Access to High-Cost Biological Agents: Perceptions of Brazilian Patients with Inflammatory Bowel Diseases
Abstract
1. Introduction
2. Materials and Methods
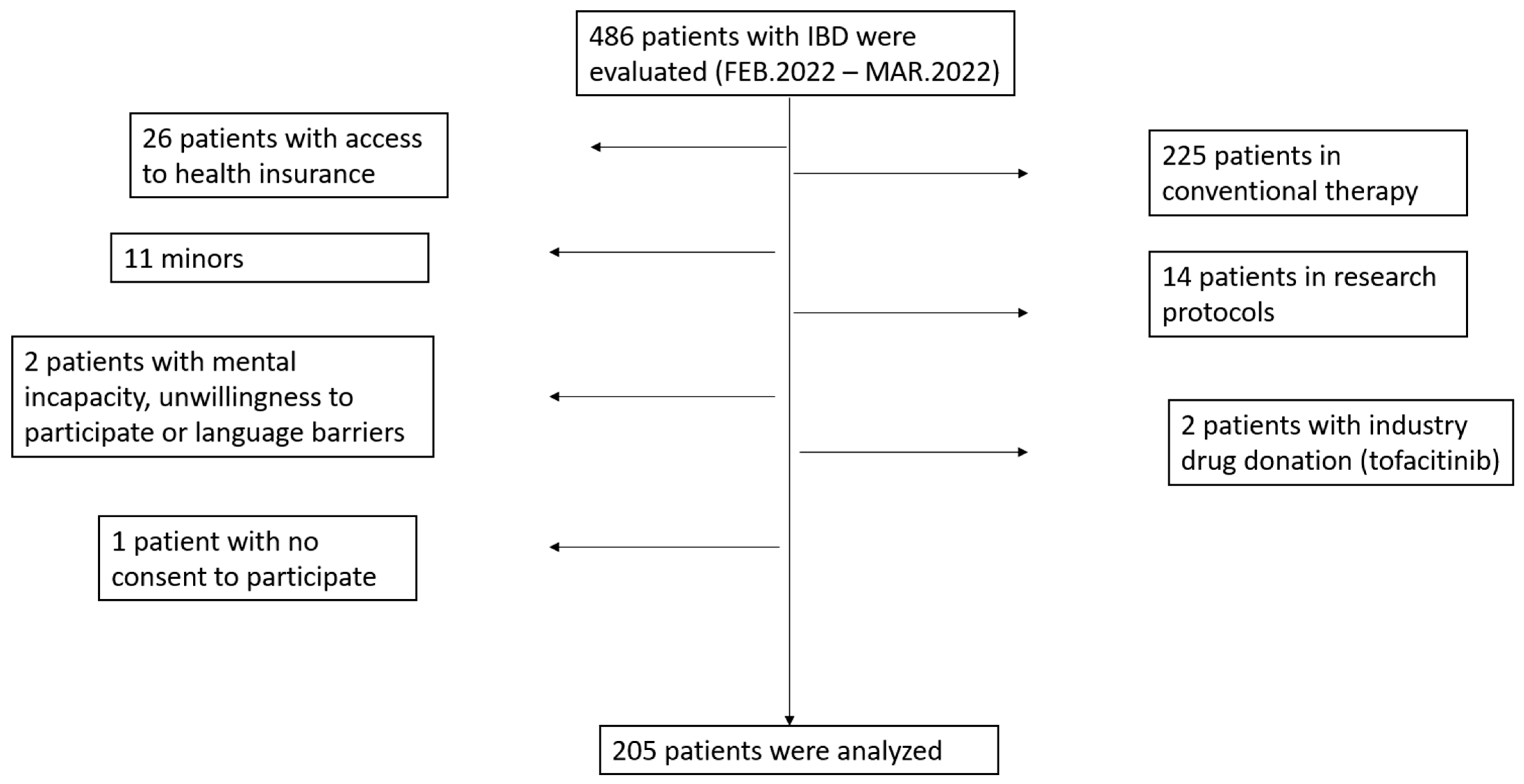
2.1. Study Design and Population
Data Variables Obtained from the Questionnaire-Based Survey
- What was the biologic prescribed?
- Is there a lack or delay in the initiation of continuing biologics?
- If yes, what is the number of absences in delivering the biologics?
- What is the average time to regularize the distribution of the biologics?
- Do you fear that missing the biological infusion can cause impairment in your treatment or lead to complications?
- Did the patient think that obtaining the biologics is a bureaucratic process?
- Did the attendant or the pharmacist of the high-cost pharmacy solve doubts about the storage of the biologics and the next steps after obtaining the drug?
- In the case of lack or delay in the distribution of the biologics, was there an explanation of the reason for the lack of the drug?
- Was there an attempt to contact the high-cost pharmacy (by phone, message, or e-mail)?
- If yes, was this contact not possible, or was it possible and easy, or possible and difficult?
- Would it be easier to obtain biologics at the tertiary hospital after your medical appointment or at the infusion clinic immediately before the infusion?
- Would it be easier to get the drug at the high-cost pharmacy and leave it for infusion at the tertiary hospital or the outside infusion clinic?
- Do you know about the sponsored assistance program by the distributing pharmaceutical company of the medicine drug?
- Do you believe that it is important to have the treatment initiation program by the laboratory producing the biologics?
2.2. Ethical Considerations
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Patient Perceptions
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Quaresma, A.B.; Kaplan, G.G.; Kotze, P.G. The globalization of inflammatory bowel disease: The incidence and prevalence of inflammatory bowel disease in Brazil. Curr. Opin. Gastroenterol. 2019, 35, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Gasparini, R.G.; Sassaki, L.Y.; Saad-Hossne, R. Inflammatory bowel disease epidemiology in São Paulo State, Brazil. Clin. Exp. Gastroenterol. 2018, 11, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Parra, R.S.; Chebli, J.M.; Amarante, H.M.; Flores, C.; Parente, J.M.; Ramos, O.; Fernandes, M.; Rocha, J.J.; Feitosa, M.R.; Feres, O.; et al. Quality of life, work productivity impairment and healthcare resources in inflammatory bowel diseases in Brazil. World J. Gastroenterol. 2019, 25, 5862–5882. [Google Scholar] [CrossRef] [PubMed]
- Sassaki, L.Y.; Miszputen, S.J.; Junior, R.L.K.; Catapani, W.R.; Bafutto, M.; Scotton, A.S.; Zaltman, C.; Baima, J.P.; Ramos, H.S.; Faria, M.A.G.; et al. Real-world treatment patterns and disease control over one year in patients with inflammatory bowel disease in Brazil. World J. Gastroenterol. 2021, 27, 3396–3412. [Google Scholar] [CrossRef]
- de Sá Brito Fróes, R.; da Luz Moreira, A.; Carneiro, A.J.V.; Moreira, J.P.L.; Luiz, R.R.; de Barros Moreira, A.M.H.; Moreira, J.P.L.; Luiz, R.R.; de Souza, H.S. Prevalence, Indirect Costs, and Risk Factors for Work Disability in Patients with Crohn’s Disease at a Tertiary Care Center in Rio de Janeiro. Dig. Dis. Sci. 2021, 66, 2925–2934. [Google Scholar] [CrossRef]
- de S. B. Fróes, R.; Carvalho, A.T.P.; de VCarneiro, A.J.; de Barros Moreira, A.M.H.; Moreira, J.P.L.; Luiz, R.R.; de Souza, H.S. The socio-economic impact of work disability due to inflammatory bowel disease in Brazil. Eur. J. Health Econ. 2018, 19, 463–470. [Google Scholar] [CrossRef]
- Tsai, L.; Ma, C.; Dulai, P.S.; Prokop, L.J.; Eisenstein, S.; Ramamoorthy, S.L.; Feagan, B.G.; Jairath, V.; Sandborn, W.J.; Singh, S. Contemporary Risk of Surgery in Patients with Ulcerative Colitis and Crohn’s Disease: A Meta-Analysis of Population-Based Cohorts. Clin. Gastroenterol. Hepatol. 2021, 19, 2031–2045.e11. [Google Scholar] [CrossRef]
- Guedes, A.L.V.; Lorentz, A.L.; Rios, L.F.A.R.; Freitas, B.C.; Dias, A.G.N.; Uhlein, A.L.E.; Neto, F.O.V.; Jesus, J.F.S.; de Sá Novaes Torres, T.; Rocha, R.; et al. Hospitalizations and in-hospital mortality for inflammatory bowel disease in Brazil. World J. Gastrointest. Pharmacol. Ther. 2022, 13, 1–10. [Google Scholar] [CrossRef]
- Palacio, F.G.M.; de Souza, L.M.P.; Moreira, J.P.L.; Luiz, R.R.; de Souza, H.S.P.; Zaltman, C. Hospitalization and surgery rates in patients with inflammatory bowel disease in Brazil: A time-trend analysis. BMC Gastroenterol. 2021, 21, 192. [Google Scholar] [CrossRef]
- Melsheimer, R.; Geldhof, A.; Apaolaza, I.; Schaible, T. Remicade® (infliximab): 20 years of contributions to science and medicine. Biologics 2019, 13, 139–178. [Google Scholar]
- Bonovas, S.; Pansieri, C.; Piovani, D.; Macaluso, F.S.; Orlando, A.; Festa, S.; Papi, C.; Pugliese, D.; Armuzzi, A. Use of biologics and small molecule drugs for the management of moderate to severe ulcerative colitis: IG-IBD technical review based on the GRADE methodology. Dig. Liver Dis. 2022, 54, 428–439. [Google Scholar] [CrossRef]
- Cushing, K.; Higgins, P.D.R. Management of Crohn Disease: A Review. JAMA 2021, 325, 69–80. [Google Scholar] [CrossRef]
- Khoudari, G.; Mansoor, E.; Click, B.; Alkhayyat, M.; Saleh, M.A.; Sinh, P.; Katz, J.; Cooper, G.S.; Regueiro, M. Rates of Intestinal Resection and Colectomy in Inflammatory Bowel Disease Patients After Initiation of Biologics: A Cohort Study. Clin. Gastroenterol. Hepatol. 2020, 20, e974–e983. [Google Scholar] [CrossRef]
- Ben-Horin, S.; Novack, L.; Mao, R.; Guo, J.; Zhao, Y.; Sergienko, R.; Zhang, J.; Kobayashi, T.; Hibi, T.; Chowers, Y.; et al. Efficacy of Biologic Drugs in Short-Duration Versus Long-Duration Inflammatory Bowel Disease: A Systematic Review and an Individual-Patient Data Meta-Analysis of Randomized Controlled Trials. Gastroenterology 2022, 162, 482–494. [Google Scholar] [CrossRef]
- Vilela, E.G.; Rocha, H.C.; Moraes, A.C.; Santana, G.O.; Parente, J.M.; Sassaki, L.Y.; Miszputen, S.J.; Quaresma, A.B.; Clara, A.P.H.S.; De Jesus, A.C.S.; et al. Inflammatory bowel disease care in brazil: How it is performed, obstacles and demands from the physicians’ perspective. Arq. Gastroenterol. 2020, 57, 416–427. [Google Scholar] [CrossRef]
- Hamdeh, S.; Aziz, M.; Altayar, O.; Olyaee, M.; Murad, M.H.; Hanauer, S.B. Early vs. Late Use of Anti-TNFa Therapy in Adult Patients with Crohn Disease: A Systematic Review and Meta-Analysis. Inflamm. Bowel Dis. 2020, 26, 1808–1818. [Google Scholar] [CrossRef]
- Solitano, V.; D’Amico, F.; Zacharopoulou, E.; Peyrin-Biroulet, L.; Danese, S. Early Intervention in Ulcerative Colitis: Ready for Prime Time? J. Clin. Med. 2020, 9, 2646. [Google Scholar] [CrossRef]
- Ungaro, R.C.; Yzet, C.; Bossuyt, P.; Baert, F.J.; Vanasek, T.; D’Haens, G.R.; Joustra, V.W.; Panaccione, R.; Novacek, G.; Reinisch, W.; et al. Deep Remission at 1 Year Prevents Progression of Early Crohn’s Disease. Gastroenterology 2020, 159, 139–147. [Google Scholar] [CrossRef]
- Quaresma, A.B.; Kotze, P.G. Reduction of surgical rates in inflammatory bowel diseases biologic era: Similarities between Spain and Latin America. J. Gastroenterol. Hepatol. 2020, 35, 1453. [Google Scholar] [CrossRef]
- Manceur, A.M.; Ding, Z.; Muser, E.; Obando, C.; Voelker, J.; Pilon, D.; Kinkead, F.; Lafeuille, M.-H.; Lefebvre, P. Burden of Crohn’s disease in the United States: Long-term healthcare and work-loss related costs. J. Med. Econ. 2020, 23, 1092–1101. [Google Scholar] [CrossRef]
- Park, K.T.; Ehrlich, O.G.; Allen, J.I.; Meadows, P.; Szigethy, E.M.; Henrichsen, K.; Kim, S.C.; Lawton, R.C.; Murphy, S.M.; Regueiro, M.; et al. The Cost of Inflammatory Bowel Disease: An Initiative from the Crohn’s & Colitis Foundation. Inflamm. Bowel Dis. 2020, 26, 1–10. [Google Scholar] [PubMed]
- Qiu, Y.; Chen, B.L.; Mao, R.; Zhang, S.H.; He, Y.; Zeng, Z.R.; Ben-Horin, S.; Chen, M.-H. Systematic review with meta-analysis: Loss of response and requirement of anti-TNFα dose intensification in Crohn’s disease. J. Gastroenterol. 2017, 52, 535–554. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Gulati, A.; Alipour, O.; Shao, L. Relapse from deep remission after therapeutic de-escalation in inflammatory bowel disease: A systematic review and meta-analysis. J. Crohns Colitis 2020, 14, 1413–1423. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.W.; Shen, J.; Zheng, Q.; Ran, Z.H. Loss of response to scheduled infliximab therapy for Crohn’s disease in adults: A systematic review and meta-analysis. J. Dig. Dis. 2019, 20, 65–72. [Google Scholar] [CrossRef]
- Torres, J.; Boyapati, R.K.; Kennedy, N.A.; Louis, E.; Colombel, J.F.; Satsangi, J. Systematic Review of Effects of Withdrawal of Immunomodulators or Biologic Agents from Patients With Inflammatory Bowel Disease. Gastroenterology 2015, 149, 1716–1730. [Google Scholar] [CrossRef]
- Louis, E. Tailoring Biologic or Immunomodulator Treatment Withdrawal in Inflammatory Bowel Disease. Front. Med. 2019, 6, 302. [Google Scholar] [CrossRef]
- de Oliveira, R.T.G.; Agostinho, G.L.P.L.; Granja, R.; Oyafuso, L.K.M.; Criado, P.R. Socioeconomic impact of high-cost drugs in Brazilian dermatology. Legal and financial aspects, and impact on clinical practice. An. Bras. Dermatol. 2021, 96, 200–209. [Google Scholar] [CrossRef]
- Parra, R.S.; Chebli, J.M.F.; Queiroz, N.S.F.; Damião, A.O.M.C.; de Azevedo, M.F.C.; Chebli, L.A.; Bertges, E.R.; Alves, A.J.T., Jr.; Ambrogini, O., Jr.; da Silva, B.L.P.S.; et al. Long-term effectiveness and safety of ustekinumab in bio-naïve and bio-experienced anti-tumor necrosis factor patients with Crohn’s disease: A real-world multicenter Brazilian study. BMC Gastroenterol. 2022, 22, 199. [Google Scholar] [CrossRef]
- Danese, S.; Subramaniam, K.; Van Zyl, J.; Adsul, S.; Lindner, D.; Roth, J.; Vermeire, S. Vedolizumab treatment persistence and safety in a 2-year data analysis of an extended access programme. Aliment. Pharmacol. Ther. 2021, 53, 265–272. [Google Scholar] [CrossRef]
- Singh, S.; George, J.; Boland, B.S.; Vande Casteele, N.; Sandborn, W.J. Primary Non-Response to Tumor Necrosis Factor Antagonists is Associated with Inferior Response to Second-line Biologics in Patients with Inflammatory Bowel Diseases: A Systematic Review and Meta-analysis. J. Crohns Colitis 2018, 12, 635–643. [Google Scholar] [CrossRef]
| Characteristics | Results |
|---|---|
| Mean age, years (range) | 40.7 (19–75) |
| Gender, n (%) | |
| Female | 104 (50.7) |
| Male | 101 (49.3) |
| Occupation | |
| Employed | 112 (54.6) |
| Unemployed | 87 (42.4) |
| Government assistance | 40 (19.5) |
| Did not answer | 6 (2.9) |
| Crohn’s disease | 161 (78.5) |
| Montreal Classification, n (%) | |
| Age at diagnosis | |
| A1 (<17 years) | 10 (6.2) |
| A2 (17–40 years) | 101 (62.7) |
| A3 (>40 years) | 50 (31.1) |
| Disease location | |
| L1 (ileal) | 39 (24.2) |
| L2 (colonic) | 35 (21.8) |
| L3 (ileocolonic) | 82 (50.9) |
| L4 (upper gastrointestinal tract) | 5 (3.1) |
| Behavior | |
| B1 (inflammatory) | 53 (32.9) |
| B2/B3 (stenosing/penetrating) | 108 (67.1) |
| Ulcerative colitis | 44 (21.5) |
| Montreal Classification, n (%) | |
| E1 | 6 (13.6) |
| E2 | 12 (27.3) |
| E3 | 26 (59.1) |
| Mean disease duration, years (range) | 11.9 (2–24) |
| CD | 12.5 (2–24) |
| UC | 9.7 (2–20) |
| History of perianal disease * | 76 (47.2) |
| Previous bowel resection in CD | 96 (59.6) |
| Biologics in use, n (%) | |
| Infliximab | 128 (62.5) |
| Adalimumab | 39 (19.0) |
| Certolizumab pegol | 8 (3.9) |
| Golimumab | 1 (0.5) |
| Vedolizumab | 14 (6.8) |
| Ustekinumab | 15 (7.3) |
| Variable in Study | n (%) |
|---|---|
| At least a lack of dispensation of biologics | 172 (83.9) |
| Single shortage | 42 (24.4) |
| Two shortages | 47 (27.3) |
| Three or more shortages | 78 (45.3) |
| Did not answer | 5 (2.9) |
| Average time to regularize biologic distribution | |
| One month | 44 (25.6) |
| Two months | 64 (37.2) |
| Three or more months | 56 (32.6) |
| Did not answer | 7 (2.4) |
| Infusion or storage explanations * | |
| Yes | 140 (68.3) |
| No | 53 (25.9) |
| Explanations regarding the lack of dispensation | |
| Yes | 113 (65.7) |
| No | 48 (27.9) |
| Did not answer | 12 (5.8) |
| Success in contacting the high-cost pharmacy | |
| Yes | 106 (80.3) |
| Easy contact | 68 (51.5) |
| Difficult contact | 48 (36.4) |
| No | 16 (12.1) |
| Did not answer | 6 (2.9) |
| Bureaucratic process | |
| Yes | 188 (91.7) |
| No | 12 (5.8) |
| Did not answer | 5 (2.9) |
| Variable | n (%) |
|---|---|
| Delivery preference | |
| High-cost pharmacy | 92 (44.9) |
| Another place | 105 (51.2) |
| Infusion clinic | 42 (40.0) |
| Hospital | 27 (25.7) |
| Infusion clinic or hospital | 36 (34.3) |
| Did not answer | 8 (3.9) |
| Schedule the biologic at the infusion clinic | |
| Easy | 183 (89.3) |
| Difficult | 5 (2.4) |
| Did not answer | 17 (8.3) |
| Feeling of impairment of treatment * | |
| Yes | 101 (58.7) |
| No | 54 (31.4) |
| Did not answer | 17 (9.9) |
| Aware of the pharmaceutical industry program | |
| Yes | 95 (46.3) |
| No | 101 (49.3) |
| Did not answer | 9 (4.4) |
| Importance of starting the treatment by industry | |
| Yes | 151 (73.7) |
| No | 26 (12.7) |
| Did not answer | 28 (13.6) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parra, R.S.; da Costa Ferreira, S.; Machado, V.F.; Nigro, C.M.C.; da Rocha, J.J.R.; de Almeida Troncon, L.E.; Feres, O. Access to High-Cost Biological Agents: Perceptions of Brazilian Patients with Inflammatory Bowel Diseases. J. Clin. Med. 2023, 12, 2672. https://doi.org/10.3390/jcm12072672
Parra RS, da Costa Ferreira S, Machado VF, Nigro CMC, da Rocha JJR, de Almeida Troncon LE, Feres O. Access to High-Cost Biological Agents: Perceptions of Brazilian Patients with Inflammatory Bowel Diseases. Journal of Clinical Medicine. 2023; 12(7):2672. https://doi.org/10.3390/jcm12072672
Chicago/Turabian StyleParra, Rogerio Serafim, Sandro da Costa Ferreira, Vanessa Foresto Machado, Cintia Maura Caseiro Nigro, José Joaquim Ribeiro da Rocha, Luiz Ernesto de Almeida Troncon, and Omar Feres. 2023. "Access to High-Cost Biological Agents: Perceptions of Brazilian Patients with Inflammatory Bowel Diseases" Journal of Clinical Medicine 12, no. 7: 2672. https://doi.org/10.3390/jcm12072672
APA StyleParra, R. S., da Costa Ferreira, S., Machado, V. F., Nigro, C. M. C., da Rocha, J. J. R., de Almeida Troncon, L. E., & Feres, O. (2023). Access to High-Cost Biological Agents: Perceptions of Brazilian Patients with Inflammatory Bowel Diseases. Journal of Clinical Medicine, 12(7), 2672. https://doi.org/10.3390/jcm12072672






