Clinical Results after Release of Sternocleidomastoid Muscle Surgery for Neglected Congenital Muscular Torticollis—Unipolar vs. Bipolar Release Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Surgical Procedures
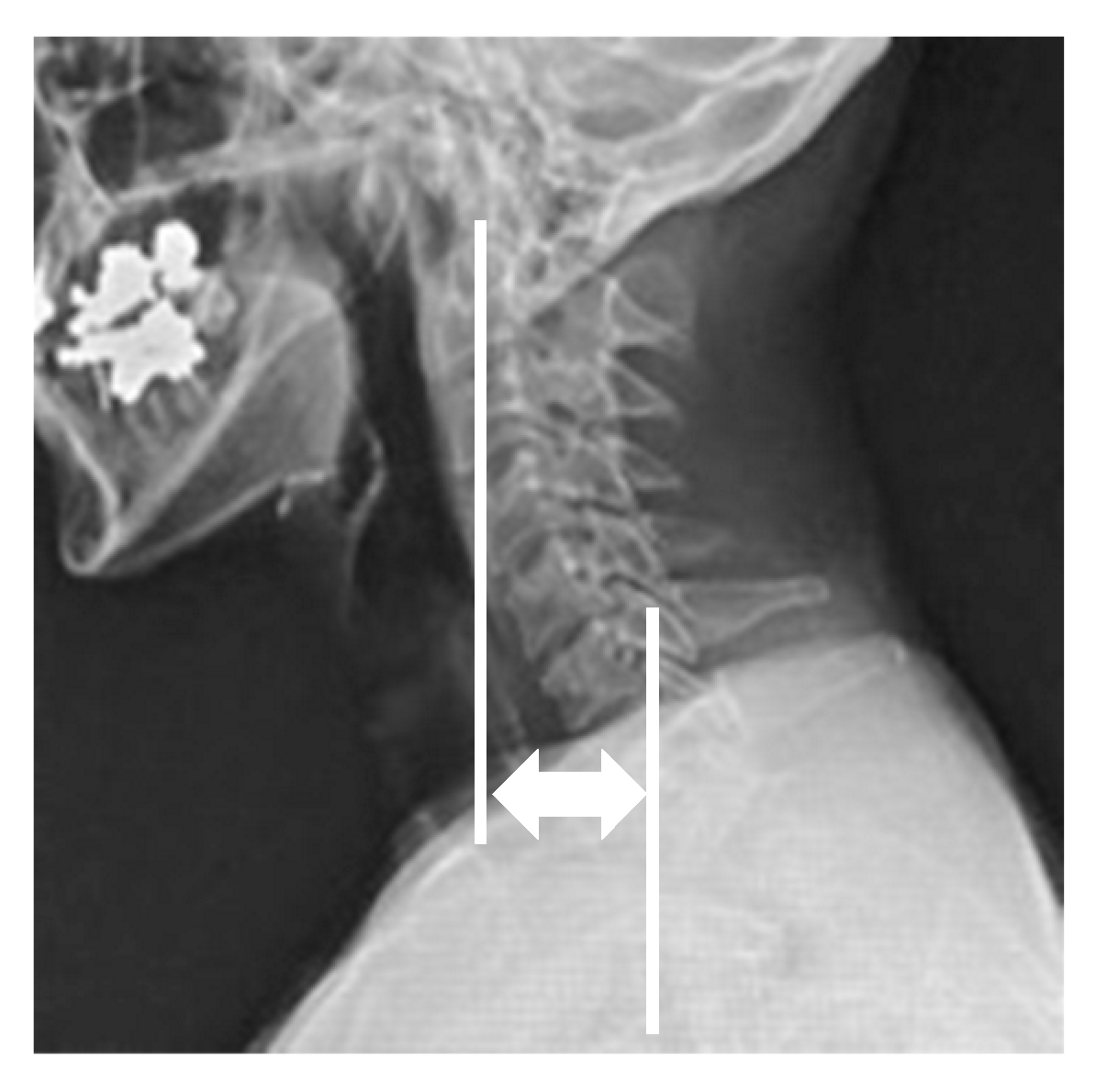
2.2. Outcome Measurements
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Surgical Data and Adverse Events
3.3. Radiographic Outcomes
3.4. Clinical Outcomes
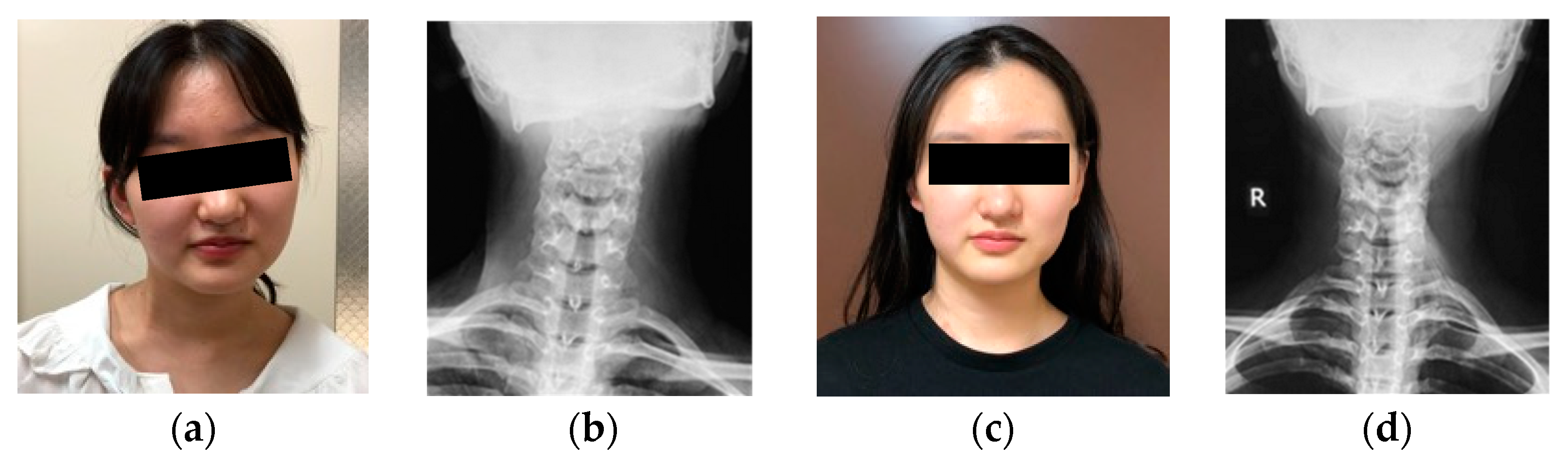
3.5. Representative Case of Bipolar Release of Sternocleidomastoid Muscle
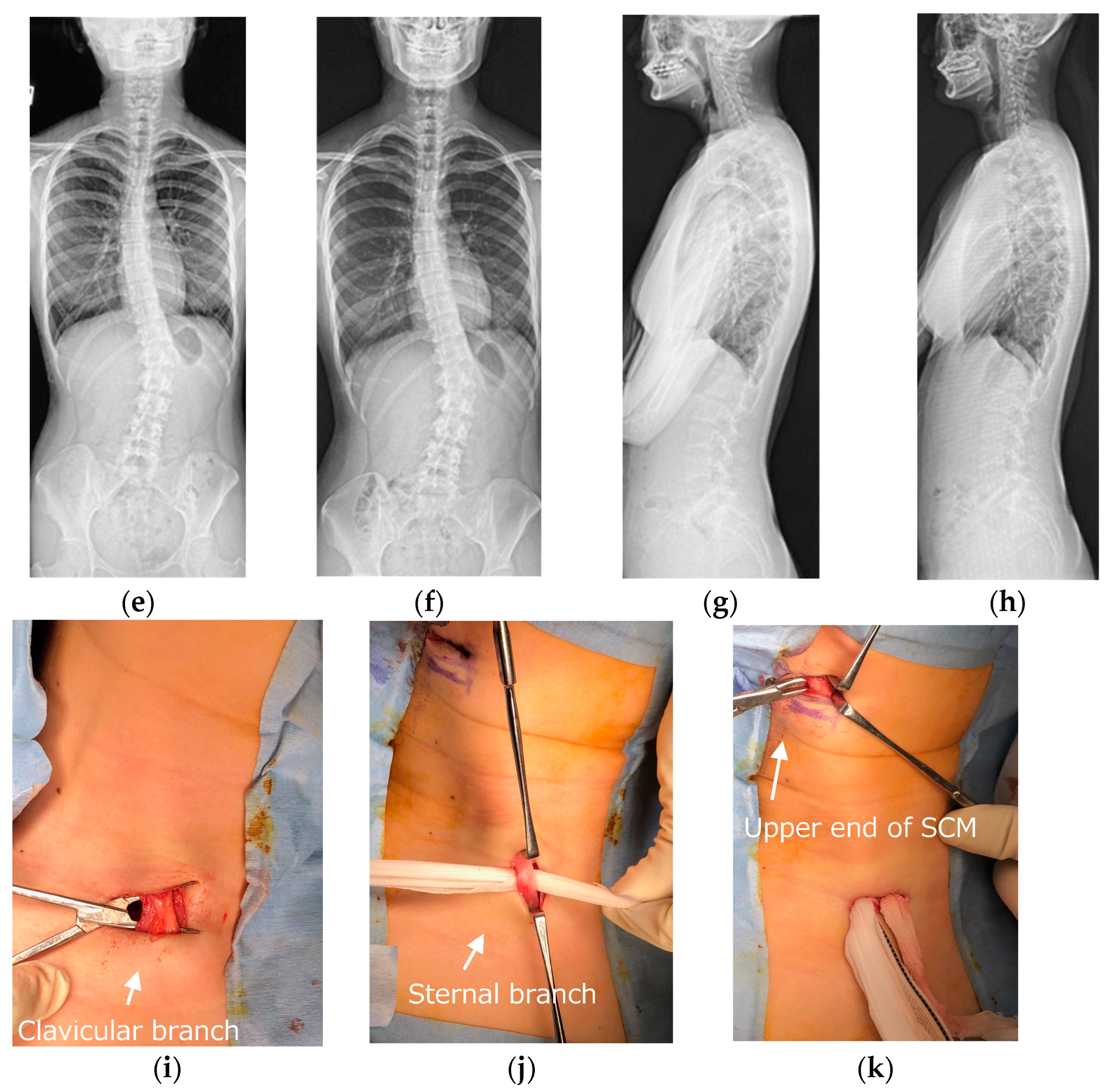
3.6. Representative Case of Unipolar Release of Sternocleidomastoid Muscle
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hsieh, Y.Y.; Tsai, F.J.; Lin, C.C.; Chang, F.C.; Tsai, C.H. Breech deformation complex in neonates. J. Reprod. Med. 2000, 45, 933–935. [Google Scholar] [PubMed]
- Do, T.T. Congenital muscular torticollis: Current concepts and review of treatment. Curr. Opin. Pediatr. 2006, 18, 26–29. [Google Scholar] [PubMed]
- Wei, J.L.; Schwartz, K.M.; Weaver, A.L.; Orvidas, L.J.; Bs, K.M.S. Pseudotumor of infancy and congenital muscular torticollis: 170 cases. Laryngoscope 2001, 111 Pt 1, 688–695. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.N.; Chou, M.L. Ultrasonographic study of the sternocleidomastoid muscle in the management of congenital muscular torticollis. J. Pediatr. Surg. 1997, 32, 1648–1651. [Google Scholar] [CrossRef] [PubMed]
- Fielding, J.W.; Hawkins, R.J. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J. Bone Jt. Surg. Am. 1977, 59, 37–44. [Google Scholar] [CrossRef]
- Ishii, K.; Toyama, Y.; Nakamura, M.; Chiba, K.; Matsumoto, M. Management of chronic atlantoaxial rotatory fixation. Spine 2012, 37, E278–E285. [Google Scholar] [CrossRef]
- Cheng, J.C.; Wong, M.W.; Tang, S.P.; Chen, T.M.; Shum, S.L.; Wong, E.M. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. A prospective study of eight hundred and twenty-one cases. J. Bone Jt. Surg. Am. 2001, 83, 679–687. [Google Scholar] [CrossRef]
- Lee, K.; Chung, E.; Lee, B.-H. A comparison of outcomes of asymmetry in infants with congenital muscular torticollis according to age upon starting treatment. J. Phys. Ther. Sci. 2017, 29, 543–547. [Google Scholar] [CrossRef]
- Kwon, D.R.; Park, G.Y. Efficacy of microcurrent therapy in infants with congenital muscular torticollis involving the entire sternocleidomastoid muscle: A randomized placebo-controlled trial. Clin. Rehabil. 2014, 28, 983–991. [Google Scholar] [CrossRef]
- Ling, C.M. The influence of age on the results of open sternomastoid tenotomy in muscular torticollis. Clin. Orthop. Relat. Res. 1976, 116, 142–148. [Google Scholar] [CrossRef]
- Seo, S.J.; Kim, J.H.; Joh, Y.H.; Park, D.H.; Lee, I.J.; Lim, H.; Park, M.C. Change of Facial asymmetry in patients with congenital muscular torticollis after surgical release. J. Craniofacial Surg. 2016, 27, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Ahn, H.S.; Yim, S.Y. Effectiveness of surgical treatment for neglected congenital muscular torticollis: A systematic review and meta-analysis. Plast. Reconstr. Surg. 2015, 136, 67e–77e. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.C.; Tang, S.P. Outcome of surgical treatment of congenital muscular torticollis. Clin. Orthop. Relat. Res. 1999, 362, 190–200. [Google Scholar] [CrossRef]
- Lim, K.S.; Shim, J.S.; Lee, Y.S. Is sternocleidomastoid muscle release effective in adults with neglected congenital muscular torticollis? Clin. Orthop. Relat. Res. 2014, 472, 1271–1278. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, S.; Shyam, A.K.; Sancheti, P.; Arora, P.; Nagda, T.; Naik, P. Adult presentation of congenital muscular torticollis: A series of 12 patients treated with a bipolar release of sternocleidomastoid and Z-lengthening. J. Bone Jt. Surg. Br. Vol. 2011, 93, 828–832. [Google Scholar] [CrossRef]
- Akazawa, H.; Nakatsuka, Y.; Miyake, Y.; Takahashi, Y. Congenital muscular torticollis: Long-term follow-up of thirty-eight partial resections of the sternocleidomastoid muscle. Arch. Orthop. Trauma Surg. 1993, 112, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Seyhan, N.; Jasharllari, L.; Keskin, M.; Savacı, N. Efficacy of bipolar release in neglected congenital muscular torticollis patients. Musculoskelet. Surg. 2012, 96, 55–57. [Google Scholar] [CrossRef]
- Hardgrib, N.; Rahbek, O.; Møller-Madsen, B.; Maimburg, R.D. Do obstetric risk factors truly influence the etiopathogenesis of congenital muscular torticollis? J. Orthop. Traumatol. 2017, 18, 359–364. [Google Scholar] [CrossRef]
- Ho, B.C.; Lee, E.H.; Singh, K. Epidemiology, presentation and management of congenital muscular torticollis. Singap. Med. J. 1999, 40, 675–679. [Google Scholar]
- Davids, J.R.; Wenger, D.R.; Mubarak, S.J. Congenital muscular torticollis: Sequela of intrauterine or perinatal compartment syndrome. J. Pediatr. Orthop. 1993, 13, 141–147. [Google Scholar]
- Chen, H.-X.; Tang, S.-P.; Gao, F.-T.; Xu, J.-L.; Jiang, X.-P.; Cao, J.; Fu, G.-B.; Sun, K.; Liu, S.-Z.; Shi, W. Fibrosis, adipogenesis, and Muscle atrophy in congenital muscular torticollis. Medicine 2014, 93, e138. [Google Scholar] [CrossRef] [PubMed]
- Qiu, X.; Cui, Z.; Tang, G.; Deng, H.; Xiong, Z.; Han, S.; Tang, S. The Effectiveness and safety of botulinum toxin injections for the treatment of congenital muscular torticollis. J. Craniofacial Surg. 2020, 31, 2160–2166. [Google Scholar] [CrossRef] [PubMed]
- Omidi-Kashani, F.; Hasankhani, E.G.; Sharifi, R.; Mazlumi, M. Is surgery recommended in adults with neglected congenital muscular torticollis? A prospective study. BMC Musculoskelet. Disord. 2008, 9, 158. [Google Scholar] [CrossRef] [PubMed]
- Glassman, S.D.; Berven, S.; Bridwell, K.; Horton, W.; Dimar, J.R. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 2005, 30, 682–688. [Google Scholar] [CrossRef]
- Tang, J.A.; Scheer, J.K.; Smith, J.S.; Deviren, V.; Bess, S.; Hart, R.A.; Lafage, V.; Shaffrey, C.I.; Schwab, F.; Ames, C.P.; et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012, 71, 662–669, discussion 669. [Google Scholar] [CrossRef]
- Ginsberg, L.E.; Eicher, S.A. Great auricular nerve: Anatomy and imaging in a case of perineural tumor spread. AJNR Am. J. Neuroradiol. 2000, 21, 568–571. [Google Scholar]

| Demographics | Group of Bipolar Release of Sternocleidomastoid (n = 3) | Group of Unipolar Release of Sternocleidomastoid (n = 18) | p-Value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age at surgery (years old) | 40.0 ± 17.0 | 32.3 ± 13.1 | 0.47 |
| Sex | 2/3 females | 12/18 females | 1.00 |
| Height (cm) | 162.9 ± 6.1 | 165.8 ± 6.7 | 0.69 |
| Weight (kg) | 55.0 ± 8.0 | 59.1 ± 9.1 | 0.62 |
| Body mass index (kg/m2) | 20.6 ± 1.8 | 21.6 ± 3.5 | 0.84 |
| Affected side (right side) | 3/3 cases | 12/18 cases | 0.53 |
| History of previous surgery for congenital muscular torticollis | 1/3 cases | 4/18 cases | 1.00 |
| Follow-up period (months) | 16.0 ± 5.7 | 10.4 ± 7.6 | 0.22 |
| Radiographic Parameters | Group of Bipolar Release of Sternocleidomastoid (n = 3) | Group of Unipolar Release of Sternocleidomastoid (n = 18) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Preoperative Mean ± SD | Postoperative Mean ± SD | Preoperative Mean ± SD | Postoperative Mean ± SD | P1 | P2 | P3 | P4 | |
| Cervicomandibular angle (°) | 13.7 ± 2.1 | 3.3 ± 0.5 | 15.4 ± 6.5 | 4.1 ± 2.6 | 0.10 | <0.01 | 1.00 | 0.92 |
| C2 to T1 difference (mm) | 12.0 ± 4.5 | 3.3 ± 1.2 | 14.2 ± 7.7 | 5.2 ± 4.8 | 0.10 | <0.01 | 0.69 | 0.84 |
| Clavicle angle (°) | 2.0 ± 1.6 | 1.3 ± 0.5 | 2.7 ± 1.3 | 1.2 ± 0.5 | 070 | <0.01 | 0.62 | 0.77 |
| Central sacral vertical line (mm) | 7.0 ± 5.4 | 5.7 ± 2.6 | 13.5 ± 10.3 | 5.3 ± 2.8 | 0.70 | <0.05 | 0.36 | 0.84 |
| Cervical lordosis (flexion) (°) | −14.3 ± 4.9 | −23.7 ± 10.0 | −28.6 ± 9.7 | −27.4 ± 6.1 | 0.40 | 0.61 | 0.02 | 0.62 |
| Cervical lordosis (neutral) (°) | 7.3 ± 11.0 | 19.7 ± 9.4 | 3.6 ± 9.6 | 7.1 ± 9.4 | 0.40 | 0.27 | 0.77 | 0.09 |
| Cervical lordosis (extension) (°) | 27.7 ± 11.7 | 42.7 ± 5.2 | 33.6 ± 11.7 | 44.1 ± 12.3 | 0.20 | <0.05 | 0.69 | 0.77 |
| Cervical range of motion (°) | 42.0 ± 7.1 | 66.3 ± 11.1 | 62.2 ± 12.2 | 71.5 ± 13.1 | 0.10 | <0.05 | 0.02 | 0.55 |
| C7 sagittal vertical axis (mm) | −15.0 ± 28.2 | −4.3 ± 34.4 | −12.1 ± 23.3 | −13.6 ± 24.8 | 1.00 | 0.73 | 1.00 | 0.55 |
| C2–7 sagittal vertical axis (mm) | 28.7 ± 11.5 | 14.7 ± 6.3 | 31.6 ± 11.4 | 18.4 ± 8.1 | 0.40 | <0.01 | 0.69 | 0.62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Funao, H.; Isogai, N.; Otomo, N.; Yamanouchi, K.; Mizukoshi, R.; Fujita, N.; Ebata, S.; Ishii, K.; Yagi, M. Clinical Results after Release of Sternocleidomastoid Muscle Surgery for Neglected Congenital Muscular Torticollis—Unipolar vs. Bipolar Release Surgery. J. Clin. Med. 2024, 13, 131. https://doi.org/10.3390/jcm13010131
Funao H, Isogai N, Otomo N, Yamanouchi K, Mizukoshi R, Fujita N, Ebata S, Ishii K, Yagi M. Clinical Results after Release of Sternocleidomastoid Muscle Surgery for Neglected Congenital Muscular Torticollis—Unipolar vs. Bipolar Release Surgery. Journal of Clinical Medicine. 2024; 13(1):131. https://doi.org/10.3390/jcm13010131
Chicago/Turabian StyleFunao, Haruki, Norihiro Isogai, Nao Otomo, Kento Yamanouchi, Ryo Mizukoshi, Naruhito Fujita, Shigeto Ebata, Ken Ishii, and Mitsuru Yagi. 2024. "Clinical Results after Release of Sternocleidomastoid Muscle Surgery for Neglected Congenital Muscular Torticollis—Unipolar vs. Bipolar Release Surgery" Journal of Clinical Medicine 13, no. 1: 131. https://doi.org/10.3390/jcm13010131
APA StyleFunao, H., Isogai, N., Otomo, N., Yamanouchi, K., Mizukoshi, R., Fujita, N., Ebata, S., Ishii, K., & Yagi, M. (2024). Clinical Results after Release of Sternocleidomastoid Muscle Surgery for Neglected Congenital Muscular Torticollis—Unipolar vs. Bipolar Release Surgery. Journal of Clinical Medicine, 13(1), 131. https://doi.org/10.3390/jcm13010131






