropathy Among Patients with Type 2 Diabetes: Effect Modification of Body Mass Index. Diabetes Metab. Syndr. Obes. 2022, 15, 527–534. [Google Scholar] [CrossRef]
- Khafagi, A.T.; Yehia, M.A.; Helmy, A.K.; Hassan, W.; Abdelhakim, N. Effect of Erythropoietin-stimulating agent on uremic neuropathy in hemodialysis patients: A single-center open-label prospective study. Egypt. J. Neurol. Psychiatry Neurosurg. 2022, 58, 53. [Google Scholar] [CrossRef]
- Kabakus, N.; Ayar, A.; Yoldas, T.K.; Ulvi, H.; Dogan, Y.; Yilmaz, B.; Kilic, N. Reversal of iron deficiency anemia-induced peripheral neuropathy by iron treatment in children with iron deficiency anemia. J. Trop. Pediatr. 2002, 48, 204–209. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total (n = 700) | Stage 1–2 CKD (n = 143) | Stage 3 CKD (n = 303) | Stage 4–5 CKD (n = 254) | p for Trend |
|---|---|---|---|---|---|
| Basic demographic | |||||
| Age (years) | 67 (59–76) | 62 (50–69) | 68 (61–78) | 69 (61–78) | <0.001 * |
| Male, n (%) | 404 (57.7) | 78 (54.2) | 196 (64.7) | 130 (50.8) | 0.201 |
| Diabetes mellitus, n (%) | 344 (49.1) | 75 (52.1) | 127 (41.9) | 139 (54.3) | 0.315 |
| Hypertension, n (%) | 546 (78.1) | 94 (65.3) | 228 (75.2) | 224 (87.5) | <0.001 * |
| Glomerulonephritis, n (%) | 236 (33.7) | 45 (31.5) | 95 (31.4) | 96 (37.8) | 0.141 |
| Body mass index (kg/m2) | 25 (23–28) | 25 (24–29) | 25 (23–28) | 25 (22–28) | 0.016 * |
| Laboratory values | |||||
| Hemoglobin (g/dL) | 12.0 (10.5–13.8) | 13.6 (12.4–14.8) | 12.8 (11.3–14.3) | 10.6 (9.4–11.5) | <0.001 * |
| Albumin (g/dL) | 4.1 (3.9–4.3) | 4.2 (4.0–4.5) | 4.2 (4.0–4.3) | 4.0 (3.8–4.2) | <0.001 * |
| BUN (mg/dL) | 28 (20–45) | 15 (12–19) | 24 (20–30) | 51 (39–69) | <0.001 * |
| Creatinine (mg/dL) | 1.7 (1.2–2.8) | 0.9 (0.7–1.1) | 1.6 (1.4–1.8) | 3.5 (2.6–5.3) | <0.001 * |
| eGFR (mL/min) | 37.9 (21.5–54.6) | 78.9 (66.6–96.5) | 43.3 (35.7–49.6) | 17.4 (9.3–22.5) | <0.001 * |
| UPCR (g/g) | 0.40 (0.16–1.34) | 0.22 (0.14–0.54) | 0.25 (0.12–0.61) | 1.24 (0.49–2.60) | <0.001 * |
| Total cholesterol (mg/dL) | 151 (128–176) | 155 (133–180) | 152 (128–176) | 144 (125–171) | 0.096 |
| HbA1c (%) a | 6.7 (6.1–7.5) | 6.6 (6.1–7.6) | 6.7 (6.1–7.6) | 6.6 (5.9–7.5) | 0.692 |
| Calcium (mg/dL) b | 9.2 (8.9, 9.6) | 9.3 (8.8, 9.6) | 9.3 (9.0, 9.6) | 9.0 (8.7, 9.4) | <0.001 * |
| Phosphorus (mg/dL) b | 3.6 (3.2–4.0) | 3.5 (3.1–3.8) | 3.4 (3.1–3.7) | 3.9 (3.4–4.5) | <0.001 * |
| Hands | |||||
| ESC (μS) | 46.5 (30.5–63.5) | 54.0 (39.0–68.0) | 45.5 (30.0–63.0) | 41.8 (26.5–60.5) | <0.001 * |
| Pathological, n (%) | 278 (39.7) | 38 (26.6) | 124 (40.9) | 116 (45.7) | <0.001 * |
| Asymmetry (%) | 8 (3–15) | 5 (2–13) | 8 (3–15) | 9 (3–15) | 0.008 * |
| Feet | |||||
| ESC (μS) | 60.0 (43.0–72.0) | 64.5 (53.5–74.0) | 60.5 (43.0–72.5) | 55.0 (39.0–69.8) | <0.001 * |
| Pathological, n (%) | 237 (33.9) | 31 (21.7) | 103 (34.0) | 103 (40.6) | <0.001 * |
| Asymmetry (%) | 5 (2–10) | 3 (1–7) | 5 (2–10) | 6 (2–13) | 0.006 * |
| CAN score | 33 (28–38) | 32 (25–37) | 34 (29–38) | 33 (28–38) | 0.004 * |
| Nephropathy score | 46 (34–58) | 55 (44–69) | 44 (33–56) | 44 (31–56) | <0.001 * |
| ESC (μS) | ||||
|---|---|---|---|---|
| Hands | Feet | |||
| Variables | r | p | r | p |
| Age (years) | −0.32 | <0.001 * | −0.32 | <0.001 * |
| Male, n (%) | 0.04 | 0.254 | 0.03 | 0.465 |
| Diabetes mellitus, n (%) | −0.14 | <0.001 * | −0.23 | <0.001 * |
| Hypertension, n (%) | −0.10 | 0.009 * | −0.09 | 0.013 * |
| Body mass index (kg/m2) | 0.14 | <0.001 * | 0.06 | 0.091 |
| Hemoglobin (g/dL) | 0.28 | <0.001 * | 0.22 | <0.001 * |
| Albumin (g/dL) | 0.24 | <0.001 * | 0.24 | <0.001 * |
| BUN (mg/dL) | −0.15 | <0.001 * | −0.12 | 0.002 * |
| Creatinine (mg/dL) | −0.18 | <0.001 * | −0.15 | <0.001 * |
| eGFR (mL/min) | 0.21 | <0.001 * | 0.18 | <0.001 * |
| UPCR (mg/g) | −0.15 | <0.001 * | −0.12 | 0.002 * |
| Total cholesterol (mg/dL) | 0.06 | 0.121 | 0.08 | 0.044 * |
| HbA1c (%) a | −0.04 | 0.518 | −0.04 | 0.466 |
| Calcium (mmol/L) b | 0.08 | 0.064 | 0.06 | 0.204 |
| Phosphorus (mg/dL) b | −0.05 | 0.228 | −0.03 | 0.536 |
| Variables | Hands ESC (μS) | Feet ESC (μS) | ||||
|---|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | |||||
| Univariate | Multivariate | Univariate | Multivariate | |||
| Model 1 | Model 2 | Model 1 | Model 2 | |||
| Age (years) | −0.48 (−0.59, −0.37) * | −0.38 (−0.50, −0.27) * | −0.40 (−0.52, −0.28) * | −0.43 (−0.53, −0.33) * | −0.35 (−0.46, −0.25) * | −0.38 (−0.49, −0.27) * |
| DM, n (%) | −5.44 (−8.45, −2.42) * | −4.87 (−7.79, −1.95) * | −4.89 (−7.88, −1.89) * | −8.26 (−10.97, −5.55) * | −7.30 (−9.96, −4.64) * | −7.27 (−10.04, −4.49) * |
| BMI (kg/m2) | 0.63 (0.30, 0.97) * | 0.61 (0.29, 0.94) * | 0.41 (0.07, 0.74) * | 0.21 (−0.10, 0.52) | 0.23 (−0.06, 0.53) | 0.14 (−0.17, 0.45) |
| eGFR (mL/min) | 0.16 (0.11, 0.21) * | 0.09 (0.03, 0.14) * | −0.01 (−0.08, 0.06) | 0.13 (0.08, 0.18) * | 0.07 (0.02, 0.12) * | 0.00 (−0.06, 0.07) |
| Hb (g/dL) | 2.55 (1.90, 3.21) * | - | 1.46 (0.61, 2.31) * | 1.68 (1.07, 2.30) * | - | 0.57 (−0.22, 1.36) |
| Albumin (g/dL) | 7.99 (4.99, 11.00) * | - | 7.62 (3.27, 11.97) * | 6.91 (4.11, 9.70) * | - | 8.80 (4.76, 12.84) * |
| UPCR (g/g) | −0.82 (−1.43, −0.21) * | - | −0.30 (−0.96, 0.35) | −0.83 (−1.39, −0.27) * | - | −0.26 (−0.87, 0.35) |
| DM (n = 344) | ||||||
| Variables | Hands ESC (μS) | Feet ESC (μS) | ||||
| β (95% CI) | β (95% CI) | |||||
| Univariate | Multivariate | Univariate | Multivariate | |||
| Model 1 | Model 2 | Model 1 | Model 2 | |||
| Age (years) | −0.31 (−0.49, −0.13) * | −0.17 (−0.36, 0.01) | −0.21 (−0.41, 0.00) * | −0.18 (−0.35, −0.01) * | −0.09 (−0.27, 0.09) | −0.12 (−0.32, 0.08) |
| BMI (kg/m2) | 0.81 (0.37, 1.25) * | 0.60 (0.16, 1.05) * | 0.47 (0.01, 0.92) * | 0.40 (−0.03, 0.82) | 0.22 (−0.21, 0.65) | 0.17 (−0.28, 0.62) |
| eGFR (mL/min) | 0.18 (0.11, 0.25) * | 0.15 (0.07, 0.22) * | −0.02 (−0.13, 0.09) | 0.15 (0.08, 0.22) * | 0.13 (0.06, 0.20) * | −0.02 (−0.12, 0.09) |
| Hb (g/dL) | 2.22 (1.36, 3.08) * | - | 1.32 (0.10, 2.54) * | 1.62 (0.78, 2.46) * | - | 0.80 (−0.40, 2.00) |
| Albumin (g/dL) | 14.37 (9.33, 19.41) * | - | 10.77 (4.64, 16.90) * | 14.51 (9.63, 19.39) * | - | 12.68 (6.65, 18.71) * |
| UPCR (g/g) | −0.76 (−1.41, −0.11) * | - | −0.18 (−0.93, 0.57) | −0.81 (−1.43, −0.19) * | - | −0.13 (−0.87, 0.61) |
| Non-DM (n = 356) | ||||||
| Variables | Hands ESC (μS) | Feet ESC (μS) | ||||
| β (95% CI) | β (95% CI) | |||||
| Univariate | Multivariate | Univariate | Multivariate | |||
| Model 1 | Model 2 | Model 1 | Model 2 | |||
| Age (years) | −0.55 (−0.69, −0.41) * | −0.51 (−0.66, −0.37) * | −0.48 (−0.63, −0.33) * | −0.53 (−0.65, −0.42) * | −0.52 (−0.64, −0.40) * | −0.49 (−0.62, −0.36) * |
| BMI (kg/m2) | 0.71 (0.19, 1.23) * | 0.68 (0.19, 1.17) * | 0.42 (−0.08, 0.93) | 0.35 (−0.09, 0.80) | 0.30 (−0.11, 0.72) | 0.21 (−0.23, 0.65) |
| eGFR (mL/min) | 0.13 (0.05, 0.21) * | 0.03 (−0.05, 0.11) | −0.02 (−0.11, 0.08) | 0.10 (0.04, 0.17) * | 0.01 (−0.06, 0.08) | 0.01 (−0.07, 0.09) |
| Hb (g/dL) | 2.86 (1.89, 3.83) * | - | 1.75 (0.54, 2.97) * | 1.67 (0.81, 2.53) * | - | 0.57 (−0.48, 1.63) |
| Albumin (g/dL) | 4.75 (0.98, 8.51) * | - | 5.76 (−0.70, 12.22) | 2.92 (−0.36, 6.20) | - | 6.88 (1.27, 12.48) * |
| UPCR (g/g) | −0.27 (−1.74, 1.20) | - | 0.25 (−1.29, 1.78) | 0.28 (−0.97, 1.54) | - | 0.55 (−0.78, 1.88) |
| ESC (μS) | ||||
|---|---|---|---|---|
| Hands | Feet | |||
| Variables | r | p | r | p |
| MNSI_Q (score) | −0.20 | <0.001 * | −0.19 | <0.001 * |
| MNSI_P (score) | −0.26 | <0.001 * | −0.30 | <0.001 * |
| DN4 (score) | −0.18 | <0.001 * | −0.22 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiu, L.-T.; Lin, Y.-L.; Wang, C.-H.; Hwu, C.-M.; Liou, H.-H.; Hsu, B.-G. Electrochemical Skin Conductance by Sudoscan in Non-Dialysis Chronic Kidney Disease Patients. J. Clin. Med. 2024, 13, 187. https://doi.org/10.3390/jcm13010187
Chiu L-T, Lin Y-L, Wang C-H, Hwu C-M, Liou H-H, Hsu B-G. Electrochemical Skin Conductance by Sudoscan in Non-Dialysis Chronic Kidney Disease Patients. Journal of Clinical Medicine. 2024; 13(1):187. https://doi.org/10.3390/jcm13010187
Chicago/Turabian StyleChiu, Liang-Te, Yu-Li Lin, Chih-Hsien Wang, Chii-Min Hwu, Hung-Hsiang Liou, and Bang-Gee Hsu. 2024. "Electrochemical Skin Conductance by Sudoscan in Non-Dialysis Chronic Kidney Disease Patients" Journal of Clinical Medicine 13, no. 1: 187. https://doi.org/10.3390/jcm13010187
APA StyleChiu, L.-T., Lin, Y.-L., Wang, C.-H., Hwu, C.-M., Liou, H.-H., & Hsu, B.-G. (2024). Electrochemical Skin Conductance by Sudoscan in Non-Dialysis Chronic Kidney Disease Patients. Journal of Clinical Medicine, 13(1), 187. https://doi.org/10.3390/jcm13010187








