1. Introduction
Massive, irreparable rotator cuff tears are difficult injuries to treat. They are characterized by the retraction of the torn supraspinatus tendon to an extent where it can no longer reach its native footprint on the greater tuberosity of the humerus. There are a number of approaches to the operative management of such tears, including arthroscopic debridement, interposition with synthetic [
1,
2,
3,
4,
5] or biological [
6,
7,
8] grafts, tendon transfers [
9,
10,
11], and reverse total shoulder arthroplasty [
12,
13,
14].
Whilst the aforementioned strategies have their merits, Mihata et al.’s SCR is a relatively novel joint-preserving treatment that does not rely on the torn tendon as interposition grafts do, and may be particularly beneficial for younger patients who are too young for arthroplasty [
15,
16]. Fascia lata was the original graft material used. However, biomechanical studies have found human dermal allograft and synthetic polytetrafluoroethylene (PTFE) provide comparable structural properties [
17,
18,
19]. Furthermore, patch grafts circumvent the need to harvest autografts and the associated donor site morbidity [
17,
20,
21].
The size of the patch is important for the success of this procedure. Mihata’s protocol described as optimal anteroposterior length, exactly the length of the defect, whereas optimal mediolateral length was 15 mm longer than the distance from the superior glenoid to the supraspinatus insertion point. This excess accommodated for the creation of a 15 mm patch footprint on the superior glenoid [
22,
23,
24].
We hypothesized that our preoperative protocol for the measurement of the mediolateral length using plain film radiography in a standardized position could provide valuable information to guide the surgeon intraoperatively. A further development of this concept was the creation of a patient database to propose ordinal patch sizes that would be appropriate for patients within a range.
To our knowledge, there has been no study to provide a standardized preoperative protocol using plain film radiography to measure the distance between the superior glenoid and the supraspinatus insertion point for superior capsular reconstruction. The aims of the present study were therefore (1) to evaluate inter-rater and intra-rater reliability in measuring the distance between the superior glenoid and the supraspinatus insertion point, and (2) to apply this a preoperative protocol to the creation of a database for determining the appropriate mediolateral dimension of synthetic patch grafts for SCR.
2. Materials and Methods
Ten subjects with normal shoulders were recruited for this study. An inter- and intra-rater reliability trial was conducted using plain film radiography to assess the distance between the superior glenoid and the supraspinatus insertion point on the greater tuberosity of the humerus. Thirty subjects were recruited for the creation of a database to propose three standardized patch sizes for future operations.
This research was approved by the IRB of the authors’ affiliated institutions. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the South Eastern Sydney Local Health District (LNR/13/POWH/186 on 1 May 2022). Informed consent for enrolment into the study and for the publication of these findings was obtained from each participant.
The inclusion criterion for the inter- and intra-rater reliability trial and the database component of the study was subjects with shoulders capable of a minimum of 30° passive abduction and a minimum of 45° passive external rotation. The exclusion criteria for both the inter-and intra-rater reliability trial and the database component of the study were: (1) <18 years of age, (2) glenohumeral arthritis, (3) superior migration of the humeral head, (4) previous rotator cuff repair, and (5) previous shoulder arthroplasty.
2.1. Equipment
A Carestream ODYSSEY HF SeriesTM (Quantum Medical Imaging, North Ronkonkoma, NY, USA) X-ray machine was used for all examinations.
2.2. Raters
Three raters participated in this study: Rater A, a musculoskeletal radiographer with over 20 years of experience, Rater B a medical student with no experience in plain film radiography, and Rater C, a medical practitioner with limited experience in plain film radiography.
All raters were briefed on the study protocol. A training session was held to ensure positioning, imaging technique, application of the Carestream system, and landmarks for the placement of the calibration and ruler markers were standardized for accurate measurement.
2.3. Positioning Protocol
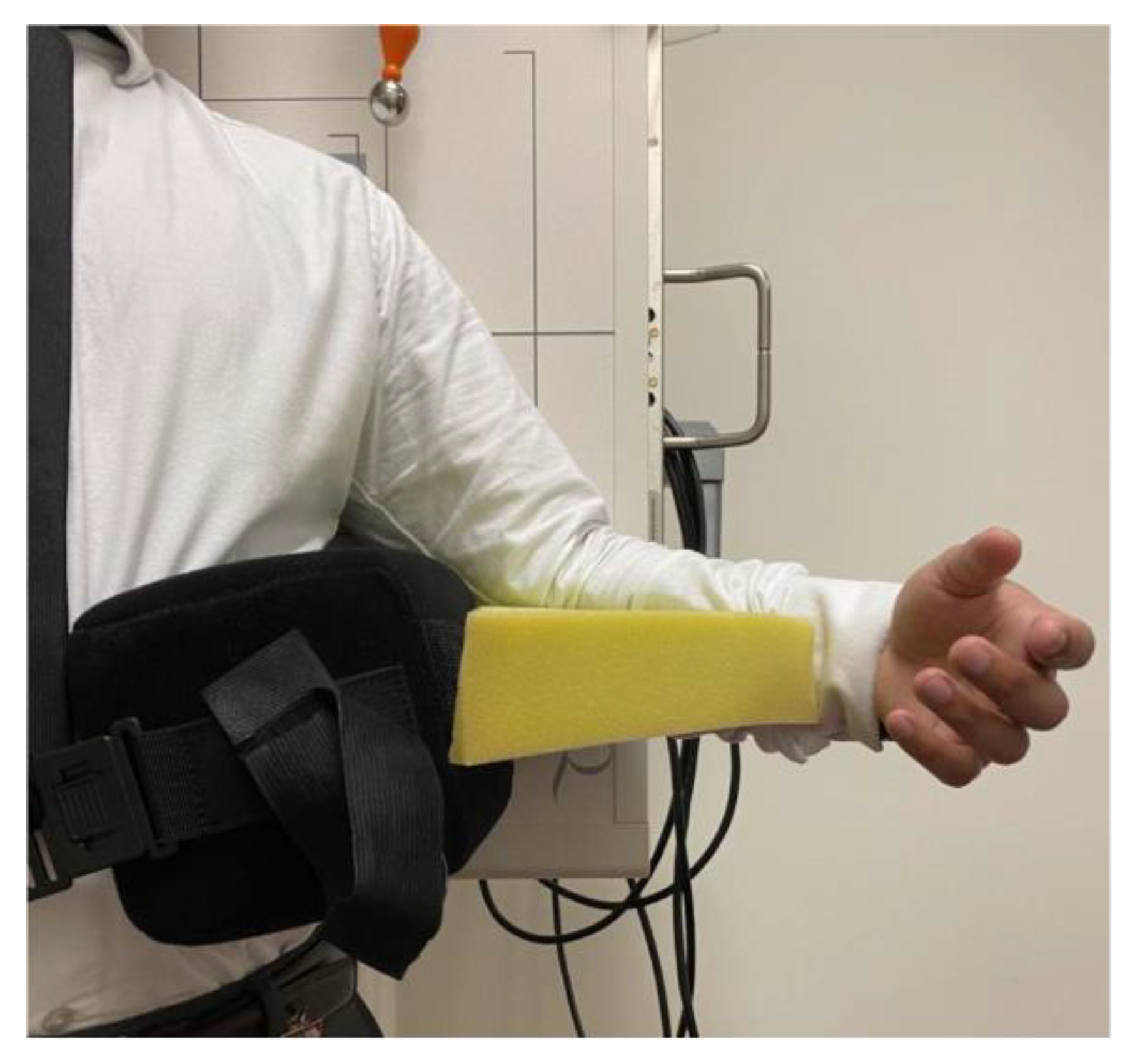
All subjects were examined standing upright, with the shoulder of interest placed at 30° of abduction and 45° of external rotation. To create 30° of abduction, an abduction pillow was placed above their ipsilateral iliac crest and secured with a waist strap. To create 45° of external rotation, a foam pad was placed between the abduction pillow and the subject’s forearm, whilst keeping the subject’s elbow flush against the abduction pillow.
A true anterior-posterior view of the glenohumeral joint was used for the evaluation. Thus, the subject’s scapula on the imaged side was laid flush against the image detector. As a result, the subject’s thorax was rotated toward the affected shoulder at 30–45°. (
Figure 1).
2.4. Scanning Protocol
To ensure standardization, the X-ray tube was positioned at 20° caudal angulation centered at the glenohumeral joint. The superior glenoid and greater tuberosity were used as reference landmarks for measurement and quality of the image. A radiographic reference ball was placed at the level of the coracoid process, in contact with the subject’s skin.
After capturing the plain film radiograph, the raters were instructed to calibrate the system using the radiographic reference ball. Using the calibration measurement tool, a straight line was drawn through the diameter of the ball, and a real length value of 25 mm was entered manually. Upon calibration, the ruler device was used to place a marker at the superior aspect of the glenoid where the medial anchors would be placed and another at the greater tuberosity where the lateral anchors would be placed. The distance would then be generated. (
Figure 2).
2.5. Inter-Rater Trial
For the evaluation of inter-rater reliability, the ten subjects were examined by the three raters. Each rater positioned each subject and captured three different radiographs of the same subject with a 5 min interval between capturing each radiograph. A total of 90 assessments were performed for the inter-rater trial. The subject was repositioned at the beginning of each inter-rater trial.
2.6. Intra-Rater Trial
For the evaluation of intra-rater reliability, Rater A examined six subjects, obtaining three radiographs per examination. Therefore, each subject was evaluated three times, with a one-hour interval between each assessment. A total of 18 assessments were performed for the intra-rater trial. The subject was repositioned at the beginning of each assessment in accordance with the aforementioned protocol. Rater A positioned, captured, and assessed the radiographs independently of external inputs from other raters.
2.7. SCR Database
A cohort of 30 subjects who presented to the clinic were recruited. A database for recording the distance between the superior glenoid and the supraspinatus insertion point on the greater tuberosity of the humerus using the aforementioned protocol was generated. The results were measured and grouped using a histogram to propose patch sizes for SCR.
2.8. Statistical Analysis
The reliability of plain film radiography in calculating the distance between the superior glenoid and the greater tuberosity was assessed with a two-way random-effects model to generate interclass correlation coefficients (ICC) with 95% confidence intervals, using SPSS version 24. ICCs were interpreted with the guidelines formulated by Cicchetti and Sparrow: 0.00 to 0.39, poor; 0.40 to 0.59, fair; 0.60 to 0.74, good; 0.75 to 1.00, excellent [
25].
3. Results
The 10 subjects recruited for the inter-rater trial comprised 4 females and 6 males. The 30 subjects recruited for the database comprised 16 males and 14 females.
3.1. Inter-Rater Testing
The reliability of the measurement between the superior glenoid and the point of insertion of the supraspinatus in the inter-rater trial was excellent. The ICC value was 0.94 (95% CI), with a lower bound value of 0.84 and an upper bound value of 0.98. The average measurement of the space was 26.5 mm, with a standard deviation of 0.7 mm between the raters.
3.2. Intra-Rater Testing
The reliability of the measurement between the superior glenoid and the point of insertion of the supraspinatus in the intra-rater trial was excellent. The ICC value was 0.76 (95% CI), with a lower bound value of 0.34 and an upper bound value of 0.96. The average measurement of the space was 25.9 mm, with a standard deviation of 0.7 mm between each session.
3.3. Database Result
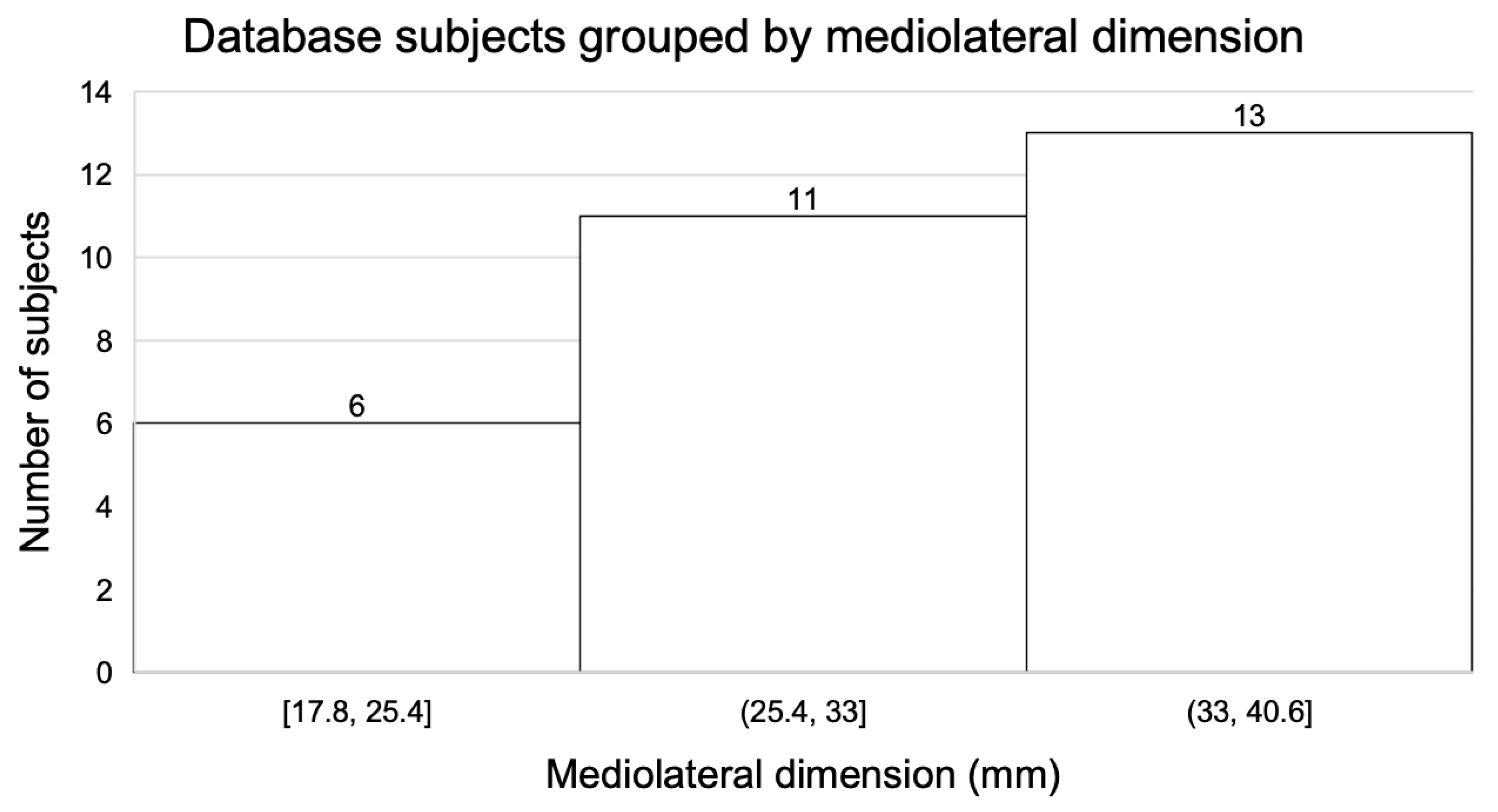
A database of 30 recorded measurements between the superior glenoid and the point of insertion of the supraspinatus using our X-ray protocol was established (
Figure 3). The subjects were then allocated to one of three groups (
Figure 4) based on the mediolateral dimensions generated by the protocol. The dimensions of the six subjects in the first group ranged from 17.8 mm to 25.4 mm, with a mean of 23 mm. The dimensions of the eleven subjects in the second group ranged from 25.4 mm to 33 mm, with a mean of 28 mm. The dimensions of the thirteen subjects in the third group ranged from 33 to 40.6 mm, with a mean of 37 mm. The mean distance of the database group overall was 30.8 mm and ranged from 17 mm to 40.6 mm, with a standard deviation of 6.2 mm.
To accommodate for the surgical landing sites and areas for suturing both medially and laterally, 10 mm was added to the mean of each of the three groups. Thus, the proposed patch sizes, from small to large, were 33 mm, 38 mm, and 47 mm.
4. Discussion
This study investigated the reliability of using plain film radiographs in measuring the distance between the superior glenoid and the point of insertion of the supraspinatus on the greater tuberosity. Statistical analyses demonstrated excellent reliability of this protocol, regardless of the rater experience. A database was generated using the protocol, and three standardized patch sizes were subsequently proposed for use in future superior capsular reconstructions.
Whilst massive, irreparable rotator cuff tears are best visualized using soft tissue imaging modalities such as MRI, the sequelae of cuff tear arthropathy that ends in glenohumeral acetabulization and osteoarthritis mean that plain film radiographs are also often required to assess the extent of bony damage [
16,
26]. In contrast to MRI, plain film radiography is readily accessible, inexpensive, and timely, both in the conduction of the study and in the development of the images. Whilst ultrasound is also an inexpensive soft-tissue imaging modality, it is user-dependent and dynamic, which in the context of preoperative templating makes it less suitable than a plain film radiograph [
27]. Nonetheless, 2D radiographic investigations such as plain film radiographs are subject to variability, with factors including positioning and appropriate choice of landmarks, which are just two of the multiple factors that can influence a result. Thus, a reliability assessment was required to test the robustness of our novel protocol.
To our knowledge, there have been no studies to design a standardized preoperative imaging protocol to template graft sizes in superior capsular reconstruction. Previous technical notes described the use of a measuring probe intraoperatively to determine the dimensions of the graft [
22,
23,
24,
28,
29]. However, arthroscopy is a highly technical procedure, and as expected, proficiency is gained through experience. Accordingly, intraoperative arthroscopic measurement speed and accuracy is lower for less experienced surgeons [
30,
31]. Furthermore, given the relatively recent debut of Mihata’s SCR in 2012, a reliable preoperative radiographic protocol would aid in minimizing intraoperative measurement errors. In addition, preoperative planning may help to facilitate the procedure, as increased operative time has been shown to be an independent predictor of surgical site infection and hospital length of stay [
32].
There are many graft options available on the market, each varying in area, thickness, and material. These factors invariably influence the cost of the procedure. A greater graft thickness has shown to be an important factor in maintaining the acromiohumeral distance, with superior biomechanical properties compared to those of thinner grafts [
20,
33]. SCR grafts are commonly folded upon themselves to increase their thickness. Therefore, a preoperative reference on the required area of the graft to bridge the gap between the superior glenoid and the greater tuberosity allows the surgeon to account for the excess required to create the ideal thickness of 6–8 mm [
34].
The strength of this study is the ease and reliability with which this protocol can be implemented, independent of the rater experience. One limitation for both components of this study was the cohort size. A limitation of the database component is that our subjects may not be representative of other age or ethnic groups.
5. Conclusions
Our preoperative X-ray protocol demonstrated excellent reliability in measuring the distance between the superior glenoid and the insertion of the supraspinatus tendon, independent of the rater experience. The utilization of this easily replicable protocol and its database will provide valuable information for surgeons performing superior capsular reconstruction.
Author Contributions
Conceptualization, R.S.T., R.R., T.K.L., P.H.L. and G.A.C.M.; methodology, R.S.T., R.R., T.K.L., L.H. and G.A.C.M.; software, P.H.L.; validation, R.S.T., P.H.L., H.S.A.A.-H. and G.A.C.M.; formal analysis, R.S.T., R.R., P.H.L. and G.A.C.M.; investigation, R.S.T., T.K.L., L.H. and H.S.A.A.-H.; resources, G.A.C.M.; data curation, R.S.T., R.R., T.K.L. and P.H.L.; writing—original draft preparation, R.S.T., R.R. and P.H.L.; writing—review and editing, R.S.T., R.R., P.H.L., H.S.A.A.-H. and G.A.C.M.; visualization, R.S.T. and G.A.C.M.; supervision, G.A.C.M.; project administration, R.S.T., R.R. and G.A.C.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the South Eastern Sydney Local Health District (12/310 (LNR/13/POWH/186) on 1 May 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Available upon request.
Acknowledgments
The authors sincerely thank Linda Dodd and Marina Zimmermann for the support and administrative assistance that they dedicated toward this project.
Conflicts of Interest
G.A.C.M. is a paid consultant and has research funding from Smith and Nephew and is also on the Editorial Board of the following publications: Journal of Shoulder and Elbow Surgery; Shoulder and Elbow. The other authors, R.S.T., R.R., T.K.L., L.H., H.S.A.A.-H. and P.H.L., their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- Ozaki, J.; Fujimoto, S.; Masuhara, K.; Tamai, S.; Yoshimoto, S. Reconstruction of chronic massive rotator cuff tears with synthetic materials. Clin. Orthop. Relat. Res. 1986, 202, 173–183. [Google Scholar] [CrossRef]
- Shepherd, H.M.; Lam, P.H.; Murrell, G.A.C. Synthetic Patch Rotator Cuff Repair: A 10-year Follow-Up. Shoulder Elb. 2014, 6, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Seker, V.; Hackett, L.; Lam, P.H.; Murrell, G.A.C. Evaluating the Outcomes of Rotator Cuff Repairs with Polytetrafluoroethylene Patches for Massive and Irreparable Rotator Cuff Tears with a Minimum 2-Year Follow-up. Am. J. Sports Med. 2018, 46, 3155–3164. [Google Scholar] [CrossRef]
- Sunwoo, J.Y.; Lam, P.H.; Murrell, G.A.C. A Comparison of Two Arthroscopic Techniques for Interpositional Polytetrafluoroethylene Patch Repair for Massive Irreparable Rotator Cuff Tears: Speed and Biomechanics. HSS J. 2018, 14, 186–191. [Google Scholar] [CrossRef]
- Ting, R.S.; Deng, A.; Rosenthal, R.; Al-Housni, H.S.A.; Zhong, K.; Lam, P.H.; Murrell, G.A.C. Biomechanical and morphological comparison of two interposition graft rotator cuff repair techniques. ANZ J. Surg. 2023, 93, 649–655. [Google Scholar] [CrossRef]
- Hirooka, A.; Yoneda, M.; Wakaitani, S.; Isaka, Y.; Hayashida, K.; Fukushima, S.; Okamura, K. Augmentation with a Gore-Tex patch for repair of large rotator cuff tears that cannot be sutured. J. Orthop. Sci. 2002, 7, 451–456. [Google Scholar] [CrossRef]
- Neumann, J.A.; Zgonis, M.H.; Rickert, K.D.; Bradley, K.E.; Kremen, T.J.; Boggess, B.R.; Toth, A.P. Interposition Dermal Matrix Xenografts: A Successful Alternative to Traditional Treatment of Massive Rotator Cuff Tears. Am. J. Sports Med. 2017, 45, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Sano, H.; Mineta, M.; Kita, A.; Itoi, E. Tendon patch grafting using the long head of the biceps for irreparable massive rotator cuff tears. J. Orthop. Sci. 2010, 15, 310–316. [Google Scholar] [CrossRef]
- Camp, C.L.; Elhassan, B.; Dines, J.S. Clinical Faceoff: Irreparable Rotator Cuff Tears in Young, Active Patients: Tendon Transfer versus Superior Capsular Reconstruction? Clin. Orthop. Relat. Res. 2018, 476, 2313–2317. [Google Scholar] [CrossRef] [PubMed]
- Delaney, R.A.; Kadow, T.R.; Garcia, D.; Minorini, R.; Baratz, M.E.; Lin, A. Latissimus Dorsi Tendon Transfer vs. Superior Capsular Reconstruction for Treatment of Irreparable Rotator Cuff Tears: A Retrospective Comparison Study with Short-term Clinical Results. JSES Open Access 2019, 3, 249. [Google Scholar] [CrossRef]
- Milano, G.; Saccomanno, M.F.; Colosio, A.; Adriani, M.; Galli, S.; Scaini, A.; Marchi, G. Arthroscopic Superior Capsule Reconstruction with Doubled Autologous Semitendinosus Tendon Graft. Arthrosc. Tech. 2020, 9, e1665–e1672. [Google Scholar] [CrossRef] [PubMed]
- Walton, J.R.; Bowman, N.K.; Khatib, Y.; Linklater, J.; Murrell, G.A. Restore Orthobiologic Implant. J. Bone Jt. Surg. 2007, 89, 786–791. [Google Scholar] [CrossRef]
- Rockwood, C.A., Jr.; Williams, G.R., Jr.; Burkhead, W.Z., Jr. Débridement of degenerative, irreparable lesions of the rotator cuff. J. Bone Jt. Surg. 1995, 77, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Pandey, V.; Willems, W.J. Rotator cuff tear: A detailed update. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2015, 2, 1–14. [Google Scholar] [CrossRef]
- Mihata, T.; Lee, T.Q.; Watanabe, C.; Fukunishi, K.; Ohue, M.; Tsujimura, T.; Kinoshita, M. Clinical Results of Arthroscopic Superior Capsule Reconstruction for Irreparable Rotator Cuff Tears. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 459–470. [Google Scholar] [CrossRef]
- Ting, R.S.; Rosenthal, R.; Al-Housni, H.S.; Lam, P.H.; Murrell, G.A.C. Factors influencing clinical outcomes in superior capsular reconstruction: A scoping review. J. Clin. Orthop. Trauma 2023, 36, 102081. [Google Scholar] [CrossRef]
- Shah, S.S.; Kontaxis, A.; Jahandar, A.; Bachner, E.; Gulotta, L.V.; Dines, D.M.; Warren, R.F.; Dines, J.S.; Taylor, S.A. Superior capsule reconstruction using a single 6-mm-thick acellular dermal allograft for massive rotator cuff tears: A biomechanical cadaveric comparison to fascia lata allograft. J. Shoulder Elb. Surg. 2021, 30, 2166–2176. [Google Scholar] [CrossRef]
- Cline, K.E.; Tibone, J.E.; Ihn, H.; Akeda, M.; Kim, B.-S.; McGarry, M.H.; Mihata, T.; Lee, T.Q. Superior Capsule Reconstruction Using Fascia Lata Allograft Compared with Double- and Single-Layer Dermal Allograft: A Biomechanical Study. Arthrosc. J. Arthrosc. Relat. Surg. 2021, 37, 1117–1125. [Google Scholar] [CrossRef]
- Ting, R.S.; Guo, A.A.; Rosenthal, R.; Al-Housni, H.S.A.; Lam, P.H.; Murrell, G.A.C. Biomechanical Comparison of Synthetic Polytetrafluoroethylene (PTFE) vs. Human Dermal Allograft (HDA), 2 vs. 3 Glenoid Anchors, and Suture vs. Minitape in Superior Capsule Reconstruction. HSS J. 2022, 19, 44–52. [Google Scholar] [CrossRef]
- Okamura, K.; Abe, M.; Yamada, Y.; Makihara, T.; Yoshimizu, T.; Sakaki, Y.; Suzumori, Y.; Mihata, T. Arthroscopic superior capsule reconstruction with Teflon felt synthetic graft for irreparable massive rotator cuff tears: Clinical and radiographic results at minimum 2-year follow-up. J. Shoulder Elb. Surg. 2021, 30, 625–634. [Google Scholar] [CrossRef]
- Okamura, K.; Makihara, T. Cable Graft: Simple Superior Capsule Reconstruction Technique for Irreparable Rotator Cuff Tear Using a Teflon Patch. Arthrosc. Tech. 2020, 9, e575–e580. [Google Scholar] [CrossRef] [PubMed]
- Mihata, T.; Lee, T.Q.; Hasegawa, A.; Kawakami, T.; Fukunishi, K.; Fujisawa, Y.; Itami, Y.; Ohue, M.; Neo, M. Arthroscopic Superior Capsule Reconstruction Can Eliminate Pseudoparalysis in Patients with Irreparable Rotator Cuff Tears. Am. J. Sports Med. 2018, 46, 2707–2716. [Google Scholar] [CrossRef]
- Mihata, T.; Lee, T.Q.; Fukunishi, K.; Itami, Y.; Fujisawa, Y.; Kawakami, T.; Ohue, M.; Neo, M. Return to Sports and Physical Work After Arthroscopic Superior Capsule Reconstruction Among Patients with Irreparable Rotator Cuff Tears. Am. J. Sports Med. 2018, 46, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Mihata, T.; Lee, T.Q.; Hasegawa, A.; Fukunishi, K.; Kawakami, T.; Fujisawa, Y.; Ohue, M.; Neo, M. Five-Year Follow-up of Arthroscopic Superior Capsule Reconstruction for Irreparable Rotator Cuff Tears. J. Bone Jt. Surg. 2019, 101, 1921–1930. [Google Scholar] [CrossRef]
- Cicchetti, D.V.; Sparrow, S.A. Developing criteria for establishing interrater reliability of specific items: Applications to assessment of adaptive behavior. Am. J. Ment. Defic. 1981, 86, 127–137. [Google Scholar] [PubMed]
- Kuzel, B.R.; Grindel, S.; Papandrea, R.; Ziegler, D. Fatty Infiltration and Rotator Cuff Atrophy. J. Am. Acad. Orthop. Surg. 2013, 21, 613–623. [Google Scholar] [CrossRef]
- Lenza, M.; Buchbinder, R.; Takwoingi, Y.; Johnston, R.V.; Hanchard, N.C.; Faloppa, F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst. Rev. 2013, 2013, CD009020. [Google Scholar] [CrossRef]
- Dimock, R.A.C.; Malik, S.; Consigliere, P.; Imam, M.A.; Narvani, A.A. Superior Capsule Reconstruction: What Do We Know? Arch. Bone Jt. Surg. 2019, 7, 3–11. [Google Scholar]
- Sanchez, G.; Rossy, W.H.; Lavery, K.P.; McHale, K.J.; Ferrari, M.B.; Sanchez, A.; Provencher, M.T. Arthroscopic Superior Capsule Reconstruction Technique in the Setting of a Massive, Irreparable Rotator Cuff Tear. Arthrosc. Tech. 2017, 6, e1399–e1404. [Google Scholar] [CrossRef]
- Tashiro, Y.; Miura, H.; Nakanishi, Y.; Okazaki, K.; Iwamoto, Y. Evaluation of Skills in Arthroscopic Training Based on Trajectory and Force Data. Clin. Orthop. Relat. Res. 2009, 467, 546–552. [Google Scholar] [CrossRef]
- Oakley, S.P.; Portek, I.; Szomor, Z.; Turnbull, A.; Murrell, G.A.C.; Kirkham, B.W.; Lassere, M.N. Poor accuracy and interobserver reliability of knee arthroscopy measurements are improved by the use of variable angle elongated probes. Ann. Rheum. Dis. 2002, 61, 540–543. [Google Scholar] [CrossRef] [PubMed]
- Boddapati, V.; Fu, M.C.; Schairer, W.W.; Ranawat, A.S.; Dines, D.M.; Taylor, S.A.; Dines, J.S. Increased Shoulder Arthroscopy Time Is Associated with Overnight Hospital Stay and Surgical Site Infection. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.C.; Im, H.Y.; Lam, P.H. Effect of human dermal allograft thickness on glenohumeral stability for superior capsular reconstruction in irreparable supraspinatus tears: A biomechanical analysis of the superior capsular reconstruction—A cadaveric study. Shoulder Elb. 2020, 14, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Mihata, T.; McGarry, M.H.; Kahn, T.; Goldberg, I.; Neo, M.; Lee, T.Q. Biomechanical Effect of Thickness and Tension of Fascia Lata Graft on Glenohumeral Stability for Superior Capsule Reconstruction in Irreparable Supraspinatus Tears. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 418–426. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).