Percutaneous Drainage vs. Surgery as Definitive Treatment for Anastomotic Leak after Intestinal Resection in Patients with Crohn’s Disease
Abstract
:1. Introduction
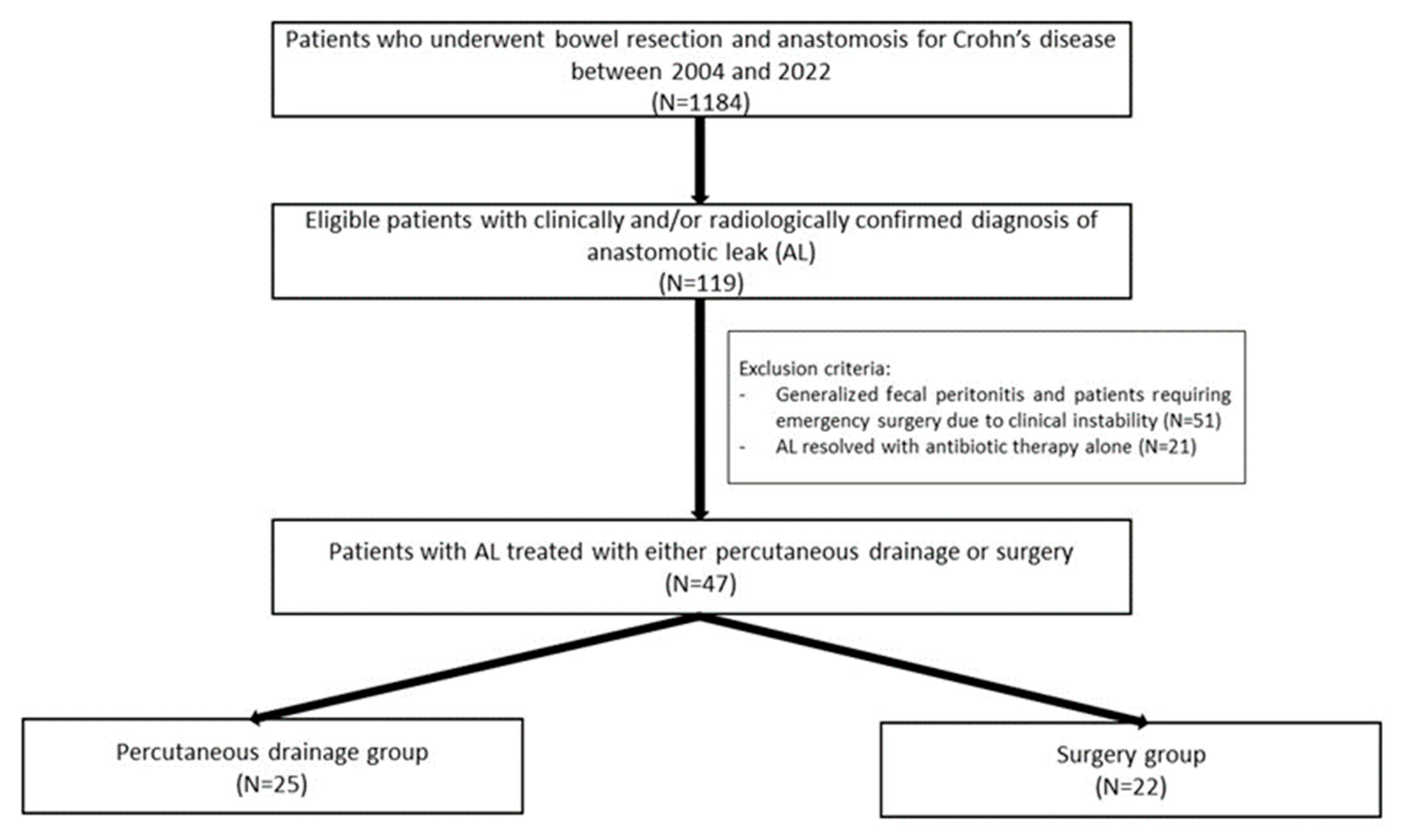
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burr, N.E.; Lord, R.; Hull, M.A.; Subramanian, V. Decreasing Risk of First and Subsequent Surgeries in Patients with Crohn’s Disease in England from 1994 through 2013. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2019, 17, 2042–2049.e4. [Google Scholar] [CrossRef] [PubMed]
- Iesalnieks, I.; Kilger, A.; Glaß, H.; Müller-Wille, R.; Klebl, F.; Ott, C.; Strauch, U.; Piso, P.; Schlitt, H.J.; Agha, A. Intraabdominal septic complications following bowel resection for Crohn’s disease: Detrimental influence on long-term outcome. Int. J. Colorectal Dis. 2008, 23, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Post, S.; Betzler, M.; von Ditfurth, B.; Schürmann, G.; Küppers, P.; Herfarth, C. Risks of Intestinal Anastomoses in Crohn’s Disease. Ann. Surg. 1991, 213, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Celentano, V.; Pellino, G.; Spinelli, A.; Selvaggi, F. Anastomosis configuration and technique following ileocaecal resection for Crohn’s disease: A multicentre study. Updat. Surg. 2021, 73, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Ashburn, J.H.; Stocchi, L.; Kiran, R.P.; Dietz, D.W.; Remzi, F.H. Consequences of Anastomotic Leak After Restorative Proctectomy for Cancer: Effect on Long-term Function and Quality of Life. Dis. Colon. Rectum. 2013, 56, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Buisson, A.; Chevaux, J.B.; Allen, P.B.; Bommelaer, G.; Peyrin-Biroulet, L. Review article: The natural history of postoperative Crohn’s disease recurrence. Aliment. Pharmacol. Ther. 2012, 35, 625–633. [Google Scholar] [CrossRef]
- Byrne, J.; Stephens, R.; Isaacson, A.; Yu, H.; Burke, C. Image-guided Percutaneous Drainage for Treatment of Post-Surgical Anastomotic Leak in Patients with Crohn’s Disease. J. Crohns Colitis 2016, 10, 38–42. [Google Scholar] [CrossRef]
- Rottoli, M.; Tanzanu, M.; Manzo, C.A.; Bacchi Reggiani, M.L.; Gionchetti, P.; Rizzello, F.; Boschi, L.; Poggioli, G. Strictureplasty for Crohn’s disease of the small bowel in the biologic era: Long-term outcomes and risk factors for recurrence. Tech Coloproctol. 2020, 24, 711–720. [Google Scholar] [CrossRef]
- Stöss, C.; Berlet, M.; Reischl, S.; Nitsche, U.; Weber, M.C.; Friess, H.; Wilhelm, D.; Neumann, P.A. Crohn’s disease: A population-based study of surgery in the age of biological therapy. Int. J. Color. Dis. 2021, 36, 2419–2426. [Google Scholar] [CrossRef]
- Jones, D.W.; Finlayson, S.R.G. Trends in Surgery for Crohn’s Disease in the Era of Infliximab. Ann. Surg. 2010, 252, 307–312. [Google Scholar] [CrossRef]
- Ellis, C.T.; Maykel, J.A. Defining Anastomotic Leak and the Clinical Relevance of Leaks. Clin. Colon. Rectal Surg. 2021, 34, 359–365. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Weitz, J.; Hohenberger, W.; Heald, R.J.; Moran, B.; Ulrich, A.; Holm, T.; Wong, W.D.; Tiret, E.; Moriya, Y.; et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: A proposal by the International Study Group of Rectal Cancer. Surgery 2010, 147, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Felder, S.I.; Barmparas, G.; Murrell, Z.; Fleshner, P. Risk factors for failure of percutaneous drainage and need for reoperation following symptomatic gastrointestinal anastomotic leak. Am. J. Surg. 2014, 208, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Iesalnieks, I.; Bittermann, T.; Schlitt, H.J.; Hackl, C. Reversal of end-ileostomy in patients with Crohn’s disease. Int. J. Color. Dis. 2021, 36, 2119–2125. [Google Scholar] [CrossRef] [PubMed]
- Rottoli, M.; Casadei, B.; Vallicelli, C.; Vitali, G.; Ghignone, F.; Melina, M.; Tanzanu, M.; Poggioli, G. Morbidity associated with closure of ileostomy after a three-stage ileal pouch-anal anastomosis. Updat. Surg. 2019, 71, 533–537. [Google Scholar] [CrossRef]
- Waterland, P.; Athanasiou, T.; Patel, H. Post-operative abdominal complications in Crohn’s disease in the biological era: Systematic review and meta-analysis. World J. Gastrointest. Surg. 2016, 8, 274. [Google Scholar] [CrossRef]
- Dignass, A.; Van Assche, G.; Lindsay, J.O.; Lémann, M.; Söderholm, J.; Colombel, J.F.; Danese, S.; D’Hoore, A.; Gassull, M.; Gomollón, F.; et al. The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Current management. J. Crohns Colitis 2010, 4, 28–62. [Google Scholar] [CrossRef]
- Clancy, C.; Boland, T.; Deasy, J.; McNamara, D.; Burke, J.P. A Meta-analysis of Percutaneous Drainage Versus Surgery as the Initial Treatment of Crohn’s Disease-related Intra-abdominal Abscess. J. Crohns Colitis 2016, 10, 202–208. [Google Scholar] [CrossRef]
- Hedrick, T.L.; Kane, W. Management of Acute Anastomotic Leaks. Clin. Colon. Rectal Surg. 2021, 34, 400–405. [Google Scholar] [CrossRef]
- Adamina, M.; Bonovas, S.; Raine, T.; Spinelli, A.; Warusavitarne, J.; Armuzzi, A.; Bachmann, O.; Bager, P.; Biancone, L.; Bokemeyer, B.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Surgical Treatment. J. Crohns Colitis 2020, 14, 155–168. [Google Scholar] [CrossRef]
- Garcia, J.C.; Topazian, M. Abscesses in Crohn’s Disease. J. Clin. Gastroenterol. 2001, 32, 4. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, A.; Matsui, T.; Sakurai, T.; Ueki, T.; Nakabayashi, S.; Yao, T.; Futami, K.; Arima, S.; Ono, H. The clinical characteristics and outcome of intraabdominal abscess in Crohn’s disease. J. Gastroenterol. 2004, 39, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Celentano, V.; Giglio, M.C.; Pellino, G.; Rottoli, M.; Sampietro, G.; Spinelli, A.; Selvaggi, F. High complication rate in Crohn’s disease surgery following percutaneous drainage of intra-abdominal abscess: A multicentre study. Int. J. Color. Dis. 2022, 37, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Pellino, G.; Keller, D.S.; Sampietro, G.M.; Angriman, I.; Carvello, M.; Celentano, V.; Colombo, F.; Di Candido, F.; Laureti, S.; Luglio, G.; et al. Correction to: Inflammatory bowel disease position statement of the Italian Society of Colorectal Surgery (SICCR): Crohn’s disease. Tech. Coloproctol. 2020, 24, 903. [Google Scholar] [CrossRef] [PubMed]
- El-Hussuna, A.; Karer, M.L.M.; Uldall Nielsen, N.N.; Mujukian, A.; Fleshner, P.R.; Iesalnieks, I.; Horesh, N.; Kopylov, U.; Jacoby, H.; Al-Qaisi, H.M.; et al. Postoperative complications and waiting time for surgical intervention after radiologically guided drainage of intra-abdominal abscess in patients with Crohn’s disease. BJS Open 2021, 5, zrab075. [Google Scholar] [CrossRef]
| Overall (n = 47) | Percutaneous Drainage (PD) (n = 25) | Surgery (n = 22) | p * | |
|---|---|---|---|---|
| Patient and preoperative features | ||||
| Age (years) | 45 (33–56) | 48 (38–53) | 37.5 (31–56) | 0.2 |
| Male gender | 32 (70%) | 18 (76%) | 14 (64%) | 0.4 |
| BMI (kg/m2) | 22.0 (19.5–24.6) | 22.6 (21.3–24.6) | 20.8 (19.0–24.5) | 0.3 |
| Steroids at surgery | 20 (45%) | 11 (44%) | 9 (40%) | 0.9 |
| History of biologic therapy | 19 (40%) | 12 (48%) | 7 (32%) | 0.3 |
| Disease behavior | ||||
| stenotic | 33 (72%) | 18 (76%) | 15 (68%) | 0.6 |
| penetrating | 23 (49%) | 13 (52%) | 10 (45%) | 0.7 |
| Abscess at surgery | 8 (17%) | 4 (16%) | 4 (18%) | 0.8 |
| Previous abdominal surgery | 21 (45%) | 14 (56%) | 7 (32%) | 0.1 |
| Serum albumin (g/dL) | 3.9 (3.6–4.3) | 3.8 (3.5–4.1) | 4.1 (3.6–4.4) | 0.040 |
| Hemoglobin (g/dL) | 13.0 (12.1–14.3) | 13.1 (11.9–14.4) | 12.9 (12.6–14.1) | 0.9 |
| Diagnosis and surgical features | ||||
| POD of leak | 7 (5–12) | 9 (7–16) | 5 (4–6) | 0.001 |
| Abscess diameter (mm) | 50 (40–63) | 60 (47–80) | 42.5 (35–50) | 0.007 |
| WBC (103/mm3) | 12.5 (9.2–14.5) | 11.4 (9.2–14.3) | 13 (8.8–16.2) | 0.4 |
| Serum CRP (mg/dL) | 13.4 (8.9–18.7) | 12.3 (7.8–18.6) | 15.9 (9.9–22.6) | 0.3 |
| Procalcitonin (ng/mL) | 0.6 (0.1–2.8) | 0.1 (0.1–6.9) | 0.9 (0.2–2.8) | 0.5 |
| Year of intervention | 0.1 | |||
| 2004–2015 | 28 (60%) | 12 (43%) | 16 (57%) | |
| 2016–2022 | 19 (40%) | 13 (68%) | 6 (32%) | |
| Type of anastomosis | ||||
| ileo-colic | 25 (53%) | 17 (68%) | 8 (36%) | 0.030 |
| ileo-colic and colo-rectal | 8 (17%) | 3 (12%) | 5 (23%) | 0.5 |
| ileo-colic and ileo-ileal | 4 (8.5%) | 3 (12%) | 1 (4%) | 0.3 |
| ileo-ileal | 4 (8.5%) | 1 (4%) | 3 (14%) | 0.6 |
| ileo-rectal | 6 (13%) | 1 (4%) | 5 (23%) | 0.1 |
| Follow-up | ||||
| Success rate of primary treatment | 42 (89%) | 21 (84%) | 21 (95%) | 0.2 |
| Resolution time (days) | 13 (8–26) | 14 (6–38) | 13 (10–22) | 0.9 |
| Follow-up (months) | 19 (12–58) | 17 (11–56) | 21 (12–69) | 0.7 |
| Discharge at 90 days | 46 (98%) | 25 (100%) | 21 (95%) | 0.3 |
| Re-admission at 90 days | 2 (4%) | 2 (8%) | 0 (0%) | 0.2 |
| Re-intervention at 90 days | 6 (13%) | 4 (16%) | 2 (9%) | 0.5 |
| Medical complications at 90 days | 7 (15%) | 3 (12%) | 4 (18%) | 0.6 |
| Pneumonia | 3 (6%) | 1 (4%) | 2 (9%) | 0.5 |
| Septic | 2 (4%) | 2 (8%) | 0 (0%) | 0.2 |
| Other | 2 (4%) | 0 (0%) | 2 (9%) | 0.1 |
| Surgical complications at 90 days | 10 (21%) | 6 (24%) | 4 (36%) | 0.6 |
| Wound infection | 3 (6%) | 2 (8%) | 1 (5%) | 0.6 |
| IASC | 6 (13%) | 4 (16%) | 2 (9%) | 0.5 |
| Other | 1 (2%) | 0 (0%) | 1 (5%) | 0.3 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| OR (CI 95%) | p | OR (CI 95%) | p | |
| Age | 1.02 (0.98–1.06) | 0.4 | ||
| Male gender | 0.55 (0.16–1.96) | 0.4 | ||
| BMI (kg/m2) | 1.03 (0.90–1.17) | 0.7 | ||
| Steroids | 0.94 (0.30–2.99) | 0.9 | ||
| Biologics | 1.98 (0.60–6.51) | 0.3 | ||
| Stenotic disease | 1.48 (0.41–5.34) | 0.5 | ||
| Penetrating disease | 1.30 (0.41–1.40) | 0.7 | ||
| Abscess at surgery | 0.86 (0.19–3.93) | 0.8 | ||
| Previous abdominal surgery | 2.73 (0.83–9.01) | 0.100 | ||
| Serum albumin (g/dL) | 0.88 (0.77–1.01) | 0.051 | ||
| Hemoglobin (g/dL) | 0.91 (0.69–1.20) | 0.5 | ||
| POD leak | 1.24 (1.03–1.49) | 0.020 | 1.25 (1.03–1.53) | 0.027 |
| Abscess diameter (mm) | 1.05 (1.01–1.09) | 0.021 | ||
| WBC (103/mm3) | 0.92 (0.80–1.06) | 0.2 | ||
| Serum CRP (mg/dL) | 0.95 (0.86–1.04) | 0.3 | ||
| Procalcitonin (ng/dl) | 1.21 (0.59–2.45) | 0.6 | ||
| Year of intervention (2016–2022 vs. before) | 2.89 (0.85–9.82) | 0.089 | 6.36 (1.04–39.03) | 0.046 |
| Ileo-colic anastomosis alone (vs. other) | 3.72 (2.29–12.45) | 0.033 | 6.34 (1.15–35.04) | 0.034 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belvedere, A.; Dajti, G.; Larotonda, C.; Angelicchio, L.; Rizzello, F.; Gionchetti, P.; Poggioli, G.; Rottoli, M. Percutaneous Drainage vs. Surgery as Definitive Treatment for Anastomotic Leak after Intestinal Resection in Patients with Crohn’s Disease. J. Clin. Med. 2023, 12, 1392. https://doi.org/10.3390/jcm12041392
Belvedere A, Dajti G, Larotonda C, Angelicchio L, Rizzello F, Gionchetti P, Poggioli G, Rottoli M. Percutaneous Drainage vs. Surgery as Definitive Treatment for Anastomotic Leak after Intestinal Resection in Patients with Crohn’s Disease. Journal of Clinical Medicine. 2023; 12(4):1392. https://doi.org/10.3390/jcm12041392
Chicago/Turabian StyleBelvedere, Angela, Gerti Dajti, Cristina Larotonda, Laura Angelicchio, Fernando Rizzello, Paolo Gionchetti, Gilberto Poggioli, and Matteo Rottoli. 2023. "Percutaneous Drainage vs. Surgery as Definitive Treatment for Anastomotic Leak after Intestinal Resection in Patients with Crohn’s Disease" Journal of Clinical Medicine 12, no. 4: 1392. https://doi.org/10.3390/jcm12041392
APA StyleBelvedere, A., Dajti, G., Larotonda, C., Angelicchio, L., Rizzello, F., Gionchetti, P., Poggioli, G., & Rottoli, M. (2023). Percutaneous Drainage vs. Surgery as Definitive Treatment for Anastomotic Leak after Intestinal Resection in Patients with Crohn’s Disease. Journal of Clinical Medicine, 12(4), 1392. https://doi.org/10.3390/jcm12041392







