Comparison of Lactate Clearance with Established Risk Assessment Tools in Predicting Outcomes in Acute Upper Gastrointestinal Bleeding
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Baseline Characteristics and Outcomes
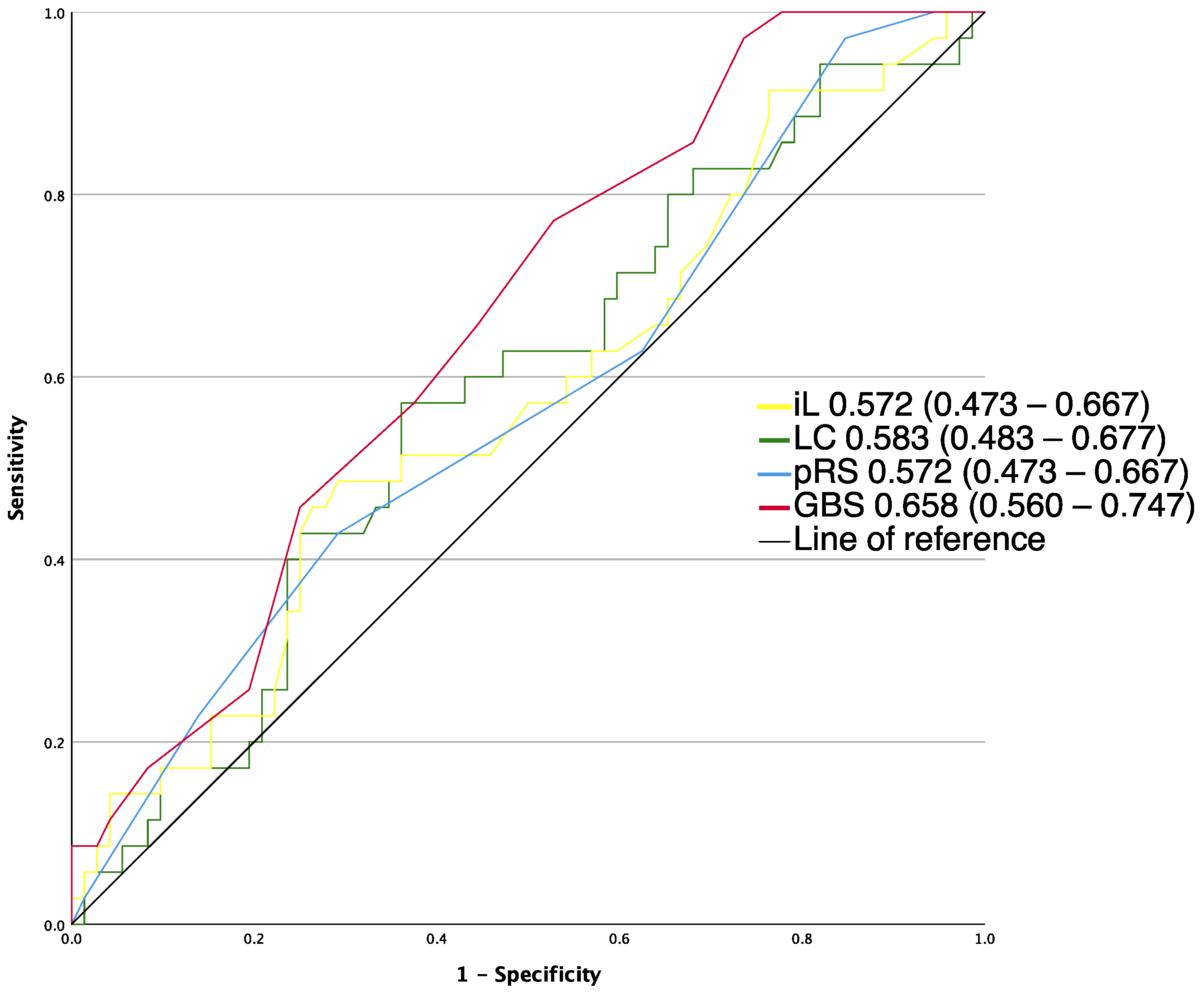
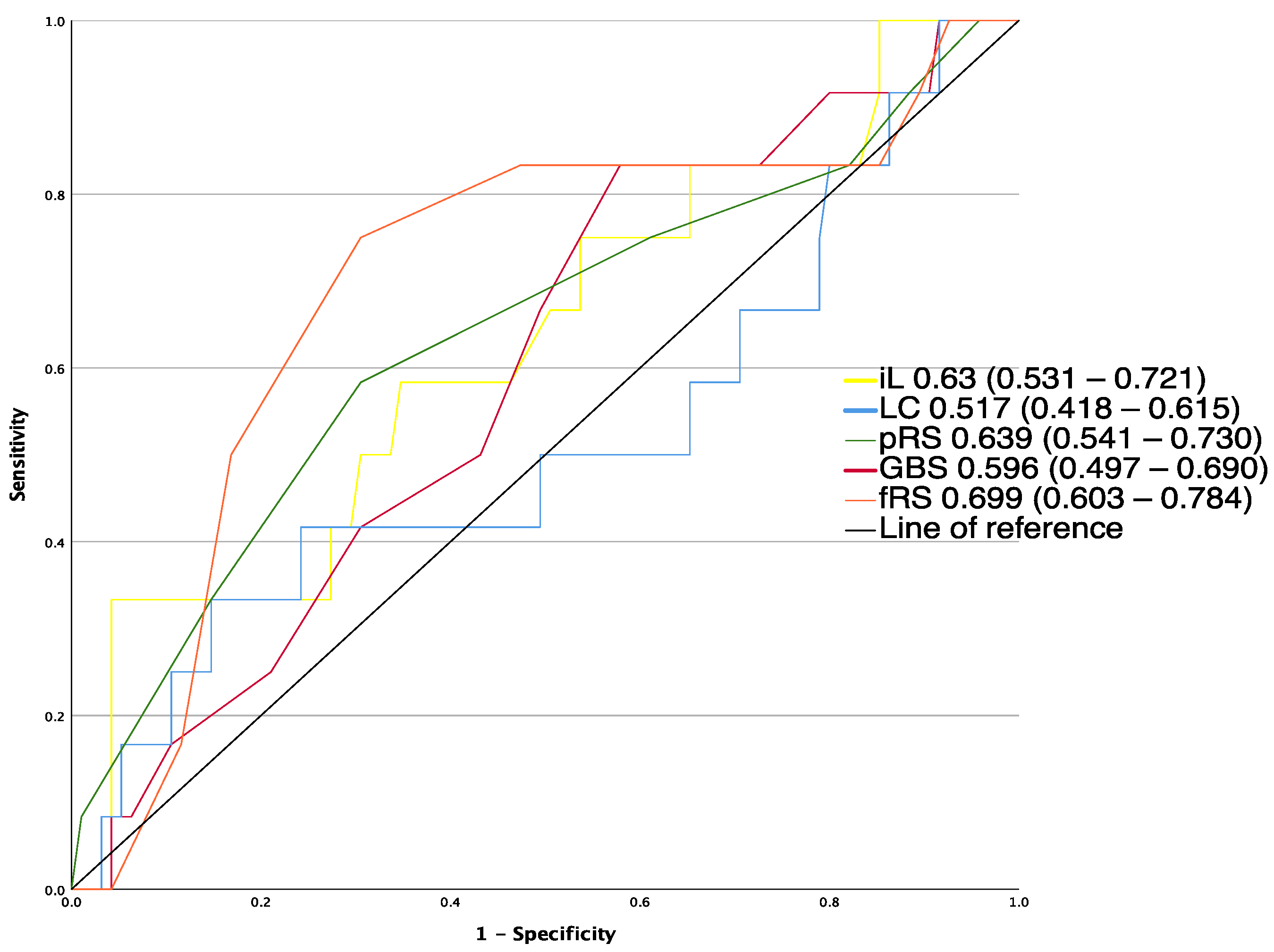
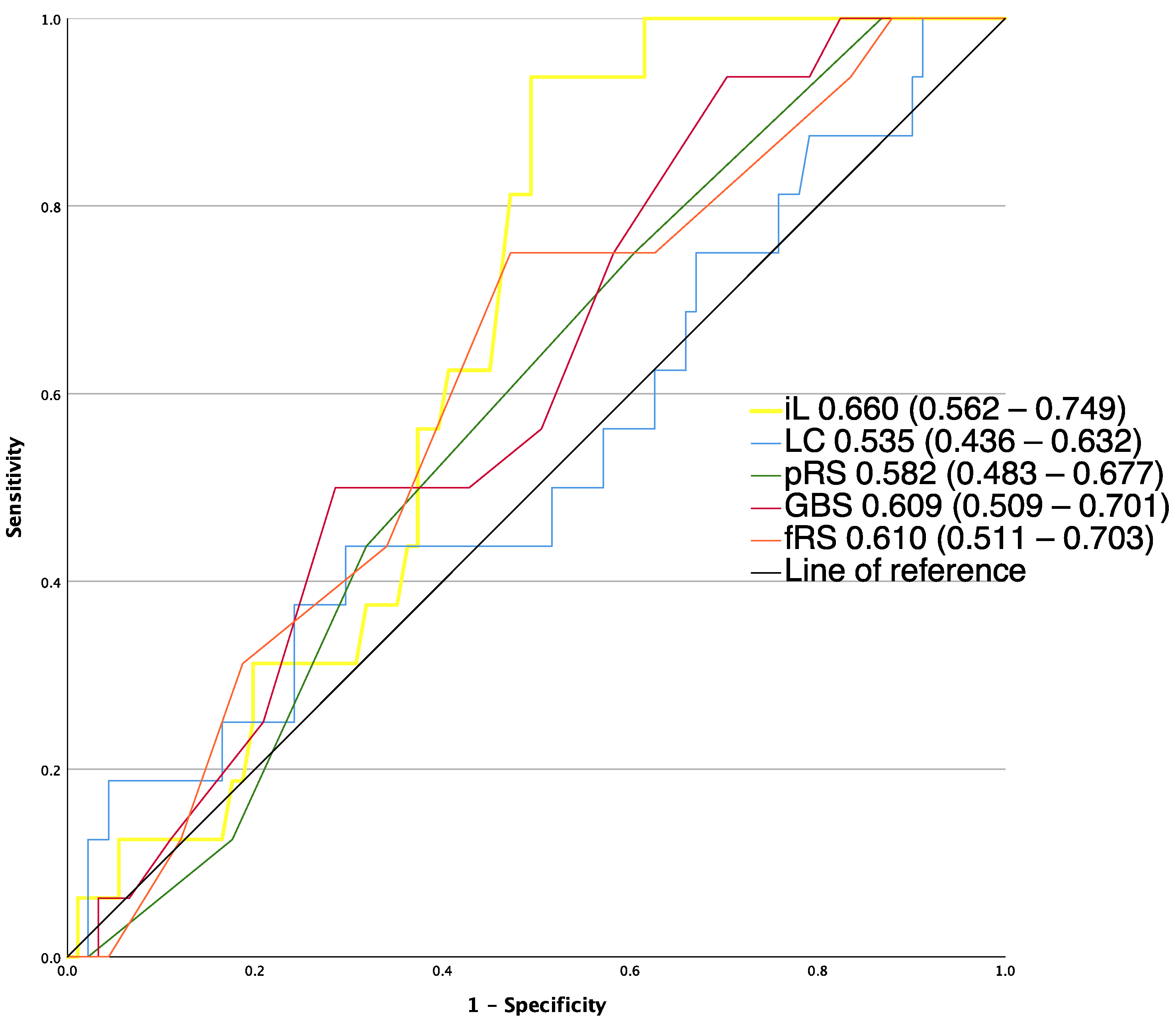
3.2. Performance of Risk Assessment Tools in Predicting Intervention, Mortality and Rebleeding
3.3. Performance of Bleeding Risk Scoring Systems at Optimal Cutoffs
3.4. Factors Associated with the Need for Hemostatic Intervention
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crooks, C.; Card, T.; West, J. Reductions in 28-day mortality following hospital admission for upper gastrointestinal hemorrhage. Gastroenterology 2011, 141, 62–70. [Google Scholar] [CrossRef]
- Hearnshaw, S.A.; Logan, R.F.A.; Lowe, D.; Travis, S.P.L.; Murphy, M.F.; Palmer, K.R. Acute upper gastrointestinal bleeding in the UK: Patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut 2011, 60, 1327–1335. [Google Scholar] [CrossRef]
- Gralnek, I.M.; Stanley, A.J.; Morris, A.J.; Camus, M.; Lau, J.; Lanas, A.; Van Hooft, J.E. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2021. Endoscopy 2021, 53, 300–332. [Google Scholar] [CrossRef]
- Laine, L.; Barkun, A.N.; Saltzman, J.R.; Martel, M.; Leontiadis, G.I. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am. J. Gastroenterol. 2021, 116, 899–917. [Google Scholar] [CrossRef]
- Rockall, T.A.; Logan, R.F.; Devlin, H.B.; Northfield, T.C. Risk assessment after acute upper gastrointestinal haemorrhage. Gut 1996, 38, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Blatchford, O.; Murray, W.R.; Blatchford, M. A risk score to predict need for treatment for uppergastrointestinal haemorrhage. Lancet 2000, 356, 1318–1321. [Google Scholar] [CrossRef] [PubMed]
- Stanley, A.J.; Ashley, D.; Dalton, H.R.; Mowat, C.; Gaya, D.R.; Thompson, E.; Murray, W. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: Multicentre validation and prospective evaluation. Lancet 2009, 373, 42–47. [Google Scholar] [CrossRef]
- Liang, P.S.; Saltzman, J.R. A National Survey on the Initial Management of Upper Gastrointestinal Bleeding. J. Clin. Gastroenterol. 2014, 48, e93–e98. [Google Scholar] [CrossRef]
- Baxter, J.; Cranfield, K.R.; Clark, G.; Harris, T.; Bloom, B.; Gray, A.J. Do lactate levels in the emergency department predict outcome in adult trauma patients? A systematic review. J. Trauma. Acute Care Surg. 2016, 81, 555–566. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Levy, M. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef] [PubMed]
- Ko, B.S.; Kim, Y.-J.; Jung, D.H.; Sohn, C.H.; Seo, D.W.; Lee, Y.-S.; Lim, K.S.; Jung, H.-Y.; Kim, W.Y. Early Risk Score for Predicting Hypotension in Normotensive Patients with Non-Variceal Upper Gastrointestinal Bleedin. J. Clin. Med. 2019, 8, 37. [Google Scholar] [CrossRef]
- El-Kersh, K.; Chaddha, U.; Sinha, R.S.; Saad, M.; Guardiola, J.; Cavallazzi, R. Predictive Role of Admission Lactate Level in Critically Ill Patients with Acute Upper Gastrointestinal Bleeding. J. Emerg. Med. 2015, 49, 318–325. [Google Scholar] [CrossRef]
- Horvatits, T.; Mahmud, N.; Serper, M.; Seiz, O.; Reher, D.; Drolz, A.; Sarnast, N.; Gu, W.; Erasmus, H.P.; Allo, G.; et al. MELD-Lactate Predicts Poor Outcome in Variceal Bleeding in Cirrhosis. Dig. Dis. Sci. 2023, 68, 1042–1050. [Google Scholar] [CrossRef]
- Stokbro, L.A.; Schaffalitzky de Muckadell, O.B.; Laursen, S.B. Arterial lactate does not predict outcome better than existing risk scores in upper gastrointestinal bleeding. Scand. J. Gastroenterol. 2018, 53, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Wada, T.; Hagiwara, A.; Uemura, T.; Yahagi, N.; Kimura, A. Early lactate clearance for predicting active bleeding in critically ill patients with acute upper gastrointestinal bleeding: A retrospective study. Intern. Emerg. Med. 2016, 11, 737–743. [Google Scholar] [CrossRef]
- Kim, K.; Lee, D.H.; Lee, D.H.; Choi, Y.H.; Bae, S.J. Early lactate clearance for predicting outcomes in patients with gastrointestinal bleeding. Irish J. Med. Sci. 2022, 13, 1–7. [Google Scholar] [CrossRef]
- De Jonghe, B.; Cheval, C.; Misset, B.; Timsit, J.F.; Garrouste, M.; Montuclard, L.; Carlet, J. Relationship between blood lactate and early hepatic dysfunction in acute circulatory failure. J. Crit. Care 1999, 14, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Sterling, S.A.; Puskarich, M.A.; Jones, A.E. The effect of liver disease on lactate normalization in severe sepsis and septic shock: A cohort study. Clin. Exp. Emerg. Med. 2015, 2, 197–202. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Stanley, A.J.; Laine, L.; Dalton, H.R.; Ngu, J.H.; Schultz, M.; Abazi, R.; Laursen, S.B. Comparison of risk scoring systems for patients presenting with upper gastrointestinal bleeding: International multicentre prospective study. BMJ 2017, 356, i6432. [Google Scholar] [CrossRef]
- Zhang, Z.; Xu, X. Lactate clearance is a useful biomarker for the prediction of all-cause mortality in critically ill patients: A systematic review and meta-analysis*. Crit. Care Med. 2014, 42, 2118–2125. [Google Scholar] [CrossRef]
- Ryoo, S.M.; Lee, J.; Lee, Y.-S.; Lee, J.H.; Lim, K.S.; Huh, J.W.; Hong, S.-B.; Lim, C.-M.; Koh, Y.; Kim, W.Y. Lactate Level Versus Lactate Clearance for Predicting Mortality in Patients with Septic Shock Defined by Sepsis-3. Crit. Care Med. 2018, 46, e489–e495. [Google Scholar] [CrossRef]
- Lau, J.Y.; Yu, Y.; Tang, R.S.; Chan, H.C.; Yip, H.C.; Chan, S.M.; Sung, J.J. Timing of endoscopy for acute upper gastrointestinal bleeding. N. Engl. J. Med. 2020, 382, 1299–1308. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.L.; Wong, S.H.; Lau, L.H.; Lui, R.N.; Mak, J.W.; Tang, R.S.; Sung, J.J. Timing of endoscopy for acute upper gastrointestinal bleeding: A territory-wide cohort study. Gut 2022, 71, 1544–1550. [Google Scholar] [CrossRef]
- Levraut, J.; Ciebiera, J.-P.; Chave, S.; Rabary, O.; Jambou, P.; Carles, M.; Grimaud, D. Mild Hyperlactatemia in Stable Septic Patients Is Due to Impaired Lactate Clearance Rather Than Overproduction. Am. J. Respir. Crit. Care Med. 1998, 157, 1021–1026. [Google Scholar] [CrossRef] [PubMed]
- Luchette, F.A.; Jenkins, W.A.; Friend, L.A.; Su, C.; Fischer, J.E.; James, J.H. Hypoxia is not the sole cause of lactate production during shock. J. Trauma. 2002, 52, 415–419. [Google Scholar] [CrossRef]
- McCarter, F.D.; James, J.H.; Luchette, F.A.; Wang, L.; Friend, L.A.; King, J.-K.; Evans, J.M.; George, M.A.; Fischer, J.E. Adrenergic Blockade Reduces Skeletal Muscle Glycolysis and Na+, K+-ATPase Activity during Hemorrhage. J. Surg. Res. 2001, 99, 235–244. [Google Scholar] [CrossRef]
- Laursen, S.B.; Dalton, H.R.; Murray, I.A.; Michell, N.; Johnston, M.R.; Schultz, M.; Zhang, W. Performance of New Thresholds of the Glasgow Blatchford Score in Managing Patients with Upper Gastrointestinal Bleeding. Clin. Gastroenterol. Hepatol. 2015, 13, 115–121.e2. [Google Scholar] [CrossRef]
- Jimenez-Rosales, R.; Lopez-Tobaruela, J.M.; Lopez-Vico, M.; Ortega-Suazo, E.J.; Martinez-Cara, J.G.; Redondo-Cerezo, E. Performance of the New ABC and MAP(ASH) Scores in the Prediction of Relevant Outcomes in Upper Gastrointestinal Bleeding. J. Clin. Med. 2023, 12, 1085. [Google Scholar] [CrossRef]
- Laursen, S.B.; Hansen, J.M.; Schaffalitzky de Muckadell, O.B. The Glasgow Blatchford Score Is the Most Accurate Assessment of Patients with Upper Gastrointestinal Hemorrhage. Clin. Gastroenterol. Hepatol. 2012, 10, 1130–1135.e1. [Google Scholar] [CrossRef] [PubMed]
- Laursen, S.B.; Oakland, K.; Laine, L.; Bieber, V.; Marmo, R.; Redondo-Cerezo, E.; Stanley, A.J. ABC score: A new risk score that accurately predicts mortality in acute upper and lower gastrointestinal bleeding: An international multicentre study. Gut 2021, 70, 707–716. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Cerezo, E.; Vadillo-Calles, F.; Stanley, A.J.; Laursen, S.; Laine, L.; Dalton, H.R.; Ngu, J.H.; Schultz, M.; Jiménez-Rosales, R. MAP(ASH): A new scoring system for the prediction of intervention and mortality in upper gastrointestinal bleeding. J. Gastroenterol. Hepatol. 2020, 35, 82–89. [Google Scholar] [CrossRef] [PubMed]
| Total | Non-Intervention | Intervention | p-Value | |
|---|---|---|---|---|
| Age (median (IQR)) | 70 (56–77) | 68 (51–76) | 73 (61–81) | 0.027 |
| Women, n (%) | 48 (44.9) | 32 (44.4) | 16 (45.7) | 0.901 |
| Coronary heart disease | 13 (12.1) | 10 (13.9) | 3 (8.6) | 0.43 |
| Congestive heart failure | 15 (14.0) | 8 (11.1) | 7 (20.0) | 0.214 |
| Cerebrovascular disease | 18 (16.8) | 9 (12.5) | 9 (25.7) | 0.086 |
| Peripheral vascular disease | 19 (17.7) | 11 (15.3) | 8 (22.9) | 0.336 |
| Chronic pulmonary disease | 12 (11.2) | 11 (15.3) | 1 (2.9) | 0.056 |
| Peptic ulcer disease | 27 (25.2) | 20 (27.8) | 7 (20.0) | 0.385 |
| Diabetes without end-organ damage | 23 (21.5) | 13 (12.1) | 10 (9.3) | 0.214 |
| Diabetes with end-organ damage | 6 (5.6) | 4 (5.6) | 2 (5.7) | 0.973 |
| Moderate/severe renal disease | 25 (23.4) | 20 (27.8) | 5 (14.3) | 0.122 |
| Non-metastatic tumor | 14 (13.1) | 8 (11.1) | 6 (17.1) | 0.385 |
| Moderate/severe liver disease | 20 (18.7) | 15 (20.8) | 5 (14.3) | 0.415 |
| Metastatic solid tumor | 13 (12.1) | 5 (6.9) | 8 (22.9) | 0.018 |
| CCI median, (IQR) | 6 (4–8) | 6 (3–8) | 7 (4–8) | 0.09 |
| Antithrombotic drug, n(%) | 34 (32.1) | 27 (37.5) | 7 (20.6) | 0.082 |
| Anticoagulants, n (%) | 26 (24.8) | 14 (19.7) | 12 (35.3) | 0.084 |
| Signs of bleeding, n (%) | ||||
| Hematemesis | 39 (36.4) | 24 (33.3) | 15 (42.9) | 0.922 |
| Melaena | 71 (66.4) | 48 (66.7) | 23 (65.7) | 0.922 |
| Hematochezia | 13 (12.1) | 9 (12.5) | 4 (11.4) | 0.874 |
| Syncope | 12 (11.2) | 9 (12.5) | 3 (8.6) | 0.546 |
| Pulse rate, median (IQR), beats per minute | 83 (75–102) | 82 (76–102) | 86 (71–102) | 0.718 |
| Tachycardia | 30 (28.0) | 20 (27.8) | 10 (28.6) | 0.932 |
| Systolic blood pressure, median (IQR), mmHg | 120 (95–138) | 125 (96–140) | 117 (93–130) | 0.16 |
| Signs of shock | 46 (43.0) | 30 (41.7) | 16 (45.7) | 0.692 |
| Bleeding etiologies, n (%) | ||||
| Peptic ulcers | 40 (38.1) | 21 (29.2) | 19 (54.2) | 0.012 |
| Neoplasms | 12 (11.4) | 4 (5.6) | 8 (22.9) | 0.008 |
| Others | 41 (39.1) | 33 (45.8) | 8 (22.9) | 0.022 |
| Laboratory parameters, median (IQR) | ||||
| Urea (mg/dL) | 79 (47–120) | 76 (41–108) | 88 (61–185) | 0.023 |
| Hemoglobin (g/dL) | 8.4 (6.7–9.9) | 8.6 (6.7–10.1) | 7.9 (6.1–8.8) | 0.057 |
| Initial Lactate (mmol/L) | 2.7 (1.6–5.4) | 2.7 (1.6–5.0) | 3.1 (1.7–6.0) | 0.195 |
| Subsequent Lactate (mmol/L) | 1.8 (1.2–3.9) | 2.0 (1.1–3.5) | 1.6 (1.4–4.0) | 0.87 |
| Hours between lactate measurement, | 2.9 (1.7–4.5) | 2.9 (1.6–4.4) | 3.2 (1.8–4.9) | 0.450 |
| Lactate clearance (%) | 18.7 (2.7–48.2) | 16.8 (−0.6–41.2) | 28.9 (8.7–51) | 0.376 |
| Initial lactate elevated (%) | 64 (59.8) | 42 (58.3) | 22 (62.9) | 0.654 |
| Risk scores median, (IQR) | ||||
| GBS | 12 (9–14) | 11 (8–14) | 13 (11–15) | 0.004 |
| p-RS | 4 (3–5) | 4 (3–5) | 4 (3–5) | 0.123 |
| f-RS | 6 (4–7) | 5 (4–6) | 7 (6–9) | <0.001 |
| Outcome | Number of Patients (%) |
|---|---|
| Active Bleeding at Endoscopy | 27 (25.2) |
| Endoscopic intervention | 30 (29.1) |
| Radiological intervention | 6 (5.6) |
| Surgical intervention | 2 (1.9) |
| Any interventions | 35 (32.7) |
| Patients received transfusions | 63 (60) |
| Number of packed red-blood-cells transfused (median (range)) | 2 (0–4) |
| 30-day mortality | 12 (11.2) |
| 30-day rebleeding rate | 16 (15.0) |
| Cutoff Value | Identified Patients | Need for Intervention | Sensitivity % | Specificity % | PPV % | NPV % | |
|---|---|---|---|---|---|---|---|
| Initial lactate | ≤3.8 mmol/L | 68 (64.5%) | 18 (26.1%) | 48.6 | 70.8 | 44.7 | 73.9 |
| Lactate clearance | ≤23.8% | 60 (56.1%) | 15 (25.0%) | 57.1 | 63.9 | 42.6 | 75.0 |
| GBS | ≤10 | 42 (39.3%) | 8 (19%) | 22.9 | 52.8 | 41.5 | 81.0 |
| pRS | ≤4 | 71 (66.4%) | 20 (28.2%) | 42.9 | 70.8 | 41.7 | 71.8 |
| Odds Ratio | Confidence Interval | p-Value | |
|---|---|---|---|
| Age | 1.031 | 0.993–1.071 | |
| Cerebrovascular disease | 1.763 | 0.468–6.646 | 0.402 |
| Chronic pulmonary disease | 0.184 | 0.018–1.89 | 0.154 |
| Metastatic solid tumor | 4.007 | 1.018–15.775 | 0.047 |
| Antithrombotic drugs | 0.361 | 0.115–1.138 | 0.082 |
| Anticoagulants | 0.855 | 0.267–2.735 | 0.792 |
| Urea (mg/dL) | 1.006 | 1.000–1.013 | 0.047 |
| Hemoglobin (g/dL) | 0.831 | 0.66–1.046 | 0.114 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allo, G.; Gillessen, J.; Gülcicegi, D.; Kasper, P.; Chon, S.-H.; Goeser, T.; Bürger, M. Comparison of Lactate Clearance with Established Risk Assessment Tools in Predicting Outcomes in Acute Upper Gastrointestinal Bleeding. J. Clin. Med. 2023, 12, 2716. https://doi.org/10.3390/jcm12072716
Allo G, Gillessen J, Gülcicegi D, Kasper P, Chon S-H, Goeser T, Bürger M. Comparison of Lactate Clearance with Established Risk Assessment Tools in Predicting Outcomes in Acute Upper Gastrointestinal Bleeding. Journal of Clinical Medicine. 2023; 12(7):2716. https://doi.org/10.3390/jcm12072716
Chicago/Turabian StyleAllo, Gabriel, Johannes Gillessen, Dilan Gülcicegi, Philipp Kasper, Seung-Hun Chon, Tobias Goeser, and Martin Bürger. 2023. "Comparison of Lactate Clearance with Established Risk Assessment Tools in Predicting Outcomes in Acute Upper Gastrointestinal Bleeding" Journal of Clinical Medicine 12, no. 7: 2716. https://doi.org/10.3390/jcm12072716
APA StyleAllo, G., Gillessen, J., Gülcicegi, D., Kasper, P., Chon, S.-H., Goeser, T., & Bürger, M. (2023). Comparison of Lactate Clearance with Established Risk Assessment Tools in Predicting Outcomes in Acute Upper Gastrointestinal Bleeding. Journal of Clinical Medicine, 12(7), 2716. https://doi.org/10.3390/jcm12072716






