Clinical Significance and Outcome in Patients with Asymptomatic Versus Symptomatic Subsegmental Pulmonary Embolism
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Inclusion Criteria
2.3. Study Design
2.4. Treatment and Follow-Up
2.5. Study Variables
2.6. Statistical Analysis
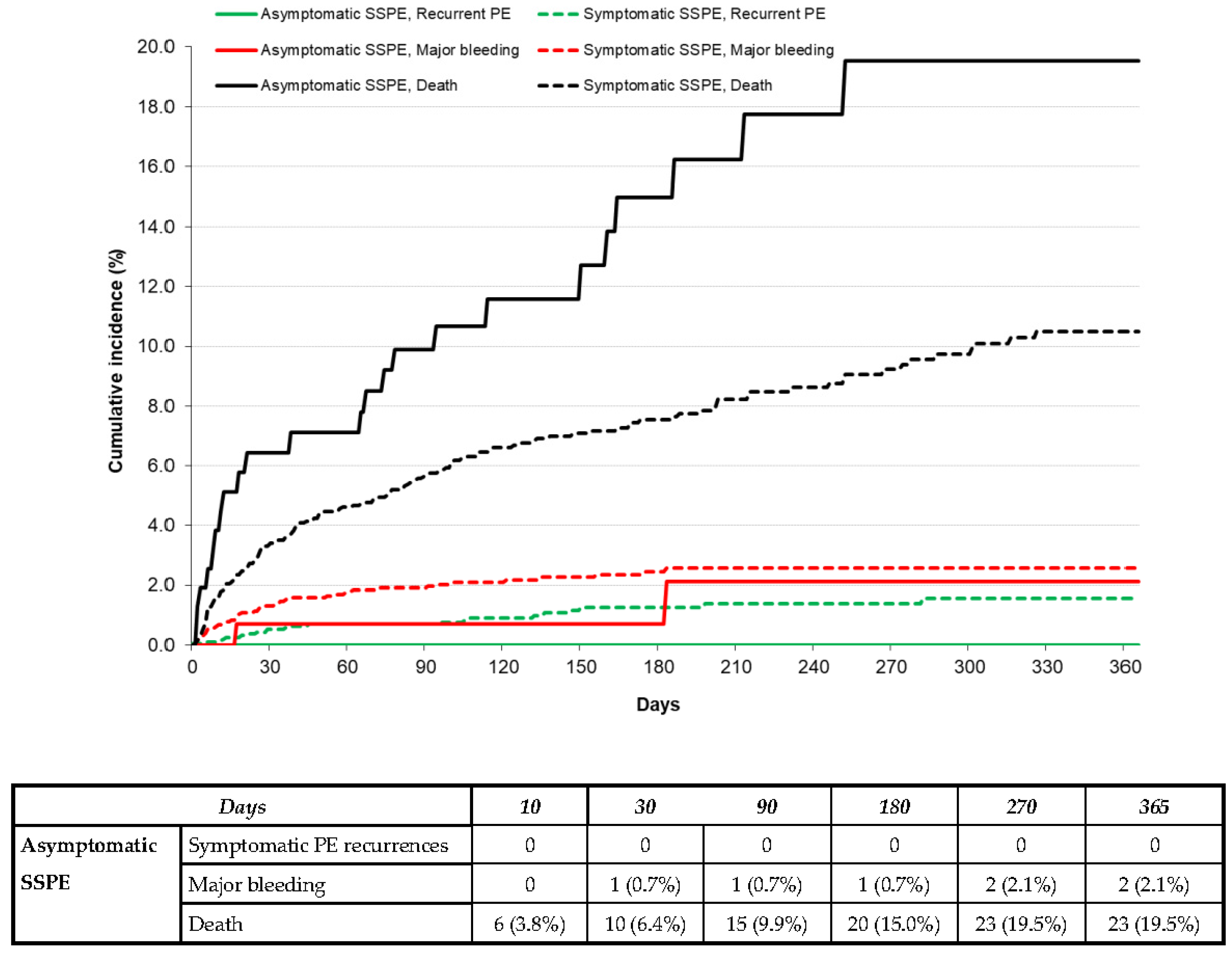
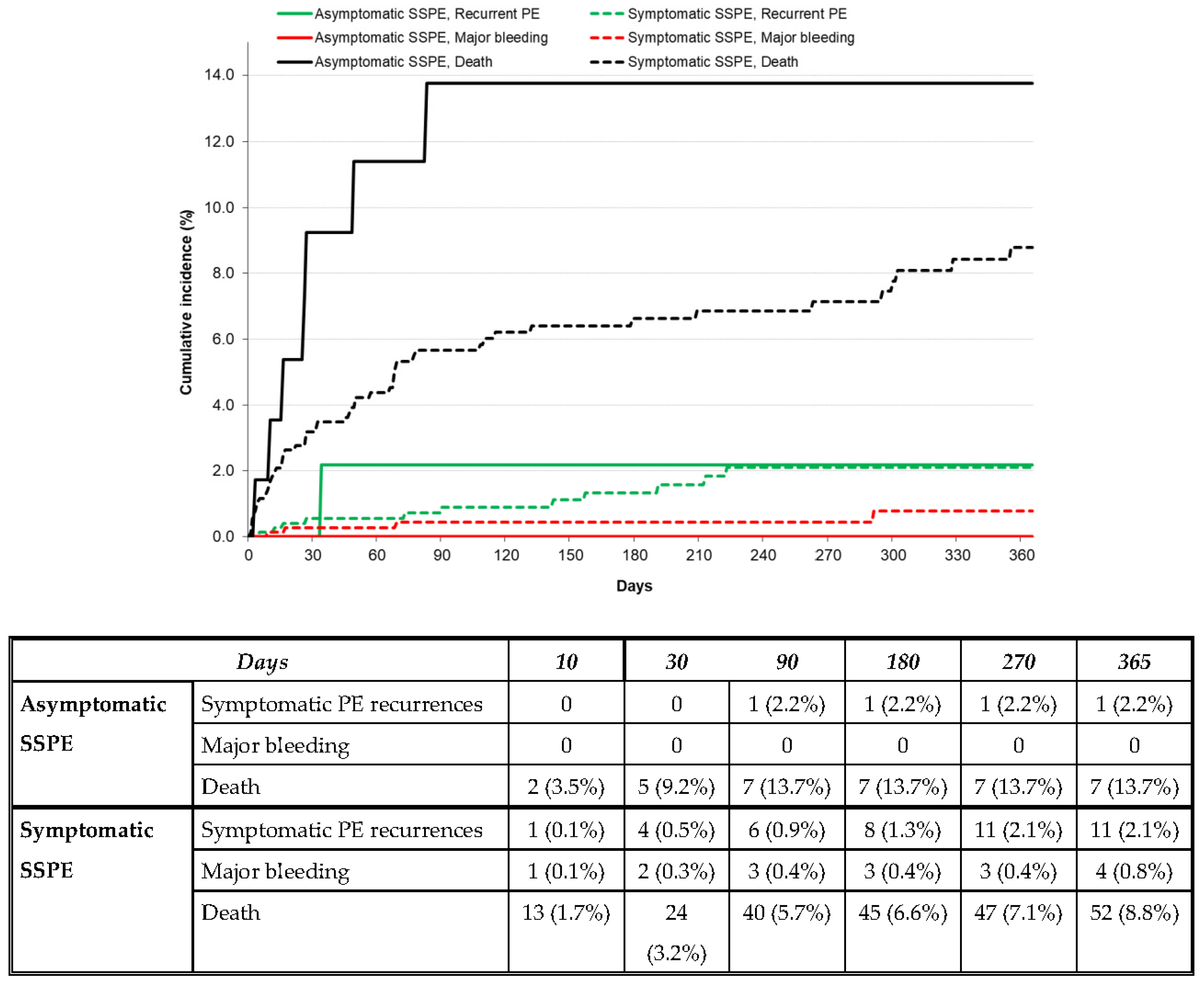
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Wiener, R.S.; Schwartz, L.M.; Woloshin, S. Time trends in pulmonary embolism in the United States: Evidence of overdiagnosis. Arch. Intern. Med. 2011, 171, 831–837. [Google Scholar] [CrossRef]
- Stein, P.D.; Goodman, L.R.; Hull, R.D.; Dalen, J.E.; Matta, F. Diagnosis and management of isolated subsegmental pulmonary embolism: Review and assessment of the options. Clin. Appl. Thromb. Hemost. 2012, 18, 20–26. [Google Scholar] [CrossRef]
- Le Gal, G.; Righini, M.; Parent, F.; van Strijen, M.; Couturaud, F. Diagnosis and management of subsegmental pulmonary embolism. J. Thromb. Haemost. 2006, 4, 724–731. [Google Scholar] [CrossRef]
- Carrier, M.; Klok, F.A. Symptomatic subsegmental pulmonary embolism: To treat or not to treat? Hematol. Am. Soc. Hematol. Educ. Program. 2017, 2017, 237–241. [Google Scholar] [CrossRef]
- Carrier, M.; Righini, M.; Wells, P.S.; Perrier, A.; Anderson, D.R.; Rodger, M.A.; Pleasance, S.; Le Gal, G. Subsegmental pulmonary embolism diagnosed by computed tomography: Incidence and clinical implications. A systematic review and meta-analysis of the management outcome studies. J. Thromb. Haemost. 2010, 8, 1716–1722. [Google Scholar] [CrossRef]
- Monreal, M.; Falgá, C.; Valdés, M.; Suárez, C.; Gabriel, F.; Tolosa, C.; Montes, J.; Riete Investigators. Fatal pulmonary embolism and fatal bleeding in cancer patients with venous thromboembolism: Findings from the RIETE registry. J. Thromb. Haemost. 2006, 4, 1950–1956. [Google Scholar] [CrossRef]
- Fernández-Capitán, C.; Rodriguez Cobo, A.; Jiménez, D.; Madridano, O.; Ciammaichella, M.; Usandizaga, E.; Otero, R.; Di Micco, P.; Moustafa, F.; Monreal, M.; et al. Symptomatic subsegmental versus more central pulmonary embolism: Clinical outcomes during anticoagulation. Res. Pract. Thromb. Haemost. 2020, 5, 168–178. [Google Scholar] [CrossRef]
- Nieto, J.A.; Solano, R.; Ruiz-Ribó, M.D.; Ruiz-Gimenez, N.; Prandoni, P.; Kearon, C.; Monreal, M.; Riete Investigators. Fatal bleeding in patients receiving anticoagulant therapy for venous thromboembolism: Findings from the RIETE registry. J. Thromb. Haemost. 2010, 8, 1216–1222. [Google Scholar] [CrossRef]
- Laporte, S.; Mismetti, P.; Décousus, H.; Uresandi, F.; Otero, R.; Lobo, J.L.; Monreal, M.; RIETE Investigators. Clinical predictors for fatal pulmonary embolism in 15,520 patients with venous thromboembolism: Findings from the Registro Informatizado de la Enfermedad TromboEmbolica venosa (RIETE) Registry. Circulation 2008, 117, 1711–1716. [Google Scholar] [CrossRef]
- Bikdeli, B.; Jimenez, D.; Hawkins, M.; Ortíz, S.; Prandoni, P.; Brenner, B.; Decousus, H.; Masoudi, F.A.; Trujillo-Santos, J.; Krumholz, H.M.; et al. Rationale, Design and Methodology of the Computerized Registry of Patients with Venous Thromboembolism (RIETE). Thromb. Haemost. 2018, 118, 214–224. [Google Scholar] [CrossRef]
- Hirao-Try, Y.; Vlazny, D.T.; Meverden, R.; Houghton, D.E.; Casanegra, A.I.; Froehling, D.A.; Hodge, D.O.; Peterson, L.G.; McBane, R.D.; Wysokinski, W.E. Single versus multiple and incidental versus symptomatic subsegmental pulmonary embolism: Clinical characteristics and outcome. J. Thromb. Thrombolysis 2022, 54, 82–90. [Google Scholar] [CrossRef]
- Bariteau, A.; Stewart, L.K.; Emmett, T.W.; Kline, J.A. Systematic Review and Meta-Analysis of Outcomes of Patients with Subsegmental Pulmonary Embolism with and without Anticoagulation Treatment. Acad. Emerg. Med. 2018, 25, 828–835. [Google Scholar] [CrossRef]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef]
- Le Gal, G.; Kovacs, M.J.; Bertoletti, L.; Couturaud, F.; Dennie, C.; Hirsch, A.M.; Huisman, M.V.; Klok, F.A.; Kraaijpoel, N.; Mallick, R.; et al. Risk for Recurrent Venous Thromboembolism in Patients with Subsegmental Pulmonary Embolism Managed without Anticoagulation. Ann. Intern. Med. 2022, 175, 29–35. [Google Scholar] [CrossRef]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jimenez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur. Heart J. 2020, 41, 543–603. [Google Scholar] [CrossRef]
- Yoo, H.H.; Nunes-Nogueira, V.S.; Fortes Villas Boas, P.J. Anticoagulant Treatment for Subsegmental Pulmonary Embolism. Cochrane Vascular Group, Ed.; Cochrane Database Syst. Rev. Internet.. 2020. Available online: http://doi.wiley.com/10.1002/14651858.CD010222.pub4 (accessed on 5 June 2022).
- Pena, E.; Kimpton, M.; Dennie, C.; Peterson, R.; Le Gal, G.; Carrier, M. Difference in interpretation of computed tomography pulmonary angiography diagnosis of subsegmental thrombosis in patients with suspected pulmonary embolism. J. Thromb. Haemost. 2012, 10, 496–498. [Google Scholar] [CrossRef]
- Stein, P.D.; Fowler, S.E.; Goodman, L.R.; Gottschalk, A.; Hales, C.A.; Hull, R.D.; Leeper, K.V., Jr.; Popovich, J., Jr.; Quinn, D.A.; Sos, T.A.; et al. Multidetector computed tomography for acute pulmonary embolism. N. Engl. J. Med. 2006, 354, 2317–2327. [Google Scholar] [CrossRef]
- Hutchinson, B.D.; Navin, P.; Marom, E.M.; Truong, M.T.; Bruzzi, J.F. Overdiagnosis of pulmonary embolism by pulmonary CT angiography. Am. J. Roentgenol. 2015, 205, 271–277. [Google Scholar] [CrossRef]
| Asymptomatic SSPE | Symptomatic SSPE | Odds Ratio (95% CI) | |
|---|---|---|---|
| Patients, N | 160 | 1975 | |
| Demographics, | |||
| Male gender | 83 (52%) | 987 (50%) | 1.08 (0.78–1.49) |
| Age (mean years ± SD) | 68 ± 15 † | 64 ± 17 | p = 0.009 |
| Body weight (mean kg ± SD) | 72 ± 15 * | 76 ± 17 | p = 0.039 |
| Comorbidities, | |||
| Hypertension | 65 (41%) | 871 (44%) | 0.87 (0.62–1.20) |
| Diabetes | 20 (13%) | 294 (16%) | 0.82 (0.50–1.34) |
| Atrial fibrillation | 7 (4.4%) | 105 (5.3%) | 0.81 (0.37–1.78) |
| Chronic lung disease | 18 (11%) | 292 (15%) | 0.73 (0.44–1.21) |
| Chronic heart failure | 8 (5.0%) | 182 (9.2%) | 0.52 (0.25–1.07) |
| Prior myocardial infarction | 6 (3.8%) | 140 (7.1%) | 0.51 (0.22–1.18) |
| Prior ischemic stroke | 15 (9.4%) | 117 (5.9%) | 1.64 (0.94–2.89) |
| Peripheral artery disease | 6 (4.0%) | 67 (3.6%) | 1.12 (0.48–2.62) |
| Recent major bleeding | 8 (5.0%) | 60 (3.0%) | 1.68 (0.79–3.58) |
| Recent COVID-19 infection | 14 (8.8%) | 278 (14.0%) | 0.59 (0.33–1.03) |
| Risk factors for PE, | |||
| Active cancer | 68 (43%) ‡ | 310 (16%) | 3.97 (2.84–5.56) |
| Recent immobilization | 35 (22%) | 478 (24%) | 0.88 (0.59–1.29) |
| Recent surgery | 26 (16%) | 215 (11%) | 1.59 (1.02–2.47) |
| Hormonal use | 5 (3.2%) | 111 (5.8%) | 0.53 (0.21–1.32) |
| Recent travel | 2 (1.3%) | 49 (2.6%) | 0.49 (0.12–2.04) |
| Pregnancy | 1 (0.63%) | 23 (1.2%) | 0.53 (0.07–3.98) |
| None of the above (unprovoked) | 49 (31%) ‡ | 962 (49%) | 0.46 (0.33–0.66) |
| Asymptomatic SSPE | Symptomatic SSPE | Odds Ratio (95% CI) | |
|---|---|---|---|
| Patients, N | 160 | 1975 | |
| Signs/symptoms, | |||
| Dyspnea | 0 ‡ | 1337 (68%) | - |
| Chest pain | 0 ‡ | 796 (40%) | - |
| Syncope | 0 ‡ | 165 (8.4%) | - |
| Hemoptysis | 0 ‡ | 81 (4.1%) | - |
| Lower-limb pain | 0 ‡ | 409 (21%) | - |
| Lower-limb swelling | 0 ‡ | 387 (20%) | - |
| SBP levels < 100 mmHg | 10 (7.0%) | 99 (5.0%) | 1.43 (0.73–2.80) |
| Heart rate > 110 bpm | 16 (11%) | 214 (11%) | 1.00 (0.58–1.71) |
| Blood levels, | |||
| Sat O2 levels < 90% (n = 876) | 7 (13%) | 156 (19%) | 0.64 (0.28–1.43) |
| Positive D-dimer (n = 1491) | 68 (96%) | 1339 (94%) | 1.37 (0.42–4.45) |
| Raised troponin (n = 965) | 15 (32%) | 200 (22%) | 1.68 (0.89–3.17) |
| Lower-limb ultrasound, | |||
| Proximal DVT | 14 (8.8%) | 278 (14%) | 0.59 (0.33–1.03) |
| Distal DVT | 11 (6.9%) | 111 (5.6%) | 1.24 (0.65–2.35) |
| Normal | 37 (23%) | 502 (25%) | 0.88 (0.60–1.29) |
| Not performed | 98 (61%) * | 1042 (53%) | 1.42 (1.02–1.97) |
| Prognostic scoring, | |||
| Simplified PESI < 1 points | 49 (31%) ‡ | 909 (46%) | 0.52 (0.37–0.73) |
| Initial therapy, | |||
| Low-molecular-weight heparin | 133 (83%) | 1640 (83%) | 1.01 (0.65–1.55) |
| Unfractionated heparin | 10 (6.3%) | 82 (4.2%) | 1.54 (0.78–3.03) |
| Fondaparinux | 3 (1.9%) | 27 (1.4%) | 1.38 (0.41–4.59) |
| Direct oral anticoagulants | 5 (3.3%) † | 187 (9.5%) | 0.32 (0.13–0.80) |
| Rivaroxaban | 2 (1.3%) * | 113 (5.7%) | 0.21 (0.05–0.85) |
| Apixaban | 2 (1.3%) | 59 (3%) | 0.41 (0.10–1.70) |
| Thrombolytics | 0 | 2 (0.10%) | - |
| No initial therapy | 5 (3.1%) | 12 (0.6%) | 5.17 (1.84–15.2) |
| Long-term therapy, | |||
| Low-molecular-weight heparin | 83 (52%) ‡ | 549 (28%) | 2.80 (2.02–3.88) |
| Vitamin K antagonists | 33 (21%) ‡ | 753 (38%) | 0.42 (0.28–0.63) |
| Fondaparinux | 0 | 12 (0.61%) | - |
| Direct oral anticoagulants | 31 (21%) * | 585 (31%) | 0.60 (0.40–0.91) |
| Rivaroxaban | 12 (7.5%) † | 299 (15%) | 0.45 (0.25–0.83) |
| Apixaban | 13 (8.1%) | 195 (9.9%) | 0.81 (0.45–1.45) |
| Edoxaban | 5 (3.1%) | 68 (3.4%) | 0.90 (0.36–2.28) |
| Dabigatran | 1 (0.6%) | 23 (1.2%) | 0.53 (0.07–3.98) |
| No long-term therapy | 4 (2.5%) | 18 (0.9%) | 2.78 (0.93–8.34) |
| Asymptomatic SSPE | Symptomatic SSPE | Hazard Ratio (95% CI) | |||
|---|---|---|---|---|---|
| N | Events per 100 Patient Years | N | Events per 100 Patient Years | ||
| During anticoagulation | |||||
| Patients, N | 160 | 1975 | |||
| Duration of therapy, | |||||
| Median days (IQR) | 148 (94–306) | 173 (101–306) | |||
| Mean days ± SD | 240 ± 267 | 277 ± 382 | p = 0.101 | ||
| Outcomes, | |||||
| Recurrent VTE | 3 | 2.98 (0.76–8.10) | 38 | 2.60 (1.86–3.53) | 1.15 (0.28–3.32) |
| Recurrent PE | 2 | 1.98 (0.33–6.55) | 12 | 0.81 (0.44–1.37) | 2.46 (0.37–9.74) |
| Recurrent DVT | 1 | 0.97 (0.05–4.79) | 27 | 1.84 (1.24–2.64) | 0.53 (0.03–2.80) |
| Major bleeding | 3 | 2.91 (0.74–7.93) | 51 | 3.44 (2.59–4.48) | 0.85 (0.21–2.42) |
| Gastrointestinal | 2 | 1.94 (0.33–6.42) | 16 | 1.07 (0.64–1.71) | 1.81 (0.28–6.85) |
| Intracranial | 1 | 0.97 (0.05–4.79) | 9 | 0.60 (0.29–1.10) | 1.61 (0.07–9.82) |
| Death | 24 | 23.3 (15.3–34.1) † | 179 | 12.0 (10.3–13.8) | 1.95 (1.25–2.94) |
| Fatal PE | 0 | - | 6 | 0.40 (0.16–0.83) | - |
| Fatal bleeding | 1 | 0.97 (0.05–4.79) | 11 | 0.74 (0.39–1.28) | 1.32 (0.06–7.73) |
| After discontinuing anticoagulant therapy | |||||
| Patients, N | 58 | 781 | |||
| Duration of therapy, | |||||
| Median days (IQR) | 154 (43–331) | 198 (75–475) | |||
| Mean days ± SD | 287 ± 419 | 367 ± 485 | p = 0.169 | ||
| Outcomes, | |||||
| Recurrent VTE | 2 | 4.38 (0.73–14.5) | 40 | 5.16 (3.74–6.96) | 0.85 (0.14–2.96) |
| Recurrent PE | 2 | 4.38 (0.73–14.48) | 27 | 3.45 (2.32–4.95) | 1.27 (0.20–4.55) |
| Recurrent DVT | 0 | - | 13 | 1.67 (0.93–2.79) | - |
| Major bleeding | 0 | - | 6 | 0.77 (0.31–1.59) | - |
| Gastrointestinal | 0 | - | 4 | 0.51 (0.16–1.23) | - |
| Intracranial | 0 | - | 0 | - | - |
| Death | 8 | 17.5 (8.14–33.3) | 67 | 8.53 (6.66–10.8) | 2.06 (0.92–4.10) |
| Causes of death | |||||
| Fatal PE | 0 | - | 1 | 0.13 (0.01–0.63) | - |
| Fatal bleeding | 0 | - | 5 | 0.64 (0.23–1.41) | - |
| Asymptomatic SSPE | Symptomatic SSPE | Hazard Ratio (95% CI) | |||
|---|---|---|---|---|---|
| N | Events per 100 Patient Years | N | Events per 100 Patient Years | ||
| In patients on LMWH, N | |||||
| Symptomatic PE | 0 | - | 3 | 0.52 (0.13–1.41) | - |
| Symptomatic DVT | 0 | - | 2 | 0.34 (0.06–1.14) | - |
| Major bleeding | 3 | 4.80 (1.22–13.1) | 28 | 4.85 (3.29–6.92) | 0.99 (0.24–2.93) |
| In patients on VKAs, N | |||||
| Symptomatic PE | 1 | 3.18 (0.16–15.7) | 24 | 3.16 (2.07–4.63) | 1.01 (0.05–5.37) |
| Symptomatic DVT | 2 | 6.83 (1.15–22.6) | 10 | 1.29 (0.65–2.29) | 5.31 (0.79–21.8) |
| Major bleeding | 0 | - | 18 | 2.32 (1.42–3.59) | - |
| In patients on DOACs, N | |||||
| Symptomatic PE | 0 | - | 0 | - | - |
| Symptomatic DVT | 0 | - | 0 | - | - |
| Major bleeding | 0 | - | 3 | 2.43 (0.62–6.62) | - |
| In patients on other drugs, N | |||||
| Symptomatic PE | 0 | - | 0 | - | - |
| Symptomatic DVT | 0 | - | 0 | - | - |
| Major bleeding | 0 | - | 2 | 33.0 (5.54–109.2) | - |
| Asymptomatic SSPE | Symptomatic SSPE | |||||||
|---|---|---|---|---|---|---|---|---|
| Confirmed DVT | No DVT | Confirmed DVT | No DVT | |||||
| N | Events per 100 Patient Years | N | Events per 100 Patient Years | N | Events per 100 Patient Years | N | Events per 100 Patient Years | |
| During anticoagulation | ||||||||
| Patients, N | 25 | 37 | 389 | 502 | ||||
| Median days (IQR) | 218 ± 253 | 240 ± 179 | 357 ± 586 | 275 ± 313 | ||||
| Mean days ± SD | 97 (38–257) | 199 (98–342) | 185 (104–349) | 184 (102–345) | ||||
| Outcomes, | ||||||||
| Recurrent VTE | 0 | - | 0 | - | 9 | 2.46 (1.20–4.51) | 9 | 2.41 (1.18–4.43) |
| Recurrent PE | 0 | - | 0 | - | 6 | 1.64 (0.66–3.40) | 8 | 2.14 (1.00–4.07) |
| Recurrent DVT | 0 | - | 0 | - | 4 | 1.05 (0.34–2.54) | 1 | 0.26 (0.01–1.31) |
| Major bleeding | 0 | - | 0 | - | 10 | 2.66 (1.35–4.75) | 12 | 3.20 (1.73–5.44) |
| Gastrointestinal | 0 | - | 0 | - | 4 | 1.06 (0.34–2.55) | 5 | 1.33 (0.49–2.94) |
| Intracranial | 0 | - | 0 | - | 2 | 0.53 (0.09–1.74) | 1 | 0.26 (0.01–1.31) |
| Death | 5 | 33.5 (12.3–74.3) | 2 | 8.46 (1.42–27.9) | 31 | 8.16 (5.64–11.4) | 30 | 7.94 (5.46–11.2) |
| After discontinuing anticoagulant therapy | ||||||||
| Patients, N | 5 | 14 | 119 | 198 | ||||
| Median days (IQR) | 184 ± 72 | 445 ± 627 | 452 ± 582 | 418 ± 533 | ||||
| Mean days ± SD | 199 (130–208) | 162 (58–596) | 206 (65–636) | 243 (88–529) | ||||
| Outcomes, | ||||||||
| Recurrent VTE | 0 | - | 0 | - | 10 | 7.21 (3.66–12.8) | 10 | 4.42 (2.24–7.87) |
| Recurrent PE | 0 | - | 0 | - | 4 | 2.74 (0.87–6.61) | 9 | 3.97 (1.94–7.29) |
| Recurrent DVT | 0 | - | 0 | - | 6 | 4.28 (1.74–8.91) * | 1 | 0.44 (0.02–2.18) * |
| Major bleeding | 0 | - | 0 | - | 0 | - | 1 | 0.44 (0.02–2.19) |
| Death | 0 | - | 1 | 5.86 (0.29–28.9) | 11 | 7.47 (3.93–13.0) | 18 | 7.94 (4.85–12.3) |
| Symptomatic PE Recurrences | Death | |||
|---|---|---|---|---|
| Univariable | Multivariable | Univariable | Multivariable | |
| Patients, N | ||||
| Demographics, | ||||
| Male gender | 1.18 (0.70–1.98) | - | 1.36 (1.06–1.76) * | 0.67 (0.52–0.87) † |
| Age >70 years | 0.68 (0.39–1.17) | - | 2.47 (1.90–3.19) ‡ | 1.81 (1.38–2.37) ‡ |
| Body weight >75 kg | 1.71 (1.01–2.89) * | 1.77 (1.05–2.98) * | 0.49 (0.38–0.65) ‡ | 0.59 (0.45–0.77) ‡ |
| Comorbidities, | ||||
| Hypertension | 1.35 (0.74–0.81) | - | 1.33 (1.03–1.71) * | 0.82 (0.62–1.07) |
| Diabetes | 1.54 (0.81–2.93) | - | 2.01 (1.47–2.74) ‡ | 1.63 (1.20–2.20) † |
| Atrial fibrillation | 1.20 (0.43–3.32) | - | 2.62 (1.69–4.06) ‡ | 1.90 (1.26–2.87) † |
| Chronic lung disease | 1.32 (0.70–2.52) | - | 2.16 (1.59–2.93) ‡ | 1.16 (0.86–1.57) |
| Chronic heart failure | 0.61 (0.22–1.70) | - | 2.20 (1.53–3.17) ‡ | 1.83 (1.26–2.66) † |
| Prior myocardial infarction | 0.41 (0.10–1.67) | - | 2.17 (1.45–3.26) ‡ | 1.42 (0.96–2.11) |
| Prior ischemic stroke | 1.50 (0.60–3.75) | - | 2.50 (1.66–3.78) ‡ | 1.47 (0.99–2.18) |
| Peripheral artery disease | 0.52 (0.07–3.81) | - | 2.28 (1.32–3.94) † | 1.36 (0.81–2.28) |
| Recent major bleeding | 1.32 (0.32–5.48) | - | 1.61 (0.87–2.98) | - |
| Risk factors for SSPE, | ||||
| Unprovoked | Ref. | Ref. | Ref. | Ref. |
| Transient risk factors | 0.70 (0.38–1.20) | - | 1.90 (1.32–2.74) † | 2.15 (1.48–3.13) ‡ |
| Active cancer | 1.70 (0.95–3.03) | 1.94 (1.08–3.50) * | 12.2 (8.72–17.2) † | 10.9 (7.77–15.2) ‡ |
| Initial SSPE presentation, | ||||
| Asymptomatic SSPE | 0.77 (0.25–2.37) | 0.70 (0.22–2.24) | 1.83 (1.22–2.75) † | 1.07 (0.73–1.56) |
| Use of anticoagulant therapy, | ||||
| Off anticoagulation | 1.69 (1.01–2.81) * | 1.77 (1.07–2.91) * | 0.54 (0.41–0.72) † | 0.50 (0.38–0.66) ‡ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Cobo, A.; Fernández-Capitán, C.; Tung-Chen, Y.; Salgueiro-Origlia, G.; Ballaz, A.; Bortoluzzi, C.; Sarlon-Bartoli, G.; Pesce, M.L.; Najib, D.; Monreal, M.; et al. Clinical Significance and Outcome in Patients with Asymptomatic Versus Symptomatic Subsegmental Pulmonary Embolism. J. Clin. Med. 2023, 12, 1640. https://doi.org/10.3390/jcm12041640
Rodríguez-Cobo A, Fernández-Capitán C, Tung-Chen Y, Salgueiro-Origlia G, Ballaz A, Bortoluzzi C, Sarlon-Bartoli G, Pesce ML, Najib D, Monreal M, et al. Clinical Significance and Outcome in Patients with Asymptomatic Versus Symptomatic Subsegmental Pulmonary Embolism. Journal of Clinical Medicine. 2023; 12(4):1640. https://doi.org/10.3390/jcm12041640
Chicago/Turabian StyleRodríguez-Cobo, Ana, Carmen Fernández-Capitán, Yale Tung-Chen, Giorgina Salgueiro-Origlia, Aitor Ballaz, Cristiano Bortoluzzi, Gabrielle Sarlon-Bartoli, Maria Lourdes Pesce, Dally Najib, Manuel Monreal, and et al. 2023. "Clinical Significance and Outcome in Patients with Asymptomatic Versus Symptomatic Subsegmental Pulmonary Embolism" Journal of Clinical Medicine 12, no. 4: 1640. https://doi.org/10.3390/jcm12041640
APA StyleRodríguez-Cobo, A., Fernández-Capitán, C., Tung-Chen, Y., Salgueiro-Origlia, G., Ballaz, A., Bortoluzzi, C., Sarlon-Bartoli, G., Pesce, M. L., Najib, D., Monreal, M., & The RIETE Investigators. (2023). Clinical Significance and Outcome in Patients with Asymptomatic Versus Symptomatic Subsegmental Pulmonary Embolism. Journal of Clinical Medicine, 12(4), 1640. https://doi.org/10.3390/jcm12041640







