Repeated Measurements Are Necessary for Evaluating Accurate Diurnal Rhythm Using a Self-Intraocular Pressure Measurement Device
Abstract
1. Introduction
2. Patients and Methods
2.1. IOP Measurement
2.2. Classification of Diurnal IOP Rhythm
2.3. Main Outcome Measures
2.4. Statistical Analysis
3. Results
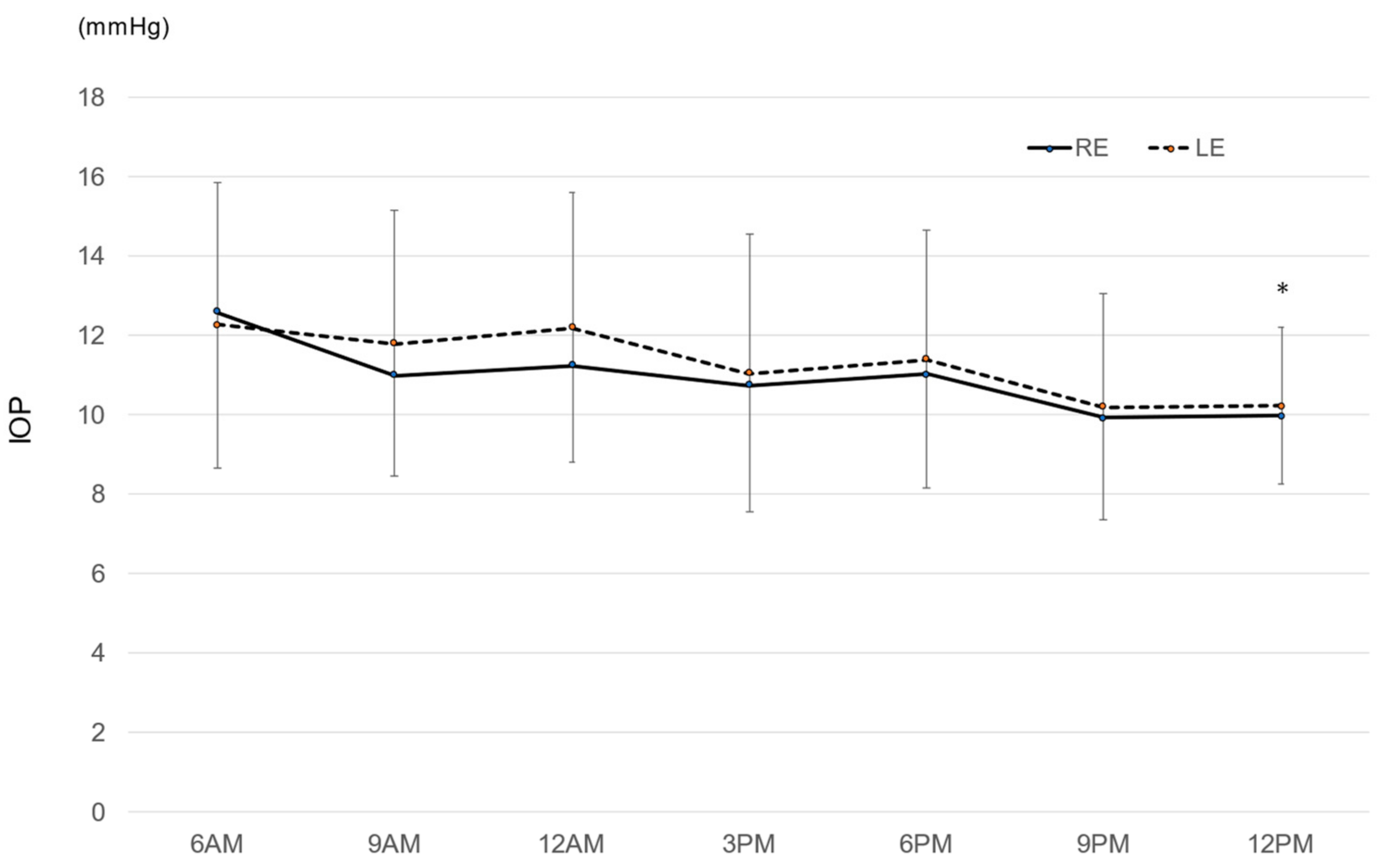
3.1. Diurnal IOP during the Investigated Period
3.2. Magnitude of Diurnal IOP Change
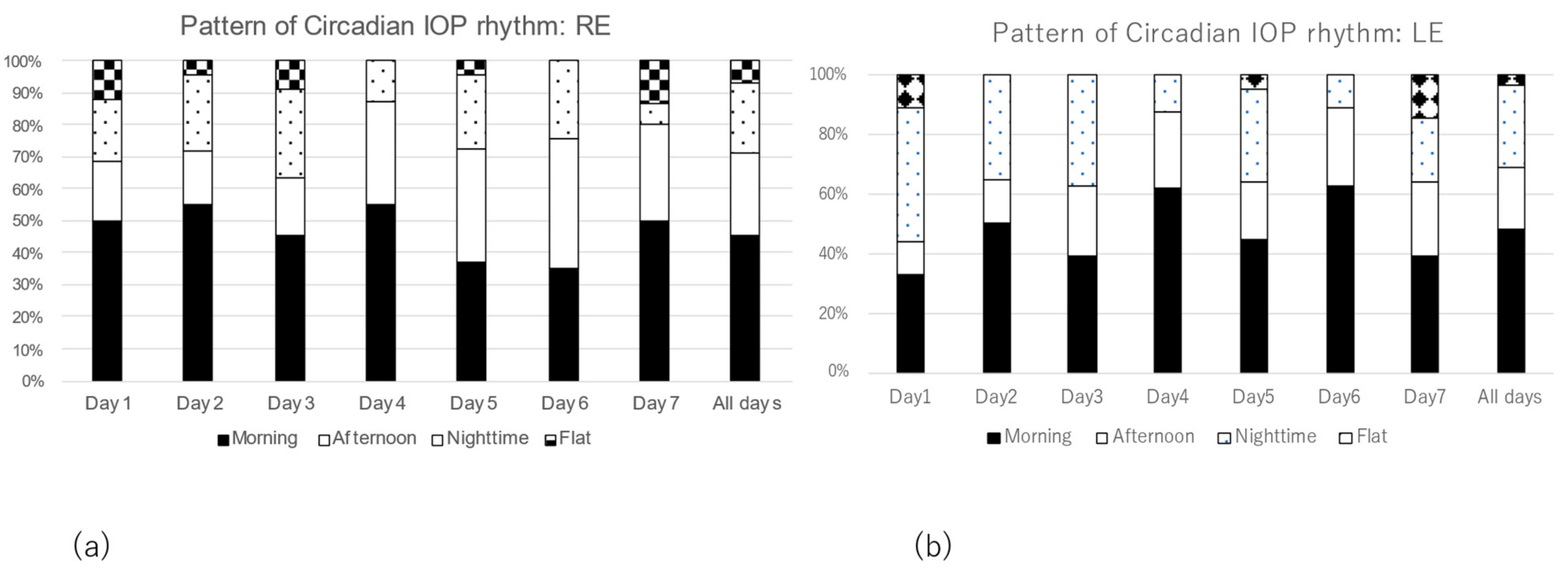
3.3. Comparison of Patterns of Diurnal IOP Rhythm
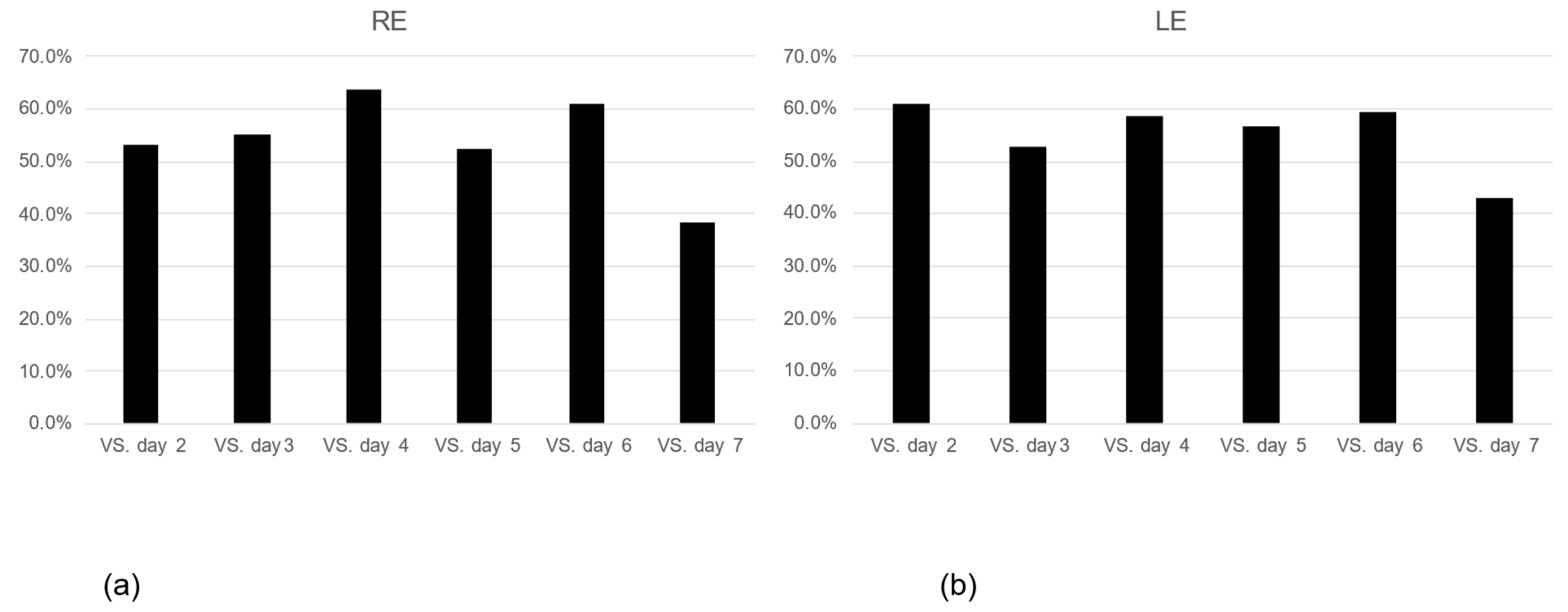
3.4. The Consistency of Diurnal IOP Rhythm and Its Associated Factors
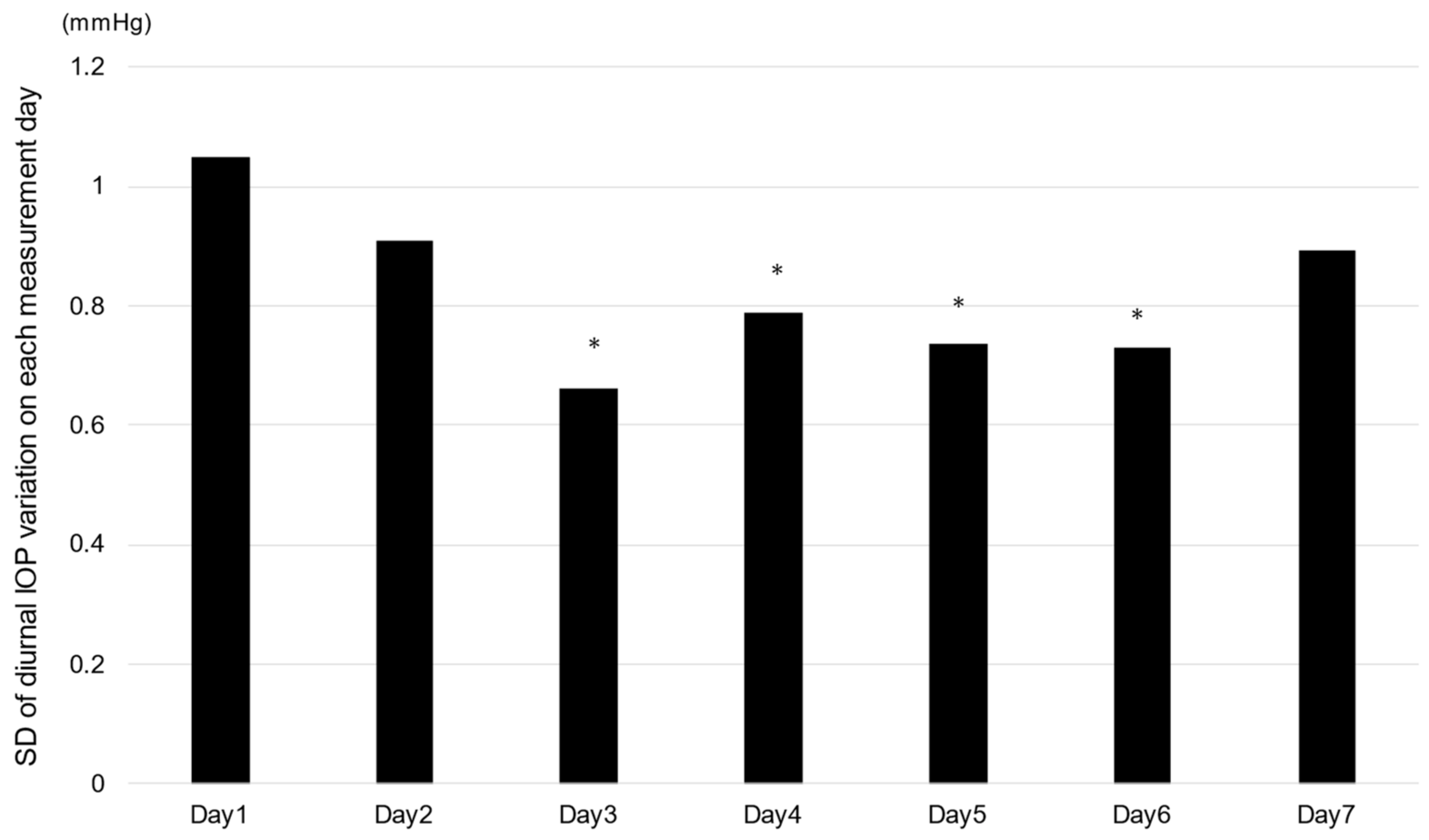
3.5. Magnitude of Fluctuation of Diurnal IOP Changes on Each Measurement Day
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aptel, F.; Weinreb, R.N.; Chiquet, C.; Mansouri, K. 24-h monitoring devices and nyctohemeral rhythms of intraocular pressure. Prog. Retin. Eye Res. 2016, 55, 108–148. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Budde, W.; Stroux, A.; Oberacher-Velten, I.M.; Jünemann, A. Single intraocular pressure measurements and diurnal intraocular pressure profiles. Am. J. Ophthalmol. 2005, 139, 1136–1137. [Google Scholar] [CrossRef] [PubMed]
- Barkana, Y.; Anis, S.; Liebmann, J.; Tello, C.; Ritch, R. Clinical utility of intraocular pressure monitoring outside of normal office hours in patients with glaucoma. Arch. Ophthalmol. 2006, 124, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.K.; Lee, C.K.; Kim, J.; Hong, S.; Kim, C.Y.; Seong, G.J. Instability of 24-hour intraocular pressure fluctuation in healthy young subjects: A prospective, cross-sectional study. BMC Ophthalmol. 2014, 14, 127. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.; Quérat, L.; Åkerstedt, C. Self-tonometry as a complement in the investigation of glaucoma patients. Acta Ophthalmol. 2016, 94, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Quérat, L.; Chen, E. Monitoring daily intraocular pressure fluctuations with self-tonometry in healthy subjects. Acta Ophthalmol. 2017, 95, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Realini, T.; Weinreb, R.N.; Wisniewski, S. Short-term repeatability of diurnal intraocular pressure patterns in glaucomatous individuals. Ophthalmology 2011, 118, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, M.; Kanamori, A.; Fujihara, M.; Yamada, Y.; Nakamura, M.; Negi, A. Assessment of IcareONE rebound tonometer for self-measuring intraocular pressure. Acta Ophthalmol. 2014, 92, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Mudie, L.; LaBarre, S.; Varadaraj, V.; Karakus, S.; Onnela, J.; Munoz, B.; Friedman, D.S. The Icare HOME (TA022) Study: Performance of an Intraocular Pressure Measuring Device for Self-Tonometry by Glaucoma Patients. Ophthalmology 2016, 123, 1675–1684. [Google Scholar] [CrossRef] [PubMed]
- Nakakura, S. Icare® rebound tonometers: Review of their characteristics and ease of use. Clin. Ophthalmol. 2018, 12, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; De Francesco, T.; Schlenker, M.; Ahmed, I.I. Icare Home Tonometer: A Review of Characteristics and Clinical Utility. Clin. Ophthalmol. 2020, 14, 4031–4045. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Katalinic, P.; Kalloniatis, M.; Hennessy, M.P.; Zangerl, B. Diurnal Intraocular Pressure Fluctuations with Self-tonometry in Glaucoma Patients and Suspects: A Clinical Trial. Optom. Vis.Sci. Off. Publ. Am. Acad. Optom. 2018, 95, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Schweier, C.; Hanson, J.V.; Funk, J.; Töteberg-Harms, M. Repeatability of intraocular pressure measurements with Icare PRO rebound, Tono-Pen AVIA, and Goldmann tonometers in sitting and reclining positions. BMC Ophthalmol. 2013, 13, 44. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, A.; Nakakura, S.; Fujio, Y.; Fukuma, Y.; Mori, E.; Tabuchi, H.; Kiuchi, Y. A Pilot Evaluation Assessing the Ease of Use and Accuracy of the New Self/Home-Tonometer IcareHOME in Healthy Young Subjects. J. Glaucoma 2016, 25, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Termühlen, J.; Mihailovic, N.; Alnawaiseh, M.; Dietlein, T.S.; Rosentreter, A. Accuracy of Measurements With the iCare HOME Rebound Tonometer. J. Glaucoma 2016, 25, 533–538. [Google Scholar] [CrossRef]
- Dabasia, P.L.; Lawrenson, J.G.; Murdoch, I.E. Evaluation of a new rebound tonometer for self-measurement of intraocular pressure. Br. J. Ophthalmol. 2016, 100, 1139–1143. [Google Scholar] [CrossRef] [PubMed]
- Chun, Y.S.; Park, I.K.; Shin, K.U.; Kim, J.M. Long-term Reliability of Diurnal Intraocular Pressure Patterns in Healthy Asians. Korean J. Ophthalmol. 2017, 31, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Muttuvelu, D.V.; Baggesen, K.; Ehlers, N. Precision and accuracy of the ICare tonometer-Peripheral and central IOP measurements by rebound tonometry. Acta Ophthalmol. 2010, 90, 322–326. [Google Scholar] [CrossRef] [PubMed]
- Miki, A.; Ieki, Y.; Kiryu, J.; Yaoeda, K.; Shirakashi, M. Central and peripheral intraocular pressure measured by a rebound tonometer. Clin. Ophthalmol. 2011, 5, 1113–1118. [Google Scholar] [CrossRef] [PubMed]

| RE | LE | |
|---|---|---|
| logMAR | 0.072 | 0.11 |
| (range: −0.176~1.301) | (range: −0.176~1.222) | |
| HFA-MD (24-2·30-2) (dB) | −11.2 | −10.8 |
| HFA-MD (10-2) (dB) | −12.4 | −12.3 |
| # of anti-glaucoma eyedrops | 2.5 | 2.4 |
| Mean ambulatory IOP (GAT) (mmHg) | 12.4 | 12.4 |
| (range: 9.3~17.5) | (range: 8.0~17.3) | |
| CCT (um) | 511 ± 186.4 | 515.3 ± 188.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shigemoto, Y.; Hasebe, Y.; Kitamura, K.; Fukuda, Y.; Sakamoto, M.; Matsubara, M.; Minaguchi, S.; Kashiwagi, K. Repeated Measurements Are Necessary for Evaluating Accurate Diurnal Rhythm Using a Self-Intraocular Pressure Measurement Device. J. Clin. Med. 2023, 12, 2460. https://doi.org/10.3390/jcm12072460
Shigemoto Y, Hasebe Y, Kitamura K, Fukuda Y, Sakamoto M, Matsubara M, Minaguchi S, Kashiwagi K. Repeated Measurements Are Necessary for Evaluating Accurate Diurnal Rhythm Using a Self-Intraocular Pressure Measurement Device. Journal of Clinical Medicine. 2023; 12(7):2460. https://doi.org/10.3390/jcm12072460
Chicago/Turabian StyleShigemoto, Yumi, Yuka Hasebe, Kazuyoshi Kitamura, Yoshiko Fukuda, Masako Sakamoto, Mio Matsubara, Shinya Minaguchi, and Kenji Kashiwagi. 2023. "Repeated Measurements Are Necessary for Evaluating Accurate Diurnal Rhythm Using a Self-Intraocular Pressure Measurement Device" Journal of Clinical Medicine 12, no. 7: 2460. https://doi.org/10.3390/jcm12072460
APA StyleShigemoto, Y., Hasebe, Y., Kitamura, K., Fukuda, Y., Sakamoto, M., Matsubara, M., Minaguchi, S., & Kashiwagi, K. (2023). Repeated Measurements Are Necessary for Evaluating Accurate Diurnal Rhythm Using a Self-Intraocular Pressure Measurement Device. Journal of Clinical Medicine, 12(7), 2460. https://doi.org/10.3390/jcm12072460







