Analysis of the Efficacy and Risk Factors for Failure of Balloon Dilation for Benign Ureteral Stricture
Abstract
1. Introduction
2. Materials and Methods
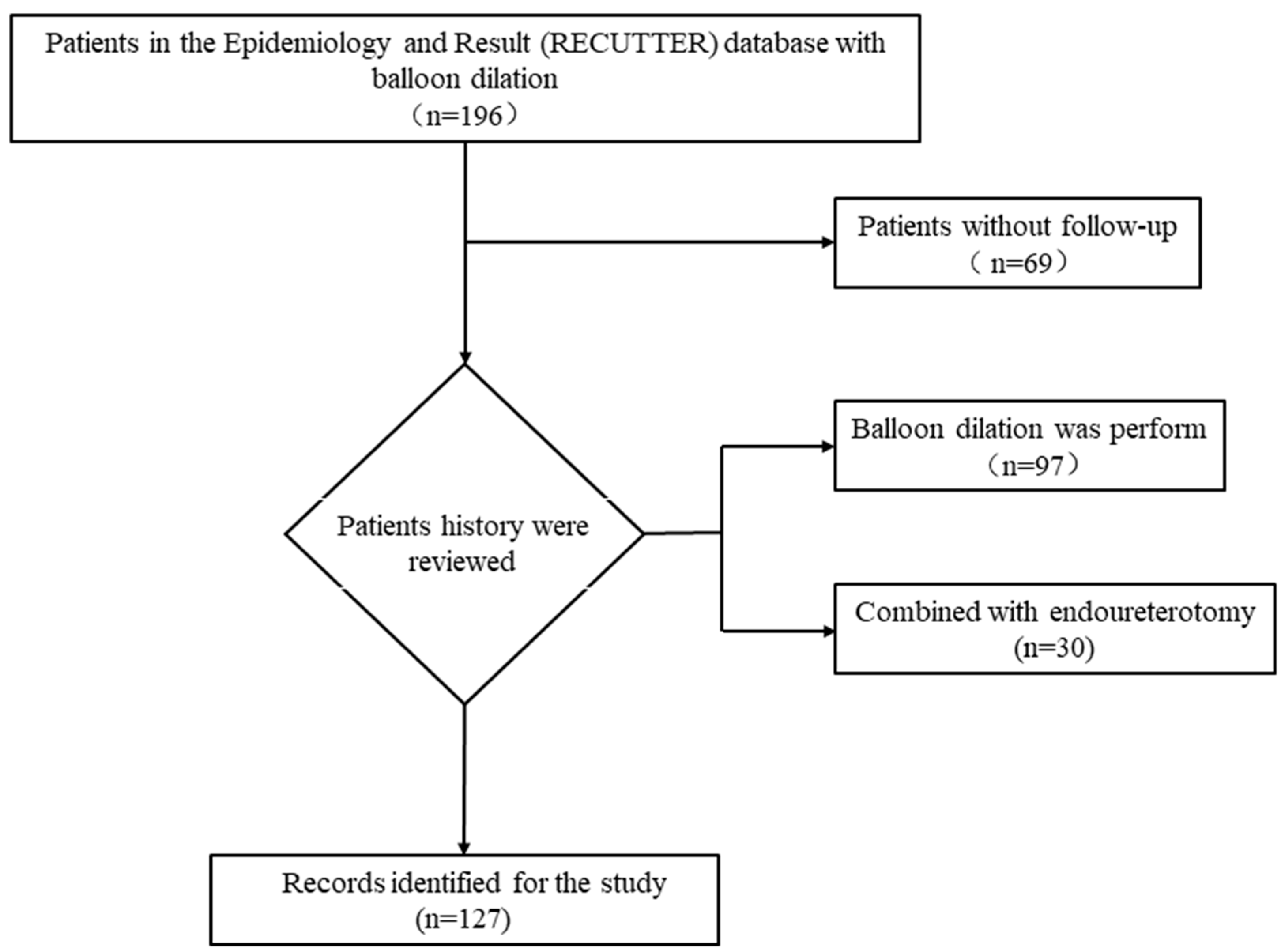
2.1. Study Population
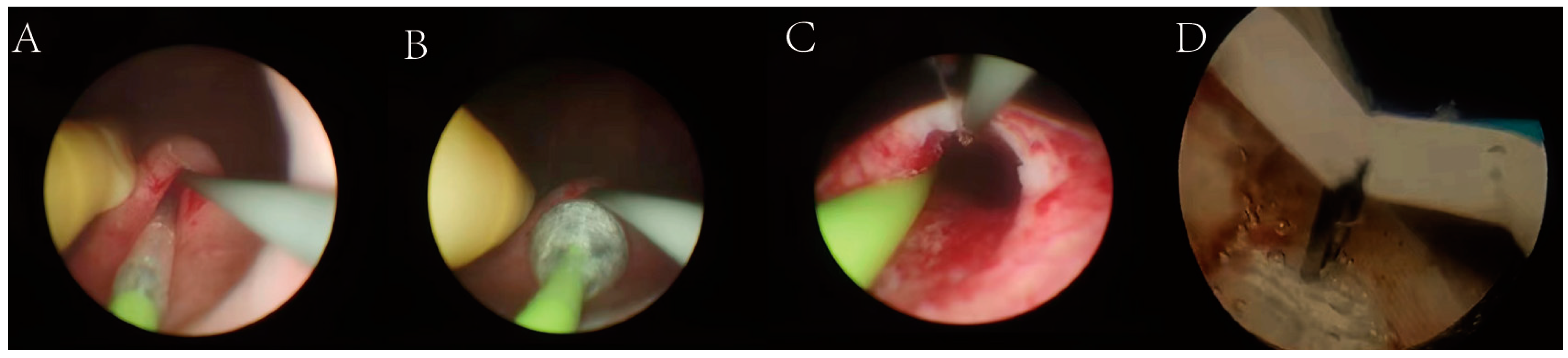
2.2. Operation Methods
2.3. Statistical Analysis
3. Results
- Comparison of 3-month, 6-month, and 1-year outcomes of balloon dilation versus balloon dilation combined with endoureterotomy for lower ureteral stricture.
- 2.
- Comparison of the efficacy of balloon dilatation in the primary treatment and in the secondary treatment.
- 3.
- Analysis of risk factors for failure of balloon dilatation.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tyritzis, S.; Wiklund, N.J. Ureteral strictures revisited…trying to see the light at the end of the tunnel: A comprehensive review. J. Endourol. 2015, 29, 124–136. [Google Scholar] [CrossRef]
- Ganzer, R.; Franz, T.; Rai, B.; Siemer, S.; Stolzenburg, J.-U. Management of ureteral strictures and hydronephrosis. Urologe 2015, 54, 1147–1156. [Google Scholar] [CrossRef]
- Bilotta, A.; Wiegand, L.; Heinsimer, K.J.I.; Heinsimer, K.R. Ureteral reconstruction for complex strictures: A review of the current literature. Int. Urol. Nephrol. 2021, 53, 2211–2219. [Google Scholar] [CrossRef] [PubMed]
- Osther, P.; Geertsen, U.; Nielsen, H.J.J. Ureteropelvic junction obstruction and ureteral strictures treated by simple high-pressure balloon dilation. J. Endourol. 1998, 12, 429–431. [Google Scholar] [CrossRef] [PubMed]
- Meretyk, S.; Albala, D.; Clayman, R.; Denstedt, J.D.; Kavoussi, L.R. Endoureterotomy for treatment of ureteral strictures. J. Urol. 1992, 147, 1502–1506. [Google Scholar] [CrossRef] [PubMed]
- Bhayani, S.; Landman, J.; Slotoroff, C.; Figenshau, R.S. Transplant ureter stricture: Acucise endoureterotomy and balloon dilation are effective. J. Endourol. 2003, 17, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Fontaine, A.; Nijjar, A.; Rangaraj, R.J.J. Update on the use of percutaneous nephrostomy/balloon dilation for the treatment of renal transplant leak/obstruction. J. Vasc. Interv. Radiol. 1997, 8, 649–653. [Google Scholar] [CrossRef]
- Bromwich, E.; Coles, S.; Atchley, J.; Fairley, I.; Langham, J.; Keoghane, S.R. A 4-year review of balloon dilation of ureteral strictures in renal allografts. J. Endourol. 2006, 20, 1060–1061. [Google Scholar] [CrossRef]
- Lu, H.; Zheng, C.; Liang, B.; Xiong, B. Analysis of long-term effect of ureteral balloon dilatation combined with internal and external drainage tube in the treatment of benign ureteral stricture. BMC Urol. 2022, 22, 4. [Google Scholar] [CrossRef]
- Destro, F.; Selvaggio, G.; Marinoni, F.; Pansini, A.; Riccipetitioni, G. High-pressure balloon dilatation in children: Our results in 30 patients with pom and the implications of the cystoscopic evaluation. La Pediatr. Med. E Chir. 2020, 42, 1. [Google Scholar] [CrossRef]
- Ooms, L.; Moelker, A.; Roodnat, J.; Jzermans, J.; Idu, M.; Terkivatan, T. Antegrade balloon dilatation as a treatment option for posttransplant ureteral strictures: Case series of 50 patients. Exp. Clin. Transplant. 2018, 16, 150–155. [Google Scholar] [PubMed]
- Lazarou, G.; Rahimi, S.; Cui, N.; Zormpa, M. Endoscopic balloon dilation in the management of ureteral stricture after urogynecologic surgery: A case report. J. Reprod. Med. 2012, 57, 89–92. [Google Scholar]
- Ravery, V.; de la Taille, A.; Hoffmann, P.; Mouliner, F.; Hermieu, J.F.; Delmas, V.; Boccon-Gibod, L. Balloon catheter dilatation in the treatment of ureteral and ureteroenteric stricture. J. Endourol. 1998, 12, 335–340. [Google Scholar] [CrossRef]
- Capozza, N.; Torino, G.; Nappo, S.; Collura, G.; Mele, E. Primary obstructive megaureter in infants: Our experience with endoscopic balloon dilation and cutting balloon ureterotomy. J. Endourol. 2015, 29, 1–5. [Google Scholar] [CrossRef]
- Collado, A.; Caparrós, J.; Guirado, L.; Rosales, A.; Marti, J.; Sola, R.; Vicente, J. Balloon dilatation in the treatment of ureteral stenosis in kidney transplant recipients. Eur. Endourol. 1998, 34, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Zhang, W.; Peng, Y.; Li, L.; Gao, X.; Liu, M.; Fang, Z. Endoscopic balloon dilatation in the treatment of benign ureteral strictures: A meta-analysis and systematic review. J. Endourol. 2019, 33, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.; Ghiraldi, E.; Ellis, J.; Friedlander, J.I. Endoscopic management of ureteral strictures: An update. Curr. Urol. Rep. 2018, 19, 24. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.; Yin, L.; Yang, K.; Wang, J.; Li, X.; Xiong, S.; Yu, X. Posteriorly augmented anastomotic ureteroplasty with lingual mucosal onlay grafts for long proximal ureteral strictures: 10 cases of experience. J. Endourol. 2021, 35, 192–199. [Google Scholar] [CrossRef]
- Varda, B.K.; Johnson, E.K.; Clark, C.; Chung, B.I.; Nelson, C.P.; Chang, S.L. National trends of perioperative outcomes and costs for open, laparoscopic and robotic pediatric pyeloplasty. J. Urol. 2014, 191, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- Krajewski, W.; Wojciechowska, J.; Dembowski, J.; Zdrojowy, R.; Szydelko, T. Hydronephrosis in the course of ureteropelvic junction obstruction: An underestimated problem? Current opinions on the pathogenesis, diagnosis and treatment. Adv. Clin. Exp. Med. 2017, 26, 857–864. [Google Scholar] [CrossRef]
- Hamid, R.; Bhat, N.A.; Rashid, K.A. Congenital midureteric stricture: Challenges in diagnosis and management. Case Rep. Urol. 2015, 2015, 969246. [Google Scholar] [CrossRef] [PubMed]
- Strother, M.C.; Mucksavage, P. Minimally invasive techniques for the management of adult upj obstruction. Curr. Urol. Rep. 2016, 17, 39. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, W.; Maxted, W.; Pahira, J.J. Ureteral stricture: Experience with 31 cases. J. Urol. 1988, 140, 737–740. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.; Roberts, J.; Grattan-Smith, D.J.U. Retrograde balloon dilation of ureteropelvic obstructions in infants and children: Early results. Urology 1995, 46, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Romero, R.; Angulo, J.; Parente, A.; Rivas, S.; Tardaguila, A.R. Primary obstructive megaureter: The role of high pressure balloon dilation. J. Endourol. 2014, 28, 517–523. [Google Scholar] [CrossRef]
- Ortiz, R.; Parente, A.; Perez-Egido, L.; Burgos, L.; Angulo, J.M. Long-term outcomes in primary obstructive megaureter treated by endoscopic balloon dilation. Experience after 100 cases. Front. Pediatr. 2018, 6, 275. [Google Scholar] [CrossRef]
- Grüntzig, A.; Kumpe, D.J.A.A. Technique of percutaneous transluminal angioplasty with the grüntzig ballon catheter. Am. J. Roentgenol. 1979, 132, 547–552. [Google Scholar] [CrossRef]
- Kristo, B.; Phelan, M.; Gritsch, H.; Schulam, P.G. Treatment of renal transplant ureterovesical anastomotic strictures using antegrade balloon dilation with or without holmium:Yag laser endoureterotomy. Urology 2003, 62, 831–834. [Google Scholar] [CrossRef]
- Anastasescu, R.; Merrot, T.; Chaumoître, K.; Panuel, M.; Alessandrini, P. Antegrade percutaneous balloon dilation of ureteral strictures after failed pelviureteric or ureterovesical reimplantation in children. Urology 2011, 77, 1444–1449. [Google Scholar] [CrossRef]
- Huffman, J.; Bagley, D.J.T.J. Balloon dilation of the ureter for ureteroscopy. J. Urol. 1988, 140, 954–956. [Google Scholar] [CrossRef]
- Wolf, J.; Elashry, O.; Clayman, R.J.T.J. Long-term results of endoureterotomy for benign ureteral and ureteroenteric strictures. J. Urol. 1997, 158, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, A.; Smaldone, M.; Ricchiuti, D.; Averch, T.D. Management of benign ureteral strictures in the endoscopic era. J. Endourol. 2009, 23, 1909–1912. [Google Scholar] [CrossRef]
- Richter, F.; Irwin, R.; Watson, R.; Lang, E.K. Endourologic management of benign ureteral strictures with and without compromised vascular supply. Urology 2000, 55, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Li, X.; Li, X.; Zhang, C.; Yang, K.; Xiong, G.; Zhou, L.; Wang, G. Fluoroscopy-free minimally invasive ureteral stricture balloon dilatation: A retrospective safety and efficacy cohort study. Transl. Androl. Urol. 2021, 10, 2962–2969. [Google Scholar] [CrossRef]
- Byun, S.; Kim, J.; Oh, S.; Kim, H.H. Simple retrograde balloon dilation for treatment of ureteral strictures: Etiology-based analysis. Yonsei Med. J. 2003, 44, 273–278. [Google Scholar] [CrossRef]
- Lim, G.; Yu, Y.; Choi, K.; Rhee, S.R.; Park, D.S.; Hong, Y.K. Retrograde balloon dilation as a therapeutic option for post-gynecologic surgery ureteral stricture followed by ureteroureterostomy: A comparative study regarding stricture length. Yeungnam Univ. J. Med. 2018, 35, 179–186. [Google Scholar] [CrossRef] [PubMed]
| Parameter | No. (%) |
|---|---|
| Patients | 127 |
| Mean age (years) | 36.89 ± 14.82 |
| BMI (kg/m2) | 23.31 ± 3.41 |
| Gender | |
| Male | 58 (45.67) |
| Female | 69 (54.33) |
| Treatment methods | |
| Balloon dilatation | 97 (76.38) |
| Balloon dilation combined with endoureterotomy | 30 (23.62) |
| Location of stricture | |
| Upper | 45 (35.43) |
| Middle | 4 (3.15) |
| Lower | 68 (53.55) |
| Multiple stricture | 10 (7.87) |
| Degree of hydronephrosis | |
| NA | 42 (33.07) |
| Mild/moderate | 63 (49.61) |
| Severe | 22 (17.32) |
| Urethral repair surgery | |
| Yes | 32 (25.20) |
| No | 95 (74.80) |
| Preoperative SCr (μmol/L) | 78.79 ± 41.70 |
| Preoperative BUN (mmol/L) | 5.14 ± 2.71 |
| Preoperative eGFR (mL/min) | 100.21 ± 25.58 |
| Length of ureteral stricture (cm) | 1.48 ± 1.19 |
| Balloon circumference (mm) | 24.85 ± 3.36 |
| Balloon pressure (atm) | 25.82 ± 4.31 |
| Dilation time (min) | 3.04 ± 4.31 |
| Variable | Balloon Dilation | Balloon Dilation Combined with Endoureterotomy | p Value |
|---|---|---|---|
| Patients, n (%) | |||
| Non-failure group | 29 (78.38) | 27 (90) | 0.202 |
| Failure group | 8 (21.62) | 3 (10) | |
| Mean age (years) | 40.76 ± 14.77 | 31.27 ± 15.36 | 0.014 |
| BMI (kg/m2) | 22.74 ± 3.10 | 21.89 ± 3.54 | 0.324 |
| Gender, n (%) | 0.505 | ||
| Male | 14 (37.84) | 9 (30) | |
| Female | 23 (62.16) | 21 (70) | |
| Degree of hydronephrosis | 0.645 | ||
| NA | 9 (24.32) | 13 (43.33) | |
| Mild/moderate | 23 (62.16) | 13 (43.33) | |
| Severe | 5 (13.52) | 4 (13.34) | |
| Preoperative SCr (μmol/L) | 91.20 ± 70.76 | 69.87 ± 12.38 | 0.113 |
| Preoperative BUN (mmol/L) | 6.14 ± 6.63 | 4.78 ± 1.14 | 0.140 |
| Preoperative eGFR (mL/min) | 91.65 ± 29.88 | 105.69 ± 17.08 | 0.089 |
| Length of ureteral stricture (cm) | 1.29 ± 0.57 | 1.86 ± 1.04 | 0.027 |
| Balloon circumference (mm) | 24.21 ± 3.14 | 24.46 ± 3.14 | 0.767 |
| Balloon pressure (atm) | 26.65 ± 4.25 | 25.91 ± 4.23 | 0.537 |
| Dilation time (min) | 2.91 ± 0.63 | 2.79 ± 0.94 | 0.5617 |
| Variable | Failure Group | Non-Failure Group | p Value |
|---|---|---|---|
| Patients, n (%) | 21 (21.65) | 76 (78.35) | |
| Mean age (years) | 37.62 ± 13.57 | 37.86 ± 15.23 | 0.949 |
| BMI (kg/m2) | 23.98 ± 2.66 | 23.43 ± 3.26 | 0.497 |
| Gender, n (%) | 0.238 | ||
| Male | 13 (61.9) | 36 (47.37) | |
| Female | 8 (38.1) | 40 (52.63) | |
| Degree of hydronephrosis | 0.696 | ||
| NA | 8 (38.1) | 21 (21.65) | |
| Mild/moderate | 9 (42.86) | 41 (42.27) | |
| Severe | 4 (19.04) | 14 (14.43) | |
| Preoperative SCr (μmol/L) | 74.83 ± 19.83 | 84.40 ± 51.86 | 0.422 |
| Preoperative BUN (mmol/L) | 5.09 ± 1.26 | 5.48 ± 3.46 | 0.616 |
| Preoperative eGFR (mL/min) | 101.30 ± 18.64 | 99.33 ± 29.48 | 0.798 |
| Length of ureteral stricture (cm) | 1.23 ± 0.67 | 1.21 ± 0.53 | |
| Location of stricture | 0.595 | ||
| Upper | 10 (62.5) | 35 (49.3) | |
| Middle | 0 (0) | 4 (5.63) | |
| Lower | 6 (37.5) | 32 (45.07) | |
| Urethral repair surgery | 0.303 | ||
| Yes | 7 (33.33) | 17 (22.37) | |
| No | 14 (66.67) | 59 (77.63) | |
| Multiple stricture | 0.022 | ||
| Presence | 5 (23.81) | 5 (6.58) | |
| Absence | 16 (76.19) | 71 (93.42) | |
| Balloon circumference (mm) | 25.83 ± 3.02 | 24.09 ± 3.02 | 0.032 |
| Balloon pressure (atm) | 27.25 ± 4.19 | 25.20 ± 4.50 | 0.076 |
| Dilation time (min) | 3.1 ± 0.77 | 3.04 ± 0.60 | 0.728 |
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Mean age (years) | 0.999 | 0.967–1.032 | 0.948 | |||
| BMI (kg/m2) | 1.06 | 0.898–1.251 | 0.492 | |||
| Gender, n (%) | 1.806 | 0.671–4.855 | 0.242 | |||
| Degree of hydronephrosis | 1.429 | 0.363–5.627 | 0.61 | |||
| Preoperative SCr (μmol/L) | 0.992 | 0.972–1.012 | 0.422 | |||
| Preoperative BUN (mmol/L) | 0.947 | 0.763–1.175 | 0.619 | |||
| Preoperative eGFR (mL/min) | 1.003 | 0.982–1.024 | 0.795 | |||
| Length of ureteral stricture (cm) | 1.059 | 0.363–3.090 | 0.917 | |||
| Upper stricture | 1.138 | 0.429–3.017 | 0.795 | |||
| Middle/lower stricture | 1.8 | 0.654–4.956 | 0.255 | |||
| Urethral repair surgery | 0.576 | 0.201–1.656 | 0.306 | |||
| Multiple stricture | 0.225 | 0.058–0.872 | 0.031 | 0.143 | 0.023–0.895 | 0.038 |
| Balloon circumference (mm) | 1.193 | 1.008–1.413 | 0.04 | 1.221 | 1.002–1.491 | 0.05 |
| Balloon pressure (ATM) | 1.129 | 0.985–1.294 | 0.082 | 1.145 | 0.972–1.348 | 0.106 |
| Dilation time (min) | 1.148 | 0.533–2.471 | 0.724 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, B.; Gao, W.; Yang, K.; Liu, H.; Han, Y.; Diao, M.; Zuo, C.; Zhang, M.; Diao, Y.; Li, Z.; et al. Analysis of the Efficacy and Risk Factors for Failure of Balloon Dilation for Benign Ureteral Stricture. J. Clin. Med. 2023, 12, 1655. https://doi.org/10.3390/jcm12041655
Wang B, Gao W, Yang K, Liu H, Han Y, Diao M, Zuo C, Zhang M, Diao Y, Li Z, et al. Analysis of the Efficacy and Risk Factors for Failure of Balloon Dilation for Benign Ureteral Stricture. Journal of Clinical Medicine. 2023; 12(4):1655. https://doi.org/10.3390/jcm12041655
Chicago/Turabian StyleWang, Bing, Wenzhi Gao, Kunlin Yang, Honglei Liu, Yangjun Han, Mingxin Diao, Chao Zuo, Minghua Zhang, Yingzhi Diao, Zhihua Li, and et al. 2023. "Analysis of the Efficacy and Risk Factors for Failure of Balloon Dilation for Benign Ureteral Stricture" Journal of Clinical Medicine 12, no. 4: 1655. https://doi.org/10.3390/jcm12041655
APA StyleWang, B., Gao, W., Yang, K., Liu, H., Han, Y., Diao, M., Zuo, C., Zhang, M., Diao, Y., Li, Z., Li, X., Wang, G., Zhang, P., Wang, C., Xiao, C., Huang, C., Gu, Y., & Li, X. (2023). Analysis of the Efficacy and Risk Factors for Failure of Balloon Dilation for Benign Ureteral Stricture. Journal of Clinical Medicine, 12(4), 1655. https://doi.org/10.3390/jcm12041655





