Sacrospinous Hysteropexy Versus Prolapse Hysterectomy with Apical Fixation: A Retrospective Comparison over an 18 Year Period
Abstract
1. Introduction
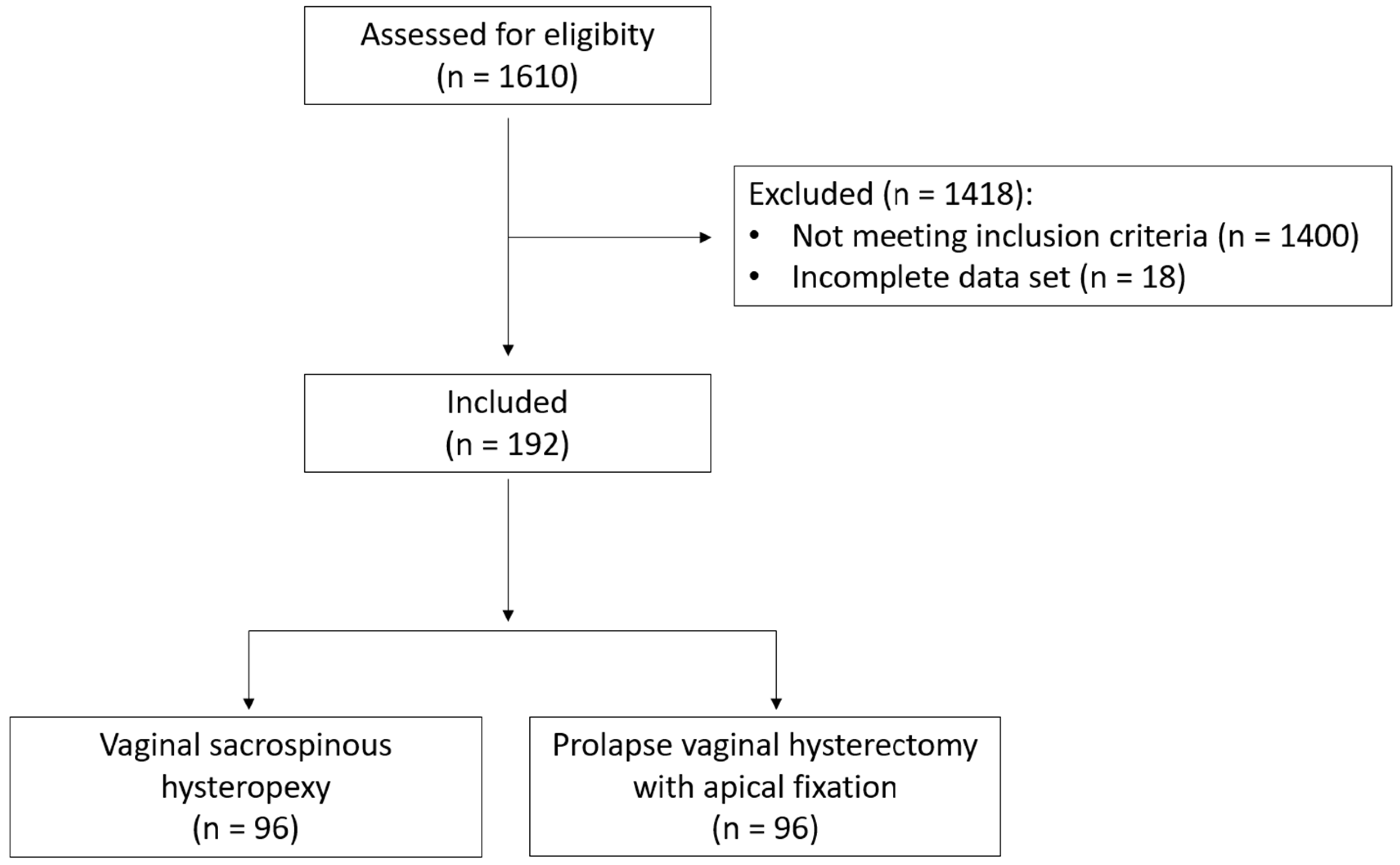
2. Materials and Methods
2.1. Description of the Surgical Procedure
2.1.1. Sacrospinous Hysteropexy
2.1.2. Vaginal Hysterectomy
2.2. Primary Outcome Parameters
- Operating time, defined as starting and ending with the patients’ anesthesia in the operating theatre;
- Intraoperative blood loss, as documented by the surgeons immediately post intervention;
- Intraoperative complications, defined as any deviance from standardized procedure documented by the surgeon;
- Intraoperative conversion to other surgical management options;
- Postoperative complications as classified by the Clavien–Dindo classification [22]
2.3. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Primary Outcomes
3.3. Intraoperative and Postoperative Complications
3.4. Logistic Regression
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, J.M.; Vaughan, C.P.; Goode, P.S.; Redden, D.T.; Burgio, K.L.; Richter, H.E.; Markland, A.D. Prevalence and Trends of Symptomatic Pelvic Floor Disorders in U.S. Women. Obstet. Gynecol. 2014, 123, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Mao, M.; Ai, F.; Zhang, Y.; Kang, J.; Liang, S.; Xu, T.; Zhu, L. Changes in the Symptoms and Quality of Life of Women with Symptomatic Pelvic Organ Prolapse Fitted with a Ring with Support Pessary. Maturitas 2018, 117, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, M.; Hayward, L. Pelvic Floor Dysfunction and Its Effect on Quality of Sexual Life. Sex. Med. Rev. 2019, 7, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Baessler, K.; Christmann-Schmid, C.; Maher, C.; Haya, N.; Crawford, T.; Brown, J. Surgery for Women with Pelvic Organ Prolapse with or without Stress Urinary Incontinence. Cochrane Database Syst. Rev. 2018, 2018, CD013108. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Feiner, B.; Baessler, K.; Christmann-Schmid, C.; Haya, N.; Brown, J. Surgery for Women with Apical Vaginal Prolapse. Cochrane Database Syst. Rev. 2016, 2016, CD012376. [Google Scholar] [CrossRef]
- Smith, F.; Holman, C.; Moorin, R.; Tsokos, N. Lifetime Risk of Undergoing Surgery for Pelvic Organ Prolapse. Obstet. Gynecol. 2010, 116, 1096–1100. [Google Scholar] [CrossRef]
- Løwenstein, E.; Ottesen, B.; Gimbel, H. Incidence and Lifetime Risk of Pelvic Organ Prolapse Surgery in Denmark from 1977 to 2009. Int. Urogynecol. J. 2015, 26, 49–55. [Google Scholar] [CrossRef]
- Kurkijärvi, K.; Aaltonen, R.; Gissler, M.; Mäkinen, J. Pelvic Organ Prolapse Surgery in Finland from 1987 to 2009: A National Register Based Study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 214, 71–77. [Google Scholar] [CrossRef]
- Altman, D.; Falconer, C.; Cnattingius, S.; Granath, F. Pelvic Organ Prolapse Surgery Following Hysterectomy on Benign Indications. Am. J. Obstet. Gynecol. 2008, 198, 572.e1–572.e6. [Google Scholar] [CrossRef]
- Blandon, R.E.; Bharucha, A.E.; Melton, L.J.; Schleck, C.D.; Babalola, E.O.; Zinsmeister, A.R.; Gebhart, J.B. Incidence of Pelvic Floor Repair after Hysterectomy: A Population-Based Cohort Study. Am. J. Obstet. Gynecol. 2007, 197, 664.e1–664.e7. [Google Scholar] [CrossRef]
- Forsgren, C.; Lundholm, C.; Johansson, A.L.V.; Cnattingius, S.; Zetterström, J.; Altman, D. Vaginal Hysterectomy and Risk of Pelvic Organ Prolapse and Stress Urinary Incontinence Surgery. Int. Urogynecol. J. 2012, 23, 43–48. [Google Scholar] [CrossRef]
- Husby, K.R.; Gradel, K.O.; Klarskov, N. Pelvic Organ Prolapse Following Hysterectomy on Benign Indication: A Nationwide, Nulliparous Cohort Study. Am. J. Obstet. Gynecol. 2022, 226, 386.e1–386.e9. [Google Scholar] [CrossRef]
- Chene, G.; Tardieu, A.-S.; Savary, D.; Krief, M.; Boda, C.; Anton-Bousquet, M.-C.; Mansoor, A. Anatomical and Functional Results of McCall Culdoplasty in the Prevention of Enteroceles and Vaginal Vault Prolapse after Vaginal Hysterectomy. Int. Urogynecol. J. 2008, 19, 1007–1011. [Google Scholar] [CrossRef]
- De Castro, E.B.; Brito, L.G.O.; Juliato, C.R.T. Vaginal Hysterectomy with Bilateral Sacrospinous Fixation plus an Anterior Mesh versus Abdominal Sacrocervicopexy for the Treatment of Primary Apical Prolapse in Postmenopausal Women: A Randomized Controlled Study. Int. Urogynecol. J. 2019, 31, 365–372. [Google Scholar] [CrossRef]
- Detollenaere, R.J.; den Boon, J.; Stekelenburg, J.; IntHout, J.; Vierhout, M.E.; Kluivers, K.B.; van Eijndhoven, H.W.F. Sacrospinous Hysteropexy versus Vaginal Hysterectomy with Suspension of the Uterosacral Ligaments in Women with Uterine Prolapse Stage 2 or Higher: Multicentre Randomised Non-Inferiority Trial. BMJ 2015, 351, h3717. [Google Scholar] [CrossRef]
- Schulten, S.F.M.; Detollenaere, R.J.; Stekelenburg, J.; IntHout, J.; Kluivers, K.B.; van Eijndhoven, H.W.F. Sacrospinous Hysteropexy versus Vaginal Hysterectomy with Uterosacral Ligament Suspension in Women with Uterine Prolapse Stage 2 or Higher: Observational Follow-up of a Multicentre Randomised Trial. BMJ 2019, 366, l5149. [Google Scholar] [CrossRef]
- Meriwether, K.V.; Antosh, D.D.; Olivera, C.K.; Kim-Fine, S.; Balk, E.M.; Murphy, M.; Grimes, C.L.; Sleemi, A.; Singh, R.; Dieter, A.A.; et al. Uterine Preservation vs Hysterectomy in Pelvic Organ Prolapse Surgery: A Systematic Review with Meta-Analysis and Clinical Practice Guidelines. Am. J. Obstet. Gynecol. 2018, 219, 129–146.e2. [Google Scholar] [CrossRef]
- Oversand, S.H.; Staff, A.C.; Borstad, E.; Svenningsen, R. The Manchester Procedure: Anatomical, Subjective and Sexual Outcomes. Int. Urogynecol. J. 2018, 29, 1193–1201. [Google Scholar] [CrossRef]
- Kapoor, S.; Sivanesan, K.; Robertson, J.A.; Veerasingham, M.; Kapoor, V. Sacrospinous Hysteropexy: Review and Meta-Analysis of Outcomes. Int. Urogynecol. J. 2017, 28, 1285–1294. [Google Scholar] [CrossRef]
- Bump, R.C. Discussion: Epidemiology of Urinary Incontinence. Urology 1997, 50, 15–17. [Google Scholar] [CrossRef]
- Schüssler, B.; Laycock, J.; Norton, P.A.; Stanton, S.L. Pelvic Floor Re-Education: Principles and Practice; Springer-Verlag: London, UK, 1994. [Google Scholar]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo Classification of Surgical Complications: Five-Year Experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Erguler, K. Barnard: Barnard’s Unconditional Test; R Project for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
- Gohel, D.; Panagiotis, S. Flextable: Functions for Tabular Reporting; R Project for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Wickham, H.; Chang, W.; Henry, L.; Pedersen, T.L.; Takahashi, K.; Wilke, C.; Woo, K.; Yutani, H.; Dunnington, D. Ggplot2: Create Elegant Data Visualisations Using the Grammar of Graphics; R Project for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Dietz, V.; van der Vaart, C.H.; van der Graaf, Y.; Heintz, P.; Schraffordt Koops, S.E. One-Year Follow-up after Sacrospinous Hysteropexy and Vaginal Hysterectomy for Uterine Descent: A Randomized Study. Int. Urogynecol. J. 2010, 21, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Vergeldt, T.F.M.; Weemhoff, M.; IntHout, J.; Kluivers, K.B. Risk Factors for Pelvic Organ Prolapse and Its Recurrence: A Systematic Review. Int. Urogynecol. J. 2015, 26, 1559–1573. [Google Scholar] [CrossRef] [PubMed]

| Variable | All | HE | SSH | p Value | Remark | Test |
|---|---|---|---|---|---|---|
| count | 192 | 96 | 96 | |||
| age | 58.91 (50.83–66.76) | 58.81 (50.83–66.80) | 58.91 (50.83–66.76) | 0.8334 | NAs: 0 in group HE, 0 in group SSH | Wilcoxon rank sum test with continuity correction |
| BMI | 26.22 (23.33–29.86) | 26.95 (24.4–29.71) | 25.65 (22.97–30.03) | 0.1335 | NAs: 8 in group HE, 29 in group SSH | Wilcoxon rank sum test with continuity correction |
| preoperative POP-Q stage | 3 (2–3) | 3 (2–3) | 3 (2–3) | 0.6102 | NAs: 0 in group HE, 0 in group SSH | Wilcoxon rank sum test with continuity correction |
| preoperative Oxford scale | 0 (0–2) | 0 (0–0) | 0 (0–3) | 0.0002 | NAs: 0 in group HE, 0 in group SSH | Wilcoxon rank sum test with continuity correction |
| preoperative cardiovascular issues | 0.2554 | Barnard’s Unconditiol Test | ||||
| no | 145 | 76 | 69 | |||
| yes | 47 | 20 | 27 | |||
| preoperative diabetes | 0.5289 | Barnard’s Unconditiol Test | ||||
| no | 179 | 91 | 88 | |||
| yes | 13 | 5 | 8 | |||
| preoperative renal insufficiency | 1 | Barnard’s Unconditiol Test | ||||
| no | 191 | 96 | 95 | |||
| yes | 1 | 0 | 1 | |||
| preoperative poly-medication | 0.5305 | Barnard’s Unconditiol Test | ||||
| no | 140 | 74 | 66 | |||
| yes | 31 | 14 | 17 | |||
| preoperative menopausal stage | 0.4414 | Pearson’s Chi-squared test with Yates’ continuity correction | ||||
| premenopausal | 28 | 13 | 15 | |||
| perimenopausal | 20 | 7 | 13 | |||
| postmenopausal | 105 | 53 | 52 | |||
| preoperative nicotine consumtion | 0.9846 | Barnard’s Unconditiol Test | ||||
| no | 100 | 44 | 56 | |||
| yes | 18 | 8 | 10 | |||
| preoperative parity | 0.624 | Pearson’s Chi-squared test with Yates’ continuity correction | ||||
| 0 | 12 | 4 | 8 | |||
| 1 | 35 | 17 | 18 | |||
| 2 | 85 | 41 | 44 | |||
| 3 | 38 | 21 | 17 | |||
| 4+ | 22 | 13 | 9 |
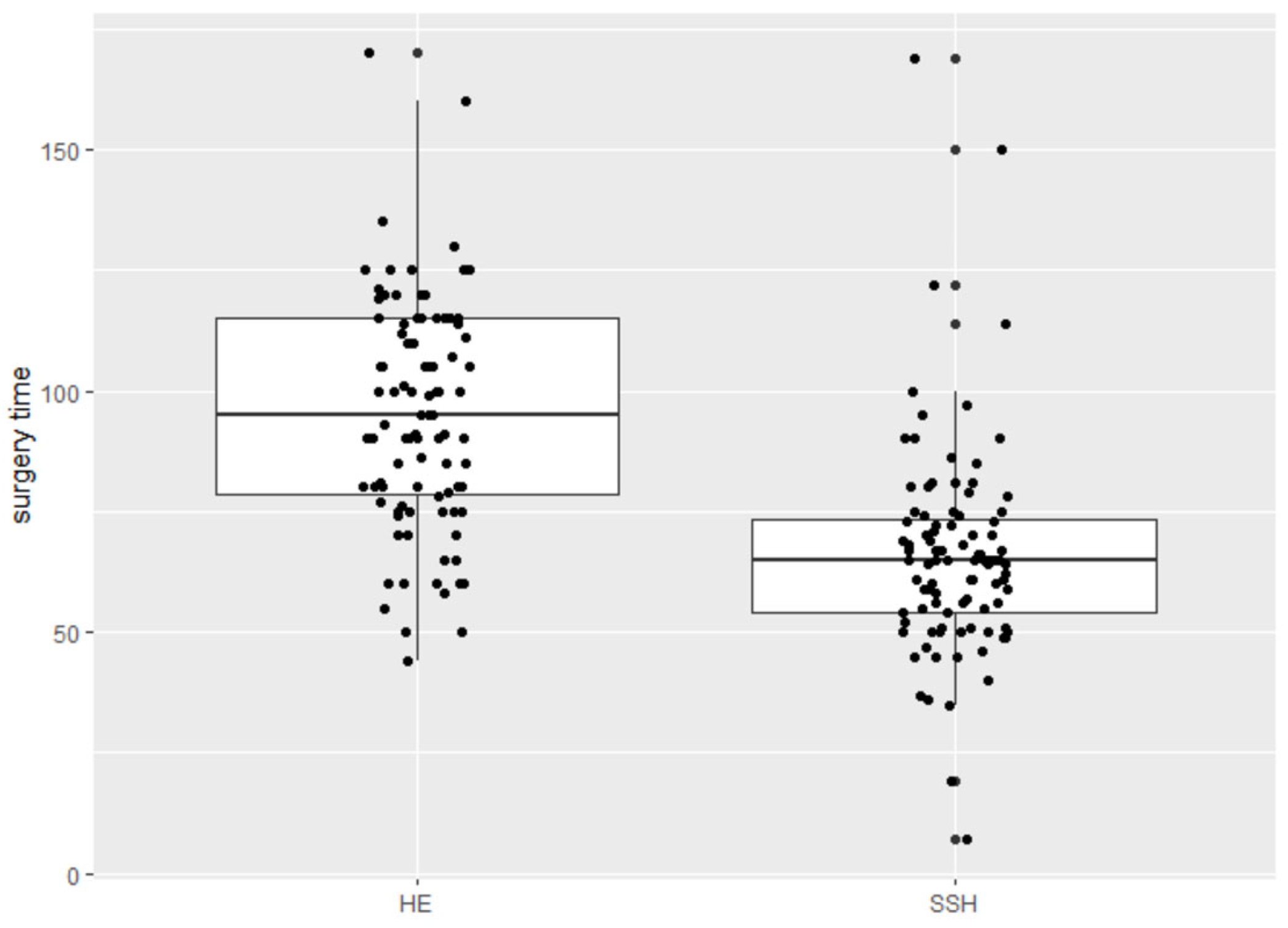
| Variable | All | HE | SSH | p Value | Remark | Test |
|---|---|---|---|---|---|---|
| surgery time (min) | 75 (61–100) | 95 (78.75–115) | 65 (54–73.25) | 0.0000 | NAs: 0 in group HE, 0 in group SSH | Wilcoxon rank sum test with continuity correction |
| postoperative hospitalisation (days) | 0.0000 | Pearson’s Chi-squared test with Yates’ continuity correction | ||||
| 1 | 1 | 0 | 1 | |||
| 2–4 | 97 | 30 | 67 | |||
| 5–7 | 32 | 28 | 4 | |||
| 8+ | 6 | 6 | 0 | |||
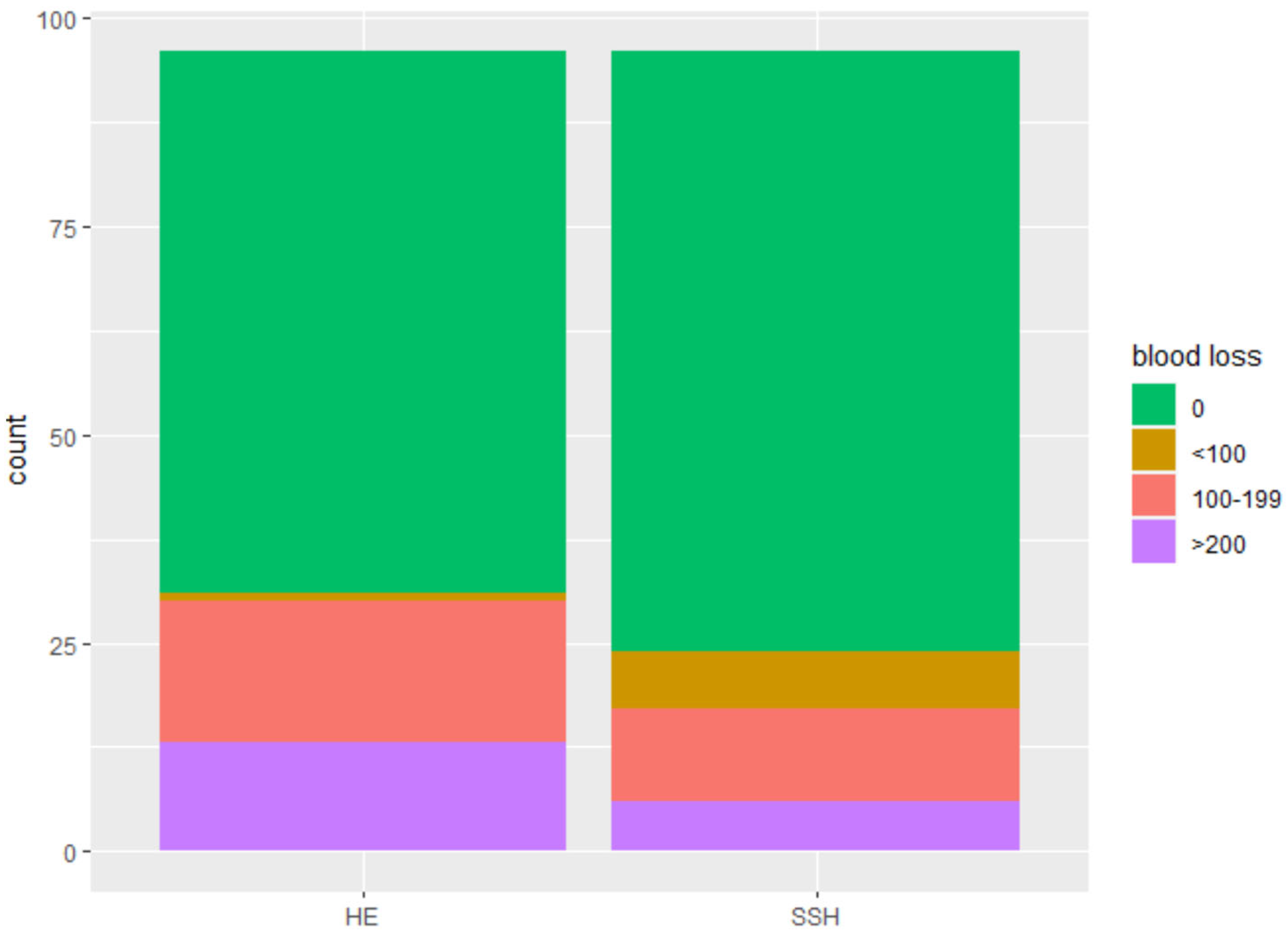
| blood loss (mL) | 0.0332 | Pearson’s Chi-squared test with Yates’ continuity correction | ||||
| 0 | 137 | 65 | 72 | |||
| <100 | 8 | 1 | 7 | |||
| 100–199 | 28 | 17 | 11 | |||
| >200 | 19 | 13 | 6 |
| Variable | All | HE | SSH | p Value | Remark | Test |
|---|---|---|---|---|---|---|
| count | 192 | 96 | 96 | |||
| postoperative complications | 0.1465 | Barnard’s Unconditiol Test | ||||
| no | 156 | 74 | 82 | |||
| yes | 36 | 22 | 14 | |||
| postoperative UTIs | 1.0000 | Barnard’s Unconditiol Test | ||||
| no | 182 | 91 | 91 | |||
| yes | 10 | 5 | 5 | |||
| postoperative bloodtransfusion | 0.2105 | Barnard’s Unconditiol Test | ||||
| no | 190 | 94 | 96 | |||
| yes | 2 | 2 | 0 | |||
| postoperative bleeding | 0.5319 | Barnard’s Unconditiol Test | ||||
| no | 186 | 94 | 92 | |||
| yes | 6 | 2 | 4 | |||
| postoperative pain | 1.0000 | Barnard’s Unconditiol Test | ||||
| no | 186 | 93 | 93 | |||
| yes | 6 | 3 | 3 | |||
| postoperative residual urine | 0.0831 | Barnard’s Unconditiol Test | ||||
| no | 175 | 84 | 91 | |||
| yes | 17 | 12 | 5 | |||
| postoperative bowel issue | 0.5319 | Barnard’s Unconditiol Test | ||||
| no | 186 | 92 | 94 | |||
| yes | 6 | 4 | 2 | |||
| postoperative wound infection | 1.0000 | Barnard’s Unconditiol Test | ||||
| no | 190 | 95 | 96 | |||
| yes | 2 | 1 | 1 | |||
| postoperative fistula | 0.5289 | Barnard’s Unconditiol Test | ||||
| no | 191 | 95 | 96 | |||
| yes | 1 | 1 | 0 | |||
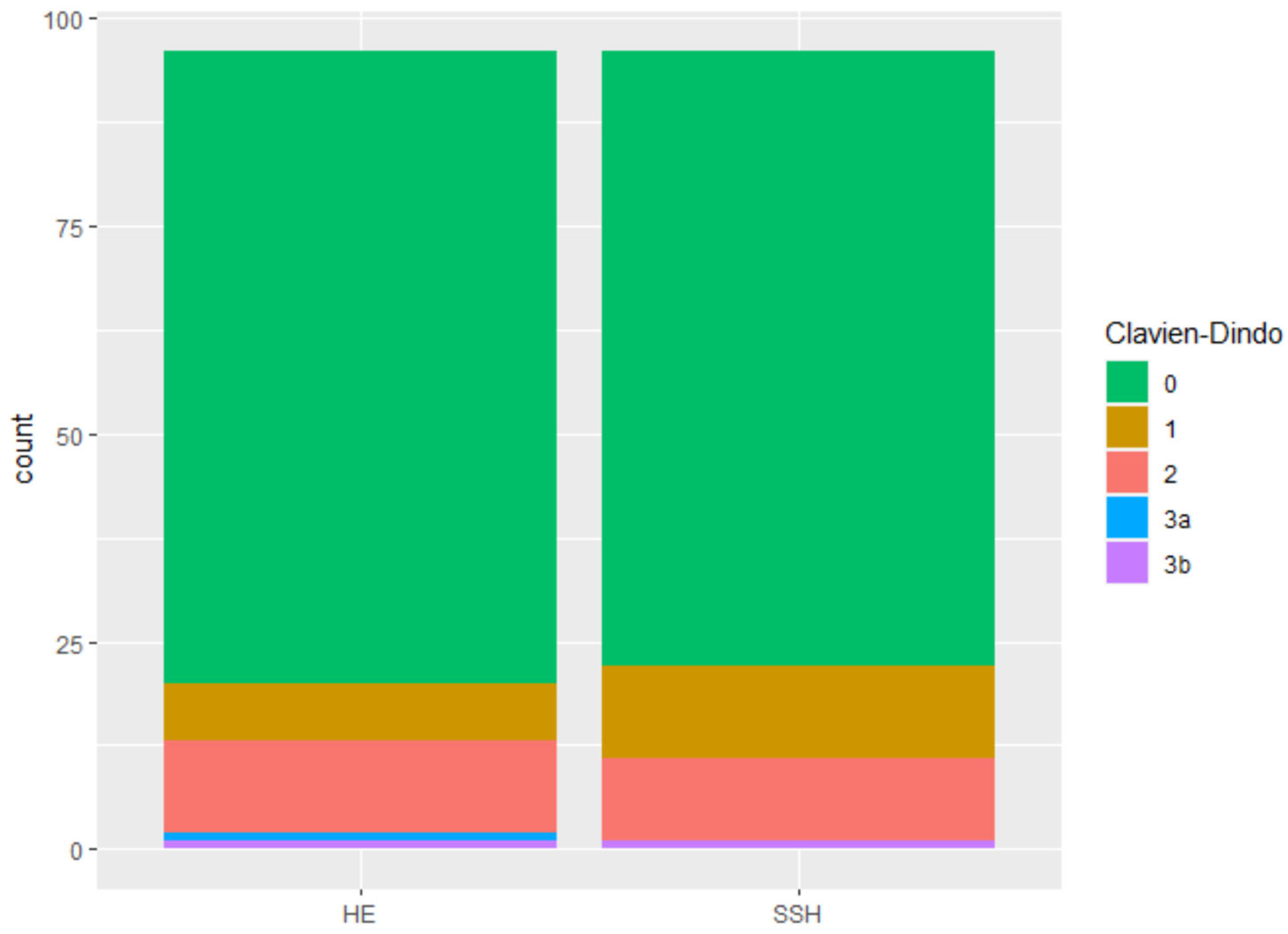
| Clavien-Dindo score | 0.7425 | Pearson’s Chi-squared test with Yates’ continuity correction | ||||
| 0 | 150 | 76 | 74 | |||
| 1 | 18 | 7 | 11 | |||
| 2 | 21 | 11 | 10 | |||
| 3a | 1 | 1 | 0 | |||
| 3b | 2 | 1 | 1 | |||
| Estimate | Standard Error | z Value | Pr (>|z|) | |
|---|---|---|---|---|
| (Intercept) | −0.845 | 1.852 | −0.456 | 0.6482 |
| SSH group | −0.655 | 0.430 | −1.521 | 0.1282 |
| age | 0.013 | 0-017 | 0.730 | 0.465 |
| BMI | −0.010 | 0.050 | −0.195 | 0.8451 |
| preoperative POP-Q stage | −0.314 | 0.483 | −1.651 | 0.5152 |
| Estimate | Standard Error | z Value | Pr (>|z|) | |
|---|---|---|---|---|
| (Intercept) | 0.235 | 2.739 | 0.086 | 0.9317 |
| age | −0.019 | 0.026 | −0.746 | 0.4556 |
| BMI | 0.013 | 0.072 | 0.184 | 0.8537 |
| preoperative POP-Q stage | −0.506 | 0.702 | −0.720 | 0.4717 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carlin, G.L.; Lange, S.; Ziegler, C.; Heinzl, F.; Bodner-Adler, B. Sacrospinous Hysteropexy Versus Prolapse Hysterectomy with Apical Fixation: A Retrospective Comparison over an 18 Year Period. J. Clin. Med. 2023, 12, 2176. https://doi.org/10.3390/jcm12062176
Carlin GL, Lange S, Ziegler C, Heinzl F, Bodner-Adler B. Sacrospinous Hysteropexy Versus Prolapse Hysterectomy with Apical Fixation: A Retrospective Comparison over an 18 Year Period. Journal of Clinical Medicine. 2023; 12(6):2176. https://doi.org/10.3390/jcm12062176
Chicago/Turabian StyleCarlin, Greta Lisa, Sören Lange, Christina Ziegler, Florian Heinzl, and Barbara Bodner-Adler. 2023. "Sacrospinous Hysteropexy Versus Prolapse Hysterectomy with Apical Fixation: A Retrospective Comparison over an 18 Year Period" Journal of Clinical Medicine 12, no. 6: 2176. https://doi.org/10.3390/jcm12062176
APA StyleCarlin, G. L., Lange, S., Ziegler, C., Heinzl, F., & Bodner-Adler, B. (2023). Sacrospinous Hysteropexy Versus Prolapse Hysterectomy with Apical Fixation: A Retrospective Comparison over an 18 Year Period. Journal of Clinical Medicine, 12(6), 2176. https://doi.org/10.3390/jcm12062176






