Relationship of Glycated Hemoglobin A1c with All-Cause and Cardiovascular Mortality among Patients with Hypertension
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Demographic Characteristics and Biochemical Covariates
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
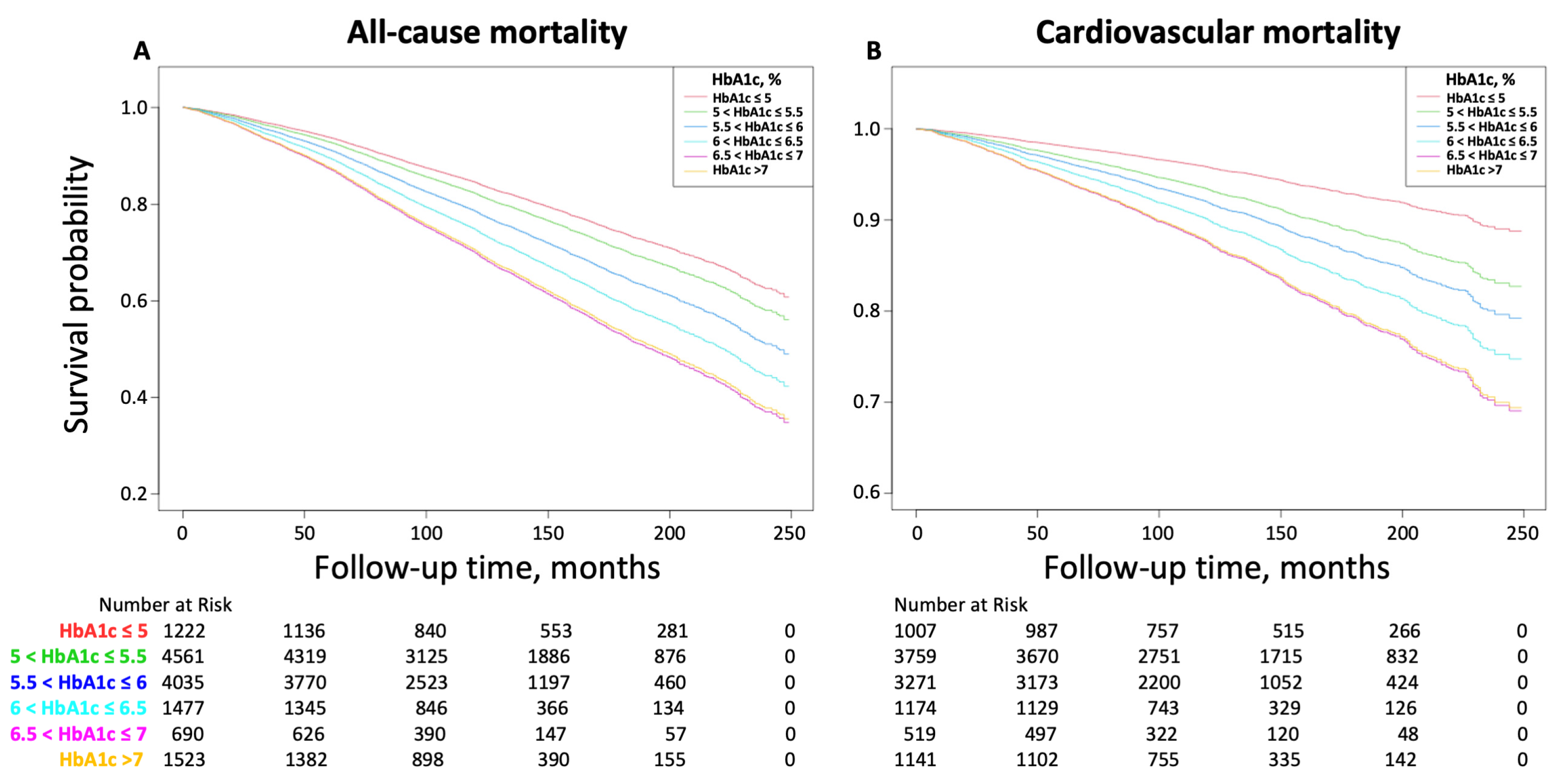
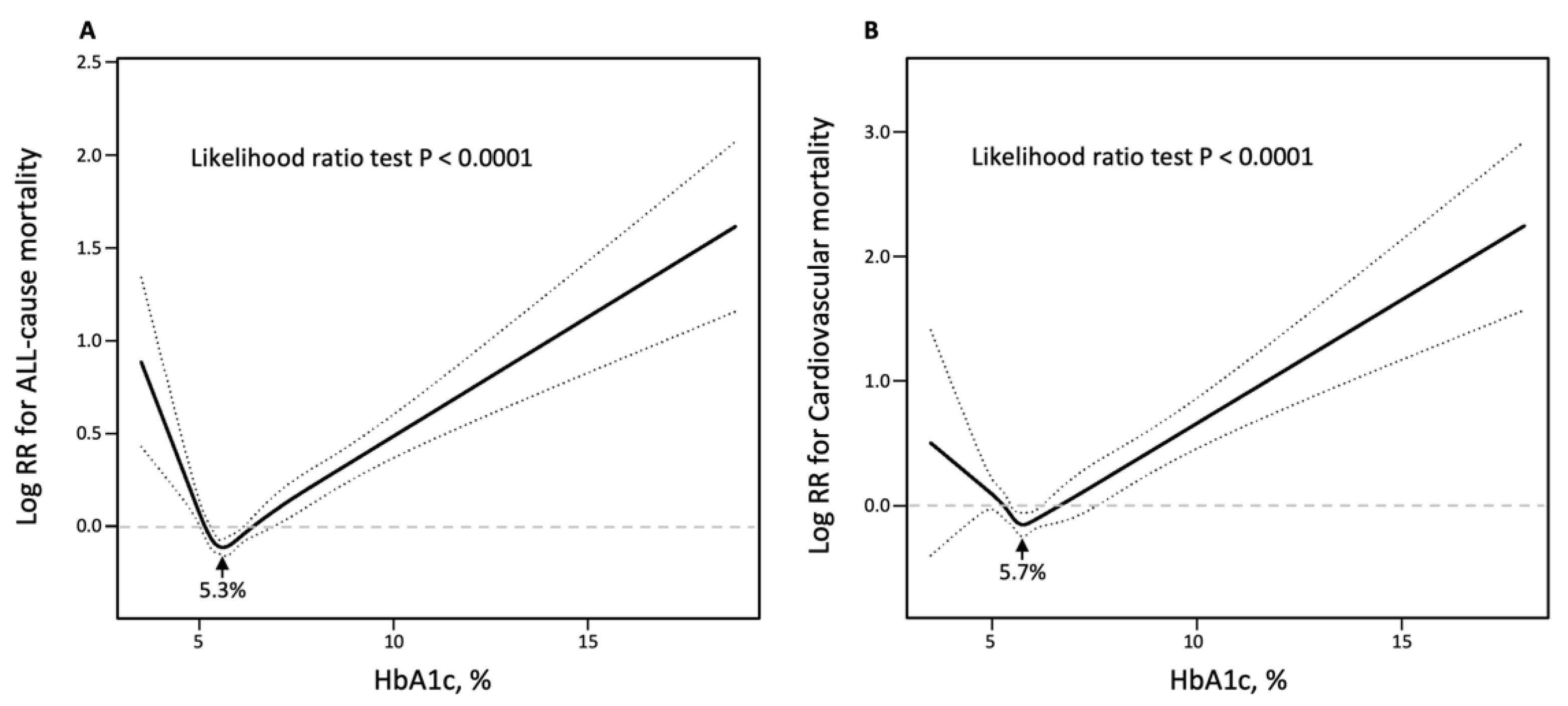
3.2. Relationship between HbA1c and All-Cause and Cardiovascular Mortality
3.3. Subgroups Analysis of the Risk of All-Cause and Cardiovascular Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Collaborators GBDRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Schutte, A.E.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Tsimihodimos, V.; Gonzalez-Villalpando, C.; Meigs, J.B.; Ferrannini, E. Hypertension and Diabetes Mellitus: Coprediction and Time Trajectories. Hypertension 2018, 71, 422–428. [Google Scholar] [CrossRef]
- Qiu, S.; Du, Z.; Li, W.; Chen, J.; Wu, H.; Liu, J.; Cai, M.; Wang, B.; Guo, H.; Sun, Z.; et al. Exploration and Validation of the Performance of Hemoglobin A1c in Detecting Diabetes in Community-Dwellers with Hypertension. Ann. Lab. Med. 2020, 40, 457–465. [Google Scholar] [CrossRef]
- Petrie, J.R.; Guzik, T.J.; Touyz, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018, 34, 575–584. [Google Scholar] [CrossRef]
- American Diabetes. A Diagnosis and classification of diabetes mellitus. Diabetes Care 2010, 33, S62–S69. [Google Scholar] [CrossRef]
- Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2011.
- Menon, V.; Greene, T.; Pereira, A.A.; Wang, X.; Beck, G.J.; Kusek, J.W.; Collins, A.J.; Levey, A.S.; Sarnak, M.J. Glycosylated hemoglobin and mortality in patients with nondiabetic chronic kidney disease. J. Am. Soc. Nephrol. 2005, 16, 3411–3417. [Google Scholar] [CrossRef]
- Andersson, C.; van Gaal, L.; Caterson, I.D.; Weeke, P.; James, W.P.; Coutinho, W.; Finer, N.; Sharma, A.M.; Maggioni, A.P.; Torp-Pedersen, C.; et al. Relationship between HbA1c levels and risk of cardiovascular adverse outcomes and all-cause mortality in overweight and obese cardiovascular high-risk women and men with type 2 diabetes. Diabetologia 2012, 55, 2348–2355. [Google Scholar] [CrossRef]
- Inoue, K.; Nianogo, R.; Telesca, D.; Goto, A.; Khachadourian, V.; Tsugawa, Y.; Sugiyama, T.; Mayeda, E.R.; Ritz, B. Low HbA1c levels and all-cause or cardiovascular mortality among people without diabetes: The US National Health and Nutrition Examination Survey 1999–2015. Int. J. Epidemiol. 2021, 50, 1373–1383. [Google Scholar] [CrossRef]
- Mongraw-Chaffin, M.; Bertoni, A.G.; Golden, S.H.; Mathioudakis, N.; Sears, D.D.; Szklo, M.; Anderson, C.A.M. Association of Low Fasting Glucose and HbA1c with Cardiovascular Disease and Mortality: The MESA Study. J. Endocr. Soc. 2019, 3, 892–901. [Google Scholar] [CrossRef]
- Blaum, C.S.; Volpato, S.; Cappola, A.R.; Chaves, P.; Xue, Q.L.; Guralnik, J.M.; Fried, L.P. Diabetes, hyperglycaemia and mortality in disabled older women: The Women’s Health and Ageing Study I. Diabet. Med. 2005, 22, 543–550. [Google Scholar] [CrossRef]
- Anyanwagu, U.; Mamza, J.; Donnelly, R.; Idris, I. Relationship between HbA1c and all-cause mortality in older patients with insulin-treated type 2 diabetes: Results of a large UK Cohort Study. Age Ageing 2019, 48, 235–240. [Google Scholar] [CrossRef]
- Goode, K.M.; John, J.; Rigby, A.S.; Kilpatrick, E.S.; Atkin, S.L.; Bragadeesh, T.; Clark, A.L.; Cleland, J.G. Elevated glycated haemoglobin is a strong predictor of mortality in patients with left ventricular systolic dysfunction who are not receiving treatment for diabetes mellitus. Heart 2009, 95, 917–923. [Google Scholar] [CrossRef]
- Ford, E.S.; Giles, W.H.; Dietz, W.H. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA 2002, 287, 356–359. [Google Scholar] [CrossRef]
- Palmer, M.K.; Toth, P.P. Trends in Lipids, Obesity, Metabolic Syndrome, and Diabetes Mellitus in the United States: An NHANES Analysis (2003–2004 to 2013–2014). Obesity 2019, 27, 309–314. [Google Scholar] [CrossRef]
- American Diabetes. A 2 Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S13–S27. [Google Scholar] [CrossRef]
- Huang, Y.Q.; Liu, L.; Huang, J.Y.; Chen, C.L.; Yu, Y.L.; Lo, K.; Feng, Y.Q. Prediabetes and risk for all-cause and cardiovascular mortality based on hypertension status. Ann. Transl. Med. 2020, 8, 1580. [Google Scholar] [CrossRef]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ortiz, E.; et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef]
- Yan, Y.Q.; Chen, J.; Huang, Y.Q. A Non-Linear Association of High-Density Lipoprotein Cholesterol with All-Cause and Cause-Specific Mortality in Diabetic Patients. Diabetes Metab. Syndr. Obes. 2021, 14, 2851–2862. [Google Scholar] [CrossRef]
- Cavero-Redondo, I.; Peleteiro, B.; Alvarez-Bueno, C.; Rodriguez-Artalejo, F.; Martinez-Vizcaino, V. Glycated haemoglobin A1c as a risk factor of cardiovascular outcomes and all-cause mortality in diabetic and non-diabetic populations: A systematic review and meta-analysis. BMJ Open 2017, 7, e015949. [Google Scholar] [CrossRef]
- Sakurai, M.; Saitoh, S.; Miura, K.; Nakagawa, H.; Ohnishi, H.; Akasaka, H.; Kadota, A.; Kita, Y.; Hayakawa, T.; NIPPON DATA90 Research Group. HbA1c and the risks for all-cause and cardiovascular mortality in the general Japanese population: NIPPON DATA90. Diabetes Care 2013, 36, 3759–3765. [Google Scholar] [CrossRef]
- Brewer, N.; Wright, C.S.; Travier, N.; Cunningham, C.W.; Hornell, J.; Pearce, N.; Jeffreys, M. A New Zealand linkage study examining the associations between A1C concentration and mortality. Diabetes Care 2008, 31, 1144–1149. [Google Scholar] [CrossRef]
- Creager, M.A.; Luscher, T.F.; Cosentino, F.; Beckman, J.A. Diabetes and vascular disease: Pathophysiology, clinical consequences, and medical therapy: Part I. Circulation 2003, 108, 1527–1532. [Google Scholar] [CrossRef]
- Brownlee, M. The pathobiology of diabetic complications: A unifying mechanism. Diabetes 2005, 54, 1615–1625. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Block, G.; Horwich, T.; Fonarow, G.C. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J. Am. Coll. Cardiol. 2004, 43, 1439–1444. [Google Scholar] [CrossRef]
- Wright, R.J.; Frier, B.M. Vascular disease and diabetes: Is hypoglycaemia an aggravating factor? Diabetes Metab. Res. Rev. 2008, 24, 353–363. [Google Scholar] [CrossRef]
- Frier, B.M.; Schernthaner, G.; Heller, S.R. Hypoglycemia and cardiovascular risks. Diabetes Care 2011, 34, S132–S137. [Google Scholar] [CrossRef]


| Total | HbA1c ≤ 5 | 5 < HbA1c ≤ 5.5 | 5.5 < HbA1c ≤ 6 | 6 < HbA1c ≤ 6.5 | 6.5 < HbA1c ≤ 7 | HbA1c > 7 | p | |
|---|---|---|---|---|---|---|---|---|
| N | 13,508 | 1222 | 4561 | 4035 | 1477 | 690 | 1523 | |
| Age, years | 58.55 ± 15.56 | 48.91 ± 17.38 | 55.77 ± 16.65 | 60.91 ± 14.38 | 63.97 ± 12.54 | 63.99 ± 12.18 | 60.67 ± 12.15 | <0.001 |
| Male, N (%) | 6787 (50.24) | 609 (49.84) | 2287 (50.14) | 2055 (50.93) | 778 (52.67) | 323 (46.81) | 735 (48.26) | 0.075 |
| Body mass index, kg/m2 | 30.45 ± 6.91 | 28.51 ± 6.52 | 29.23 ± 6.31 | 30.59 ± 6.93 | 32.00 ± 7.06 | 32.82 ± 7.47 | 32.71 ± 7.21 | <0.001 |
| Systolic blood pressure, mmHg | 135.80 ± 20.78 | 132.32 ± 20.94 | 135.38 ± 20.46 | 136.71 ± 20.92 | 136.13 ± 20.15 | 134.84 ± 19.71 | 137.53 ± 21.91 | <0.001 |
| Diastolic blood pressure, mmHg | 73.53 ± 14.05 | 75.53 ± 14.10 | 75.24 ± 13.71 | 73.53 ± 13.96 | 71.17 ± 13.79 | 69.39 ± 14.50 | 70.94 ± 14.17 | <0.001 |
| Race, N (%) | <0.001 | |||||||
| Mexican American | 2161 (16.00) | 132 (10.80) | 676 (14.82) | 621 (15.39) | 216 (14.62) | 126 (18.26) | 390 (25.61) | |
| Other Hispanic | 948 (7.02) | 64 (5.24) | 273 (5.99) | 291 (7.21) | 136 (9.21) | 57 (8.26) | 127 (8.34) | |
| Non-Hispanic White | 6259 (46.34) | 680 (55.65) | 2528 (55.43) | 1811 (44.88) | 536 (36.29) | 252 (36.52) | 452 (29.68) | |
| Non-Hispanic Black | 3337 (24.70) | 285 (23.32) | 867 (19.01) | 1046 (25.92) | 486 (32.90) | 206 (29.86) | 447 (29.35) | |
| Asian and other Race | 803 (5.94) | 61 (4.99) | 217 (4.76) | 266 (6.59) | 103 (6.97) | 49 (7.10) | 107 (7.03) | |
| Education, N (%) | <0.001 | |||||||
| Lower than high school | 4374 (32.38) | 274 (22.42) | 1310 (28.72) | 1304 (32.32) | 532 (36.02) | 273 (39.57) | 681 (44.71) | |
| High school | 3329 (24.64) | 285 (23.32) | 1102 (24.16) | 1053 (26.10) | 400 (27.08) | 168 (24.35) | 321 (21.08) | |
| More than high school | 5805 (42.97) | 663 (54.26) | 2149 (47.12) | 1678 (41.59) | 545 (36.90) | 249 (36.09) | 521 (34.21) | |
| Smoking, N (%) | <0.001 | |||||||
| Never Smoker | 6813 (50.44) | 620 (50.74) | 2306 (50.56) | 2051 (50.83) | 716 (48.48) | 339 (49.13) | 781 (51.28) | |
| Current Smoker | 2594 (19.20) | 286 (23.40) | 924 (20.26) | 771 (19.11) | 249 (16.86) | 109 (15.80) | 255 (16.74) | |
| Ex-Smoker | 4101 (30.36) | 316 (25.86) | 1331 (29.18) | 1213 (30.06) | 512 (34.66) | 242 (35.07) | 487 (31.98) | |
| Diabetes diagnosis, N (%) | <0.001 | |||||||
| No pre-diabetes | 5339 (39.52) | 1029 (84.21) | 3572 (78.32) | 738 (18.29) | 0 (0.00) | 0 (0.00) | 0 (0.00) | |
| Pre-diabetes | 4563 (33.78) | 150 (12.27) | 819 (17.96) | 2812 (69.69) | 782 (52.95) | 0 (0.00) | 0 (0.00) | |
| Diabetes | 3606 (26.70) | 43 (3.52) | 170 (3.73) | 485 (12.02) | 695 (47.05) | 690 (100.00) | 1523 (100.00) | |
| Coronary heart disease, N (%) | 1522 (11.27) | 64 (5.24) | 406 (8.90) | 467 (11.57) | 206 (13.95) | 116 (16.81) | 263 (17.27) | <0.001 |
| Acute myocardial infarction, N (%) | 1027 (7.60) | 36 (2.95) | 277 (6.07) | 308 (7.63) | 145 (9.82) | 84 (12.17) | 177 (11.62) | <0.001 |
| Chronic heart failure, N (%) | 755 (5.59) | 30 (2.45) | 194 (4.25) | 208 (5.15) | 111 (7.52) | 74 (10.72) | 138 (9.06) | <0.001 |
| Stroke, N (%) | 829 (6.14) | 58 (4.75) | 224 (4.91) | 252 (6.25) | 115 (7.79) | 54 (7.83) | 126 (8.27) | <0.001 |
| HbA1c, % | 5.98 ± 1.24 | 4.83 ± 0.22 | 5.33 ± 0.13 | 5.77 ± 0.14 | 6.26 ± 0.14 | 6.78 ± 0.14 | 8.76 ± 1.71 | <0.001 |
| Fasting blood glucose, mmol/L | 6.09 ± 2.54 | 5.00 ± 0.72 | 5.17 ± 0.75 | 5.50 ± 0.99 | 6.18 ± 1.41 | 7.12 ± 2.04 | 10.71 ± 4.73 | <0.001 |
| Creatinine, mg/dL | 85.73 ± 54.06 | 86.58 ± 76.68 | 83.23 ± 56.50 | 84.71 ± 35.56 | 87.07 ± 40.57 | 93.41 ± 77.70 | 90.48 ± 62.48 | <0.001 |
| Hemoglobin, g/L | 14.11 ± 1.55 | 14.10 ± 1.78 | 14.32 ± 1.51 | 14.11 ± 1.49 | 13.85 ± 1.52 | 13.79 ± 1.59 | 13.86 ± 1.58 | <0.001 |
| Triglyceride, mg/dL | 134.0 (90.0–202.0) | 116.0 (77.0–172.0) | 123.0 (84.0–185.0) | 134.0 (92.0–193.0) | 144.0 (99.0–212.0) | 154.0 (104.3–233.8) | 173.0 (114.5–266.5) | <0.001 |
| Total cholesterol, mg/dL | 200.13 ± 43.65 | 195.61 ± 40.24 | 203.31 ± 41.72 | 203.78 ± 43.61 | 193.48 ± 44.09 | 189.08 ± 46.87 | 196.06 ± 47.72 | <0.001 |
| HDL-C, mg/dL | 51.95 ± 15.92 | 55.38 ± 17.81 | 54.08 ± 16.84 | 52.32 ± 15.46 | 49.24 ± 13.76 | 47.65 ± 14.11 | 46.38 ± 12.96 | <0.001 |
| Antihypertensive drugs, N (%) | 8015 (59.34) | 508 (41.57) | 2212 (48.50) | 2506 (62.11) | 1091 (73.87) | 565 (81.88) | 1133 (74.39) | <0.001 |
| Hypoglycemic agents, N (%) | 2423 (17.94) | 22 (1.80) | 81 (1.78) | 312 (7.73) | 434 (29.38) | 421 (61.01) | 1153 (75.71) | <0.001 |
| Aspirin, N (%) | 322 (2.38) | 11 (0.90) | 50 (1.10) | 95 (2.35) | 62 (4.20) | 27 (3.91) | 77 (5.06) | <0.001 |
| Clopidogrel, N (%) | 438 (3.24) | 19 (1.55) | 104 (2.28) | 128 (3.17) | 66 (4.47) | 37 (5.36) | 84 (5.52) | <0.001 |
| Statin, N (%) | 3742 (27.70) | 129 (10.56) | 864 (18.94) | 1116 (27.66) | 628 (42.52) | 326 (47.25) | 679 (44.58) | <0.001 |
| All-cause mortality, N (%) | 3760 (27.84) | 278 (22.75) | 1154 (25.30) | 1089 (26.99) | 440 (29.79) | 245 (35.51) | 554 (36.38) | <0.001 |
| Cardiovascular mortality, N (%) | 1123 (10.33) | 63 (6.26) | 352 (9.36) | 325 (9.94) | 137 (11.67) | 74 (14.26) | 172 (15.07) | <0.001 |
| Model 1 HR (95% CI), p | Model 2 HR (95% CI), p | Model 3 HR (95% CI), p | |
|---|---|---|---|
| All-cause mortality | |||
| HbA1c | 1.13 (1.11, 1.16), <0.0001 | 1.15 (1.12, 1.18), <0.0001 | 1.11 (1.08, 1.15), <0.0001 |
| HbA1c threshold value | |||
| ≤threshold value 5.3 | 1.04 (0.77, 1.40), 0.8085 | 0.53 (0.40, 0.70), <0.0001 | 0.68 (0.51, 0.90), 0.0078 |
| >threshold value 5.3 | 1.10 (1.08, 1.13), <0.0001 | 1.19 (1.16, 1.22), <0.0001 | 1.14 (1.11, 1.18), <0.0001 |
| HbA1c categorical | |||
| HbA1c ≤ 5 | 0.86 (0.76, 0.98), 0.0256 | 1.32 (1.16, 1.51), <0.0001 | 1.27 (1.11, 1.45), 0.0004 |
| 5 < HbA1c ≤ 5.5 | Reference | Reference | Reference |
| 5.5 < HbA1c ≤ 6 | 1.23 (1.14, 1.34), <0.0001 | 0.98 (0.90, 1.06), 0.6200 | 0.96 (0.88, 1.05), 0.3660 |
| 6 < HbA1c ≤ 6.5 | 1.49 (1.33, 1.66), <0.0001 | 1.13 (1.01, 1.27), 0.0294 | 1.07 (0.95, 1.20), 0.2622 |
| 6.5 < HbA1c ≤ 7 | 1.82 (1.59, 2.09), <0.0001 | 1.31 (1.14, 1.51), 0.0001 | 1.08 (0.93, 1.27), 0.2988 |
| HbA1c > 7 | 1.79 (1.61, 1.98), <0.0001 | 1.73 (1.56, 1.92), <0.0001 | 1.45 (1.27, 1.66), <0.0001 |
| p for trend | <0.0001 | <0.0001 | <0.0001 |
| Cardiovascular mortality | |||
| HbA1c | 1.17 (1.13, 1.21), <0.0001 | 1.20 (1.15, 1.25), <0.0001 | 1.17 (1.11, 1.23), <0.0001 |
| HbA1c threshold value | |||
| ≤threshold value 5.7 | 1.80 (1.33, 2.45), 0.0002 | 0.76 (0.56, 1.03), 0.0776 | 0.77 (0.57, 1.05), 0.0969 |
| >threshold value 5.7 | 1.09 (1.04, 1.14), 0.0005 | 1.24 (1.18, 1.30), <0.0001 | 1.22 (1.16, 1.29), <0.0001 |
| HbA1c categorical | |||
| HbA1c ≤ 5 | 0.51 (0.39, 0.67), <0.0001 | 1.17 (0.89, 1.53), 0.2681 | 1.21 (0.92, 1.59), 0.1829 |
| 5 < HbA1c ≤ 5.5 | 0.81 (0.70, 0.95), 0.0078 | 1.13 (0.97, 1.32), 0.1080 | 1.22 (1.04, 1.42), 0.0135 |
| 5.5 < HbA1c ≤ 6 | Reference | Reference | Reference |
| 6 < HbA1c ≤ 6.5 | 1.25 (1.02, 1.53), 0.0290 | 1.24 (1.01, 1.51), 0.0386 | 1.19 (0.96, 1.46), 0.1051 |
| 6.5 < HbA1c ≤ 7 | 1.59 (1.23, 2.05), 0.0003 | 1.40 (1.09, 1.81), 0.0089 | 1.23 (0.93, 1.62), 0.1510 |
| HbA1c > 7 | 1.57 (1.30, 1.89), <0.0001 | 2.05 (1.70, 2.48), <0.0001 | 1.85 (1.47, 2.33), <0.0001 |
| p for trend | <0.0001 | <0.0001 | 0.0003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeng, R.; Zhang, Y.; Xu, J.; Kong, Y.; Tan, J.; Guo, L.; Zhang, M. Relationship of Glycated Hemoglobin A1c with All-Cause and Cardiovascular Mortality among Patients with Hypertension. J. Clin. Med. 2023, 12, 2615. https://doi.org/10.3390/jcm12072615
Zeng R, Zhang Y, Xu J, Kong Y, Tan J, Guo L, Zhang M. Relationship of Glycated Hemoglobin A1c with All-Cause and Cardiovascular Mortality among Patients with Hypertension. Journal of Clinical Medicine. 2023; 12(7):2615. https://doi.org/10.3390/jcm12072615
Chicago/Turabian StyleZeng, Ruixiang, Yuzhuo Zhang, Junpeng Xu, Yongjie Kong, Jiawei Tan, Liheng Guo, and Minzhou Zhang. 2023. "Relationship of Glycated Hemoglobin A1c with All-Cause and Cardiovascular Mortality among Patients with Hypertension" Journal of Clinical Medicine 12, no. 7: 2615. https://doi.org/10.3390/jcm12072615
APA StyleZeng, R., Zhang, Y., Xu, J., Kong, Y., Tan, J., Guo, L., & Zhang, M. (2023). Relationship of Glycated Hemoglobin A1c with All-Cause and Cardiovascular Mortality among Patients with Hypertension. Journal of Clinical Medicine, 12(7), 2615. https://doi.org/10.3390/jcm12072615








