Single-Stage Externalized Locked Plating for Treatment of Unstable Meta-Diaphyseal Tibial Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
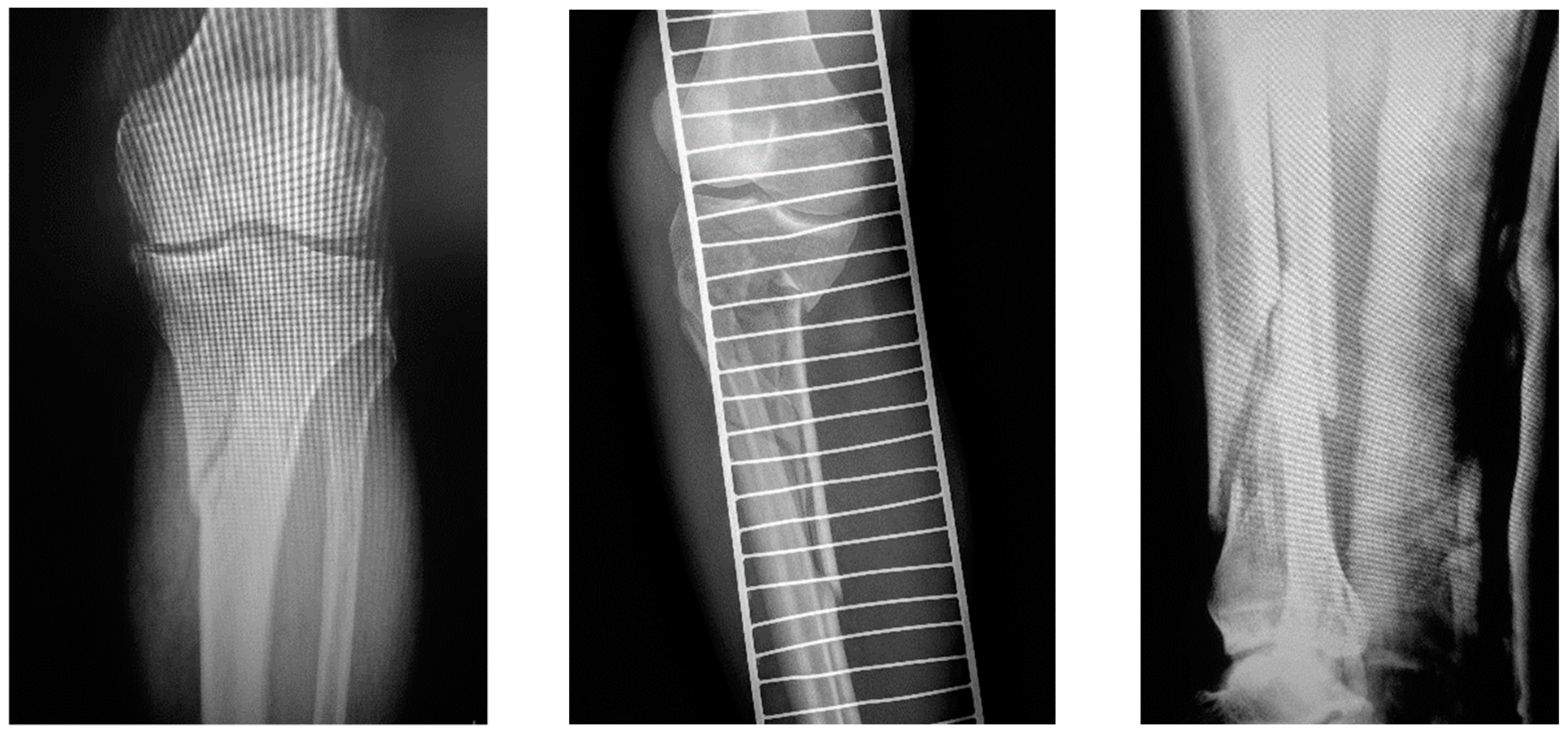
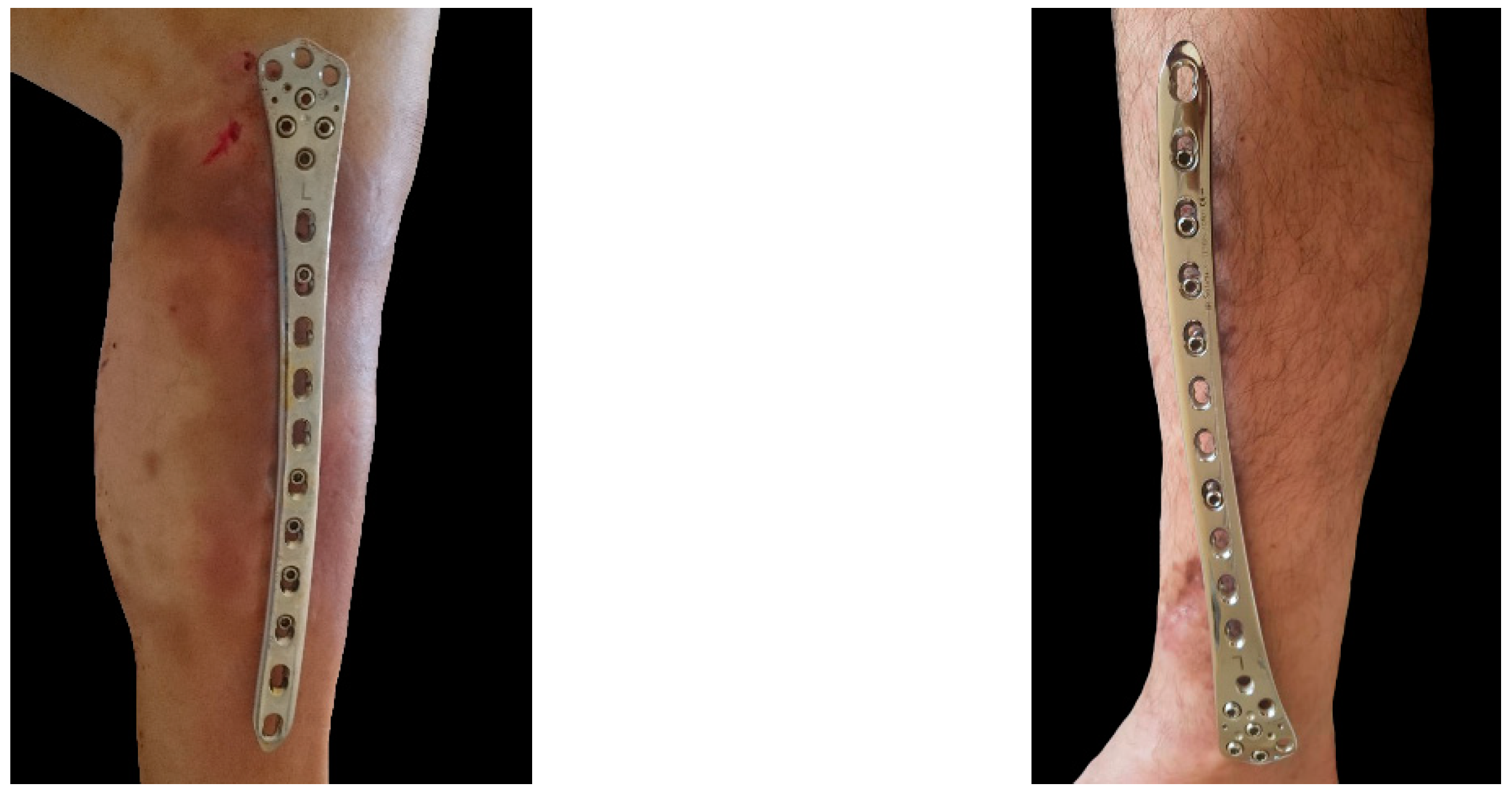
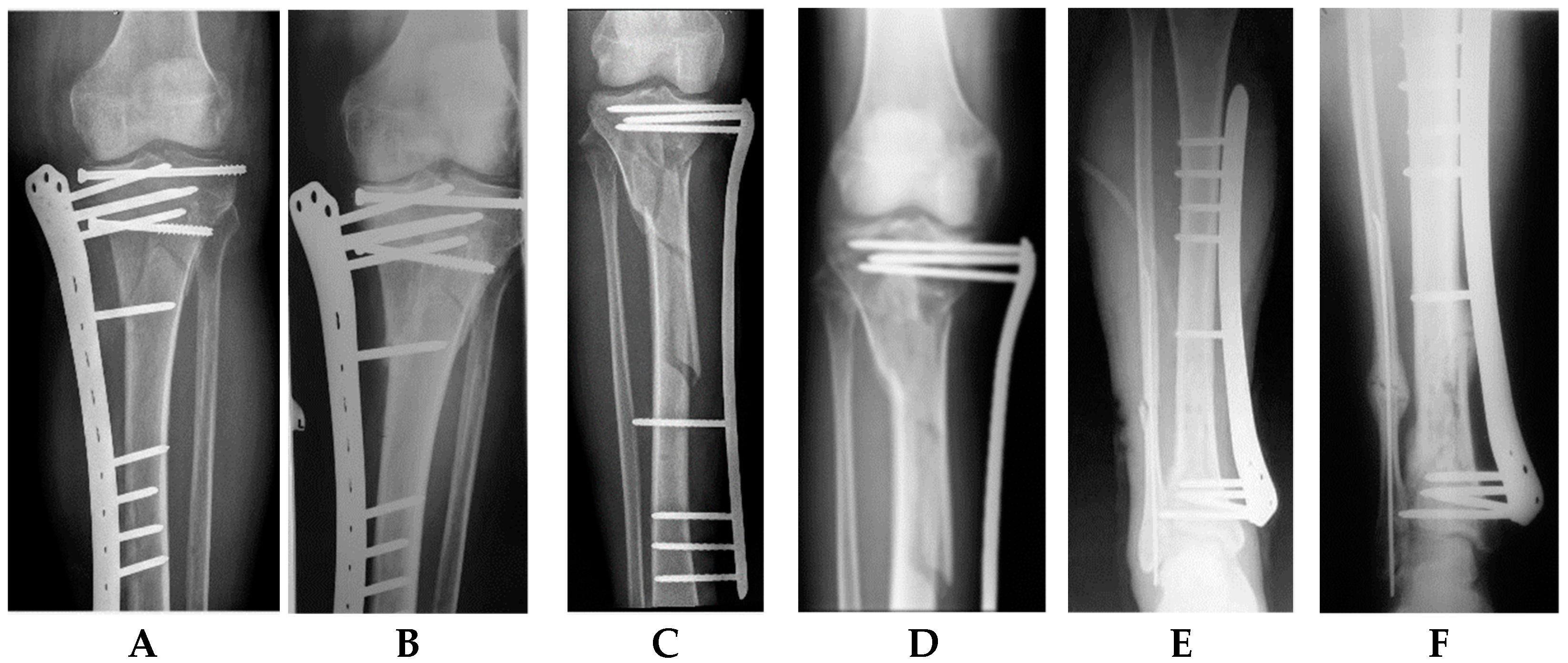
2.2. Surgical Technique
2.2.1. Patient Positioning
2.2.2. Articular Joint Surface Reduction
2.2.3. Single-Stage Externalized Locked Plating
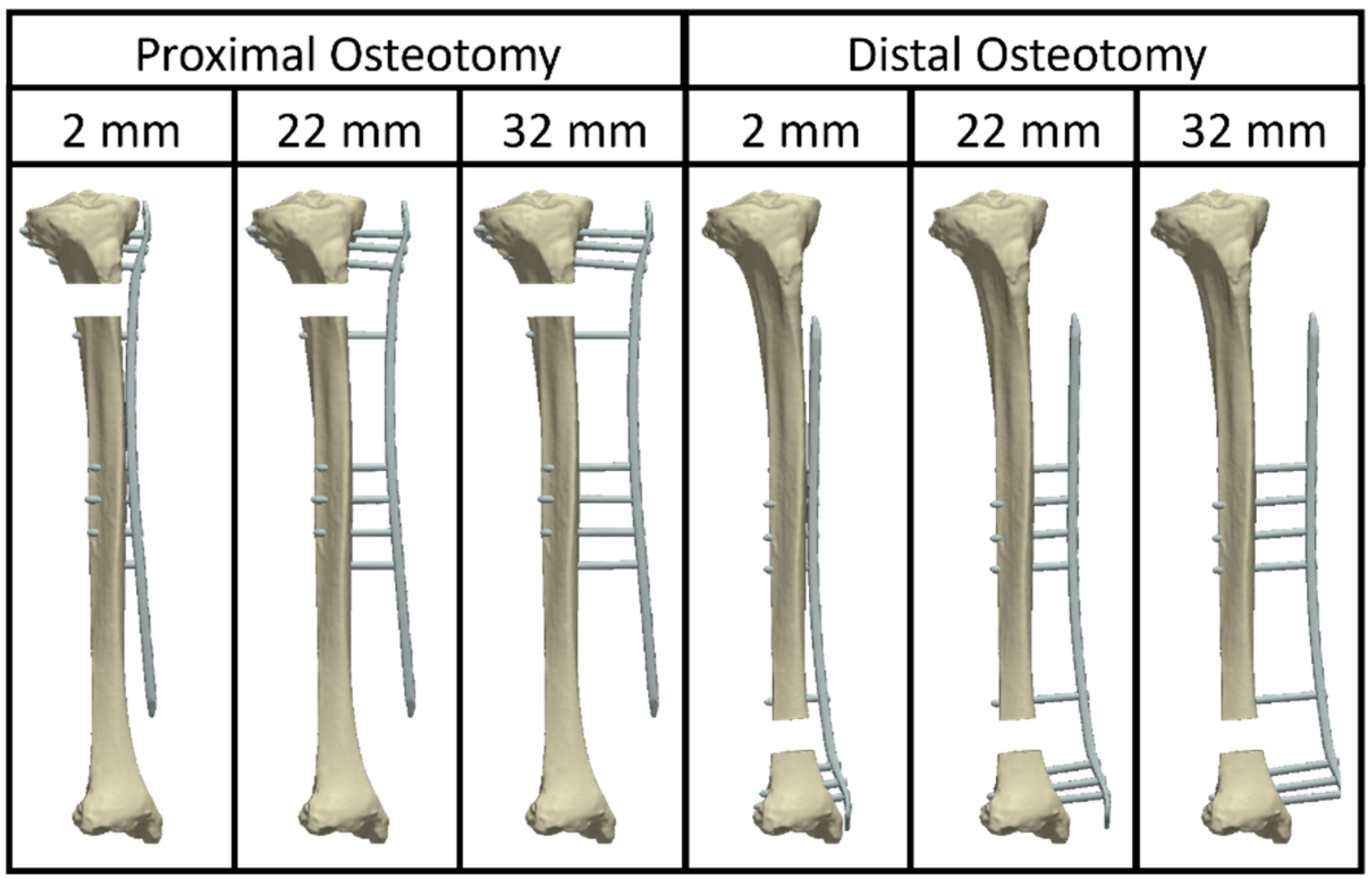
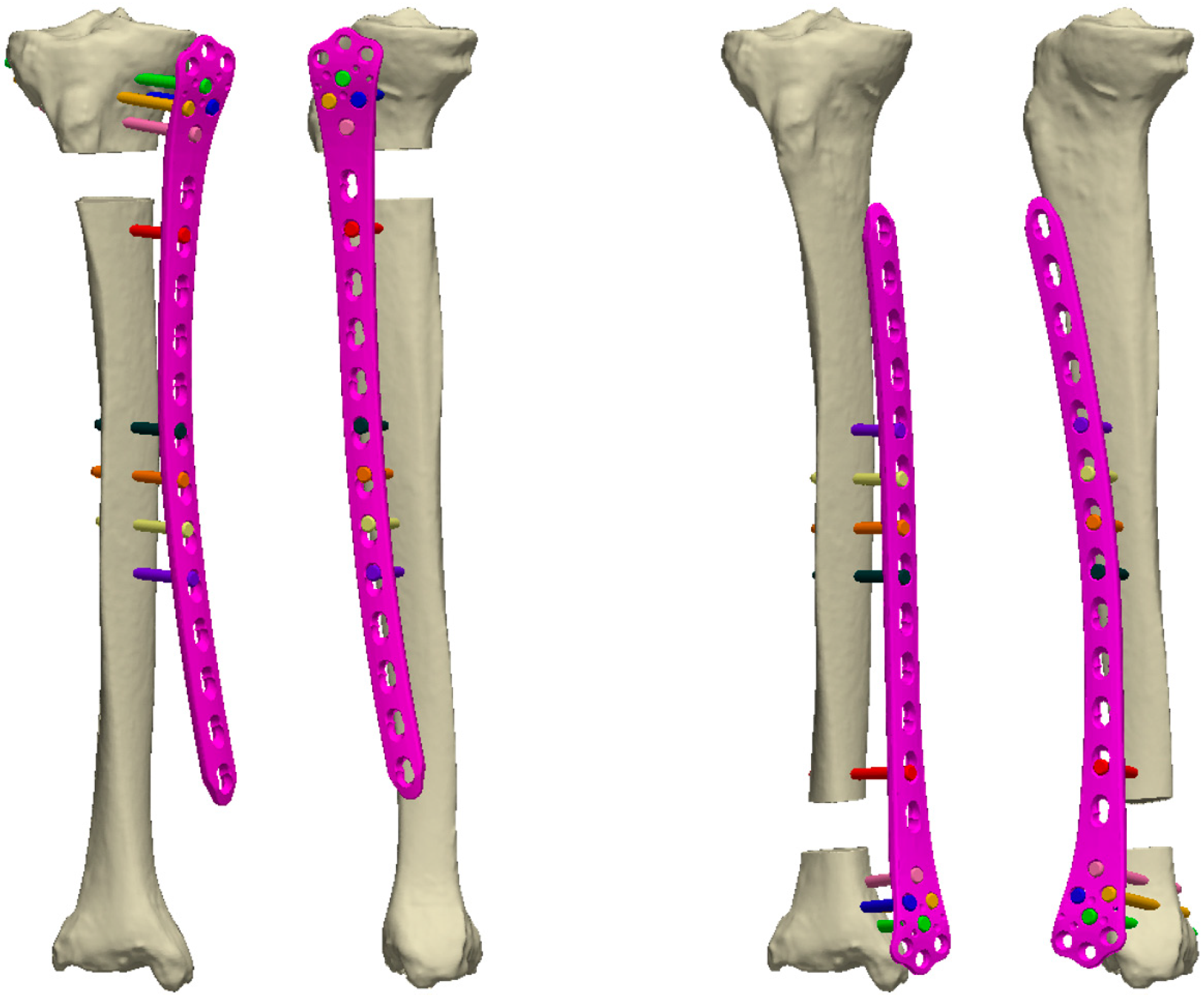
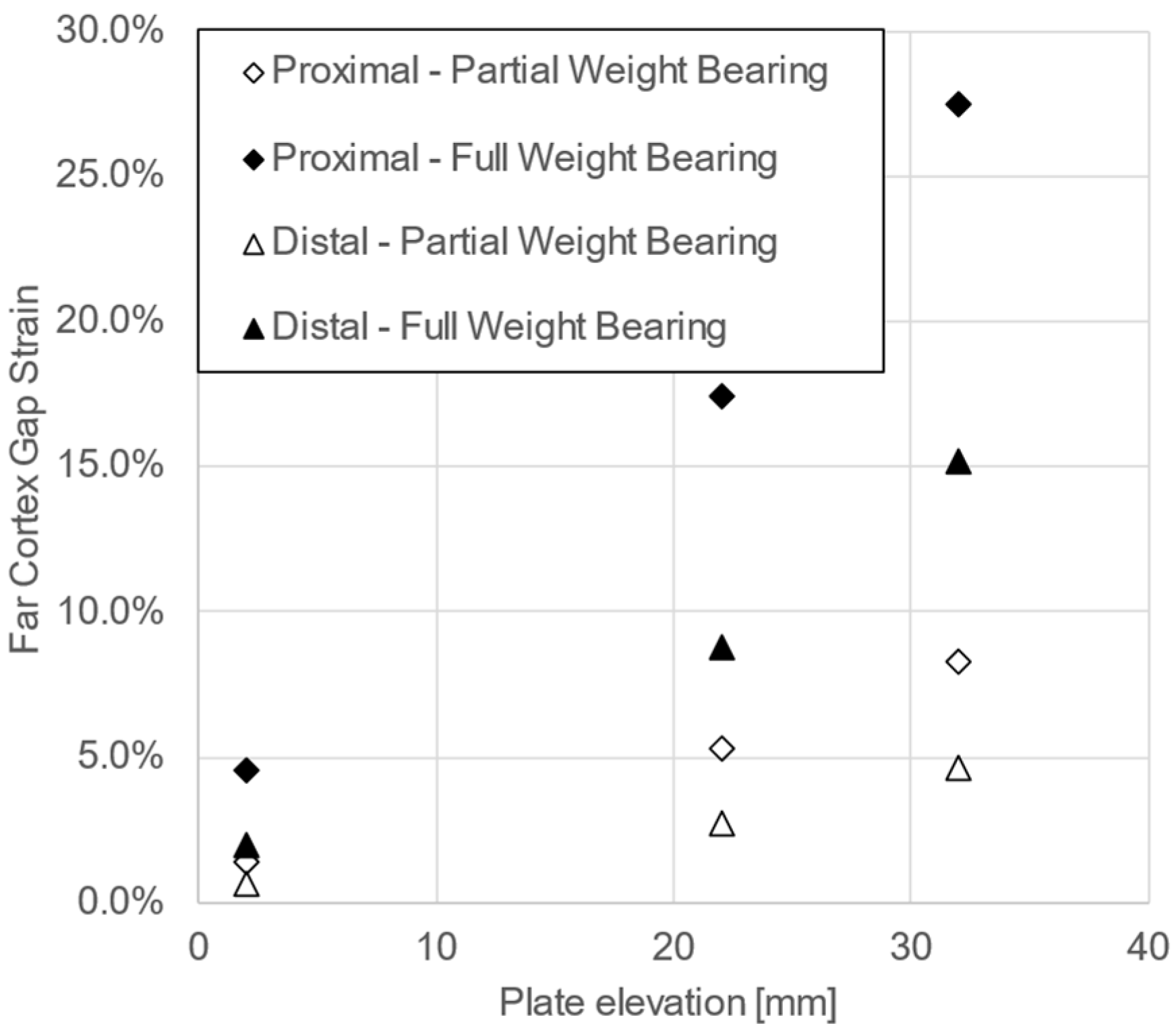
2.2.4. Virtual Biomechanical Analysis of Externalized Locked Plating
2.3. Postoperative Protocol for Active Rehabilitation and Plate Removal
2.4. Data Acquisition and Analysis
2.5. Statistical Analysis
3. Results
3.1. Clinical Outcomes
3.2. Functional Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Catagni, M.A.; Ottaviani, G.; Maggioni, M. Treatment strategies for complex fractures of the tibial plateau with external circular fixation and limited internal fixation. J. Trauma 2007, 63, 1043–1053. [Google Scholar] [CrossRef] [PubMed]
- Gosling, T.; Schandelmaier, P.; Muller, M.; Hankemeier, S.; Wagner, M.; Krettek, C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin. Orthop. Relat. Res. 2005, 439, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Bove, F.; Sala, F.; Capitani, P.; Thabet, A.M.; Scita, V.; Spagnolo, R. Treatment of fractures of the tibial plateau (Schatzker VI) with external fixators versus plate osteosynthesis. Injury 2018, 49 (Suppl. 3), S12–S18. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.W.; Tzeng, H.M.; Chou, Y.J.; Teng, H.P.; Liu, H.H.; Wong, C.Y. Treatment of distal tibial metaphyseal fractures: Plating versus shortened intramedullary nailing. Injury 2006, 37, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Zelle, B.A.; Bhandari, M.; Espiritu, M.; Koval, K.J.; Zlowodzki, M. Treatment of distal tibia fractures without articular involvement: A systematic review of 1125 fractures. J. Orthop. Trauma 2006, 20, 76–79. [Google Scholar] [CrossRef]
- Luo, P.; Xu, D.; Wu, J.; Chen, Y.H. Locked plating as an external fixator in treating tibial fractures: A PRISMA-compliant systematic review. Medicine (Baltimore) 2017, 96, e9083. [Google Scholar] [CrossRef]
- Lau, T.W.; Leung, F.; Chan, C.F.; Chow, S.P. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int. Orthop. 2008, 32, 697–703. [Google Scholar] [CrossRef]
- Scolaro, J.A.; Broghammer, F.H.; Donegan, D.J. Intramedullary Tibial Nail Fixation of Simple Intraarticular Distal Tibia Fractures. J. Orthop. Trauma 2016, 30 (Suppl. 4), S12–S16. [Google Scholar] [CrossRef]
- Kalinterakis, G.; Koutras, A.; Syllaios, A.; Michalakeas, N.; Lytras, D.; Tsilikis, I. The evolution and impact of the “damage control orthopedics” paradigm in combat surgery: A review. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 501–508. [Google Scholar] [CrossRef]
- Hasenboehler, E.; Rikli, D.; Babst, R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: A retrospective study of 32 patients. Injury 2007, 38, 365–370. [Google Scholar] [CrossRef]
- Janssen, K.W.; Biert, J.; van Kampen, A. Treatment of distal tibial fractures: Plate versus nail: A retrospective outcome analysis of matched pairs of patients. Int. Orthop. 2007, 31, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Yang, Y.; Jiang, L.S. Plate fixation versus intramedullary nailing for displaced extra-articular distal tibia fractures: A system review. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.L.; Bonar, S.; Nepola, J.V.; Decoster, T.A.; Hurwitz, S.R. Use of an articulated external fixator for fractures of the tibial plafond. J. Bone Joint. Surg. Am. 1995, 77, 1498–1509. [Google Scholar] [CrossRef] [PubMed]
- Nork, S.E.; Schwartz, A.K.; Agel, J.; Holt, S.K.; Schrick, J.L.; Winquist, R.A. Intramedullary nailing of distal metaphyseal tibial fractures. J. Bone Joint. Surg. Am. 2005, 87, 1213–1221. [Google Scholar] [CrossRef] [PubMed]
- Sitnik, A.A.; Beletsky, A.V. Minimally invasive percutaneous plate fixation of tibia fractures: Results in 80 patients. Clin. Orthop. Relat. Res. 2013, 471, 2783–2789. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fang, X.; Jiang, L.; Wang, Y.; Zhao, L. Treatment of Gustilo grade III tibial fractures with unreamed intramedullary nailing versus external fixator: A meta-analysis. Med. Sci. Monit. 2012, 18, Ra49-56. [Google Scholar] [CrossRef]
- Kerkhoffs, G.M.; Kuipers, M.M.; Marti, R.K.; Van der Werken, C. External fixation with standard AO-plates: Technique, indications, and results in 31 cases. J. Orthop. Trauma 2003, 17, 61–64. [Google Scholar] [CrossRef]
- Kloen, P. Supercutaneous plating: Use of a locking compression plate as an external fixator. J. Orthop. Trauma 2009, 23, 72–75. [Google Scholar] [CrossRef]
- Marti, R.K.; van der Werken, C. The AO-plate for external fixation in 12 cases. Acta Orthop. Scand. 1991, 62, 60–62. [Google Scholar] [CrossRef]
- Qiu, X.S.; Yuan, H.; Zheng, X.; Wang, J.F.; Xiong, J.; Chen, Y.X. Locking plate as a definitive external fixator for treating tibial fractures with compromised soft tissue envelop. Arch. Orthop. Trauma Surg. 2014, 134, 383–388. [Google Scholar] [CrossRef]
- Ma, C.H.; Wu, C.H.; Jiang, J.R.; Tu, Y.K.; Lin, T.S. Metaphyseal locking plate as an external fixator for open tibial fracture: Clinical outcomes and biomechanical assessment. Injury 2017, 48, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.H.; Tu, Y.K.; Yeh, J.H.; Yang, S.C.; Wu, C.H. Using external and internal locking plates in a two-stage protocol for treatment of segmental tibial fractures. J. Trauma 2011, 71, 614–619. [Google Scholar] [CrossRef]
- Zhang, J.; Ebraheim, N.; Li, M.; He, X.; Liu, J.; Zhu, L.; Yu, Y. External fixation using femoral less invasive stabilization system plate in tibial proximal metaphyseal fracture. Clin. Orthop. Surg. 2015, 7, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.W.; Ebraheim, N.A.; Li, M.; He, X.F.; Schwind, J.; Zhu, L.M.; Yu, Y.H. Distal tibial fracture: An ideal indication for external fixation using locking plate. Chin. J. Traumatol. 2016, 19, 104–108. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, Y.; Liu, L.; Zhou, Z.; Cao, X. Locking compression plate as an external fixator in the treatment of closed distal tibial fractures. Int. Orthop. 2015, 39, 2227–2237. [Google Scholar] [CrossRef] [PubMed]
- Apivatthakakul, T.; Sananpanich, K. The locking compression plate as an external fixator for bone transport in the treatment of a large distal tibial defect: A case report. Injury 2007, 38, 1318–1325. [Google Scholar] [CrossRef]
- Ebraheim, N.A.; Carroll, T.; Hanna, M.; Zhang, J.; Liu, J. Staged treatment of proximal tibial fracture using external locking compression plate. Orthop. Surg. 2014, 6, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Khatod, M.; Botte, M.J.; Hoyt, D.B.; Meyer, R.S.; Smith, J.M.; Akeson, W.H. Outcomes in open tibia fractures: Relationship between delay in treatment and infection. J. Trauma 2003, 55, 949–954. [Google Scholar] [CrossRef]
- Hidayat, L.; Triangga, A.F.R.; Cein, C.R.; Irfantian, A.; Rahayu, B.F.P.; Resubun, A.P.; Magetsari, R. Low profile external fixation using locking compression plate as treatment option for management of soft tissue problem in open tibia fracture grade IIIA: A case series. Int. J. Surg. Case Rep. 2022, 93, 106882. [Google Scholar] [CrossRef]
- Ma, C.H.; Wu, C.H.; Tu, Y.K.; Lin, T.S. Metaphyseal locking plate as a definitive external fixator for treating open tibial fractures--clinical outcome and a finite element study. Injury 2013, 44, 1097–1101. [Google Scholar] [CrossRef]
- Zhang, J.; Ebraheim, N.A.; Li, M.; He, X.; Liu, J.; Zhu, L.; Yu, Y.; Siddiqui, S. External Fixation Using a Locking Plate: A Reliable Way in Treating Distal Tibial Fractures. J. Orthop. Trauma 2015, 29, e454–e458. [Google Scholar] [CrossRef] [PubMed]
- Tulner, S.A.; Strackee, S.D.; Kloen, P. Metaphyseal locking compression plate as an external fixator for the distal tibia. Int. Orthop. 2012, 36, 1923–1927. [Google Scholar] [CrossRef] [PubMed]
- Kanchanomai, C.; Phiphobmongkol, V. Biomechanical evaluation of fractured tibia externally fixed with an LCP. J. Appl. Biomech. 2012, 28, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Yang, L.; Kong, X.; An, L.; Hong, G.; Guo, Z.; Zang, L. Stiffness of the locking compression plate as an external fixator for treating distal tibial fractures: A biomechanics study. BMC Musculoskelet. Disord. 2017, 18, 26. [Google Scholar] [CrossRef]
- Zhang, J.; Ebraheim, N.; Li, M.; He, X.; Schwind, J.; Liu, J.; Zhu, L. External fixation using locking plate in distal tibial fracture: A finite element analysis. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 1099–1104. [Google Scholar] [CrossRef]
- Blažević, D.; Kodvanj, J.; Adamović, P.; Vidović, D.; Trobonjača, Z.; Sabalić, S. Comparison between external locking plate fixation and conventional external fixation for extraarticular proximal tibial fractures: A finite element analysis. J. Orthop. Surg. Res. 2022, 17, 16. [Google Scholar] [CrossRef]
- Ang, B.F.H.; Chen, J.Y.; Yew, A.K.S.; Chua, S.K.; Chou, S.M.; Chia, S.L.; Koh, J.S.B.; Howe, T.S. Externalised locking compression plate as an alternative to the unilateral external fixator: A biomechanical comparative study of axial and torsional stiffness. Bone Joint. Res. 2017, 6, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Makelov, B.; Silva, J.D.; Apivatthakakul, T.; Gueorguiev, B.; Varga, P. Externalized locked plating of unstable high energy proximal tibial fractures. A FEA study. Bul. J. Orthop. Trauma 2019, 56, 113–138. [Google Scholar]
- Makelov, B.; Gueorguiev, B.; Apivatthakakul, T. Definitive external plate stabilization with metaphyseal locking plate LISS-DF in multiple trauma patient with ‘‘floating knee’’ injury. Bul. J. Orthop. Trauma. 2019, 56, 1–19. [Google Scholar]
- Eckardt, H.; Morgenstern, M.; Cadosch, D.; Stoffel, K. Flouroscopic Control of Tibial Torsion After Intramedullary Nailing: A Technical Trick. J. Orthop. Trauma 2021, 35, e507–e510. [Google Scholar] [CrossRef]
- Dragomir-Daescu, D.; Op Den Buijs, J.; McEligot, S.; Dai, Y.; Entwistle, R.C.; Salas, C.; Melton, L.J., 3rd; Bennet, K.E.; Khosla, S.; Amin, S. Robust QCT/FEA models of proximal femur stiffness and fracture load during a sideways fall on the hip. Ann. Biomed. Eng. 2011, 39, 742–755. [Google Scholar] [CrossRef] [PubMed]
- Perren, S.M. Physical and biological aspects of fracture healing with special reference to internal fixation. Clin. Orthop. Relat. Res. 1979, 138, 175–196. [Google Scholar]
- Perren, S.M. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: Choosing a new balance between stability and biology. J. Bone Joint. Surg. Br. 2002, 84, 1093–1110. [Google Scholar] [CrossRef] [PubMed]
- Possley, D.R.; Burns, T.C.; Stinner, D.J.; Murray, C.K.; Wenke, J.C.; Hsu, J.R. Temporary external fixation is safe in a combat environment. J. Trauma 2010, 69 (Suppl. 1), S135–S139. [Google Scholar] [CrossRef]
- Moss, D.P.; Tejwani, N.C. Biomechanics of external fixation: A review of the literature. Bull. NYU Hosp. Jt. Dis. 2007, 65, 294–299. [Google Scholar]
- Schmal, H.; Strohm, P.C.; Jaeger, M.; Südkamp, N.P. Flexible fixation and fracture healing: Do locked plating ‘internal fixators’ resemble external fixators? J. Orthop. Trauma 2011, 25 (Suppl. 1), S15–S20. [Google Scholar] [CrossRef]
- MacLeod, A.R.; Simpson, A.H.; Pankaj, P. Age-related optimization of screw placement for reduced loosening risk in locked plating. J. Orthop. Res. 2016, 34, 1856–1864. [Google Scholar] [CrossRef]
- Ahmad, M.; Nanda, R.; Bajwa, A.S.; Candal-Couto, J.; Green, S.; Hui, A.C. Biomechanical testing of the locking compression plate: When does the distance between bone and implant significantly reduce construct stability? Injury 2007, 38, 358–364. [Google Scholar] [CrossRef]

| Classification | Type/Grade | Number of Patients | Gender |
|---|---|---|---|
| AO/OTA fracture classification | 41-C2.2 | 7 | M |
| 41-C2.3 | 1 | F | |
| 41-A3.1 | 2 | M | |
| 41-A3.1 | 2 | F | |
| 42-C3j | 2 | M | |
| 43-A2.1 | 1 | M | |
| 43-A2.3 | 3 | M | |
| AO soft tissue grading system | IO2 | 7 | M |
| IO2 | 3 | F | |
| IO3 | 6 | M | |
| IO4 | 2 | M |
| Categories | Subgroups | Operative Time (Minutes) | Healing Time (Weeks) |
|---|---|---|---|
| Age | ≤50 years | 31.4 ± 7.1 (25–45) | 20.7 ± 6.1 (12–28) |
| >50 years | 34.4 ± 6.6 (20–45) | 20.9 ± 3.6 (16–29) | |
| p-value | 0.26 | 0.93 | |
| Fracture location | Proximal | 32.4 ± 6.8 (20–45) | 21.8 ± 3.6 (16–28) |
| Distal | 34.8 ± 6.9 (25–45) | 19.0 ± 6.1 (12–29) | |
| p-value | 0.38 | 0.25 | |
| Fracture severity | Simple | 34.3 ± 5.5 (25–42) | 18.4 ± 2.9 (14–22) |
| Complex | 32.6 ± 7.6 (20–45) | 22.4 ± 4.9 (12–29) | |
| p-value | 0.42 | 0.04 | |
| Soft tissue injury | Mild | 34.0 ± 7.1 (20–45) | 21.2 ± 5.3 (12–29) |
| Severe | 32.2 ± 6.6 (20–45) | 21.1 ± 3.8 (14–26) | |
| p-value | 0.46 | 0.76 |
| Categories | Subgroups | HSS | AOFAS | ROM knee (°) | ROM Ankle Flexion (°) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Flexion | Extension | Plantar | Dorsal | ||||||||||||||||
| 4 Weeks | Final FU | p-Value | 4 Weeks | Final FU | p-Value | 4 Weeks | Final FU | p-Value | 4 Weeks | Final FU | p-Value | 4 Weeks | Final FU | p-Value | 4 Weeks | Final FU | p-Value | ||
| Age | ≤50 years | 88.7 | 98.6 | 0.01 | 93.6 | 99.1 | 0.03 | 113.6 | 142.1 | 0.03 | 0.4 | 0.4 | 0.99 | 25.0 | 40.0 | 0.02 | 13.6 | 18.6 | 0.02 |
| >50 years | 89.9 | 96.8 | <0.01 | 91.4 | 98.3 | <0.01 | 97.7 | 121.4 | <0.01 | 2.7 | 2.0 | 0.18 | 19.6 | 35.4 | <0.01 | 11.4 | 18.5 | <0.01 | |
| p-value | 0.72 | 0.54 | – | 0.29 | 0.28 | – | 0.15 | <0.01 | – | 0.13 | 0.38 | – | 0.04 | 0.28 | – | 0.13 | 0.79 | – | |
| Fracture location | Proximal | 87.5 | 97.2 | <0.01 | 92.0 | 92.8 | <0.01 | 92.1 | 125.0 | <0.01 | 2.2 | 1.7 | 0.19 | 22.1 | 35.4 | <0.01 | 12.1 | 18.3 | <0.01 |
| Distal | 93.3 | 98.2 | 0.04 | 98.1 | 98.7 | 0.03 | 127.5 | 138.3 | 0.04 | 0.8 | 0.8 | 0.99 | 20.8 | 40.8 | 0.02 | 12.5 | 19.2 | 0.03 | |
| p-value | 0.18 | 0.55 | – | 0.98 | 0.89 | – | <0.01 | 0.29 | – | 0.55 | 0.62 | – | 0.68 | 0.29 | – | 0.82 | 0.75 | – | |
| Fracture complexity | Simple | 93.9 | 98.7 | 0.04 | 91.7 | 98.3 | 0.02 | 114.3 | 132.1 | 0.04 | 0.7 | 0.7 | 0.98 | 21.4 | 37.1 | 0.02 | 11.4 | 18.6 | 0.02 |
| Complex | 86.6 | 96.7 | <0.01 | 92.4 | 98.8 | <0.01 | 97.2 | 127.7 | <0.01 | 2.4 | 1.8 | 0.41 | 21.8 | 37.2 | <0.01 | 12.7 | 18.7 | <0.01 | |
| p-value | 0.04 | 0.21 | – | 0.38 | 0.42 | – | 0.18 | 0.79 | – | 0.42 | 0.48 | – | 0.86 | 0.93 | – | 0.42 | 0.79 | – | |
| Soft tissue injury | Mild | 91.0 | 98.5 | <0.01 | 93.0 | 98.6 | <0.01 | 103.5 | 131.0 | <0.01 | 2.2 | 1.5 | 0.32 | 22.0 | 37.0 | <0.01 | 12.0 | 19.0 | <0.01 |
| Severe | 85.7 | 96.2 | 0.01 | 91.4 | 98.5 | 0.02 | 104.4 | 127.5 | 0.02 | 1.2 | 1.2 | 0.99 | 21.2 | 37.5 | 0.01 | 12.5 | 18.1 | 0.01 | |
| p-value | 0.52 | 0.27 | – | 0.46 | 0.63 | – | 0.57 | 0.32 | – | 0.46 | 0.90 | – | 0.76 | 0.70 | – | 0.63 | 0.83 | – | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makelov, B.; Mischler, D.; Varga, P.; Apivatthakakul, T.; Fletcher, J.W.A.; Veselinov, D.; Berk, T.; Raykov, D.; Gueorguiev, B. Single-Stage Externalized Locked Plating for Treatment of Unstable Meta-Diaphyseal Tibial Fractures. J. Clin. Med. 2023, 12, 1600. https://doi.org/10.3390/jcm12041600
Makelov B, Mischler D, Varga P, Apivatthakakul T, Fletcher JWA, Veselinov D, Berk T, Raykov D, Gueorguiev B. Single-Stage Externalized Locked Plating for Treatment of Unstable Meta-Diaphyseal Tibial Fractures. Journal of Clinical Medicine. 2023; 12(4):1600. https://doi.org/10.3390/jcm12041600
Chicago/Turabian StyleMakelov, Biser, Dominic Mischler, Peter Varga, Theerachai Apivatthakakul, James W. A. Fletcher, Deyan Veselinov, Till Berk, Dimitur Raykov, and Boyko Gueorguiev. 2023. "Single-Stage Externalized Locked Plating for Treatment of Unstable Meta-Diaphyseal Tibial Fractures" Journal of Clinical Medicine 12, no. 4: 1600. https://doi.org/10.3390/jcm12041600
APA StyleMakelov, B., Mischler, D., Varga, P., Apivatthakakul, T., Fletcher, J. W. A., Veselinov, D., Berk, T., Raykov, D., & Gueorguiev, B. (2023). Single-Stage Externalized Locked Plating for Treatment of Unstable Meta-Diaphyseal Tibial Fractures. Journal of Clinical Medicine, 12(4), 1600. https://doi.org/10.3390/jcm12041600







