A Scoping Review of Measurement Tools Evaluating Awareness and Disease-Related Knowledge in Peripheral Arterial Disease Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Selection Process
2.4. Data Extraction and Synthesis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Critical Appraisal of Identified Instruments
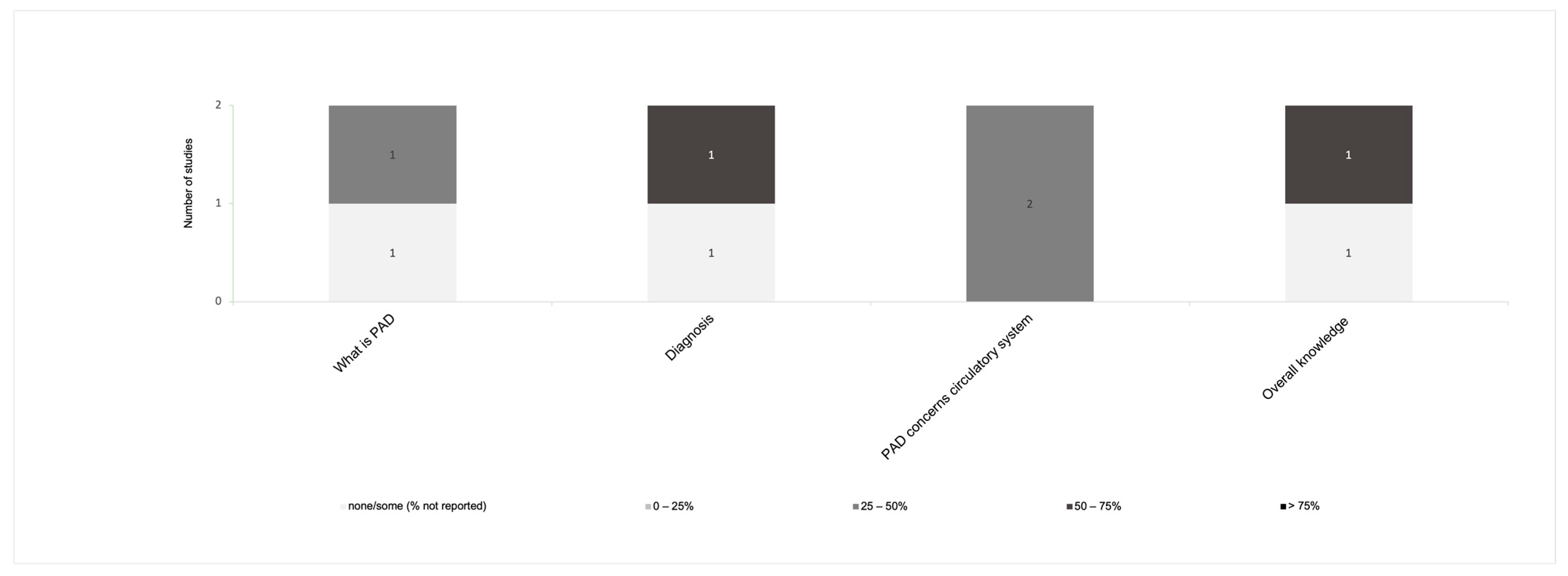
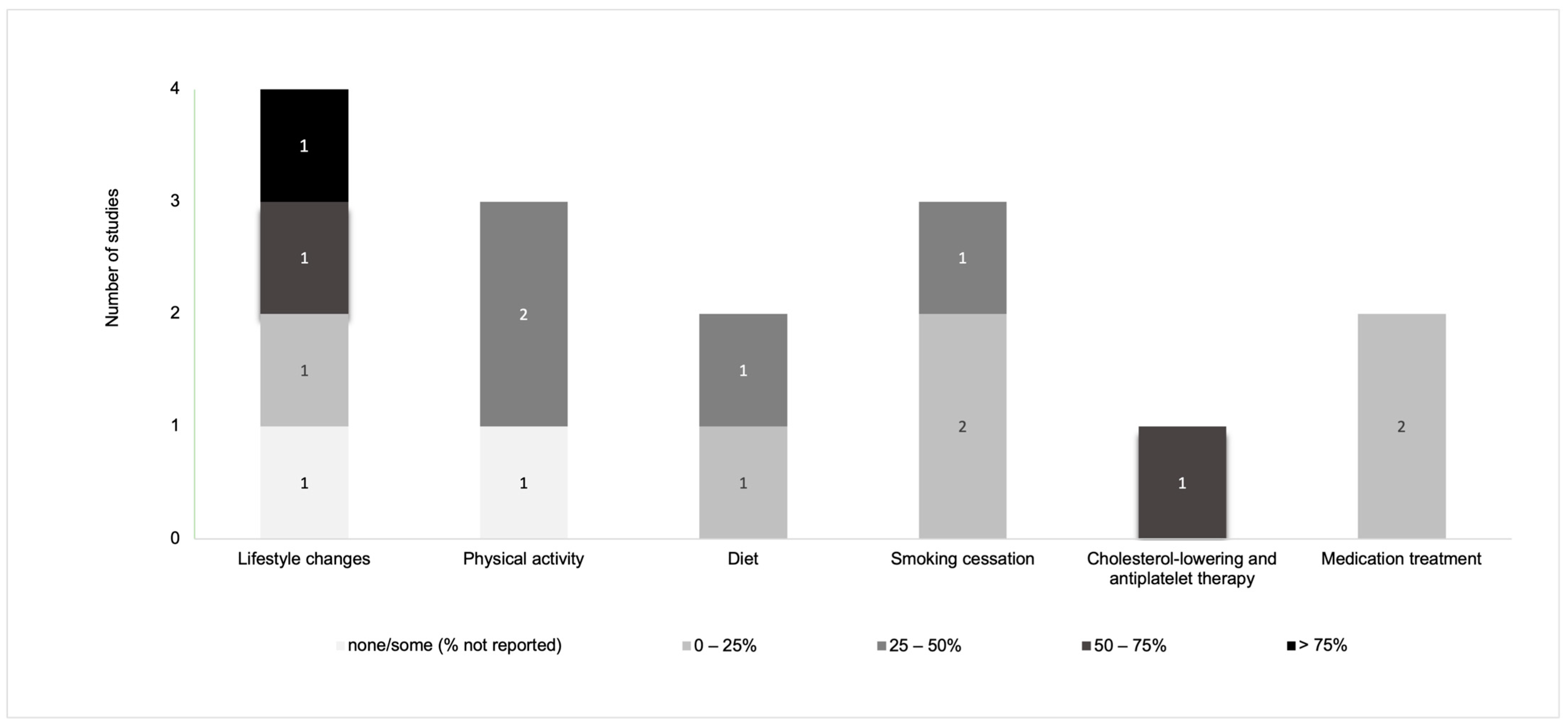
3.4. Measurement of Disease-Related Knowledge and Awareness in PAD Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fowkes, F.G.R.; Rudan, D.; Rudan, I.; Aboyans, V.; Denenberg, J.O.; McDermott, M.M.; Norman, P.E.; Sampson, U.K.A.; Williams, L.J.; Mensah, G.A.; et al. Comparison of Global Estimates of Prevalence and Risk Factors for Peripheral Artery Disease in 2000 and 2010: A Systematic Review and Analysis. Lancet 2013, 382, 1329–1340. [Google Scholar] [CrossRef] [PubMed]
- National Clinical Guideline Centre. Lower Limb Peripheral Arterial Disease: Diagnosis and Management; NICE Clinical Guidelines; National Clinical Guideline Centre: London, UK, 2012. [Google Scholar]
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients with Lower Extremity Peripheral Artery Disease: Executive Summary. Vasc. Med. 2017, 22, NP1–NP43. [Google Scholar] [CrossRef] [PubMed]
- Cronin, C.T.; McCartan, D.P.; McMonagle, M.; Cross, K.S.; Dowdall, J.F. Peripheral Artery Disease: A Marked Lack of Awareness in Ireland. Eur. J. Vasc. Endovasc. Surg. 2015, 49, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, A.T.; Murphy, T.P.; Lovell, M.B.; Twillman, G.; Treat-Jacobson, D.; Harwood, E.M.; Mohler, E.R.; Creager, M.A.; Hobson, R.W.; Robertson, R.M.; et al. Gaps in Public Knowledge of Peripheral Arterial Disease: The First National PAD Public Awareness Survey. Circulation 2007, 116, 2086–2094. [Google Scholar] [CrossRef] [PubMed]
- Lovell, M.; Harris, K.; Forbes, T.; Twillman, G.; Abramson, B.; Criqui, M.H.; Schroeder, P.; Mohler, E.R.; Hirsch, A.T. Peripheral Arterial Disease: Lack of Awareness in Canada. Can. J. Cardiol. 2009, 25, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Weragoda, J.; Weerasinghe, M.C.; Seneviratne, R.; Wijeyaratne, S.M. Gaps in Awareness of Peripheral Arterial Disease in Sri Lanka: A Cross Sectional Study. BMC Public Health 2016, 6, 1073. [Google Scholar] [CrossRef] [PubMed]
- Bridgwood, B.M.; Nickinson, A.T.O.; Houghton, J.S.M.; Pepper, C.J.; Sayers, R.D. Knowledge of Peripheral Artery Disease: What Do the Public, Healthcare Practitioners, and Trainees Know? Vasc. Med. 2020, 25, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Schwarcz, A.I.; Quijano, A.; Olin, J.W.; Ostfeld, R.J. Internal Medicine Interns Have a Poor Knowledge of Peripheral Artery Disease. Angiology 2012, 63, 597–602. [Google Scholar] [CrossRef]
- Correa-Vázquez, E.J.; de Jesús-Sosa, M.A.; Reyes-Claudio, K.M.; Chévere-Rivera, K. Cardiologist’s Knowledge of the Physiotherapy and the Challenges of Referring Patients with Peripheral Arterial Disease in Puerto Rico. Fisioterapia 2019, 41, 65–72. [Google Scholar] [CrossRef]
- Byskosh, N.; Pamulapati, V.; Xu, S.; Vavra, A.K.; Hoel, A.W.; Tian, L.; McDermott, M.M.; Butt, Z.; Ho, K.J. Identifying Gaps in Disease Knowledge among Patients with Peripheral Artery Disease. J. Vasc. Surg. 2022, 75, 1358–1368. [Google Scholar] [CrossRef]
- AlHamzah, M.; Eikelboom, R.; Hussain, M.A.; Syed, M.H.; Salata, K.; Wheatcroft, M.; Verma, S.; Al-Omran, M. Knowledge Gap of Peripheral Artery Disease Starts in Medical School. J. Vasc. Surg. 2019, 70, 241–245. [Google Scholar] [CrossRef] [PubMed]
- AlHamzah, M.; Eikelboom, R.; Syed, M.; Salata, K.; Hussain, M.A.; Al-Omran, M. Physicians’ Peripheral Arterial Disease Knowledge Gap Starts in Medical School. J. Vasc. Surg. 2017, 63, e84. [Google Scholar] [CrossRef][Green Version]
- Thomas, R.J.; Beatty, A.L.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation: A Scientific Statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019, 140, e69–e89. [Google Scholar] [CrossRef] [PubMed]
- Balady, G.J.; Williams, M.A.; Ades, P.A.; Bittner, V.; Comoss, P.; Foody, J.M.; Franklin, B.; Sanderson, B.; Southard, D. Core Components of Cardiac Rehabilitation/Secondary Prevention Programs: 2007 Update: A Scientific Statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils O. Circulation 2007, 115, 2675–2682. [Google Scholar] [CrossRef] [PubMed]
- Abramson, B.L.; Al-Omran, M.; Anand, S.S.; Albalawi, Z.; Coutinho, T.; de Mestral, C.; Dubois, L.; Gill, H.L.; Greco, E.; Guzman, R.; et al. Canadian Cardiovascular Society 2022 Guidelines for Peripheral Arterial Disease. Can. J. Cardiol. 2022, 38, 560–587. [Google Scholar] [CrossRef] [PubMed]
- Bolt, L.J.J.; Jacobs, M.; Sigterman, T.A.; Krasznai, A.G.; Sikkink, C.; Schurink, G.W.H.; Bouwman, L.H. Assessment of Behavioral Determinants Influencing Success of Supervised Exercise Therapy in Patients with Intermittent Claudication: A Cross Sectional Survey. Physiol. Behav. 2020, 215, 112732. [Google Scholar] [CrossRef]
- Veronovici, N.R.; Lasiuk, G.C.; Rempel, G.R.; Norris, C.M. Discharge Education to Promote Self-Management Following Cardiovascular Surgery: An Integrative Review. Eur. J. Cardiovasc. Nurs. 2014, 13, 22–31. [Google Scholar] [CrossRef]
- Shi, W.; Ghisi, G.L.M.; Zhang, L.; Hyun, K.; Pakosh, M.; Gallagher, R. Systematic Review, Meta-Analysis and Meta-Regression to Determine the Effects of Patient Education on Health Behaviour Change in Adults Diagnosed with Coronary Heart Disease. J. Clin. Nurs. 2023, 32, 5300–5327. [Google Scholar] [CrossRef]
- Krist, A.H.; Tong, S.T.; Aycock, R.A.; Longo, D.R. Engaging Patients in Decision-Making and Behavior Change to Promote Prevention. Stud. Health Technol. Inform. 2017, 240, 284–302. [Google Scholar] [CrossRef]
- Lokin, J.L.C.; Hengeveld, P.J.; Conijn, A.P.; Nieuwkerk, P.T.; Koelemay, M.J.W. Disease Understanding in Patients with Intermittent Claudication: A Qualitative Study. J. Vasc. Nurs. 2015, 33, 112–118. [Google Scholar] [CrossRef]
- Wann-Hansson, C.; Wennick, A. How Do Patients with Peripheral Arterial Disease Communicate Their Knowledge about Their Illness and Treatments? A Qualitative Descriptive Study. BMC Nurs. 2016, 15, 29. [Google Scholar] [CrossRef] [PubMed]
- Mehta, A.; Dhindsa, D.S.; Hooda, A.; Nayak, A.; Massad, C.S.; Rao, B.; Makue, L.F.; Rajani, R.R.; Alabi, O.; Quyyumi, A.A.; et al. Premature Atherosclerotic Peripheral Artery Disease: An Underrecognized and Undertreated Disorder with a Rising Global Prevalence. Trends Cardiovasc. Med. 2021, 31, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019); Cochrane. 2019. Available online: www.Training.Cochrane.Org/Handbook (accessed on 15 December 2023).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without Meta-Analysis (SWiM) in Systematic Reviews: Reporting Guideline. Br. Med. J. 2020, 2020, 368. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN Study Reached International Consensus on Taxonomy, Terminology, and Definitions of Measurement Properties for Health-Related Patient-Reported Outcomes. J. Clin. Epidemiol. 2010, 63, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT). McGill. 2018, pp. 1–11. Available online: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf (accessed on 15 December 2023).
- Keelan, S.; Foley, N.; Healy, D.; Kheirelseid, E.; McHugh, S.; Moneley, D.; Naughton, P. Poor Patient Awareness of Peripheral Arterial Disease, It Is Time to Optimize the Clinical Visit. Surgeon 2021, 20, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, P.A.; Gulati, V.; Mavor, A.I.D.; Gough, M.J.; Homer-Vanniasinkam, S. Risk Factor Awareness in Patients with Peripheral Arterial Disease. J. Cardiovasc. Surg. 2007, 48, 735. [Google Scholar]
- Willigendael, E.M.; Teijink, J.A.W.; Bartelink, M.L.; Boiten, J.; Moll, F.L.; Büller, H.R.; Prins, M.H. Peripheral Arterial Disease: Public and Patient Awareness in the Netherlands. Eur. J. Vasc. Endovasc. Surg. 2004, 27, 622–628. [Google Scholar] [CrossRef]
- Udelnow, A.; Hecht, V.; Buschmann, I.; Wilbrandt, C.; Barth, U.; Meyer, F.; Halloul, Z. Disease Knowledge and Patient Education Are Key Players for a Better Quality of Life in Vascular Surgery Patients. Eur. Surg. 2020, 53, 75–83. [Google Scholar] [CrossRef]
- Builyte, I.U.; Baltrunas, T.; Butkute, E.; Srinanthalogen, R.; Skrebunas, A.; Urbonavicius, S.; Rucinskas, K. Peripheral Artery Disease Patients Are Poorly Aware of Their Disease. Scand. Cardiovasc. J. 2019, 53, 373–378. [Google Scholar] [CrossRef]
- El Jang, D.; Jang, Y.S.; Oh, E.G.; Ko, Y.G. Factors Associated with Health-Related Quality of Life in Patients with Peripheral Arterial Disease. Korean J. Adult Nurs. 2018, 30, 266–276. [Google Scholar] [CrossRef]
- Provance, J.B.; Spertus, J.A.; Decker, C. Abstract 15970: Examining Patients’ Knowledge with Regards to Peripheral Artery Disease Treatments and Outcomes: Insights from the PORTRAIT Registry. Circulation 2018, 138, A15970. [Google Scholar]
- Martínez, L.G.; Gutiérrez, R.F.; Gallego, A.G.; García, A.P.; Vega, M.S.; Calvo, A.Z. Diseño, Validación y Aplicación Clínica de Un Cuestionario de Conocimiento (ConocEAP) de Los Pacientes Con Enfermedad Arterial Periférica. Angiología 2017, 69, 4–11. [Google Scholar] [CrossRef]
- Vasaroangrong, T.; Thosingha, O.; Riegel, B.; Ruangsetakit, C.; Viwatwongkasem, C. Factors Influencing Prehospital Delay Time among Patients with Peripheral Arterial Occlusive Disease. Eur. J. Cardiovasc. Nurs. 2016, 15, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Owens, M.; Mohan, H.; Moloney, M.A.; Roche-Nagle, G.; Baker, J.; Sheehan, S.; Mehigan, D.; Barry, M. Patient Knowledge of Peripheral Vascular Disease in an Outpatient Setting: An Achilles Heel? Ir. Med. J. 2013, 106, 116–118. [Google Scholar]
- McDermott, M.M.; Mandapat, A.L.; Moates, A.; Albay, M.; Chiou, E.; Celic, L.; Greenland, P. Knowledge and Attitudes Regarding Cardiovascular Disease Risk and Prevention in Patients with Coronary or Peripheral Arterial Disease. Arch. Intern. Med. 2003, 163, 2157–2162. [Google Scholar] [CrossRef] [PubMed]
- Gorely, T.; Crank, H.; Humphreys, L.; Nawaz, S.; Tew, G.A. “Standing Still in the Street”: Experiences, Knowledge and Beliefs of Patients with Intermittent Claudication—A Qualitative Study. J. Vasc. Nurs. 2015, 33, 4–9. [Google Scholar] [CrossRef]
- Striberger, R.; Axelsson, M.; Zarrouk, M.; Kumlien, C. Illness perceptions in patients with peripheral arterial disease: A systematic review of qualitative studies. Int. J. Nurs. Stud. 2021, 116, 103723. [Google Scholar] [CrossRef]
- Kolossváry, E.; Farkas, K.; Karahan, O.; Golledge, J.; Schernthaner, G.H.; Karplus, T.; Bernardo, J.J.; Marschang, S.; Abola, M.T.; Heinzmann, M.; et al. The importance of socio-economic determinants of health in the care of patients with peripheral artery disease: A narrative review from VAS. Vasc. Med. 2023, 28, 241–243. [Google Scholar] [CrossRef]
- Saw, S.M.; Ng, T.P. The Design and Assessment of Questionnaires in Clinical Research. Singap. Med. J. 2001, 42, 131–135. [Google Scholar]
- Grady, P.L.; Gough, L.L. Self-Management: A Comprehensive Approach to Management of Chronic Conditions. Am. J. Public Health 2014, 104, e25–e31. [Google Scholar] [CrossRef] [PubMed]
- Peerson, A.; Saunders, M. Men’s Health Literacy: Advancing Evidence and Priorities. Crit. Public Health 2009, 19, 441–456. [Google Scholar] [CrossRef]
- Ghisi, G.L.d.M.; Durieux, A.; Manfroi, W.C.; Herdy, A.H.; de Carvalho, T.; Andrade, A.; Benetti, M. Construction and Validation of the CADE-Q for Patient Education in Cardiac Rehabilitation Programs. Arq. Bras. De Cardiol. 2010, 94, 813–822. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ghisi, G.L.D.M.; Aultman, C.; Konidis, R.; Foster, E.; Sandison, N.; Alavinia, M.; Sarin, M.; Oh, P. Development and Validation of the DiAbeTes Education Questionnaire (DATE-Q) to Measure Knowledge among Diabetes and Prediabetes Patients Attending Cardiac Rehabilitation Programs. J. Cardiopulm. Rehabil. Prev. 2021, 41, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, R.Z.; Bonin, C.D.B.; Martins, E.T.C.; Pereira Junior, M.; Ghisi, G.L.d.M.; de Macedo, K.R.P.; Benetti, M. Development and Psychometric Validation of HIPER-Q to Assess Knowledge of Hypertensive Patients in Cardiac Rehabilitation. Arq. Bras. Cardiol. 2017, 110, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Abaraogu, U.O.; Dall, P.M.; Seenan, C.A. The Effect of Structured Patient Education on Physical Activity in Patients with Peripheral Arterial Disease and Intermittent Claudication: A Systematic Review. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 58–68. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat. Rev. Cardiol. 2022, 19, 180–194. [Google Scholar] [CrossRef]
- Dibben, G.O.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.D.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease: A meta-analysis. Eur. Heart J. 2023, 44, 452–469. [Google Scholar] [CrossRef]
- Yasu, T. Comprehensive cardiac rehabilitation program for peripheral arterial diseases. J. Cardiol. 2022, 80, 303–305. [Google Scholar] [CrossRef]
- Anghel, R.; Adam, C.A.; Marcu, D.T.M.; Mitu, O.; Mitu, F. Cardiac Rehabilitation in Patients with Peripheral Artery Disease—A Literature Review in COVID-19 Era. J. Clin. Med. 2022, 11, 416. [Google Scholar] [CrossRef]
- Cowie, A.; Buckley, J.; Doherty, P.; Furze, G.; Hayward, J.; Hinton, S.; Jones, J.; Speck, L.; Dalal, H.; Mills, J.; et al. Standards and core components for cardiovascular disease prevention and rehabilitation. Heart 2019, 105, 510–515. [Google Scholar] [CrossRef] [PubMed]




| Author Year Country | Study Design Participants Setting Quality | Sample Size Mean Age (SD or Range) % Male Ethnicity | Method Used for Outcomes Measurement |
|---|---|---|---|
| Wann-Hansson and Wennick ♦ 2016 [22] Sweden | Qualitative Patients with PAD undergoing vascular intervention Vascular centre 5/5 | 21 70.0 (range 50–81) years old 42.9% male NR | Focus groups Themes: Knowledge about vascular disease, risk factors and treatment |
| Gorely et al. ♦ 2015 [40] United Kingdom | Qualitative Patients with PAD and IC Hospital 5/5 | 24 71.0 (8.0) years old 71.0% male Caucasian (100%) | Focus groups Themes: experiences of living with PAD/IC, attitudes and beliefs about PAD/IC, educational needs of people with PAD/IC, attitudes and beliefs about physical activity/exercise, levers and barriers for exercise behaviour change, opinions of behaviour change interventions, particularly structured education |
| Lokin et al. ♦ 2015 [21] The Netherlands | Qualitative Patients with PAD and IC Multiple Hospital 5/5 | 19 60.8 (6.7) years old 52.6% male NR | Semi structured individual interviews Themes: Knowledge about disease, aetiology and lifestyle |
| Keelan et al. ♦ 2021 [29] Ireland | Cross-sectional VC, CVC and the ED patients Multiple Hospital 3/5 | 49 67.1 (9.7) years old 59.0% male NR | Questionnaire (structure NR) Number of items NR Awareness about disease entity, PAD risk factors and potential consequences of PAD if left untreated |
| Byskosh et al. ♦ 2022 [11] United States | Cross-sectional Patients with PAD Vascular surgery clinic 3/5 | 109 69.4 (11.0) years old 60.6% male Caucasian 56.9%/African American 34.9%/Other 8.3% | Questionnaire (multiple-choice questions) 44 items (score range 0–100%) Knowledge about general risk factors and potential consequences of PAD, awareness of own medical history and PAD education preferences. |
| Udelnow et al. ♦ 2020 [32] Germany | Prospective cohort study Patients with PAD undergoing vascular intervention Hospital 3/5 | 198 NR NR NR | Questionnaire (correct/incorrect) 20 items (score range 0–20) knowledge about the disease, self-information, smoking habits, and treatment expectations |
| Bolt et al. ♦ 2020 [17] The Netherlands | Cross-sectional survey Patients with PAD Medical centre 2/5 | 108 72.0 (range 53–92) years old 57.0% male NR | Questionnaire (5-point Likert-scale) 17 items (score range NR) 10 items regarding: knowledge (19 a/b, 20), risk perception (21 a/b/c), attitude (22/23), self-efficacy (24) and intention towards physical exercise (25). |
| Builyte et al. ♦ 2019 [33] Denmark | Cross-sectional Patients PAD or Coronary Artery Disease Hospital 4/5 | 63 PAD 68.3 (11.8) years old 71.0% male NR | Questionnaire (multiple-choice questions) 14 items (score range NR) knowledge about of risk factors for PAD and Coronary Artery Disease, consequences, severity and other non-vascular illnesses |
| El Jang et al. # 2018 [34] Korea | Cross-sectional Patients with PAD Hospital and outpatient clinic 3/5 | 104 66.4 (13.3) years old 92.3% male NR | Questionnaire (correct/incorrect/‘I don’t know’) 15 items (score range 0–15) knowledge about definition and characteristics of PAD, management (exercise, diet, smoking cessation), treatment, and risk factors |
| Provance et al. * 2018 [35] United States | Cross-sectional Patients with PAD and IC Vascular clinics 0/5 | 797 69.2 (8.7) years old 55.2% male NR | Questionnaire (correct, incorrect, and “not sure”) Items NR Knowledge about PAD treatment options |
| Martínez et al. + 2017 [36] Spain | Cross-sectional Post-Angiology and Vascular patients. Hospital 3/5 | 120 72.0 (13.0) years old 79.0% male NR | Questionnaire (true/false) 24 items (score range 0–24) Knowledge about disease, risk factors, therapeutic regimen, pharmacotherapy and warning signs |
| Vasaroangrong et al. ♦ 2016 [37] Thailand | Cross-sectional Patients with PAD Outpatient clinic 2/5 | 212 66.0 (12.6) years old 59.9% male NR | Questionnaire (yes/no) 16 items (score range NR) Knowledge about PAD symptoms (seven items), risk factors (five items), and the effects of PAD (four items) |
| Owens et al. * 2013 [38] Ireland | Cross-sectional Patients with PAD Hospital 0/5 | 97 Age distribution (years): 18–34 (3.0%); 35–54 (4.0%); 45–54 (7.1%); 55–65 (26.3%); 65–74 (37.0%); >75 (22.2%) 54.6% male NR | Questionnaire (NR) Items NR Knowledge about understanding of peripheral vascular disease, risk factors, health improvement strategies, exercise and risk of other vascular disease |
| Coughlin et al. ♦ 2007 [30] United Kingdom | Cross-sectional Patients with PAD Vascular surgery department 3/5 | 70 72.0 (range 42–89) years old 70.0% male NR | Questionnaire (open and multiple-choice questions) 5 items (score range NR) Knowledge about risk factors and prevention/treatment |
| Willigendael et al. ♦ 2004 [31] The Netherlands | Cross-sectional Patients with PAD and general population Netherlands database 3/5 | 281 Age distribution (years): 35–44 (7.0%) 45–54 (19.0%) 55–64 (23.0%) > 64 (51.0%) 49.0% male NR | Questionnaire (open and multiple-choice questions) Items NR Knowledge about risk factors, medical advice and treatment |
| McDermott et al. ♦ 2003 [39] United States | Cross-sectional Patients with PAD or Coronary Artery Disease or no disease Vascular Laboratories and Vascular Centre 2/5 | 136 70.2 (8.1) years old 52.9% male African American: 15.4% | Questionnaire (5-point Likert-scale) 3 sections (score range NR) Knowledge about health behaviour regarding CVD prevention; risk of heart disease, stroke, and death; importance of specific CVD risk factor interventions |
| Author (Year) | Content Validity | Internal Consistency | Criterion Validity | Construct Validity | Reproducibility Agreement | Reproducibility Reliability | Responsiveness | Floor and Ceiling Effect | Interpretability |
|---|---|---|---|---|---|---|---|---|---|
| Keelan (2021) [29] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| Byskosh (2022) [11] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| Udelnow (2020) [32] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| Bolt (2020) [17] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| Builyte (2019) [33] | NP | appropriate | NP | NP | NP | NP | NP | NP | NP |
| Da El et al. (2018) [34] | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Provance (2018) [35] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| Martinez (2017) [36] | NP | appropriate | NP | NP | NP | NP | NP | NP | NP |
| Vasaroangrong (2016) [37] | appropriate | NP | NP | NP | NP | appropriate | NP | NP | NP |
| Owens (2013) [38] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| Coughlin (2007) [30] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| Willigendael (2004) [31] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
| McDermott (2003) [39] | NP | NP | NP | NP | NP | NP | NP | NP | NP |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felix, C.M.d.M.; Pereira, D.A.G.; Pakosh, M.; Silva, L.P.d.; Ghisi, G.L.d.M. A Scoping Review of Measurement Tools Evaluating Awareness and Disease-Related Knowledge in Peripheral Arterial Disease Patients. J. Clin. Med. 2024, 13, 107. https://doi.org/10.3390/jcm13010107
Felix CMdM, Pereira DAG, Pakosh M, Silva LPd, Ghisi GLdM. A Scoping Review of Measurement Tools Evaluating Awareness and Disease-Related Knowledge in Peripheral Arterial Disease Patients. Journal of Clinical Medicine. 2024; 13(1):107. https://doi.org/10.3390/jcm13010107
Chicago/Turabian StyleFelix, Carolina Machado de Melo, Danielle Aparecida Gomes Pereira, Maureen Pakosh, Lilian Pinto da Silva, and Gabriela Lima de Melo Ghisi. 2024. "A Scoping Review of Measurement Tools Evaluating Awareness and Disease-Related Knowledge in Peripheral Arterial Disease Patients" Journal of Clinical Medicine 13, no. 1: 107. https://doi.org/10.3390/jcm13010107
APA StyleFelix, C. M. d. M., Pereira, D. A. G., Pakosh, M., Silva, L. P. d., & Ghisi, G. L. d. M. (2024). A Scoping Review of Measurement Tools Evaluating Awareness and Disease-Related Knowledge in Peripheral Arterial Disease Patients. Journal of Clinical Medicine, 13(1), 107. https://doi.org/10.3390/jcm13010107







