Diagnosis and Management of Barrett’s Esophagus
Abstract
1. Introduction
2. BE Risk Factors
3. BE Diagnosis
4. BE Risk of Progression to EAC
5. EAC Screening in BE
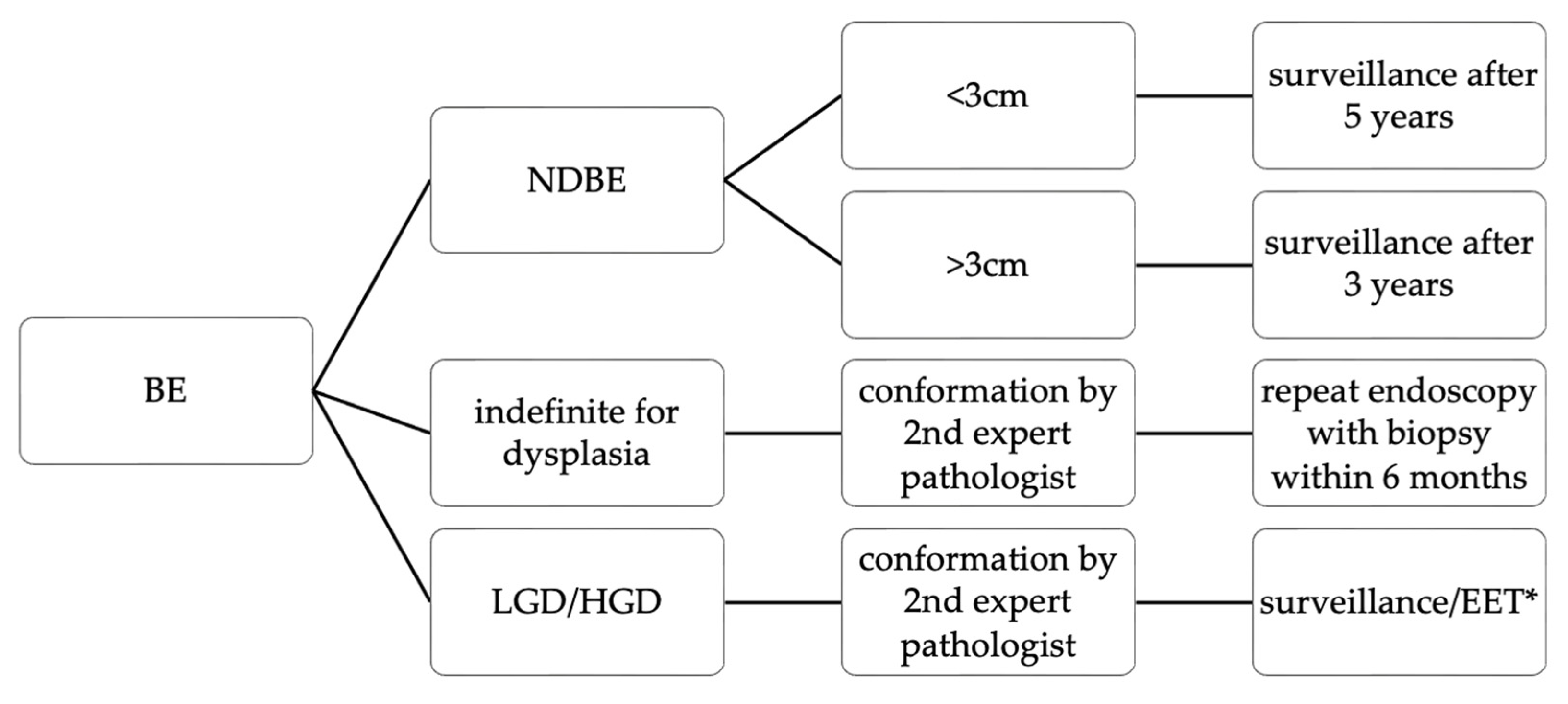
6. BE Management
6.1. Endoscopic Ablation Therapy
| LGD | HGD | |
|---|---|---|
| Polish guidelines [93] | Endoscopic ablation therapy (preferably with RFA), surveillance after 6 months if ablation was not undertaken (recommendation grade A for ablation and C for surveillance) | Endoscopic therapy (options ought to be discussed by an upper GI multidisciplinary team beforehand) |
| BSG [33,104] | ||
| ESGE [52] | Endoscopic ablation therapy (with RFA) | Endoscopic resection is recommended for all the visible lesions. If no lesions suspicious for dysplasia are visible, endoscopist ought to take 4-quadrant biopsies. In case of histopathological conformation of the HGD, endoscopic ablation (with RFA) is recommended. Otherwise, endoscopy should be repeated after 3 months. |
| AGA [110] | Surveillance or EET (endoscopic eradication therapy) | EET (removal of visible lesions with EMR) |
| Australian [111] | Surveillance every 6 months, however, reverting to a less frequent follow-up schedule should be considered if two consecutive endoscopies show no dysplasia or Endoscopic ablation may be considered—especially if LGD is definite, multifocal and present on more than one occasion | Endoscopic resection of visible/nodular lesions and RFA within the flat segments |
| ACG [91] | Surveillance (6 and 12 months after diagnosis, and annually thereafter) or EET (resection of all visible lesions, followed by ablation) and then surveillance endoscopy after 1 years, 3 years and afterwards continued every 2 years) | EET (resection of visible lesions followed by ablation and surveillance 3, 6 and 12 months after complete eradication of remaining metaplastic epithelium and then continued annually) |
| Asia-Pacific consensus [25] | Surveillance endoscopy after 6 months or Endoscopic resection of focal lesions and if there is the absence of such lesions consider RFA | Endoscopic resection followed by RFA |
6.2. Endoscopic Eradication Therapy
6.3. Surgery
7. BE Prevention
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shaheen, N.J.; Falk, G.W.; Iyer, P.G.; Gerson, L.B. ACG Clinical Guideline: Diagnosis and Management of Barrett’s Esophagus. Am. J. Gastroenterol. 2016, 111, 30–50. [Google Scholar] [CrossRef]
- Wang, R.-H. From reflux esophagitis to Barrett’s esophagus and esophageal adenocarcinoma. World J. Gastroenterol. 2015, 21, 5210–5219. [Google Scholar] [CrossRef] [PubMed]
- Ilson, D.H.; van Hillegersberg, R. Management of Patients with Adenocarcinoma or Squamous Cancer of the Esophagus. Gastroenterology 2018, 154, 437–451. [Google Scholar] [CrossRef] [PubMed]
- Botterweck, A.A.; Schouten, L.; Volovics, A.; Dorant, E.; Brandt, P.V.D. Trends in incidence of adenocarcinoma of the oesophagus and gastric cardia in ten European countries. Leuk. Res. 2000, 29, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.; Lieberman, D.A.; Kennedy, K.F.; Hamade, N.; Thota, P.; Parasa, S.; Gorrepati, V.S.; Bansal, A.; Gupta, N.; Gaddam, S.; et al. Increasing prevalence of high-grade dysplasia and adenocarcinoma on index endoscopy in Barrett’s esophagus over the past 2 decades: Data from a multicenter U.S. consortium. Gastrointest. Endosc. 2019, 89, 257–263.e3. [Google Scholar] [CrossRef] [PubMed]
- Pohl, H.; Welch, H.G. The Role of Overdiagnosis and Reclassification in the Marked Increase of Esophageal Adenocarcinoma Incidence. Gynecol. Oncol. 2005, 97, 142–146. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, E.W.; Luna, R.A.; Harrison, V.L.; Hunter, J.G. Barrett’s Esophagus: A Review of the Literature. J. Gastrointest. Surg. 2011, 15, 708–718. [Google Scholar] [CrossRef] [PubMed]
- De Sá, I.M.; Leal, C.; Silva, J.; Falcão, D.; Felix, C.; Nascimento, C.; Carvalho, P.B.; Vasconcelos, H.; Pedroto, I.; Chagas, C.; et al. Prevalence of Barrett’s esophagus in a Southern European country: A multicenter study. Eur. J. Gastroenterol. Hepatol. 2021, 33, e939–e943. [Google Scholar] [CrossRef]
- Ronkainen, J.; Aro, P.; Storskrubb, T.; Johansson, S.; Lind, T.; Bolling–Sternevald, E.; Vieth, M.; Stolte, M.; Talley, N.J.; Agréus, L. Prevalence of Barrett’s Esophagus in the General Population: An Endoscopic Study. Gastroenterology 2005, 129, 1825–1831. [Google Scholar] [CrossRef]
- Post, P.N.; Siersema, P.D.; Van Dekken, H. Rising incidence of clinically evident Barrett’s oesophagus in The Netherlands: A nation-wide registry of pathology reports. Scand. J. Gastroenterol. 2007, 42, 17–22. [Google Scholar] [CrossRef]
- Coleman, H.G.; Bhat, S.; Murray, L.J.; McManus, D.; Gavin, A.T.; Johnston, B.T. Increasing incidence of Barrett’s oesophagus: A population-based study. Eur. J. Epidemiol. 2011, 26, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Muthusamy, V.R.; Wani, S.; Gyawali, C.P.; Komanduri, S.; Bergman, J.; Canto, M.I.; Chak, A.; Corley, D.; Falk, G.W.; Fitzgerald, R.; et al. AGA Clinical Practice Update on New Technology and Innovation for Surveillance and Screening in Barrett’s Esophagus: Expert Review. Clin. Gastroenterol. Hepatol. 2022, 20, 2696–2706.e1. [Google Scholar] [CrossRef] [PubMed]
- Cook, M.B.; Wild, C.P.; Forman, D. A Systematic Review and Meta-Analysis of the Sex Ratio for Barrett’s Esophagus, Erosive Reflux Disease, and Nonerosive Reflux Disease. Eur. J. Epidemiol. 2005, 162, 1050–1061. [Google Scholar] [CrossRef]
- Thukkani, N.; Sonnenberg, A. The influence of environmental risk factors in hospitalization for GERD-related diagnoses in the United States. Aliment. Pharmacol. Ther. 2010, 31, 852–861. [Google Scholar] [CrossRef]
- A Anderson, L.; Watson, R.P.; Murphy, S.J.; Johnston, B.T.; Comber, H.; Mc Guigan, J.; Reynolds, J.V.; Murray, L.J. Risk factors for Barrett’s oesophagus and oesophageal adenocarcinoma: Results from the FINBAR study. World J. Gastroenterol. 2007, 13, 1585–1594. [Google Scholar] [CrossRef]
- Andrici, J.; Cox, M.R.; Eslick, G.D. Cigarette smoking and the risk of Barrett’s esophagus: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2013, 28, 1258–1273. [Google Scholar] [CrossRef]
- Cook, M.B.; Shaheen, N.J.; Anderson, L.A.; Giffen, C.; Chow, W.; Vaughan, T.L.; Whiteman, D.C.; Corley, D.A. Cigarette Smoking Increases Risk of Barrett’s Esophagus: An Analysis of the Barrett’s and Esophageal Adenocarcinoma Consortium. Gastroenterology 2012, 142, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Eloubeidi, M.A.; Provenzale, D. Clinical and Demographic Predictors of Barrett’s Esophagus Among Patients with Gastroesophageal Reflux Disease. J. Clin. Gastroenterol. 2001, 33, 306–309. [Google Scholar] [CrossRef] [PubMed]
- Corley, D.A.; Kubo, A.; Levin, T.R.; Block, G.; Habel, L.; Zhao, W.; Leighton, P.; Quesenberry, C.; Rumore, G.J.; Buffler, P.A. Abdominal Obesity and Body Mass Index as Risk Factors for Barrett’s Esophagus. Gastroenterology 2007, 133, 34–41. [Google Scholar] [CrossRef]
- Edelstein, Z.R.; Farrow, D.C.; Bronner, M.P.; Rosen, S.N.; Vaughan, T.L. Central Adiposity and Risk of Barrett’s Esophagus. Gastroenterology 2007, 133, 403–411. [Google Scholar] [CrossRef]
- Mokrowiecka, A.; Daniel, P.; Jasińska, A.; Pietruczuk, M.; Pawłowski, M.; Szczesniak, P.; Orszulak-Michalak, D.; Malecka-Panas, E. Serum Adiponectin, Resistin, Leptin Concentration and Central Adiposity Parameters in Barrett’s Esophagus Patients with and without Intestinal Metaplasia in Comparison to Healthy Controls and Patients with GERD. Hepato-Gastroenterology 2012, 59, 2395–2399. [Google Scholar] [CrossRef] [PubMed]
- Chak, A.; Ochs-Balcom, H.; Falk, G.; Grady, W.M.; Kinnard, M.; Willis, J.E.; Elston, R.; Eng, C. Familiality in Barrett’s Esophagus, Adenocarcinoma of the Esophagus, and Adenocarcinoma of the Gastroesophageal Junction. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1668–1673. [Google Scholar] [CrossRef]
- Juhasz, A.; Mittal, S.K.; Lee, T.H.; Deng, C.; Chak, A.; Lynch, H.T. Prevalence of Barrett Esophagus in First-Degree Relatives of Patients with Esophageal Adenocarcinoma. J. Clin. Gastroenterol. 2011, 45, 867–871. [Google Scholar] [CrossRef]
- Fock, K.M.; Talley, N.; Goh, K.L.; Sugano, K.; Katelaris, P.; Holtmann, G.; Pandolfino, J.E.; Sharma, P.; Ang, T.L.; Hongo, M.; et al. Asia-Pacific consensus on the management of gastro-oesophageal reflux disease: An update focusing on refractory reflux disease and Barrett’s oesophagus. Gut 2016, 65, 1402–1415. [Google Scholar] [CrossRef] [PubMed]
- Edelstein, Z.R.; Bronner, M.P.; Rosen, S.N.; Vaughan, T.L. Risk Factors for Barrett’s Esophagus Among Patients with Gastroesophageal Reflux Disease: A Community Clinic-Based Case–Control Study. Am. J. Gastroenterol. 2009, 104, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Eusebi, L.H.; Telese, A.; Cirota, G.G.; Haidry, R.; Zagari, R.M.; Bazzoli, F.; Ford, A.C. Systematic review with meta-analysis: Risk factors for Barrett’s oesophagus in individuals with gastro-oesophageal reflux symptoms. Aliment. Pharmacol. Ther. 2021, 53, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Kambhampati, S.; Tieu, A.H.; Luber, B.; Wang, H.; Meltzer, S.J. Risk Factors for Progression of Barrett’s Esophagus to High Grade Dysplasia and Esophageal Adenocarcinoma. Sci. Rep. 2020, 10, 4899. [Google Scholar] [CrossRef]
- Rubenstein, J.H.; McConnell, D.; Waljee, A.K.; Metko, V.; Nofz, K.; Khodadost, M.; Jiang, L.; Raghunathan, T. Validation and Comparison of Tools for Selecting Individuals to Screen for Barrett’s Esophagus and Early Neoplasia. Gastroenterology 2020, 158, 2082–2092. [Google Scholar] [CrossRef]
- Xie, S.-H.; Ness-Jensen, E.; Medefelt, N.; Lagergren, J. Open: Assessing the Feasibility of Targeted Screening for Esophageal Adenocarcinoma Based on Individual Risk Assessment in a Population-Based Cohort Study in Norway (The HUNT Study). Am. J. Gastroenterol. 2018, 113, 829–835. [Google Scholar] [CrossRef]
- Rubenstein, J.H.; Morgenstern, H.; Appelman, H.; Scheiman, J.; Schoenfeld, P.; McMahon, L.F.; Metko, V.; Near, E.; Kellenberg, J.; Kalish, T.; et al. Prediction of Barrett’s Esophagus Among Men. Am. J. Gastroenterol. 2013, 108, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Kunzmann, A.T.; Thrift, A.P.; Cardwell, C.R.; Lagergren, J.; Xie, S.; Johnston, B.T.; Anderson, L.; Busby, J.; McMenamin, Ú.C.; Spence, A.D.; et al. Model for Identifying Individuals at Risk for Esophageal Adenocarcinoma. Clin. Gastroenterol. Hepatol. 2018, 16, 1229–1236.e4. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, R.C.; Di Pietro, M.; Ragunath, K.; Ang, Y.; Kang, J.-Y.; Watson, P.; Trudgill, N.; Patel, P.; Kaye, P.V.; Sanders, S.; et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut 2014, 63, 7–42. [Google Scholar] [CrossRef] [PubMed]
- Herrero, L.A.; Curvers, W.L.; van Vilsteren, F.G.I.; Wolfsen, H.; Ragunath, K.; Song, L.-M.W.K.; Mallant-Hent, R.C.; van Oijen, A.; Scholten, P.; Schoon, E.J.; et al. Validation of the Prague C&M classification of Barrett’s esophagus in clinical practice. Endoscopy 2013, 45, 876–882. [Google Scholar] [CrossRef]
- Gorrepati, V.S.; Sharma, P. How Should We Report Endoscopic Results in Patient’s with Barrett’s Esophagus? Dig. Dis. Sci. 2018, 63, 2115–2121. [Google Scholar] [CrossRef]
- Sharma, P.; Dent, J.; Armstrong, D.; Bergman, J.J.; Gossner, L.; Hoshihara, Y.; Jankowski, J.; Junghard, O.; Lundell, L.; Tytgat, G.N.; et al. The Development and Validation of an Endoscopic Grading System for Barrett’s Esophagus: The Prague C & M Criteria. Gastroenterology 2006, 131, 1392–1399. [Google Scholar] [CrossRef]
- Participants in the Paris Workshop. The Paris endoscopic classification of superficial neoplastic lesions: Esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest. Endosc. 2003, 58, S3–S43. [Google Scholar] [CrossRef]
- Maroni, R.; Barnes, J.; Offman, J.; Scheibl, F.; Smith, S.G.; Debiram-Beecham, I.; Waller, J.; Sasieni, P.; Fitzgerald, R.C.; Rubin, G.; et al. Patient-reported experiences and views on the Cytosponge test: A mixed-methods analysis from the BEST3 trial. BMJ Open 2022, 12, e054258. [Google Scholar] [CrossRef]
- A Katzka, D.; Smyrk, T.C.; A Alexander, J.; Geno, D.M.; A Beitia, R.; O Chang, A.; Shaheen, N.J.; Fitzgerald, R.C.; Dellon, E.S. Accuracy and Safety of the Cytosponge for Assessing Histologic Activity in Eosinophilic Esophagitis: A Two-Center Study. Am. J. Gastroenterol. 2017, 112, 1538–1544. [Google Scholar] [CrossRef]
- Benaglia, T.; Sharples, L.D.; Fitzgerald, R.C.; Lyratzopoulos, G. Health Benefits and Cost Effectiveness of Endoscopic and Nonendoscopic Cytosponge Screening for Barrett’s Esophagus. Gastroenterology 2013, 144, 62–73.e6. [Google Scholar] [CrossRef]
- De Jonge, P.J.F.; Van Blankenstein, M.; Looman, C.W.N.; Casparie, M.K.; A Meijer, G.; Kuipers, E.J. Risk of malignant progression in patients with Barrett’s oesophagus: A Dutch nationwide cohort study. Gut 2010, 59, 1030–1036. [Google Scholar] [CrossRef] [PubMed]
- Desai, T.K.; Krishnan, K.; Samala, N.; Singh, J.; Cluley, J.; Perla, S.; Howden, C.W. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: A meta-analysis. Gut 2012, 61, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Sikkema, M.; de Jonge, P.J.; Steyerberg, E.W.; Kuipers, E.J. Risk of Esophageal Adenocarcinoma and Mortality in Patients With Barrett’s Esophagus: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2010, 8, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Thomas, T.; Abrams, K.R.; De Caestecker, J.S.; Robinson, R.J. Meta analysis: Cancer risk in Barrett’s oesophagus. Aliment. Pharmacol. Ther. 2007, 26, 1465–1477. [Google Scholar] [CrossRef]
- Wani, S.; Puli, S.R.; Shaheen, N.J.; Westhoff, B.; Slehria, S.; Bansal, A.; Rastogi, A.; Sayana, H.; Sharma, P. Esophageal Adenocarcinoma in Barrett’s Esophagus After Endoscopic Ablative Therapy: A Meta-Analysis and Systematic Review. Am. J. Gastroenterol. 2009, 104, 502–513. [Google Scholar] [CrossRef]
- Yousef, F.; Cardwell, C.; Cantwell, M.M.; Galway, K.; Johnston, B.T.; Murray, L. The Incidence of Esophageal Cancer and High-Grade Dysplasia in Barrett’s Esophagus: A Systematic Review and Meta-Analysis. Eur. J. Epidemiol. 2008, 168, 237–249. [Google Scholar] [CrossRef]
- Shaheen, N.J.; Crosby, M.A.; Bozymski, E.M.; Sandler, R.S. Is there publication bias in the reporting of cancer risk in Barrett’s esophagus? Gastroenterology 2000, 119, 333–338. [Google Scholar] [CrossRef]
- Hvid-Jensen, F.; Pedersen, L.; Drewes, A.M.; Sørensen, H.T.; Funch-Jensen, P. Incidence of Adenocarcinoma among Patients with Barrett’s Esophagus. N. Engl. J. Med. 2011, 365, 1375–1383. [Google Scholar] [CrossRef]
- Kunzmann, A.T.; Coleman, H.G.; Johnston, B.T.; Turkington, R.C.; McManus, D.; Anderson, L.; Thrift, A.P. Does Risk of Progression from Barrett’s Esophagus to Esophageal Adenocarcinoma Change Based on the Number of Non-dysplastic Endoscopies? Dig. Dis. Sci. 2021, 66, 1965–1973. [Google Scholar] [CrossRef]
- Chandrasekar, V.T.; Hamade, N.; Desai, M.; Rai, T.; Gorrepati, V.S.; Jegadeesan, R.; Sathyamurthy, A.; Sharma, P. Significantly lower annual rates of neoplastic progression in short- compared to long-segment non-dysplastic Barrett’s esophagus: A systematic review and meta-analysis. Endoscopy 2019, 51, 665–672. [Google Scholar] [CrossRef]
- Qumseya, B.; Sultan, S.; Bain, P.; Jamil, L.; Jacobson, B.; Anandasabapathy, S.; Agrawal, D.; Buxbaum, J.L.; Fishman, D.S.; Gurudu, S.R.; et al. ASGE guideline on screening and surveillance of Barrett’s esophagus. Gastrointest. Endosc. 2019, 90, 335–359.e2. [Google Scholar] [CrossRef]
- Weusten, B.; Bisschops, R.; Coron, E.; Dinis-Ribeiro, M.; Dumonceau, J.-M.; Esteban, J.-M.; Hassan, C.; Pech, O.; Repici, A.; Bergman, J.; et al. Endoscopic management of Barrett’s esophagus: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 2017, 49, 191–198. [Google Scholar] [CrossRef]
- Corley, D.A.; Mehtani, K.; Quesenberry, C.; Zhao, W.; de Boer, J.; Weiss, N.S. Impact of Endoscopic Surveillance on Mortality from Barrett’s Esophagus–Associated Esophageal Adenocarcinomas. Gastroenterology 2013, 145, 312–319.e1. [Google Scholar] [CrossRef]
- Codipilly, D.C.; Chandar, A.K.; Singh, S.; Wani, S.; Shaheen, N.J.; Inadomi, J.M.; Chak, A.; Iyer, P.G. The Effect of Endoscopic Surveillance in Patients with Barrett’s Esophagus: A Systematic Review and Meta-analysis. Gastroenterology 2018, 154, 2068–2086.e5. [Google Scholar] [CrossRef]
- Curvers, W.L.; Kate, F.J.T.; Krishnadath, K.K.; Visser, M.; Elzer, B.; Baak, L.C.; Bohmer, C.; Mallant-Hent, R.C.; van Oijen, A.; Naber, A.H.; et al. Low-Grade Dysplasia in Barrett’s Esophagus: Overdiagnosed and Underestimated. Am. J. Gastroenterol. 2010, 105, 1523–1530. [Google Scholar] [CrossRef] [PubMed]
- Duits, L.C.; Phoa, K.N.; Curvers, W.L.; Kate, F.J.W.T.; A Meijer, G.; A Seldenrijk, C.; Offerhaus, G.J.; Visser, M.; Meijer, S.L.; Krishnadath, K.K.; et al. Barrett’s oesophagus patients with low-grade dysplasia can be accurately risk-stratified after histological review by an expert pathology panel. Gut 2015, 64, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.; Treanor, D.; Dixon, M.; Axon, A. Low-grade dysplasia in Barrett’s esophagus has a high risk of progression. Endoscopy 2007, 39, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Thota, P.N.; Lee, H.-J.; Goldblum, J.R.; Liu, X.; Sanaka, M.R.; Gohel, T.; Kanadiya, M.; Lopez, R. Risk Stratification of Patients with Barrett’s Esophagus and Low-grade Dysplasia or Indefinite for Dysplasia. Clin. Gastroenterol. Hepatol. 2015, 13, 459–465.e1. [Google Scholar] [CrossRef] [PubMed]
- Vieth, M.; Schubert, B.; Lang-Schwarz, K.; Stolte, M. Frequency of Barrett’s neoplasia after initial negative endoscopy with biopsy: A long-term histopathological follow-up study. Endoscopy 2006, 38, 1201–1205. [Google Scholar] [CrossRef]
- Wani, S.; Falk, G.; Post, J.; Yerian, L.; Hall, M.; Wang, A.; Gupta, N.; Gaddam, S.; Singh, M.; Singh, V.; et al. Risk Factors for Progression of Low-Grade Dysplasia in Patients with Barrett’s Esophagus. Gastroenterology 2011, 141, 1179–1186.e1. [Google Scholar] [CrossRef]
- Reid, B.J.; Levine, D.S.; Longton, G.; Blount, P.L.; Rabinovitch, P.S. Predictors of Progression to Cancer in Barrett’s Esophagus: Baseline Histology and Flow Cytometry Identify Low- and High-Risk Patient Subsets. Am. J. Gastroenterol. 2000, 95, 1669–1676. [Google Scholar] [CrossRef]
- Rice, T.W. Commentary: Esophageal carcinoma confined to the wall—The need for immediate definitive therapy. J. Thorac. Cardiovasc. Surg. 1999, 117, 26–27. [Google Scholar] [CrossRef]
- Dunbar, K.B.; Spechler, S.J. The Risk of Lymph-Node Metastases in Patients with High-Grade Dysplasia or Intramucosal Carcinoma in Barrett’s Esophagus: A Systematic Review. Am. J. Gastroenterol. 2012, 107, 850–862. [Google Scholar] [CrossRef]
- Downs-Kelly, E.; Mendelin, J.E.; Bennett, A.E.; A Castilla, E.; Henricks, W.H.; Schoenfield, L.; Skacel, M.; Yerian, L.; Rice, T.W.; Rybicki, L.A.; et al. Poor Interobserver Agreement in the Distinction of High-Grade Dysplasia and Adenocarcinoma in Pretreatment Barrett’s Esophagus Biopsies. Am. J. Gastroenterol. 2008, 103, 2333–2340. [Google Scholar] [CrossRef]
- Konda, V.J.A.; Souza, R.F. Biomarkers of Barrett’s Esophagus: From the Laboratory to Clinical Practice. Dig. Dis. Sci. 2018, 63, 2070–2080. [Google Scholar] [CrossRef]
- Mokrowiecka, A.; Wierzchniewska-Ławska, A.; Smolarz, B.; Romanowicz-Makowska, H.; Malecka-Panas, E. p16 gene mutations in Barrett’s esophagus in gastric metaplasia—intestinal metaplasia—dysplasia—adenocarcinoma sequence. Adv. Med. Sci. 2012, 57, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Stachler, M.D.; Taylor-Weiner, A.; Peng, S.; McKenna, A.; Agoston, A.T.; Odze, R.D.; Davison, J.M.; Nason, K.S.; Loda, M.; Leshchiner, I.; et al. Paired exome analysis of Barrett’s esophagus and adenocarcinoma. Nat. Genet. 2015, 47, 1047–1055. [Google Scholar] [CrossRef]
- Kastelein, F.; Biermann, K.; Steyerberg, E.W.; Verheij, J.; Kalisvaart, M.; Looijenga, L.H.J.; A Stoop, H.; Walter, L.; Kuipers, E.J.; Spaander, M.C.W.; et al. Aberrant p53 protein expression is associated with an increased risk of neoplastic progression in patients with Barrett’s oesophagus. Gut 2013, 62, 1676–1683. [Google Scholar] [CrossRef] [PubMed]
- Mokrowiecka, A.; Wierzchniewska-Ławska, A.; Smolarz, B.; Romanowicz-Makowska, H.; Malecka-Panas, E. Polymorphism/loss of heterozygosity of APC gene in GERD-Barrett’s metaplasia-dysplasia-adenocarcinoma sequence. Pol. Merkur. Lekarski. 2009, 26, 385–389. [Google Scholar] [PubMed]
- Gupta, N.; Gaddam, S.; Wani, S.B.; Bansal, A.; Rastogi, A.; Sharma, P. Longer inspection time is associated with increased detection of high-grade dysplasia and esophageal adenocarcinoma in Barrett’s esophagus. Gastrointest. Endosc. 2012, 76, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Connor, M.J.; Sharma, P. Chromoendoscopy and magnification endoscopy for diagnosing esophageal cancer and dysplasia. Thorac. Surg. Clin. 2004, 14, 87–94. [Google Scholar] [CrossRef]
- Horwhat, J.D.; Maydonovitch, C.L.; Ramos, F.; Colina, R.; Gaertner, E.; Lee, H.; Wong, R.K. A Randomized Comparison of Methylene Blue-Directed Biopsy Versus Conventional Four-Quadrant Biopsy for the Detection of Intestinal Metaplasia and Dysplasia in Patients with Long-Segment Barrett’s Esophagus. Am. J. Gastroenterol. 2008, 103, 546–554. [Google Scholar] [CrossRef]
- Lim, C.H.; Rotimi, O.; Dexter, S.P.; Axon, A.T. Randomized crossover study that used methylene blue or random 4-quadrant biopsy for the diagnosis of dysplasia in Barrett’s esophagus. Gastrointest. Endosc. 2006, 64, 195–199. [Google Scholar] [CrossRef]
- Ngamruengphong, S.; Sharma, V.K.; Das, A. Diagnostic yield of methylene blue chromoendoscopy for detecting specialized intestinal metaplasia and dysplasia in Barrett’s esophagus: A meta-analysis. Gastrointest. Endosc. 2009, 69, 1021–1028. [Google Scholar] [CrossRef] [PubMed]
- Olliver, J.; Wild, C.; Sahay, P.; Dexter, S.; Hardie, L. Chromoendoscopy with methylene blue and associated DNA damage in Barrett’s oesophagus. Lancet 2003, 362, 373–374. [Google Scholar] [CrossRef]
- Repici, A.; Ciscato, C.; Wallace, M.; Sharma, P.; Anderloni, A.; Carrara, S.; Di Leo, M.; Hassan, C. Evaluation of genotoxicity related to oral methylene blue chromoendoscopy. Endoscopy 2018, 50, 1027–1032. [Google Scholar] [CrossRef]
- Coletta, M.; Sami, S.S.; Nachiappan, A.; Fraquelli, M.; Casazza, G.; Ragunath, K. Acetic acid chromoendoscopy for the diagnosis of early neoplasia and specialized intestinal metaplasia in Barrett’s esophagus: A meta-analysis. Gastrointest. Endosc. 2016, 83, 57–67.e1. [Google Scholar] [CrossRef]
- Bhandari, P.; Kandaswamy, P.; Cowlishaw, D.; Longcroft-Wheaton, G. Acetic acid-enhanced chromoendoscopy is more cost-effective than protocol-guided biopsies in a high-risk Barrett’s population. Dis. Esophagus 2012, 25, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, C.E.O.; Lima, J.C.P.; Lopes, C.V.; Malaman, D.; Salomão, A.D.; Garcia, A.C.; Teixeira, C.R. Computerized virtual chromoendoscopy versus indigo carmine chromoendoscopy combined with magnification for diagnosis of small colorectal lesions. Eur. J. Gastroenterol. Hepatol. 2010, 22, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Gono, K.; Obi, T.; Yamaguchi, M.; Ohyama, N.; Machida, H.; Sano, Y.; Yoshida, S.; Hamamoto, Y.; Endo, T. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J. Biomed. Opt. 2004, 9, 568–577. [Google Scholar] [CrossRef]
- Sharma, P.; Hawes, R.H.; Bansal, A.; Gupta, N.; Curvers, W.; Rastogi, A.; Singh, M.; Hall, M.; Mathur, S.C.; Wani, S.B.; et al. Standard endoscopy with random biopsies versus narrow band imaging targeted biopsies in Barrett’s oesophagus: A prospective, international, randomised controlled trial. Gut 2013, 62, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Furneri, G.; Klausnitzer, R.; Haycock, L.; Ihara, Z. Economic value of narrow-band imaging versus white light endoscopy for the diagnosis and surveillance of Barrett’s esophagus: Cost-consequence model. PLoS ONE 2019, 14, e0212916. [Google Scholar] [CrossRef] [PubMed]
- Picot, J.; Rose, M.; Cooper, K.; Pickett, K.; Lord, J.; Harris, P.; Whyte, S.; Böhning, D.; Shepherd, J. Virtual chromoendoscopy for the real-time assessment of colorectal polyps in vivo: A systematic review and economic evaluation. Health Technol. Assess. 2017, 21, 1–308. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, A.; Korczynski, O.; Tresch, A.; Hansen, T.; Rahman, F.; Goetz, M.; Murthy, S.; Galle, P.R.; Kiesslich, R. Acetic acid compared with i-scan imaging for detecting Barrett’s esophagus: A randomized, comparative trial. Gastrointest. Endosc. 2014, 79, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Bruno, M.J. Magnification endoscopy, high resolution endoscopy, and chromoscopy; towards a better optical diagnosis. Gut 2003, 52, iv7–iv11. [Google Scholar] [CrossRef]
- Wasielica-Berger, J.; Baniukiewicz, A.; Wroblewski, E.; Chwiesko, A.; Dabrowski, A. Magnification Endoscopy and Chromoendoscopy in Evaluation of Specialized Intestinal Metaplasia in Barrett’s Esophagus. Dig. Dis. Sci. 2011, 56, 1987–1995. [Google Scholar] [CrossRef]
- Endo, T.; Awakawa, T.; Takahashi, H.; Arimura, Y.; Itoh, F.; Yamashita, K.; Sasaki, S.; Yamamoto, H.; Tang, X.; Imai, K. Classification of Barrett’s epithelium by magnifying endoscopy. Gastrointest. Endosc. 2002, 55, 641–647. [Google Scholar] [CrossRef]
- Nguyen, T.H.; Thrift, A.P.; Rugge, M.; El-Serag, H.B. Prevalence of Barrett’s esophagus and performance of societal screening guidelines in an unreferred primary care population of U.S. veterans. Gastrointest. Endosc. 2021, 93, 409–419.e1. [Google Scholar] [CrossRef]
- Sawas, T.; Zamani, S.A.; Killcoyne, S.; Dullea, A.; Wang, K.K.; Iyer, P.G.; Fitzgerald, R.C.; Katzka, D.A. Limitations of Heartburn and Other Societies’ Criteria in Barrett’s Screening for Detecting De Novo Esophageal Adenocarcinoma. Clin. Gastroenterol. Hepatol. 2022, 20, 1709–1718. [Google Scholar] [CrossRef]
- El-Serag, H.B.; Sweet, S.; Winchester, C.C.; Dent, J. Update on the epidemiology of gastro-oesophageal reflux disease: A systematic review. Gut 2014, 63, 871–880. [Google Scholar] [CrossRef]
- Shaheen, N.J.; Falk, G.W.; Iyer, P.G.; Souza, R.F.; Yadlapati, R.H.; Sauer, B.G.; Wani, S. Diagnosis and Management of Barrett’s Esophagus: An Updated ACG Guideline. Am. J. Gastroenterol. 2022, 117, 559–587. [Google Scholar] [CrossRef]
- Bennett, C.; Moayyedi, P.; A Corley, D.; de Caestecker, J.; Falck-Ytter, Y.; Falk, G.; Vakil, N.; Sanders, S.; Vieth, M.; Inadomi, J.; et al. BOB CAT: A Large-Scale Review and Delphi Consensus for Management of Barrett’s Esophagus with No Dysplasia, Indefinite for, or Low-Grade Dysplasia. Am. J. Gastroenterol. 2015, 110, 662–682. [Google Scholar] [CrossRef]
- Ratcliffe, E.G.; Jankowski, J.A. Gastroesophageal reflux disease and Barrett esophagus: An overview of evidence-based guidelines. Pol. Arch. Intern. Med. 2019, 129, 516–525. [Google Scholar] [CrossRef]
- E Verbeek, R.; Leenders, M.; Kate, F.J.W.T.; van Hillegersberg, R.; Vleggaar, F.P.; van Baal, J.W.P.M.; van Oijen, M.G.H.; Siersema, P.D. Surveillance of Barrett’s Esophagus and Mortality from Esophageal Adenocarcinoma: A Population-Based Cohort Study. Am. J. Gastroenterol. 2014, 109, 1215–1222. [Google Scholar] [CrossRef]
- Inadomi, J.M.; Saxena, N. Screening and Surveillance for Barrett’s Esophagus: Is It Cost-Effective? Dig. Dis. Sci. 2018, 63, 2094–2104. [Google Scholar] [CrossRef]
- Lee, S.-W.; Lien, H.-C.; Chang, C.-S.; Lin, M.-X.; Chang, C.-H.; Ko, C.-W. Benefits of the Seattle biopsy protocol in the diagnosis of Barrett’s esophagus in a Chinese population. World J. Clin. Cases 2018, 6, 753–758. [Google Scholar] [CrossRef]
- Nachiappan, A.; Ragunath, K.; Card, T.; Kaye, P. Diagnosing dysplasia in Barrett’s oesophagus still requires Seattle protocol biopsy in the era of modern video endoscopy: Results from a tertiary centre Barrett’s dysplasia database. Scand. J. Gastroenterol. 2020, 55, 9–13. [Google Scholar] [CrossRef]
- Visrodia, K.; Singh, S.; Krishnamoorthi, R.; Ahlquist, D.A.; Wang, K.K.; Iyer, P.G.; Katzka, D.A. Magnitude of Missed Esophageal Adenocarcinoma After Barrett’s Esophagus Diagnosis: A Systematic Review and Meta-analysis. Gastroenterology 2016, 150, 599–607.e7. [Google Scholar] [CrossRef]
- Agha, Y.H.; Srinivasan, S.; Hyder, J.; Wuthnow, C.; Taleb, A.; Tofteland, N.; Kilgore, W.; Salyers, W. WATS(3D) versus forceps biopsy in screening for Barrett’s esophagus: Experience in community endoscopy centers. Ann. Gastroenterol. 2021, 34, 164–168. [Google Scholar] [CrossRef]
- Pan, W.; Li, X.; Wang, W.; Zhou, L.; Wu, J.; Ren, T.; Liu, C.; Lv, M.; Su, S.; Tang, Y. Identification of Barrett’s esophagus in endoscopic images using deep learning. BMC Gastroenterol. 2021, 21, 479. [Google Scholar] [CrossRef]
- Tan, J.L.; Chinnaratha, M.A.; Woodman, R.; Martin, R.; Chen, H.-T.; Carneiro, G.; Singh, R. Diagnostic Accuracy of Artificial Intelligence (AI) to Detect Early Neoplasia in Barrett’s Esophagus: A Non-comparative Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 890720. [Google Scholar] [CrossRef] [PubMed]
- Enestvedt, B.K.; Lugo, R.; Guarner-Argente, C.; Shah, P.; Falk, G.; Furth, E.; Ginsberg, G.G. Location, location, location: Does early cancer in Barrett’s esophagus have a preference? Gastrointest. Endosc. 2013, 78, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Krajciova, J.; Vackova, Z.; Spicak, J.; Martinek, J. Radiofrequency ablation for Barrett’s esophagus-related neoplasia. Int. J. Clin. Rev. 2018, 73, 366–377. [Google Scholar] [CrossRef] [PubMed]
- Di Pietro, M.; Fitzgerald, R.C. Revised British Society of Gastroenterology recommendation on the diagnosis and management of Barrett’s oesophagus with low-grade dysplasia. Gut 2018, 67, 392–393. [Google Scholar] [CrossRef]
- Qumseya, B.J.; Wani, S.; Gendy, S.; Harnke, B.; Bergman, J.J.; Wolfsen, H. Disease Progression in Barrett’s Low-Grade Dysplasia With Radiofrequency Ablation Compared With Surveillance: Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2017, 112, 849–865. [Google Scholar] [CrossRef]
- Klair, J.S.; Zafar, Y.; Nagra, N.; Murali, A.R.; Jayaraj, M.; Singh, D.; Rustagi, T.; Krishnamoorthi, R. Outcomes of Radiofrequency Ablation versus Endoscopic Surveillance for Barrett’s Esophagus with Low-Grade Dysplasia: A Systematic Review and Meta-Analysis. Dig. Dis. 2021, 39, 561–568. [Google Scholar] [CrossRef]
- Kahn, A.; Al-Qaisi, M.; Temkit, M.; Kommineni, V.T.; Callaway, J.K.; Boroff, E.S.; Burdick, G.E.; Lam-Himlin, D.M.; Vela, M.F.; Ramirez, F.C. Longitudinal outcomes of radiofrequency ablation versus surveillance endoscopy for Barrett’s esophagus with low-grade dysplasia. Dis. Esophagus 2018, 31, dox120. [Google Scholar] [CrossRef]
- Shaheen, N.J.; Sharma, P.; Overholt, B.F.; Wolfsen, H.C.; Sampliner, R.E.; Wang, K.K.; Galanko, J.A.; Bronner, M.P.; Goldblum, J.R.; Bennett, A.E.; et al. Radiofrequency Ablation in Barrett’s Esophagus with Dysplasia. N. Engl. J. Med. 2009, 360, 2277–2288. [Google Scholar] [CrossRef]
- Manner, H.; Rabenstein, T.; Pech, O.; Braun, K.; May, A.; Pohl, J.; Behrens, A.; Vieth, M.; Ell, C. Ablation of residual Barrett’s epithelium after endoscopic resection: A randomized long-term follow-up study of argon plasma coagulation vs. surveillance (APE study). Endoscopy 2014, 46, 6–12. [Google Scholar] [CrossRef]
- Sharma, P.; Shaheen, N.J.; Katzka, D.; Bergman, J.J. AGA Clinical Practice Update on Endoscopic Treatment of Barrett’s Esophagus with Dysplasia and/or Early Cancer: Expert Review. Gastroenterology 2020, 158, 760–769. [Google Scholar] [CrossRef]
- Whiteman, D.C.; Appleyard, M.; Bahin, F.F.; Bobryshev, Y.V.; Bourke, M.J.; Brown, I.; Chung, A.; Clouston, A.; Dickins, E.; Emery, J.; et al. Australian clinical practice guidelines for the diagnosis and management of Barrett’s esophagus and early esophageal adenocarcinoma. J. Gastroenterol. Hepatol. 2015, 30, 804–820. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Puri, V.; Shami, V.M.; Stukenborg, G.J.; Kozower, B.D. Comparative Effectiveness of Esophagectomy Versus Endoscopic Treatment for Esophageal High-grade Dysplasia. Ann. Surg. 2016, 263, 719–726. [Google Scholar] [CrossRef]
- Chu, J.N.; Choi, J.; Tramontano, A.; Morse, C.; Forcione, D.; Nishioka, N.S.; Abrams, J.A.; Rubenstein, J.H.; Kong, C.Y.; Inadomi, J.M.; et al. Surgical vs Endoscopic Management of T1 Esophageal Adenocarcinoma: A Modeling Decision Analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 392–400.e7. [Google Scholar] [CrossRef] [PubMed]
- Wani, S.; Drahos, J.; Cook, M.B.; Rastogi, A.; Bansal, A.; Yen, R.; Sharma, P.; Das, A. Comparison of endoscopic therapies and surgical resection in patients with early esophageal cancer: A population-based study. Gastrointest. Endosc. 2014, 79, 224–232.e1. [Google Scholar] [CrossRef] [PubMed]
- Holmes, I.; Hing, T.; Friedland, S. Combining endoscopic submucosal dissection and endoscopic mucosal resection to treat neoplasia in Barrett’s esophagus. Surg. Endosc. 2016, 30, 5330–5337. [Google Scholar] [CrossRef]
- Ishihara, R.; Iishi, H.; Uedo, N.; Takeuchi, Y.; Yamamoto, S.; Yamada, T.; Masuda, E.; Higashino, K.; Kato, M.; Narahara, H.; et al. Comparison of EMR and endoscopic submucosal dissection for en bloc resection of early esophageal cancers in Japan. Gastrointest. Endosc. 2008, 68, 1066–1072. [Google Scholar] [CrossRef]
- Pouw, R.E.; van Vilsteren, F.G.; Peters, F.P.; Herrero, L.A.; Kate, F.J.T.; Visser, M.; Schenk, B.E.; Schoon, E.J.; Peters, F.T.; Houben, M.; et al. Randomized trial on endoscopic resection-cap versus multiband mucosectomy for piecemeal endoscopic resection of early Barrett’s neoplasia. Gastrointest. Endosc. 2011, 74, 35–43. [Google Scholar] [CrossRef]
- Oka, S.; Tanaka, S.; Saito, Y.; Iishi, H.; Kudo, S.-E.; Ikematsu, H.; Igarashi, M.; Saitoh, Y.; Inoue, Y.; Kobayashi, K.; et al. Local Recurrence After Endoscopic Resection for Large Colorectal Neoplasia: A Multicenter Prospective Study in Japan. Am. J. Gastroenterol. 2015, 110, 697–707. [Google Scholar] [CrossRef]
- Geramizadeh, B.; Owen, D.A. Handling and Pathology Reporting of Gastrointestinal Endoscopic Mucosal Resection. Middle East J. Dig. Dis. 2017, 9, 5–11. [Google Scholar] [CrossRef]
- Nishizawa, T.; Yahagi, N. Endoscopic mucosal resection and endoscopic submucosal dissection. Curr. Opin. Gastroenterol. 2017, 33, 315–319. [Google Scholar] [CrossRef]
- Pimentel-Nunes, P.; Libânio, D.; Bastiaansen, B.A.J.; Bhandari, P.; Bisschops, R.; Bourke, M.J.; Esposito, G.; Lemmers, A.; Maselli, R.; Messmann, H.; et al. Endoscopic submucosal dissection for superficial gastrointestinal lesions: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2022. Endoscopy 2022, 54, 591–622. [Google Scholar] [CrossRef]
- Sun, F.; Yuan, P.; Chen, T.; Hu, J. Efficacy and complication of endoscopic submucosal dissection for superficial esophageal carcinoma: A systematic review and meta-analysis. J. Cardiothorac. Surg. 2014, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.-M. Endoscopic submucosal dissection vs endoscopic mucosal resection for superficial esophageal cancer. World J. Gastroenterol. 2014, 20, 5540–5547. [Google Scholar] [CrossRef] [PubMed]
- Draganov, P.V.; Wang, A.Y.; Othman, M.O.; Fukami, N. AGA Institute Clinical Practice Update: Endoscopic Submucosal Dissection in the United States. Clin. Gastroenterol. Hepatol. 2019, 17, 16–25.e1. [Google Scholar] [CrossRef] [PubMed]
- Gurwara, S.; Clayton, S. Esophageal Perforations: An Endoscopic Approach to Management. Curr. Gastroenterol. Rep. 2019, 21, 57. [Google Scholar] [CrossRef]
- Eroğlu, A.; Aydın, Y.; Yılmaz, Ö. Minimally invasive management of esophageal perforation. Turk. J. Thorac. Cardiovasc. Surg. 2018, 26, 496–503. [Google Scholar] [CrossRef]
- Van Munster, S.; Nieuwenhuis, E.; Weusten, B.L.A.M.; Herrero, L.A.; Bogte, A.; Alkhalaf, A.; E Schenk, B.; Schoon, E.J.; Curvers, W.; Koch, A.D.; et al. Long-term outcomes after endoscopic treatment for Barrett’s neoplasia with radiofrequency ablation ± endoscopic resection: Results from the national Dutch database in a 10-year period. Gut 2022, 71, 265–276. [Google Scholar] [CrossRef]
- Kahn, A.; Shaheen, N.J.; Iyer, P.G. Approach to the Post-Ablation Barrett’s Esophagus Patient. Am. J. Gastroenterol. 2020, 115, 823–831. [Google Scholar] [CrossRef]
- Yang, L.S.; Holt, B.A.; Williams, R.; Norris, R.; Tsoi, E.; Cameron, G.; Desmond, P.; Taylor, A.C. Endoscopic features of buried Barrett’s mucosa. Gastrointest. Endosc. 2021, 94, 14–21. [Google Scholar] [CrossRef]
- Konda, V.; Souza, R.F.; Dunbar, K.B.; Mills, J.C.; Kim, D.S.; Odze, R.D.; Spechler, S.J. An Endoscopic and Histologic Study on Healing of Radiofrequency Ablation Wounds in Patients with Barrett’s Esophagus. Am. J. Gastroenterol. 2022, 117, 1583–1592. [Google Scholar] [CrossRef]
- Van Hagen, P.; Hulshof, M.C.C.M.; Van Lanschot, J.J.B.; Steyerberg, E.W.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.L.; Richel, D.J.; Nieuwenhuijzen, G.A.P.; Hospers, G.A.P.; Bonenkamp, J.J.; et al. Preoperative Chemoradiotherapy for Esophageal or Junctional Cancer. N. Engl. J. Med. 2012, 366, 2074–2084. [Google Scholar] [CrossRef] [PubMed]
- Morgan, M.A.; Lewis, W.G.; Casbard, A.; Roberts, S.A.; Adams, R.; Clark, G.W.B.; Havard, T.J.; Crosby, T.D.L. Stage-for-stage comparison of definitive chemoradiotherapy, surgery alone and neoadjuvant chemotherapy for oesophageal carcinoma. Br. J. Surg. 2009, 96, 1300–1307. [Google Scholar] [CrossRef]
- Sun, L.; Zhang, Z.; Xu, J.; Xu, G.; Liu, X. Dietary fiber intake reduces risk for Barrett’s esophagus and esophageal cancer. Crit. Rev. Food Sci. Nutr. 2017, 57, 2749–2757. [Google Scholar] [CrossRef] [PubMed]
- Coleman, H.G.; Murray, L.J.; Hicks, B.; Bhat, S.K.; Kubo, A.; Corley, D.A.; Cardwell, C.; Cantwell, M.M. Dietary fiber and the risk of precancerous lesions and cancer of the esophagus: A systematic review and meta-analysis. Nutr. Rev. 2013, 71, 474–482. [Google Scholar] [CrossRef] [PubMed]
- McFadden, D.W.; Riggs, D.R.; Jackson, B.J.; Cunningham, C. Corn-derived carbohydrate inositol hexaphosphate inhibits Barrett’s adenocarcinoma growth by pro-apoptotic mechanisms. Oncol. Rep. 2008, 19, 563–566. [Google Scholar] [CrossRef]
- Morozov, S.; Isakov, V.; Konovalova, M. Fiber-enriched diet helps to control symptoms and improves esophageal motility in patients with non-erosive gastroesophageal reflux disease. World J. Gastroenterol. 2018, 24, 2291–2299. [Google Scholar] [CrossRef]
- Zhao, Z.; Yin, Z.; Zhang, C. Lifestyle interventions can reduce the risk of Barrett’s esophagus: A systematic review and meta-analysis of 62 studies involving 250,157 participants. Cancer Med. 2021, 10, 5297–5320. [Google Scholar] [CrossRef]
- Jarosz, M.; Taraszewska, A. Risk factors for gastroesophageal reflux disease—the role of diet. Gastroenterol. Rev. 2014, 5, 297–301. [Google Scholar] [CrossRef]
- Zhao, Z.; Pu, Z.; Yin, Z.; Yu, P.; Hao, Y.; Wang, Q.; Guo, M.; Zhao, Q. Dietary fruit, vegetable, fat and red and processed meat intakes and Barrett’s esophagus risk: A systematic review and meta-analysis. Sci. Rep. 2016, 6, 27334. [Google Scholar] [CrossRef]
- Brandt, P.A.V.D. The impact of a healthy lifestyle on the risk of esophageal and gastric cancer subtypes. Eur. J. Epidemiol. 2022, 37, 931–945. [Google Scholar] [CrossRef]
- Li, W.; Park, Y.; Wu, J.W.; Ren, J.; Goldstein, A.M.; Taylor, P.R.; Hollenbeck, A.R.; Freedman, N.D.; Abnet, C. Index-based Dietary Patterns and Risk of Esophageal and Gastric Cancer in a Large Cohort Study. Clin. Gastroenterol. Hepatol. 2013, 11, 1130–1136.e2. [Google Scholar] [CrossRef] [PubMed]
- Schulpen, M.; Peeters, P.H.; Brandt, P.A.V.D. Mediterranean diet adherence and risk of esophageal and gastric cancer subtypes in the Netherlands Cohort Study. Gastric Cancer 2019, 22, 663–674. [Google Scholar] [CrossRef]
- Balasubramanian, G.; Gupta, N.; Giacchino, M.; Singh, M.; Kanakadandi, V.; Gaddam, S.; Wani, S.B.; Higbee, A.D.; Rastogi, A.; Bansal, A.; et al. Cigarette smoking is a modifiable risk factor for Barrett’s oesophagus. United Eur. Gastroenterol. J. 2013, 1, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Thrift, A.P.; Cook, M.B.; Vaughan, T.L.; Anderson, L.; Murray, L.J.; Whiteman, D.; Shaheen, N.J.; A Corley, D. Alcohol and the Risk of Barrett’s Esophagus: A Pooled Analysis from the International BEACON Consortium. Am. J. Gastroenterol. 2014, 109, 1586–1594. [Google Scholar] [CrossRef]
- Xu, Q.; Guo, W.; Shi, X.; Zhang, W.; Zhang, T.; Wu, C.; Lu, J.; Wang, R.; Zhao, Y.; Ma, X.; et al. Association Between Alcohol Consumption and the Risk of Barrett’s Esophagus. Medicine 2015, 94, e1244. [Google Scholar] [CrossRef]
- Lou, Z.; Xing, H.; Li, D. Alcohol Consumption and the Neoplastic Progression in Barrett’s Esophagus: A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e105612. [Google Scholar] [CrossRef]
- Chen, Y.; Sun, C.; Wu, Y.; Chen, X.; Kailas, S.; Karadsheh, Z.; Li, G.; Guo, Z.; Yang, H.; Hu, L.; et al. Do proton pump inhibitors prevent Barrett’s esophagus progression to high-grade dysplasia and esophageal adenocarcinoma? An updated meta-analysis. J. Cancer Res. Clin. Oncol. 2021, 147, 2681–2691. [Google Scholar] [CrossRef]
- Jankowski, J.A.Z.; de Caestecker, J.; Love, S.B.; Reilly, G.; Watson, P.; Sanders, S.; Ang, Y.; Morris, D.; Bhandari, P.; Brooks, C.; et al. Esomeprazole and aspirin in Barrett’s oesophagus (AspECT): A randomised factorial trial. Lancet 2018, 392, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Targownik, L.E.; Fisher, D.A.; Saini, S.D. AGA Clinical Practice Update on De-Prescribing of Proton Pump Inhibitors: Expert Review. Gastroenterology 2022, 162, 1334–1342. [Google Scholar] [CrossRef]
- Singh, S.; Garg, S.K.; Singh, P.P.; Iyer, P.G.; El-Serag, H.B. Acid-suppressive medications and risk of oesophageal adenocarcinoma in patients with Barrett’s oesophagus: A systematic review and meta-analysis. Gut 2014, 63, 1229–1237. [Google Scholar] [CrossRef]
- Rayner, C.J.; Gatenby, P. Effect of antireflux surgery for Barrett’s esophagus: Long-term results. Minerva Chir. 2016, 71, 180–191. [Google Scholar] [PubMed]
- Gatenby, P.A.C.; Ramus, J.R.; Caygill, C.P.J.; Charlett, A.; Winslet, M.C.; Watson, A. Treatment modality and risk of development of dysplasia and adenocarcinoma in columnar-lined esophagus. Dis. Esophagus 2009, 22, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.L.; Zhao, W.K.; Corley, D.A. Aspirin and Nonsteroidal Anti-Inflammatory Drug Use and the Risk of Barrett’s Esophagus. Dig. Dis. Sci. 2015, 60, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wu, H.; Wang, R. Effect of nonsteroidal anti-inflammatory drugs on Barrett’s esophagus risk: A systematic review and meta-analysis. Clin. Res. Hepatol. Gastroenterol. 2021, 45, 101552. [Google Scholar] [CrossRef]
- Wang, F.; Lv, Z.S.; Fu, Y.K. Nonsteroidal anti-inflammatory drugs and esophageal inflammation—Barrett’s esophagus—adenocarcinoma sequence: A meta-analysis. Dis. Esophagus 2011, 24, 318–324. [Google Scholar] [CrossRef]
- Thrift, A.P.; Anderson, L.; Murray, L.J.; Cook, M.B.; Shaheen, N.J.; Rubenstein, J.H.; El-Serag, H.B.; Vaughan, T.L.; Schneider, J.L.; Whiteman, D.; et al. Nonsteroidal Anti-Inflammatory Drug Use is Not Associated with Reduced Risk of Barrett’s Esophagus. Am. J. Gastroenterol. 2016, 111, 1528–1535. [Google Scholar] [CrossRef]
- Khalaf, N.; Nguyen, T.; Ramsey, D.; El–Serag, H.B. Nonsteroidal Anti-inflammatory Drugs and the Risk of Barrett’s Esophagus. Clin. Gastroenterol. Hepatol. 2014, 12, 1832–1839.e6. [Google Scholar] [CrossRef]
- Greer, K.B.; Kresak, A.; Bednarchik, B.; Dawson, D.W.; Li, L.; Chak, A.; Willis, J. Insulin/Insulin-Like Growth Factor-1 Pathway in Barrett’s Carcinogenesis. Clin. Transl. Gastroenterol. 2013, 4, e31. [Google Scholar] [CrossRef]
- Trowbridge, R.; Mittal, S.K.; Sharma, P.; Hunter, W.J.; Agrawal, D.K. Vitamin D receptor expression in the mucosal tissue at the gastroesophageal junction. Exp. Mol. Pathol. 2012, 93, 246–249. [Google Scholar] [CrossRef]
- Deeb, K.K.; Trump, D.L.; Johnson, C.S. Vitamin D signalling pathways in cancer: Potential for anticancer therapeutics. Nat. Rev. Cancer 2007, 7, 684–700. [Google Scholar] [CrossRef]
- Carlberg, C.; Muñoz, A. An update on vitamin D signaling and cancer. Semin. Cancer Biol. 2022, 79, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Rouphael, C.; Kamal, A.; Sanaka, M.R.; Thota, P.N. Vitamin D in esophageal cancer: Is there a role for chemoprevention? World J. Gastrointest. Oncol. 2018, 10, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Gharahkhani, P.; Chow, W.-H.; Gammon, M.D.; Liu, G.; Caldas, C.; Wu, A.H.; Ye, W.; Onstad, L.; Anderson, L.A.; et al. No Association Between Vitamin D Status and Risk of Barrett’s Esophagus or Esophageal Adenocarcinoma: A Mendelian Randomization Study. Clin. Gastroenterol. Hepatol. 2019, 17, 2227–2235.e1. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Agoston, A.T.; Pham, T.H.; Zhang, W.; Zhang, X.; Huo, X.; Peng, S.; Bajpai, M.; Das, K.; Odze, R.D.; et al. Acidic Bile Salts Induce Epithelial to Mesenchymal Transition via VEGF Signaling in Non-Neoplastic Barrett’s Cells. Gastroenterology 2019, 156, 130–144.e10. [Google Scholar] [CrossRef]
| Risk Factor | Mentioned in |
|---|---|
| Male sex | [13,14,15] |
| White race | [13,14,15] |
| History of smoking | [13,16,17,18] |
| Chronic GERD | [13,16,19] |
| Obesity | [13,16,20,21,22] |
| Family history of BE/EAC | [13,23,24] |
| Age > 50 | [13,25] |
| Alcohol consumption | [27] |
| History of DM and oral non-metformin Anti-diabetic medications | [28] |
| Association | Criteria | Risk Factors |
|---|---|---|
| AGA [13] | ≥3 risk factors |
|
| ACG [91] | Chronic GERD and ≥3 risk factors |
|
| BSG [33] | Chronic GERD and ≥3 risk factors (the threshold of multiple risk factors should be lowered in the presence at least one first-degree relative with BE or EAC) |
|
| ESGE [52] | Screening for BE is not advised but can be considered in patients with GERD >5 years and multiple risk factors |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mejza, M.; Małecka-Wojciesko, E. Diagnosis and Management of Barrett’s Esophagus. J. Clin. Med. 2023, 12, 2141. https://doi.org/10.3390/jcm12062141
Mejza M, Małecka-Wojciesko E. Diagnosis and Management of Barrett’s Esophagus. Journal of Clinical Medicine. 2023; 12(6):2141. https://doi.org/10.3390/jcm12062141
Chicago/Turabian StyleMejza, Maja, and Ewa Małecka-Wojciesko. 2023. "Diagnosis and Management of Barrett’s Esophagus" Journal of Clinical Medicine 12, no. 6: 2141. https://doi.org/10.3390/jcm12062141
APA StyleMejza, M., & Małecka-Wojciesko, E. (2023). Diagnosis and Management of Barrett’s Esophagus. Journal of Clinical Medicine, 12(6), 2141. https://doi.org/10.3390/jcm12062141






