Delta Neutrophil Index as a New Early Mortality Predictor after Liver Transplantation
Abstract
1. Introduction
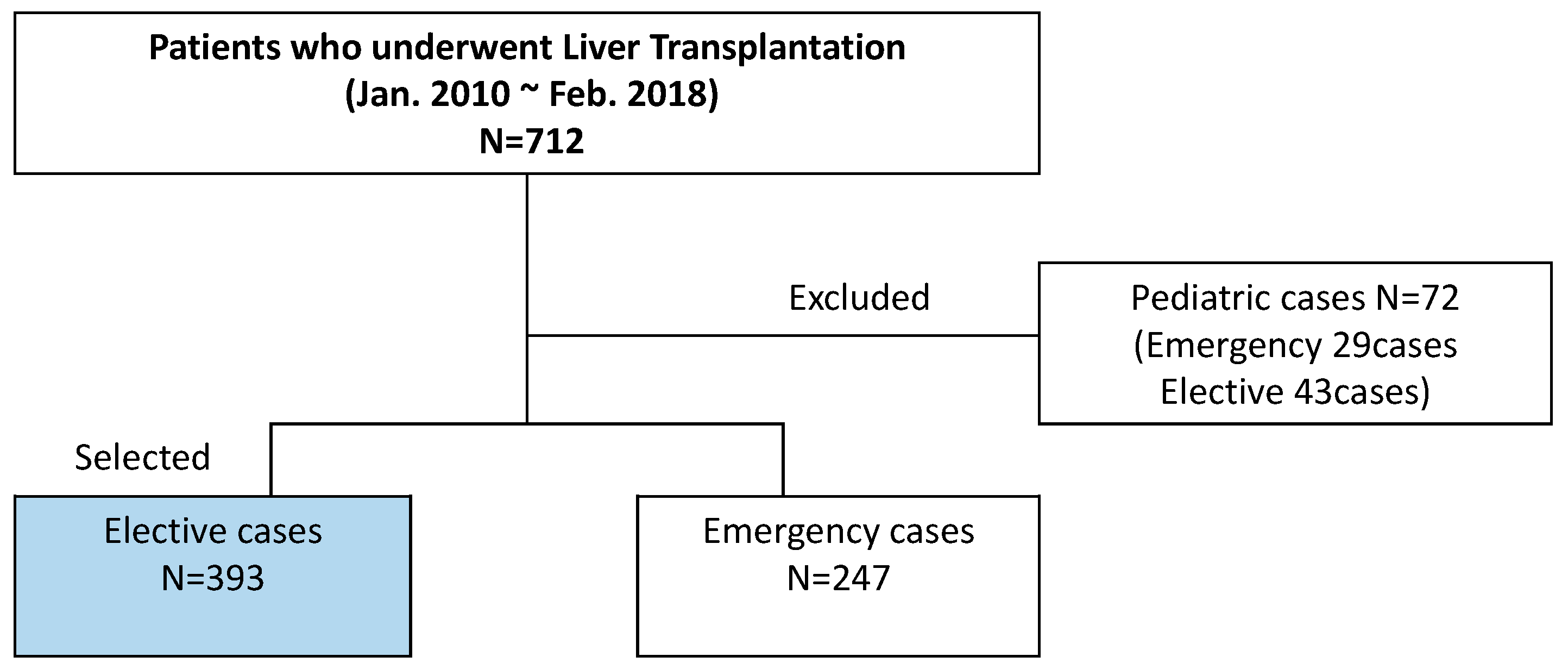
2. Materials and Methods
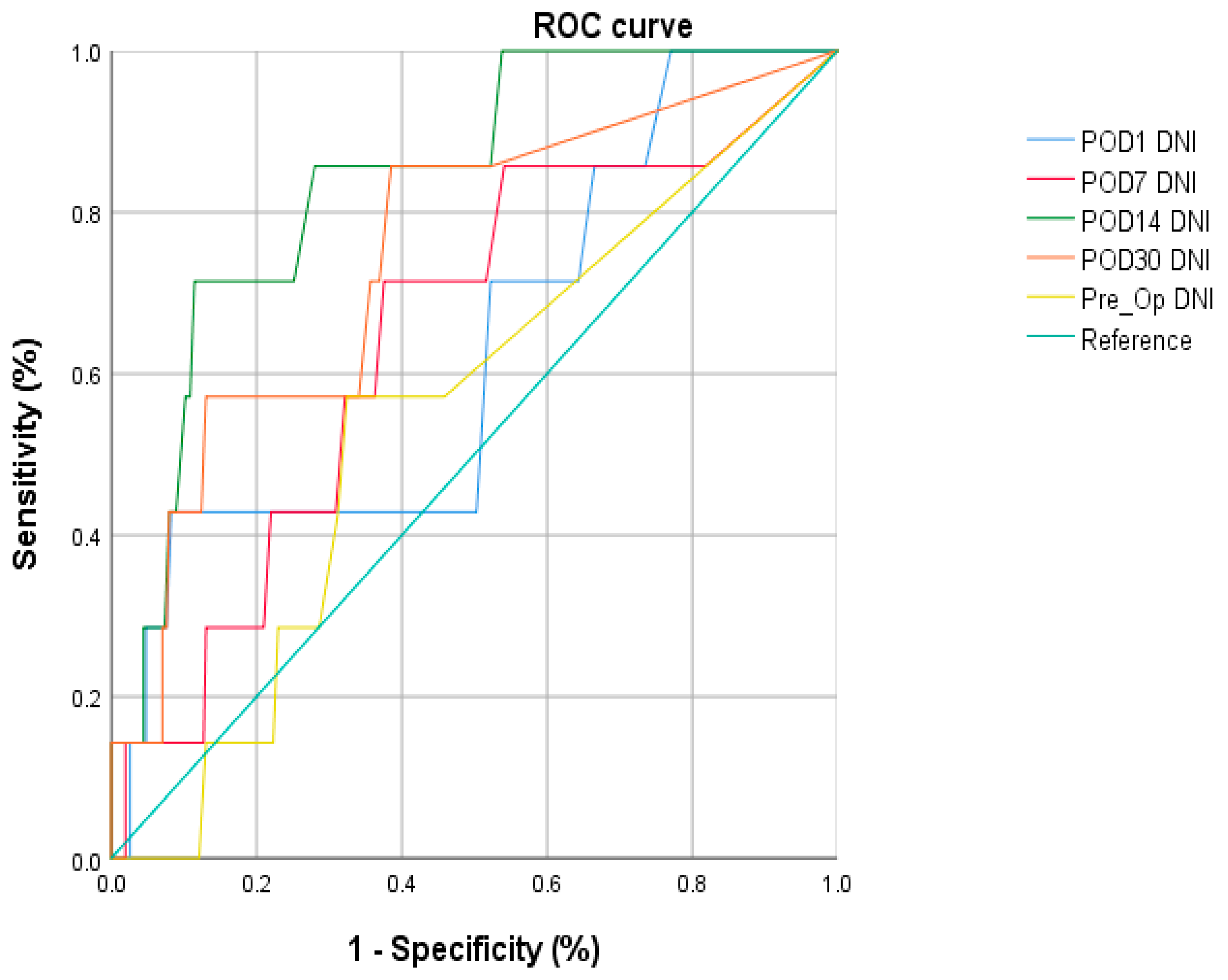
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Johnson, S.R.; Alexopoulos, S.; Curry, M.; Hanto, D.W. Primary nonfunction (PNF) in the MELD era: An SRTR database analysis. Am. J. Transplant. 2007, 7, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Goodrich, N.P.; Bragg-Gresham, J.L.; Dykstra, D.M.; Punch, J.D.; DebRoy, M.A.; Greenstein, S.M.; Merion, R.M. Characteristics associated with liver graft failure: The concept of a donor risk index. Am. J. Transplant. 2006, 6, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Halldorson, J.B.; Bakthavatsalam, R.; Fix, O.; Reyes, J.D.; Perkins, J.D. D-MELD, a simple predictor of post liver transplant mortality for optimization of donor/recipient matching. Am. J. Transplant. 2009, 9, 318–326. [Google Scholar] [CrossRef]
- Kiuchi, T.; Tanaka, K.; Ito, T.; Oike, F.; Ogura, Y.; Fujimoto, Y.; Ogawa, K. Small-for-size graft in living donor liver transplantation: How far should we go? Liver Transpl. 2003, 9, S29–S35. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, T.; Shirabe, K.; Yoshizumi, T.; Aishima, S.; Taketomi, Y.A.; Soejima, Y.; Uchiyama, H.; Kayashima, H.; Toshima, T.; Maehara, Y. Primary graft dysfunction after living donor liver transplantation is characterized by delayed functional hyperbilirubinemia. Am. J. Transplant. 2012, 12, 1886–1897. [Google Scholar] [CrossRef] [PubMed]
- Morioka, D.; Egawa, H.; Kasahara, M.; Ito, T.; Haga, H.; Takada, Y.; Shimada, H.; Tanaka, K. Outcomes of adult-to-adult living donor liver transplantation: A single institution’s experience with 335 consecutive cases. Ann. Surg. 2007, 245, 315–325. [Google Scholar] [CrossRef]
- Kaido, T.; Egawa, H.; Tsuji, H.; Ashihara, E.; Maekawa, T.; Uemoto, S. In-hospital mortality in adult recipients of living donor liver transplantation: Experience of 576 consecutive cases at a single center. Liver Transplant. 2009, 15, 1420–1425. [Google Scholar] [CrossRef]
- Wiesner, R.; Edwards, E.; Freeman, R.; Harper, A.; Kim, R.; Kamath, P.; Kremers, W.; Lake, J.; Howard, T.; Merion, R.M.; et al. Model for End-stage Liver Disease (MELD) and allocation of donor livers. Gastroenterology 2003, 124, 91–96. [Google Scholar] [CrossRef]
- De la Mata, M.; Meager, A.; Rolando, N.; Daniels, H.M.; Nouri-Aria, K.T.; Goka, A.K.; Eddleston, A.L.; Alexander, G.J.; Williams, R. Tumour necrosis factor production in fulminant hepatic failure: Relation to aetiology and superimposed microbial infection. Clin. Exp. Immunol. 1990, 82, 479–484. [Google Scholar] [CrossRef]
- Wigmore, S.J.; Walsh, T.S.; Lee, A.; Ross, J.A. Pro-inflammatory cytokine release and mediation of the acute phase protein response in fulminant hepatic failure. Intensive Care Med. 1998, 24, 224–229. [Google Scholar] [CrossRef]
- Clapperton, M.; Rolando, N.; Sandoval, L.; Davies, E.; Williams, R. Neutrophil superoxide and hydrogen peroxide production in patients with acute liver failure. Eur. J. Clin. Investig. 1997, 27, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Rolando, N.; Clapperton, M.; Wade, J.; Panetsos, G.; Mufti, G.; Williams, R. Granulocyte colony-stimulating factor improves function of neutrophils from patients with acute liver failure. Eur. J. Gastroenterol. Hepatol. 2000, 12, 1135–1140. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.J.; Nishtala, A.; Manakkat Vijay, G.K.; Abeles, R.D.; Auzinger, G.; Bernal, W.; Ma, Y.; Wendon, J.A.; Shawcross, D.L. Circulating neutrophil dysfunction in acute liver failure. Hepatology 2013, 57, 1142–1152. [Google Scholar] [CrossRef] [PubMed]
- Wyke, R.J.; Rajkovic, I.A.; Eddleston, A.L.; Williams, R. Defective opsonisation and complement deficiency in serum from patients with fulminant hepatic failure. Gut 1980, 21, 643–649. [Google Scholar] [CrossRef]
- Petrowsky, H.; Rana, A.; Kaldas, F.M.; Sharma, A.; Hong, J.C.; Agopian, V.G.; Durazo, F.; Honda, H.; Gornbein, J.; Wu, V.; et al. Liver transplantation in highest acuity recipients: Identifying factors to avoid futility. Ann. Surg. 2014, 259, 1186–1194. [Google Scholar] [CrossRef]
- Vaquero, J.; Polson, J.; Chung, C.; Helenowski, I.; Schiodt, F.V.; Reisch, J.; Lee, W.M.; Blei, A.T. Infection and the progression of hepatic encephalopathy in acute liver failure. Gastroenterology 2003, 125, 755–764. [Google Scholar] [CrossRef]
- Acute Respiratory Distress Syndrome Network; Brower, R.G.; Matthay, M.A.; Morris, A.; Schoenfeld, D.; Thompson, B.T.; Wheeler, A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar] [CrossRef]
- Rivers, E.; Nguyen, B.; Havstad, S.; Ressler, J.; Muzzin, A.; Knoblich, B.; Peterson, E.; Tomlanovich, M.; Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 2001, 345, 1368–1377. [Google Scholar] [CrossRef]
- Keegan, M.T.; Soares, M. What every intensivist should know about prognostic scoring systems and risk-adjusted mortality. Rev. Bras. Ter. Intensiv. 2016, 28, 264–269. [Google Scholar] [CrossRef]
- Kim, H.; Kong, T.; Chung, S.P.; Hong, J.H.; Lee, J.W.; Joo, Y.; Ko, D.R.; You, J.S.; Park, I. Usefulness of the Delta Neutrophil Index as a Promising Prognostic Marker of Acute Cholangitis in Emergency Departments. Shock 2017, 47, 303–312. [Google Scholar] [CrossRef]
- Ko, D.R.; Jang, J.E.; Chung, S.P.; Lee, J.W.; Lee, H.S.; Hong, J.H.; Kong, T.; You, J.S.; Park, I. Usefulness of the delta neutrophil index as an ancillary test in the emergency department for the early diagnosis of suspected acute promyelocytic leukemia. Leuk. Lymphoma 2017, 58, 2387–2394. [Google Scholar] [CrossRef] [PubMed]
- Nahm, C.H.; Choi, J.W.; Lee, J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann. Clin. Lab. Sci. 2008, 38, 241–246. [Google Scholar] [PubMed]
- Wacker, C.; Prkno, A.; Brunkhorst, F.M.; Schlattmann, P. Procalcitonin as a diagnostic marker for sepsis: A systematic review and meta-analysis. Lancet Infect. Dis. 2013, 13, 426–435. [Google Scholar] [CrossRef]
- Póvoa, P. C-reactive protein: A valuable marker of sepsis. Intensive Care Med. 2002, 28, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, J.J. Neutrophil CD64: A diagnostic marker for infection and sepsis. Clin. Chem. Lab. Med. 2009, 47, 903–916. [Google Scholar] [CrossRef] [PubMed]
- Ardron, M.J.; Westengard, J.C.; Dutcher, T.F. Band neutrophil counts are unnecessary for the diagnosis of infection in patients with normal total leukocyte counts. Am. J. Clin. Pathol. 1994, 102, 646–649. [Google Scholar] [CrossRef]
- Park, B.H.; Kang, Y.A.; Park, M.S.; Jung, W.J.; Lee, S.H.; Lee, S.K.; Kim, S.Y.; Kim, S.K.; Chang, J.; Jung, J.Y.; et al. Delta neutrophil index as an early marker of disease severity in critically ill patients with sepsis. BMC Infect. Dis. 2011, 11, 299. [Google Scholar] [CrossRef]
- Hwang, Y.J.; Chung, S.P.; Park, Y.S.; Chung, H.S.; Lee, H.S.; Park, J.W.; Lee, J.W.; Hong, J.H.; You, J.S.; Park, I. Newly designed delta neutrophil index-to-serum albumin ratio prognosis of early mortality in severe sepsis. Am. J. Emerg. Med. 2015, 33, 1577–1582. [Google Scholar] [CrossRef]
- Shiga, S.; Fujimoto, H.; Mori, Y.; Sakata, T.; Hamaguchi, Y.; Wang, F.S.; Inomata, Y.; Tohyama, K.; Ichiyama, S. Immature granulocyte count after liver transplantation. Clin. Chem. Lab. Med. 2002, 40, 775–780. [Google Scholar] [CrossRef]
- Shin, D.H.; Kim, E.J.; Kim, S.J.; Park, J.Y.; Oh, J. Delta neutrophil index as a marker for differential diagnosis between acute graft pyelonephritis and acute graft rejection. PLoS ONE 2015, 10, e0135819. [Google Scholar] [CrossRef]
- Lee, S.H.; Park, M.S.; Song, J.H.; Kim, Y.S.; Lee, J.G.; Paik, H.C.; Kim, S.Y. Perioperative factors associated with 1-year mortality after lung transplantation: A single-center experience in Korea. J. Thorac. Dis. 2017, 9, 4006–4016. [Google Scholar] [CrossRef]
- Cho, H.Y.; Jung, I.; Kim, S.J.; Park, Y.W.; Kim, Y.H.; Kwon, J.Y. Increased delta neutrophil index in women with severe preeclampsia. Am. J. Reprod. Immunol. 2017, 78, e12705. [Google Scholar] [CrossRef]
- Fishman, J.A. Infection in organ transplantation. Am. J. Transplant. 2017, 17, 856–879. [Google Scholar] [CrossRef] [PubMed]
- Van Hoek, B.; de Rooij, B.J.; Verspaget, H.W. Risk factors for infection after liver transplantation. Best Pract. Res. Clin. Gastroenterol. 2012, 26, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Sim, J.; Hong, S.Y.; Kim, B.W. Systemic Immune-Inflammatory Marker of High Meld Patients Is Associated with Early Mortality After Liver Transplantation. Transplant. Proc. 2021, 53, 2945–2952. [Google Scholar] [CrossRef]
- Korean Network for Organ Sharing (KONOS). 2021 KONOS Annual Data Report. KONOS. Available online: https://www.konos.go.kr/konosis/common/bizlogic.jsp (accessed on 8 February 2023).
- Fishman, J.A. Infection in solid organ transplant recipients. N. Engl. J. Med. 2007, 357, 2601–2614. [Google Scholar] [CrossRef] [PubMed]
| 30 Days Mortality (−) | 30 Days Mortality (+) | p-Value | ||||
|---|---|---|---|---|---|---|
| Age | 54.1 ± 8.4 | 17~72 | 51.0 ± 9.6 | 33~64 | 0.239 | |
| Sex | Male | 289 | 76.05% | 8 | 61.5% | 0.8 |
| Female | 91 | 23.95% | 5 | 38.5% | ||
| MELD | 13.5 ± 7.5 | 5~42 | 20.7 ± 11.1 | 9~43 | 0.002 | |
| OP time | 11.8 ± 2.1 | 7.2~23 | 13.1 ± 3.0 | 8~19.3 | 0.05 | |
| Transfusion | 5.83 ± 9.16 | 0~97 | 29.4 ± 25.3 | 2~72 | <0.0001 | |
| ICU duration | 4.58 ± 2.73 | 0~24 | 8.33 ± 4.5 | 1~16 | <0.0001 | |
| Renal replacement | Yes | 2 | 0.6% | 1 | 8.3% | 0.001 |
| No | 378 | 99.4% | 12 | 91.8% | ||
| Pre OP CRP | 11.1 ± 22.7 | 0~216 | 21.14 ± 21.6 | 0.8~55.4 | 0.19 | |
| Pre OP DNI | 1.0 ± 2.51 | 0~36.9 | 2.1 ± 2.3 | 0~7.4 | 0.18 | |
| POD 7 CRP | 18.3 ± 28.3 | 0.95~168.8 | 41.6 ± 57.2 | 1.6~181.7 | 0.024 | |
| POD 7 DNI | 2.1 ± 2.6 | 0~32.4 | 3.9 ± 2.9 | 0~8.2 | 0.021 | |
| POD 14 CRP | 15.5 ± 22.7 | 0~130.5 | 88.9 ± 80.2 | 7.5~212 | <0.0001 | |
| POD 14 DNI | 1.1 ± 1.5 | 0~12.5 | 8.2 ± 13.7 | 0.5~47.3 | <0.0001 | |
| DNI ≥ 2.05 on POD 14 | DNI < 2.05 on POD 14 | p-Value | ||||
|---|---|---|---|---|---|---|
| Age | 53.3 ± 9.5 | 17~71 | 54.2 ± 8.1 | 17~72 | 0.42 | |
| Sex | Male | 44 | 60.2% | 253 | 79.5% | <0.0001 |
| Female | 29 | 39.8% | 65 | 20.5% | ||
| MELD | 16.4 ± 9.1 | 6~43 | 13.1 ± 7.2 | 5~42 | 0.001 | |
| OP time | 12.4 ± 2.0 | 9~19.3 | 11.7 ± 2.2 | 7.2~23 | 0.017 | |
| Transfusion | 10.7 ± 14.4 | 0~72 | 5.5 ± 9.2 | 0~97 | <0.0001 | |
| ICU duration | 5.9 ± 3.4 | 2~17 | 4.4 ± 2.6 | 0~24 | <0.0001 | |
| Renal replacement | Yes | 2 | 2.7% | 1 | 0.3% | 0.033 |
| No | 71 | 37.3% | 317 | 99.7% | ||
| Pre OP CRP | 12.3 ± 20.9 | 0.2~142.6 | 11.2 ± 23.2 | 0.2~216.2 | 0.74 | |
| POD 7 CRP | 30.7 ± 43.2 | 2.4~181.7 | 16.3 ± 25.2 | 0.95~168.8 | 0.006 | |
| POD 14 CRP | 34.6 ± 45.7 | 0.7~212.03 | 13.3 ± 21.3 | 0.4~130.45 | <0.0001 | |
| 30 days mortality | 9/73 | 12.3% | 2/318 | 0.6% | 0.008 | |
| Variable | Univariate | Multivariate | |
|---|---|---|---|
| p-Value | p-Value | OR (95% CI) | |
| Age | 0.83 | ||
| Sex | 0.95 | ||
| Transfusion | 0.99 | ||
| CRRT history | 0.48 | ||
| MELD | 0.26 | 0.064 | 1.06 (0.99~1.15) |
| OP time | 0.36 | ||
| DNI ≥ 2.05 on POD 14 | 0.99 | 0.001 | 31.55 (3.83~260.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Son, S.; Kim, H.; Ju, M. Delta Neutrophil Index as a New Early Mortality Predictor after Liver Transplantation. J. Clin. Med. 2023, 12, 2501. https://doi.org/10.3390/jcm12072501
Lee J, Son S, Kim H, Ju M. Delta Neutrophil Index as a New Early Mortality Predictor after Liver Transplantation. Journal of Clinical Medicine. 2023; 12(7):2501. https://doi.org/10.3390/jcm12072501
Chicago/Turabian StyleLee, Jeongjun, Sunyoung Son, Heeyoung Kim, and Manki Ju. 2023. "Delta Neutrophil Index as a New Early Mortality Predictor after Liver Transplantation" Journal of Clinical Medicine 12, no. 7: 2501. https://doi.org/10.3390/jcm12072501
APA StyleLee, J., Son, S., Kim, H., & Ju, M. (2023). Delta Neutrophil Index as a New Early Mortality Predictor after Liver Transplantation. Journal of Clinical Medicine, 12(7), 2501. https://doi.org/10.3390/jcm12072501






