Interstitial Lung Disease and Pulmonary Damage in Primary Sjögren’s Syndrome: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Data Extraction and Quality Assessment
2.5. Assessment of Methodological Quality
2.6. Statistical Analysis
3. Results
3.1. Study Selection and Characteristics
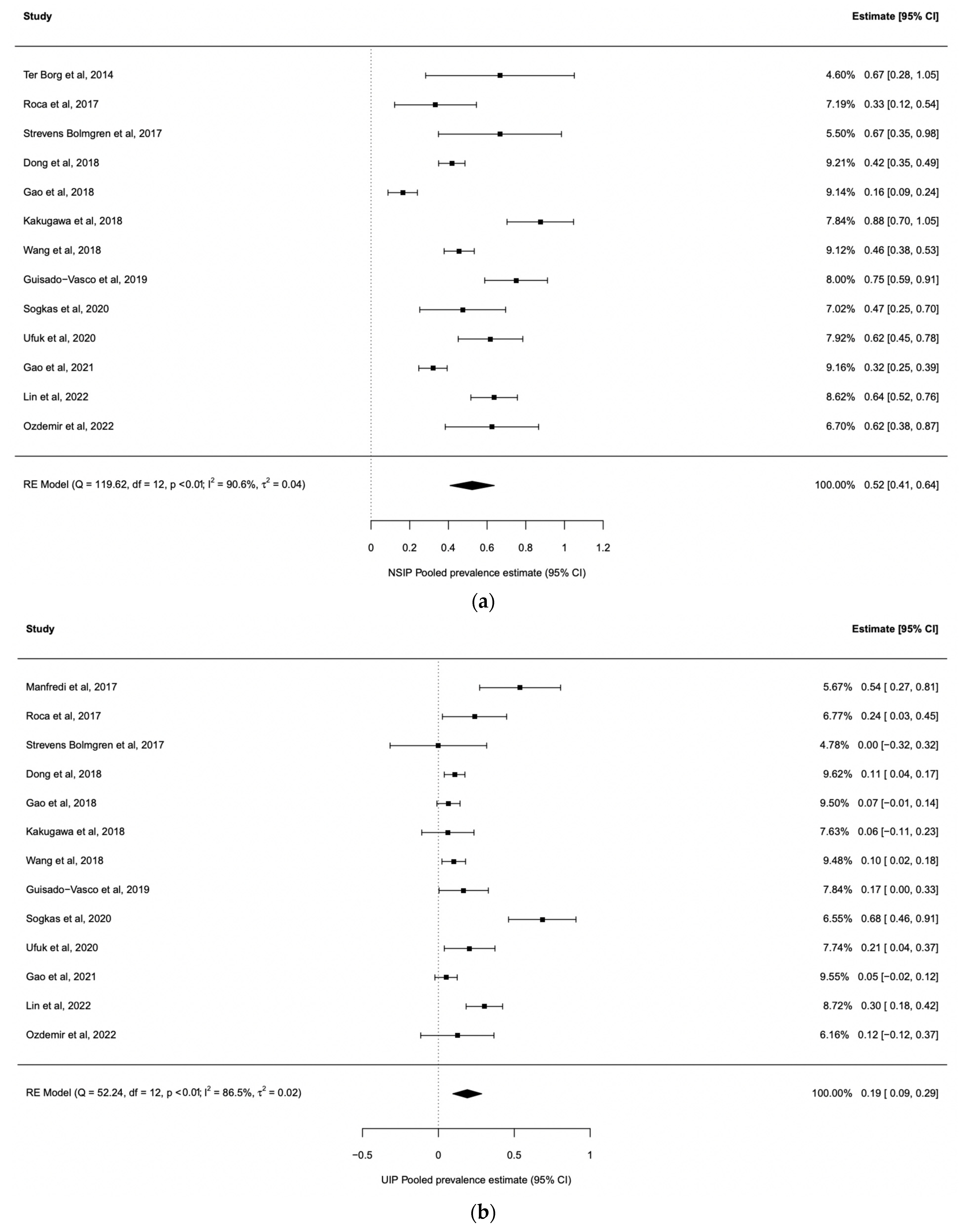
3.2. ILD Prevalence in Sjogren’s Syndrome
3.3. Risk Factors Associated with pSS-ILD
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ramos-Casals, M.; Brito-Zerón, P.; Sisó-Almirall, A.; Bosch, X. Primary Sjogren syndrome. BMJ 2012, 344, e3821. [Google Scholar] [CrossRef]
- Fox, R.I. Sjögren’s syndrome. Lancet 2005, 366, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Ito, I.; Nagai, S.; Kitaichi, M.; Nicholson, A.G.; Johkoh, T.; Noma, S.; Kim, D.S.; Handa, T.; Izumi, T.; Mishima, M. Pulmonary manifestations of primary Sjogren’s syndrome: A clinical, radiologic, and pathologic study. Am. J. Respir. Crit. Care Med. 2005, 171, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Cafaro, G.; Bursi, R.; Chatzis, L.G.; Fulvio, G.; Ferro, F.; Bartoloni, E.; Baldini, C. One year in review 2021, Sjögren’s syndrome. Clin. Exp. Rheumatol. 2021, 133, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Nannini, C.; Jebakumar, A.J.; Crowson, C.S.; Ryu, J.H.; Matteson, E.L. Primary Sjogren’s syndrome 1976-2005 and associated interstitial lung disease: A population-based study of incidence and mortality. BMJ Open 2013, 3, e003569. [Google Scholar] [CrossRef]
- Sambataro, G.; Ferro, F.; Orlandi, M.; Sambataro, D.; Torrisi, S.E.; Quartuccio, L.; Vancheri, C.; Baldini, C.; Cerinic, M.M. Clinical, morphological features and prognostic factors associated with interstitial lung disease in primary Sjӧgren’s syndrome: A systematic review from the Italian Society of Rheumatology. Autoimmun. Rev. 2020, 19, 102447. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Strek, M.E.; Cottin, V.; Dellaripa, P.F.; Bernstein, E.J.; Brown, K.K.; Danoff, S.K.; Distler, O.; Hirani, N.; Jones, K.D.; et al. Proceedings of the American College of Rheumatology/Association of Physicians of Great Britain and Ireland Connective Tissue Disease-Associated Interstitial Lung Disease Summit: A Multidisciplinary Approach to Address Challenges and Opportunities. Arthritis Rheumatol. 2019, 71, 182–195. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Brooke, B.S.; Schwartz, T.A.; Pawlik, T.M. MOOSE Reporting Guidelines for Meta-analyses of Observational Studies. JAMA Surg. 2021, 156, 787–788. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Hoy, D.; Brooks, P.; Woolf, A.; Blyth, F.; March, L.; Bain, C.; Baker, P.; Smith, E.; Buchbinder, R. Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 2012, 65, 934–939. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality if Nonrandomized Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.html (accessed on 1 December 2022).
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Sterne, J.A.; Egger, M. Funnel plots for detecting bias in metaanalysis: Guidelines on choice of axis. J. Clin. Epidemiol. 2001, 54, 1046–1055. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in metaanalysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Constantopoulos, S.H.; Papadimitriou, C.S.; Moutsopoulos, H.M. Respiratory manifestations in primary Sjogren’s syndrome. A clinical, functional, and histologic study. Chest 1985, 88, 226–229. [Google Scholar] [CrossRef]
- Papathanasiou, M.P.; Constantopoulos, S.H.; Tsampoulas, C. Reappraisal of respiratory abnormalities in primary and secondary Sjogren’s syndrome. A Control. Study Chest 1986, 90, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Papiris, S.A.; Maniati, M.; Constantopoulos, S.H.; Roussos, C.; Moutsopoulos, H.M.; Skopouli, F.N. Lung involvement in primary Sjogren’s syndrome is mainly related to the small airway disease. Ann. Rheum. Dis. 1999, 58, 61–64. [Google Scholar] [CrossRef]
- Kampolis, C.F.; Fragkioudaki, S.; Mavragani, C.P.; Zormpala, A.; Samakovli, A.; Moutsopoulos, H.M. Prevalence and spectrum of symptomatic pulmonary involvement in primary Sjogren’s syndrome. Clin. Exp. Rheumatol. 2018, 36, 94–101. [Google Scholar] [PubMed]
- Kvarnström, M.; Ottosson, V.; Nordmark, B.; Wahren-Herlenius, M. Incident cases of primary Sjögren’s syndrome during a 5-year period in Stockholm County: A descriptive study of the patients and their characteristics. Scand. J. Rheumatol. 2015, 44, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Ramírez Sepúlveda, J.I.; Kvarnström, M.; Eriksson, P.; Mandl, T.; Norheim, K.B.; Johnsen, S.J.; Hammenfors, D.; Jonsson, M.V.; Skarstein, K.; Brun, J.G.; et al. Long-term follow-up in primary Sjogren’s syndrome reveals differences in clinical presentation between female and male patients. Biol. Sex. Differ. 2017, 8, 25. [Google Scholar] [CrossRef]
- Strevens Bolmgren, V.; Olsson, P.; Wollmer, P.; Hesselstrand, R.; Mandl, T. Respiratory symptoms are poor predictors of concomitant chronic obstructive pulmonary disease in patients with primary Sjogren’s syndrome. Rheumatol. Int. 2017, 37, 813–818. [Google Scholar] [CrossRef]
- Cervera, R.; Font, J.; Ramos-Casals, M.; García-Carrasco, M.; Rosas, J.; Morlà, R.M.; Muñoz, F.J.; Artigues, A.; Pallarés, L.; Ingelmo, M. Primary Sjogren’s syndrome in men: Clinical and immunological characteristics. LUPUS 2000, 9, 61–64. [Google Scholar] [CrossRef]
- Ter Borg, E.J.; Kelder, J.C. Lower prevalence of extra-glandular manifestations and anti-SSB antibodies in patients with primary Sjogren’s syndrome and widespread pain: Evidence for a relatively benign subset. Clin. Exp. Rheumatol. 2014, 32, 349–353. [Google Scholar]
- Manfredi, A.; Sebastiani, M.; Cerri, S.; Cassone, G.; Bellini, P.; Casa, G.D.; Luppi, F.; Ferri, C. Prevalence and characterization of non-sicca onset primary Sjogren syndrome with interstitial lung involvement. Clin. Rheumatol. 2017, 36, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Botsios, C.; Furlan, A.; Ostuni, P.; Sfriso, P.; Andretta, M.; Ometto, F.; Raffeiner, B.; Todesco, S.; Punzi, L. Elderly onset of primary Sjögren’s syndrome: Clinical manifestations, serological features and oral/ocular diagnostic tests. Comparison with adult and young onset of the disease in a cohort of 336 Italian patients. Joint Bone Spine 2011, 78, 171–174. [Google Scholar] [CrossRef]
- Wang, Y.; Hou, Z.; Qiu, M.; Ye, Q. Risk factors for primary Sjogren syndrome-associated interstitial lung disease. J. Thorac. Dis. 2018, 10, 2108–2117. [Google Scholar] [CrossRef]
- Lin, D.F.; Yan, S.M.; Zhao, Y.; Zhang, W.; Li, M.T.; Zeng, X.F.; Zhang, F.-C.; Dong, Y. Clinical and prognostic characteristics of 573 cases of primary Sjogren’s syndrome. Chin. Med. J. 2010, 123, 3252–3257. [Google Scholar]
- Li, X.; Xu, B.; Ma, Y.; Li, X.; Cheng, Q.; Wang, X.; Wang, G.; Qian, L.; Wei, L. Clinical and laboratory profiles of primary Sjogren’s syndrome in a Chinese population: A retrospective analysis of 315 patients. Int. J. Rheum. Dis. 2015, 18, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Li, Y.; Wang, L.; Li, X.F.; Huang, C.B.; Wang, G.C.; Zhang, X.-W.; Zhang, Z.-L.; Zhang, X.; Xiao, W.-G.; et al. Primary Sjögren syndrome in Han Chinese: Clinical and immunological characteristics of 483 patients. Medicine 2015, 94, e667. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Zhou, J.; Guo, X.; Li, Y.; Xu, Y.; Fu, Q.; Lu, Y.; Zheng, Y. A retrospective analysis of distinguishing features of chest HRCT and clinical manifestation in primary Sjogren’s syndrome-related interstitial lung disease in a Chinese population. Clin. Rheumatol. 2018, 37, 2981–2988. [Google Scholar] [CrossRef]
- Gao, H.; Zhang, X.W.; He, J.; Zhang, J.; An, Y.; Sun, Y.; Jia, R.-L.; Li, S.-G.; Zhang, L.-J.; Li, Z.-G. Prevalence, risk factors, and prognosis of interstitial lung disease in a large cohort of Chinese primary Sjogren syndrome patients: A case-control study. Medicine 2018, 97, e11003. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Han, X.L.; Guo, H.X.; Wang, J.; Tang, Y.P.; Gao, C.; Li, X.F. Increases in tumor markers are associated with primary Sjögren’s syndrome-associated interstitial lung disease. Ther. Adv. Chronic Dis. 2020, 11, 2040622320944802. [Google Scholar] [CrossRef]
- Gao, H.; Sun, Y.; Zhang, X.Y.; Xie, L.; Zhang, X.W.; Zhong, Y.C.; Zhang, J.; Hou, Y.-K.; Li, Z.-G. Characteristics and mortality in primary Sjögren syndrome-related interstitial lung disease. Medicine 2021, 100, e26777. [Google Scholar] [CrossRef]
- Lin, W.; Xin, Z.; Zhang, J.; Liu, N.; Ren, X.; Liu, M.; Su, Y.; Liu, Y.; Yang, L.; Guo, S.; et al. Interstitial lung disease in Primary Sjögren’s syndrome. BMC Pulm. Med. 2022, 22, 73. [Google Scholar] [CrossRef] [PubMed]
- Weng, L.; Chen, Y.; Liang, T.; Lin, Y.; Liu, D.; Yu, C.; Hu, Y.; Lui, W.; Liu, Y.; Chen, X.; et al. Biomarkers of interstitial lung disease associated with primary Sjögren’s syndrome. Eur. J. Med. Res. 2022, 27, 199. [Google Scholar] [CrossRef] [PubMed]
- Ufuk, F.; Demirci, M.; Altinisik, G.; Karasu, U. Quantitative analysis of Sjogren’s syndrome related interstitial lung disease with different methods. Eur. J. Radiol. 2020, 128, 109030. [Google Scholar] [CrossRef]
- Sahin Ozdemirel, T.; Ozdemirel, A.E.; Akinci Ozyurek, B.; Yenibertiz, D.; Erdogan, Y. The evaluation of lung involvement and functional capacities in patients diagnosed with primary Sjogren’s syndrome. Int. J. Clin. Pract. 2021, 75, e14635. [Google Scholar] [CrossRef]
- Işık, Ö.Ö.; Yazıcı, A.; Çefle, A. The respiratory manifestations in patients with primary Sjögren’s syndrome: Is. interstitial lung disease related to disease activity? Turk. J. Med. Sci. 2022, 52, 1737–1743. [Google Scholar] [CrossRef]
- Taouli, B.; Brauner, M.W.; Mourey, I.; Lemouchi, D.; Grenier, P.A. Thinsection chest CT findings of primary Sjogren’s syndrome: Correlation with pulmonary function. Eur. Radiol. 2002, 12, 1504–1511. [Google Scholar] [CrossRef]
- Roca, F.; Dominique, S.; Schmidt, J.; Smail, A.; Duhaut, P.; Lévesque, H.; Marie, I. Interstitial lung disease in primary Sjogren’s syndrome. Autoimmun. Rev. 2017, 16, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Ter Borg, E.J.; Kelder, J.C. Development of new extra-glandular manifestations or associated auto-immune diseases after establishing the diagnosis of primary Sjogren’s syndrome: A long-term study of the Antonius Nieuwegein Sjogren (ANS) cohort. Rheumatol. Int. 2017, 37, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Kakugawa, T.; Sakamoto, N.; Ishimoto, H.; Shimizu, T.; Nakamura, H.; Nawata, A.; Ito, C.; Sato, S.; Hanaka, T.; Oda, K.; et al. Lymphocytic focus score is positively related to airway and interstitial lung diseases in primary Sjogren’s syndrome. Respir. Med. 2018, 137, 95–102. [Google Scholar] [CrossRef]
- Guisado-Vasco, P.; Silva, M.; Duarte-Millán, M.A.; Sambataro, G.; Bertolazzi, C.; Pavone, M.O.; Luque-Pinill, J.; Santilli, D.; Sambataro, D.; Torr, S.E.; et al. Quantitative assessment of interstitial lung disease in Sjögren’s syndrome. PLoS ONE 2019, 14, e0224772. [Google Scholar] [CrossRef] [PubMed]
- Sogkas, G.; Hirsch, S.; Olsson, K.M.; Hinrichs, J.B.; Thiele, T.; Seeliger, T.; Skripuletz, T.; Schmidt, R.E.; Witte, T.; Jablonka, A.; et al. Lung Involvement in Primary Sjögren’s Syndrome-An Under-Diagnosed Entity. Front. Med. 2020, 7, 332. [Google Scholar] [CrossRef]
- Vitali, C.; Bombardieri, S.; Jonsson, R.; Moutsopoulos, H.M.; Alexander, E.L.; Carsons, S.E.; Daniels, T.E.; Fox, P.C.; Fox, R.I.; Kassan, S.S.; et al. Classification Criteria for Sjögren’s Syndrome: A Revised Version of the European Criteria Proposed by the American-European Consensus Group. Ann. Rheum. Dis. 2002, 61, 554–558. [Google Scholar] [CrossRef]
- Huang, H.; Xie, W.; Geng, Y.; Fan, Y.; Zhang, Z. Mortality in patients with primary Sjögren’s syndrome: A systematic review and meta-analysis. Rheumatology 2021, 60, 4029–4038. [Google Scholar] [CrossRef]
- He, C.; Chen, Z.; Liu, S.; Chen, H.; Zhang, F. Prevalence and risk factors of interstitial lung disease in patients with primary Sjögren’s syndrome: A systematic review and meta-analysis. Int. J. Rheum. Dis. 2020, 23, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- Ruaro, B.; Baratella, E.; Confalonieri, P.; Wade, B.; Marrocchio, C.; Geri, P.; Busca, A.; Pozzan, R.; Andrisano, A.G.; Cova, M.A.; et al. High-Resolution Computed Tomography: Lights and Shadows in Improving Care for SSc-ILD Patients. Diagnostics 2021, 11, 1960. [Google Scholar] [CrossRef]
- Volkmann, E.R.; Tashkin, D.P.; Sim, M.; Li, N.; Goldmuntz, E.; Keyes-Elstein, L.; Pinckney, A.; Furst, D.E.; Clements, P.J.; Khanna, D.; et al. Short-term progression of interstitial lung disease in systemic sclerosis predicts long-term survival in two independent clinical trial cohorts. Ann. Rheum. Dis. 2019, 78, 122–130. [Google Scholar] [CrossRef]
- Shao, T.; Shi, X.; Yang, S.; Zhang, W.; Li, X.; Shu, J.; Alqalyoobi, S.; Zeki, A.A.; Leung, P.S.; Shuai, Z. Interstitial Lung Disease in Connective Tissue Disease: A Common Lesion with Heterogeneous Mechanisms and Treatment Considerations. Front. Immunol. 2021, 12, 684699. [Google Scholar] [CrossRef]
- Gutsche, M.; Rosen, G.D.; Swigris, J.J. Connective Tissue Disease-associated Interstitial Lung Disease: A review. Curr. Respir. Care Rep. 2012, 1, 224–232. [Google Scholar] [CrossRef]
- Chatzis, L.; Pezoulas, V.C.; Ferro, F.; Gandolfo, S.; Donati, V.; Binutti, M.; Callegher, S.Z.; Venetsanopoulou, A.; Zampeli, E.; Mavrommati, M.; et al. Sjögren’s Syndrome: The Clinical Spectrum of Male Patients. J. Clin. Med. 2020, 9, 2620. [Google Scholar] [CrossRef]
- Brandt, J.E.; Priori, R.; Valesini, G.; Fairweather, D. Sex differences in Sjögren’s syndrome: A comprehensive review of immune mechanisms. Biol. Sex. Differ. 2015, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Walsh, S.L.; Sverzellati, N.; Devaraj, A.; Keir, G.J.; Wells, A.U.; Hansell, D.M. Connective tissue disease related fibrotic lung disease: High resolution computed tomographic and pulmonary function indices as prognostic determinants. Thorax 2014, 69, 216–222. [Google Scholar] [CrossRef]
- Brito-Zerón, P.; Acar-Denizli, N.; Ng, W.F.; Horváth, I.F.; Rasmussen, A.; Seror, R.; Li, X.; Baldini, C.; Gottenberg, J.-E.; Danda, D.; et al. Epidemiological profile and north-south gradient driving baseline systemic involvement of primary Sjögren’s syndrome. Rheumatology 2020, 59, 2350–2359. [Google Scholar] [CrossRef] [PubMed]
- Berardicurti, O.; Ruscitti, P.; Di Benedetto, P.; D’Andrea, S.; Navarini, L.; Marino, A.; Cipriani, P.; Giacomelli, R. Association Between Minor Salivary Gland Biopsy During Sjӧgren’s Syndrome and Serologic Biomarkers: A Systematic Review and Meta-Analysis. Front. Immunol. 2021, 12, 686457. [Google Scholar] [CrossRef]
- Tzioufas, A.G.; Wassmuth, R.; Dafni, U.G.; Guialis, A.; Haga, H.J.; Isenberg, D.A.; Jonsson, R.; Kalden, J.R.; Kiener, H.; Sakarellos, C.; et al. Clinical, immunological, and immunogenetic aspects of autoantibody production against Ro/SSA, La/SSB and their linear epitopes in primary sjögren’s syndrome (pSS): A European multicentre study. Ann. Rheum. Dis. 2002, 61, 398–404. [Google Scholar] [CrossRef]
- Tzioufas, A.G.; Tatouli, I.P.; Moutsopoulos, H.M. Autoantibodies in sjögren’s syndrome: Clinical presentation and regulatory mechanisms. Presse Med. 2012, 41, e451–60. [Google Scholar] [CrossRef]
- Retamozo, S.; Akasbi, M.; Brito-Zerón, P.; Bosch, X.; Bove, A.; Perez-de-Lis, M.; Jimenez, I.; Soto-Cardenas, M.-J.; Gandia, M.; Diaz-Lagares, C.; et al. Anti-Ro52 antibody testing influences the classification and clinical characterisation of primary Sjögren’s syndrome. Clin. Exp. Rheumatol. 2012, 30, 686–692. [Google Scholar] [PubMed]
- Song, J.S.; Do, J.H.; Lee, S.W. The prevalence and the clinical relevance of anti-Ro52 in Korean patients with primary Sjögren’s syndrome. Rheumatol. Int. 2012, 32, 491–495. [Google Scholar] [CrossRef]
- Ruscitti, P.; Berardicurti, O.; Iacono, D.; Pantano, I.; Liakouli, V.; Caso, F.; Emmi, G.; Grembiale, R.D.; Cantatore, F.P.; Atzeni, F.; et al. Parenchymal lung disease in adult onset Still’s disease: An emergent marker of disease severity-characterisation and predictive factors from Gruppo Italiano di Ricerca in Reumatologia Clinica e Sperimentale (GIRRCS) cohort of patients. Arthritis Res. Ther. 2020, 22, 151. [Google Scholar] [CrossRef] [PubMed]
- Ruscitti, P.; Bruno, F.; Berardicurti, O.; Acanfora, C.; Pavlych, V.; Palumbo, P.; Conforti, A.; Carubbi, F.; Di Cola, I.; Di Benedetto, P.; et al. Lung involvement in macrophage activation syndrome and severe COVID-19, results from a cross-sectional study to assess clinical, laboratory and artificial intelligence-radiological differences. Ann. Rheum. Dis. 2020, 79, 1152–1155. [Google Scholar] [CrossRef] [PubMed]
- Saper, V.E.; Chen, G.; Deutsch, G.H.; Guillerman, R.P.; Birgmeier, J.; Jagadeesh, K.; Canna, S.; Schulert, G.; Deterding, R.; Xu, J.; et al. Emergent high fatality lung disease in systemic juvenile arthritis. Ann. Rheum. Dis. 2019, 78, 1722–173. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Casals, M.; Brito-Zerón, P.; Bombardieri, S.; Bootsma, H.; De Vita, S.; Dörner, T.; Fisher, B.A.; Gottenberg, J.-E.; Hernandez-Molina, G.; Kocher, A.; et al. EULAR recommendations for the management of Sjögren’s syndrome with topical and systemic therapies. Ann. Rheum. Dis. 2020, 79, 3–18. [Google Scholar] [CrossRef] [PubMed]



| Study | Design | Country | n | pSS Classification Criteria | F, % | ILD, n (%) | HRCT | NSIP, n (%) | UIP, n (%) | PFTs | DLCO (mmol/min kPa) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Constantopoulos et al., 1985 [17] | Prospective | Greece | 36 | * | 91.7% | 9 (25%) | - | - | - | - | |
| Papathanasiou et al., 1986 [18] | Prospective | Greece | 40 | * | 100% | 15 (37.5%) | - | - | - | yes | 91.23 ± 18.86 |
| Papiris et al., 1999 [19] | Prospective | Greece | 61 | 1993 ECCC | 95% | 19 (31%) | yes | - | - | yes | 85 ± 17.7 |
| Cervera et al., 2000 [24] | Prospective | Spain | 223 | 1993 ECCC | 91.5% | 19 (8.5%) | - | - | - | - | |
| Taouli et al., 2002 [41] | Retrospective | France | 35 | 1993 ECCC | 80% | 12 (34.3%) | yes | yes | 71.9 ± 15.7 | ||
| Lin et al., 2010 [29] | Retrospective | China | 522 | 2002 AECG | 91% | 116 (22.2%) | yes | - | - | - | - |
| Botsios et al., 2011 [27] | Retrospective | Italy | 336 | 2002 AECG | 96% | 5 (1.5%) | yes | - | - | - | - |
| Ter Borg et al., 2014 [25] | Prospective | Netherlands | 83 | 2002 AECG | 89% | 6 (7.2%) | yes | 4 (4.8%) | - | - | |
| Kvarnstrom et al., 2015 [21] | Prospective | Sweden | 199 | 2002 AECG | 93% | 2 (1%) | - | - | - | - | - |
| Li et al., 2015 [30] | Retrospective | China | 315 | 2002 AECG | 96% | 66 (21%) | yes | yes | - | ||
| Zhao et al., 2015 [31] | Retrospective | China | 483 | 2002 AECG | 94% | 59 (12.2%) | yes | - | - | - | - |
| Manfredi et al., 2017 [26] | Prospective | Italy | 77 | 2002 AECG | 88% | 13 (16.9%) | yes | - | 7 (9%) | yes | - |
| Ramirez Sepulveda et al., 2017 [22] | Prospective | Sweden/Norway | 967 | 2002 AECG | 93% | 48 (5%) | - | - | - | - | - |
| Roca et al., 2017 [42] | Retrospective | France | 263 | 2002 AECG | - | 21 (8%) | yes | 7 (33.3%) | 5 (23.8%) | yes | |
| Strevens Bolmgren et al., 2017 [23] | Prospective | Sweden | 51 | 2002 AECG | 96% | 9 (17.6%) | - | 6 (11.7%) | 0 | 6.5 ± 1.9 | |
| Ter Borg et al., 2017 [43] | Retrospective | Netherlands | 140 | 2002 AECG | 89% | 17 (12.1%) | yes | - | - | - | - |
| Dong et al., 2018 [32] | Retrospective | China | 527 | 2002 AECG/2016 ACR EULAR | 88% | 206 (39%) | yes | 86 (41.7%) | 22 (10.7%) | yes | 54.54 ± 21.25 |
| Gao et al., 2018 [33] | Retrospective | China | 853 | 2002 AECG | - | 165 (31.7%) | yes | 27 (39.1%) | 11 (15.9%) | yes | 57.5 ± 21.2 |
| Kakugawa et al., 2018 [44] | Retrospective | Japan | 101 | 2002 AECG | 94% | 32 (1.8%) | yes | 28 (27.7%) | 2 (2.0) | - | - |
| Wang et al., 2018 [28] | Prospective | China | 201 | 2002 AECG | 88% | 158 (78.6%) | yes | 72 (45.5%) | 16 (10.1%) | yes | 42.9 ± 19.4 |
| Kampolis et al., 2018 [20] | Prospective | Greece | 384 | 2002 AECG | 94.5% | 7 (1.8%) | yes | - | - | yes | 81.74 ± 17.38 |
| Guisado-Vasco et al., 2019 [45] | Retrospective | Spain | 102 | 2016 ACR/EULAR | 93% | 36 (35.3%) | yes | 27 (26%) | 6 (5.9%) | yes | - |
| Sogkas et al., 2020 [46] | Retrospective | Germany | 31 | 2016 ACR/EULAR | 71% | 19 (61%) | yes | 9 (29%) | 13 (42%) | yes | - |
| Shi et al., 2020 [34] | Retrospective | China | 706 | 2002 AECG | 90.5% | 168 (23.8%) | - | - | - | - | - |
| Ufuk et al., 2020 [38] | Retrospective | Turkey | 28 | 2016 ACR/EULAR | 86% | 34 (75%) | yes | 21 (75%) | 6 (21.4%) | yes | |
| Gao et al., 2021 [35] | Retrospective | China | 934 | 2002 AECG | - | 178 (19%) | yes | 57 (44.9%) | 9 (15.0%) | yes | 72.4 ± 20.9 |
| Sahin Ozdemirel et al., 2021 [39] | Retrospective | Turkey | 35 | 2016 ACR/EULAR | 94% | 1 (3%) | yes | - | - | yes | 91.28 ± 19.70 |
| Lin et al., 2022 [36] | Retrospective | China | 333 | 2002 AECG | 93.1% | 66 (19.8%) | yes | 42 (63.6%) | 20 (30.3%) | yes | 58.82 ± 21.04 |
| Weng et al., 2022 [37] | Retrospective | China | 69 | 2016 ACR/EULAR | 90% | 35 (50%) | yes | - | - | yes | - |
| Işik et al., 2022 [40] | Retrospective | Turkey | 120 | 2016 ACR/EULAR | - | 16 (13.3%) | yes | 10 (62.5%) | 2 (12.5%) | yes | 60.1 ± 20.4 |
| Moderator | Coefficient | SE | Z Value | p Value | 95% CI |
|---|---|---|---|---|---|
| Male gender | 0.24 | 0.044 | 5.54 | <0.0001 | 0.16–0.33 |
| ANA positivity | 0.19 | 0.25 | 0.77 | 0.44 | −0.30–0.68 |
| Anti-Ro/SSa positivity | 0.59 | 0.35 | 1.69 | 0.091 | −0.096–1.28 |
| Anti-La/SSb positivity | 0.42 | 0.29 | 1.45 | 0.15 | −0.15–0.98 |
| DLCO value | 0.47 | 0.17 | 2.68 | 0.0074 | 0.12–0.81 |
| Country | 0.18 | 0.045 | 4.02 | <0.0001 | 0.092–0.27 |
| HRCT | 0.16 | 0.069 | 2.35 | 0.019 | 0.027–0.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berardicurti, O.; Marino, A.; Genovali, I.; Navarini, L.; D’Andrea, S.; Currado, D.; Rigon, A.; Arcarese, L.; Vadacca, M.; Giacomelli, R. Interstitial Lung Disease and Pulmonary Damage in Primary Sjögren’s Syndrome: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 2586. https://doi.org/10.3390/jcm12072586
Berardicurti O, Marino A, Genovali I, Navarini L, D’Andrea S, Currado D, Rigon A, Arcarese L, Vadacca M, Giacomelli R. Interstitial Lung Disease and Pulmonary Damage in Primary Sjögren’s Syndrome: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(7):2586. https://doi.org/10.3390/jcm12072586
Chicago/Turabian StyleBerardicurti, Onorina, Annalisa Marino, Irene Genovali, Luca Navarini, Settimio D’Andrea, Damiano Currado, Amelia Rigon, Luisa Arcarese, Marta Vadacca, and Roberto Giacomelli. 2023. "Interstitial Lung Disease and Pulmonary Damage in Primary Sjögren’s Syndrome: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 7: 2586. https://doi.org/10.3390/jcm12072586
APA StyleBerardicurti, O., Marino, A., Genovali, I., Navarini, L., D’Andrea, S., Currado, D., Rigon, A., Arcarese, L., Vadacca, M., & Giacomelli, R. (2023). Interstitial Lung Disease and Pulmonary Damage in Primary Sjögren’s Syndrome: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(7), 2586. https://doi.org/10.3390/jcm12072586





