Early Detection of Alzheimer’s Disease in Postmenopausal Women Using Thalamic Subnuclear Volumetry
Abstract
:1. Introduction
2. Subjects and Methods
2.1. Subjects
2.2. Serum Sex Hormone Measurements
2.3. Magnetic Resonance Imaging Data Acquisition
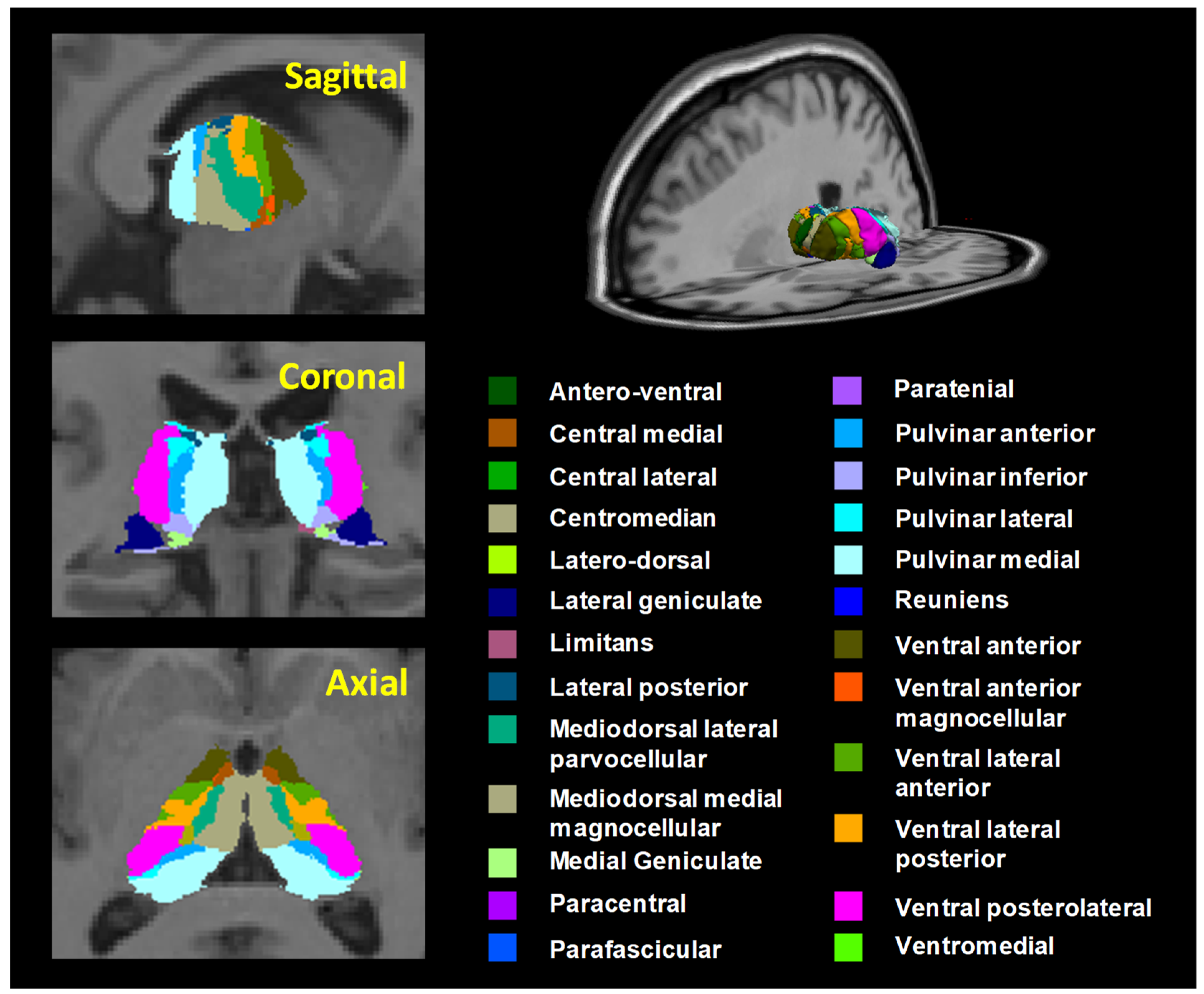
2.4. Data Processing and Analysis
3. Results
3.1. Serum Sex Hormone Levels
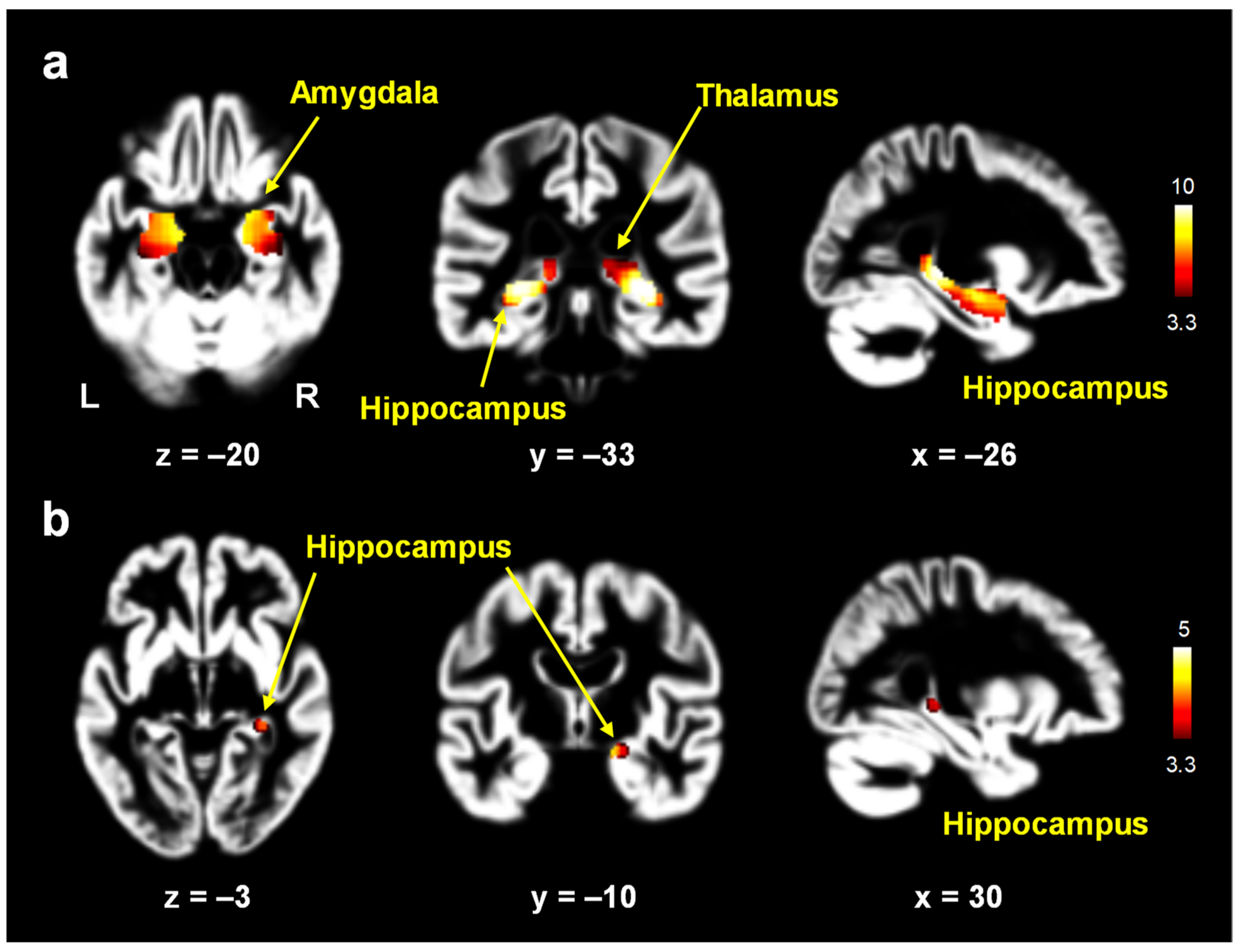
3.2. Gray Matter Volume Changes
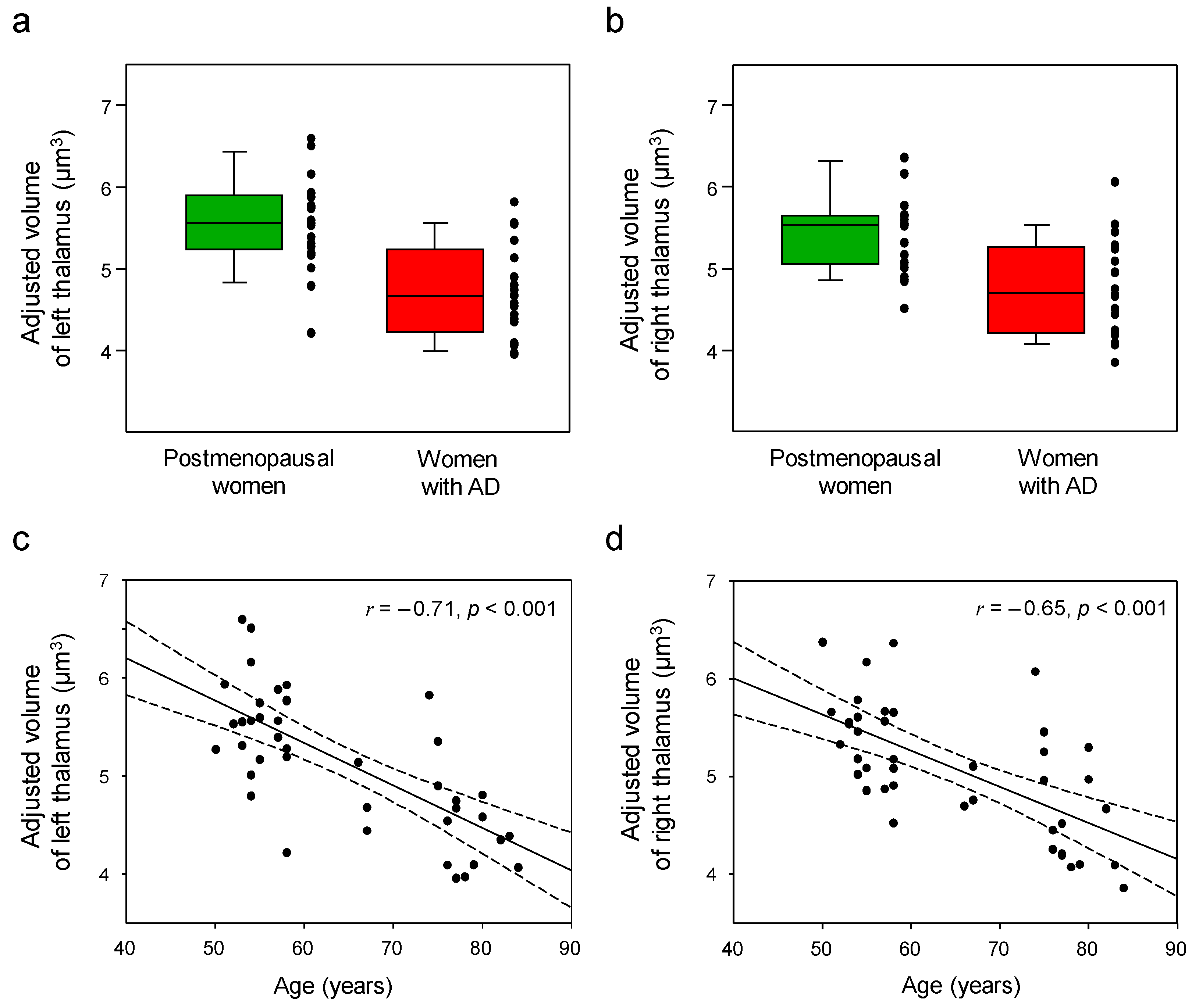
3.3. Thalamic Volume Changes
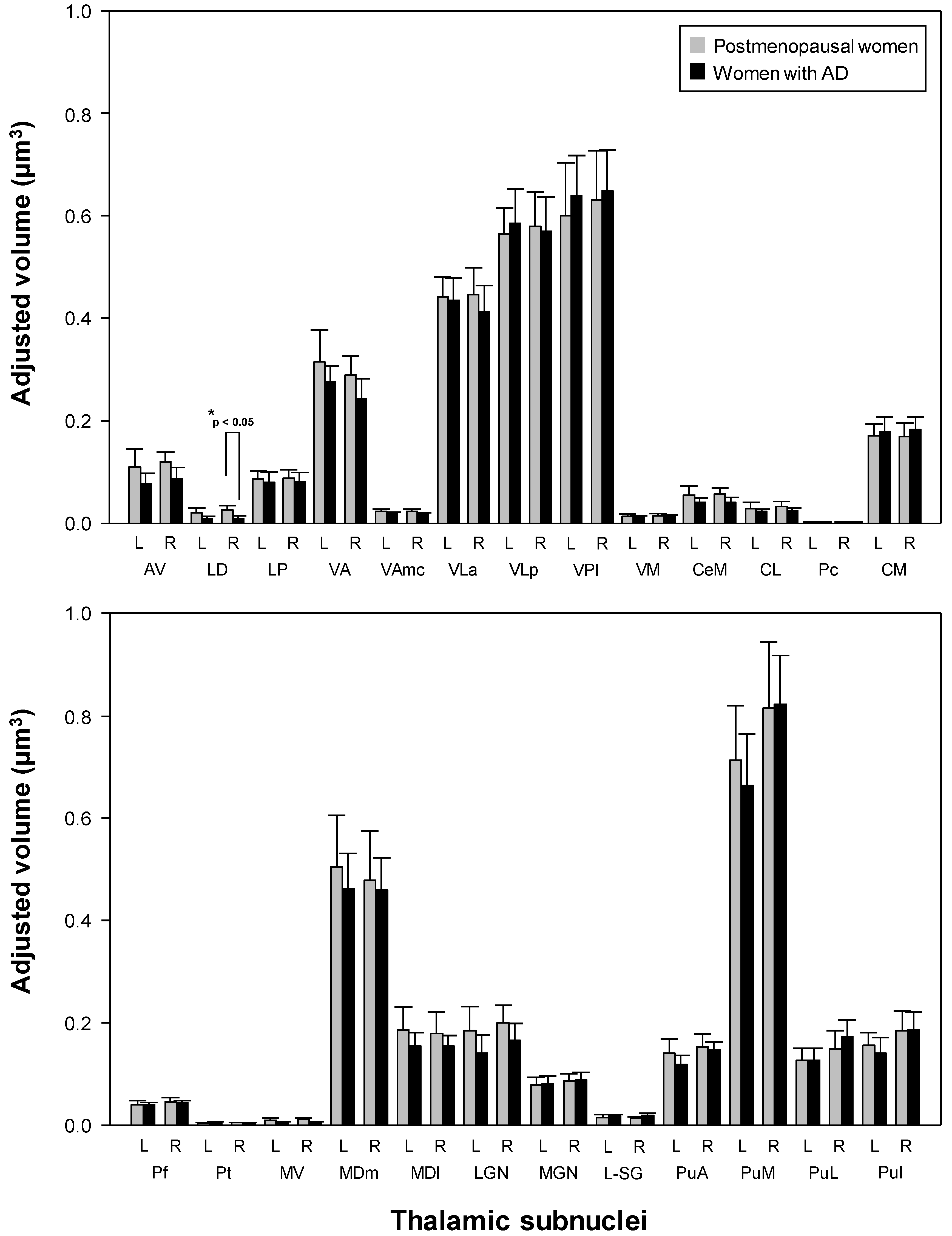
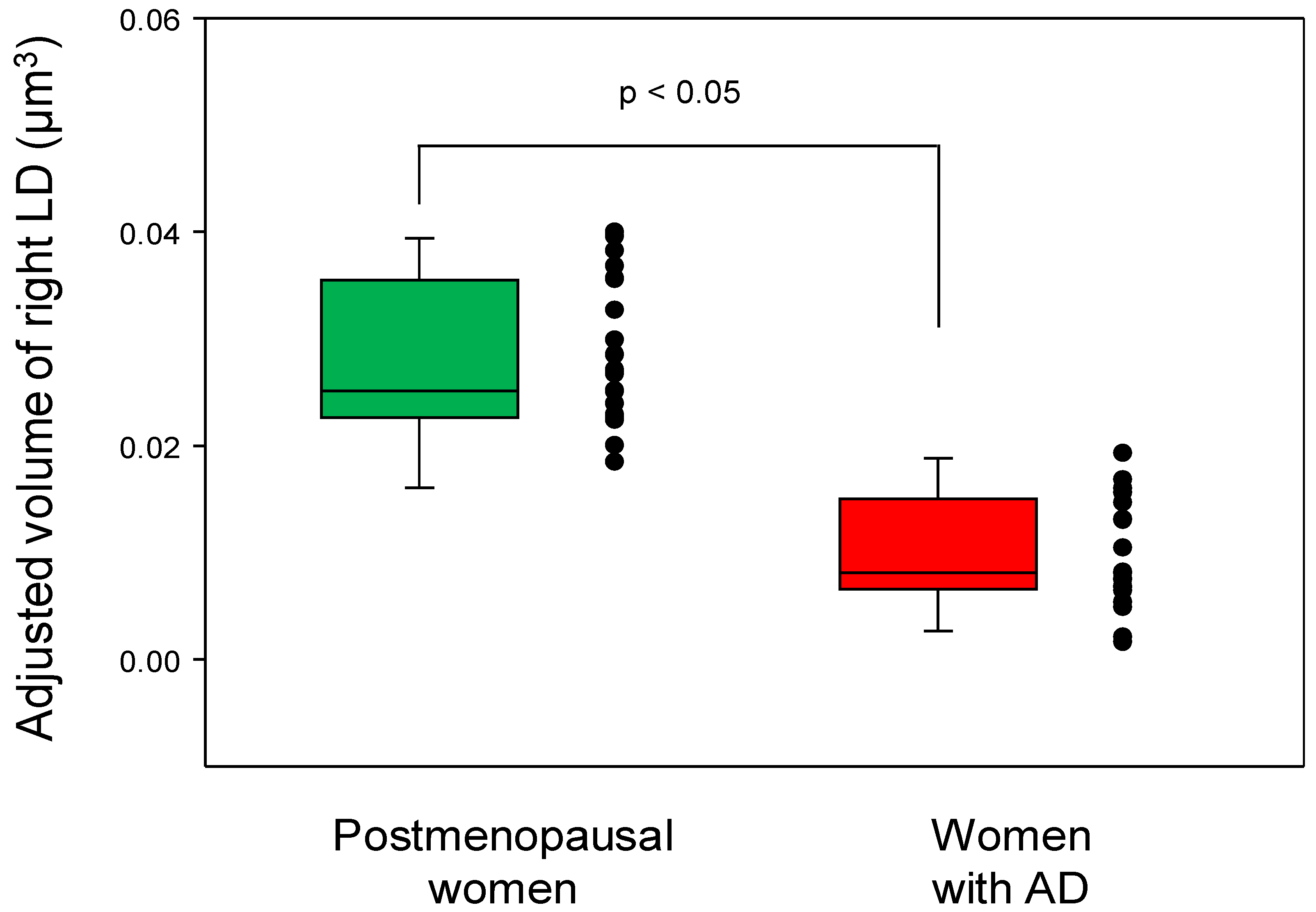
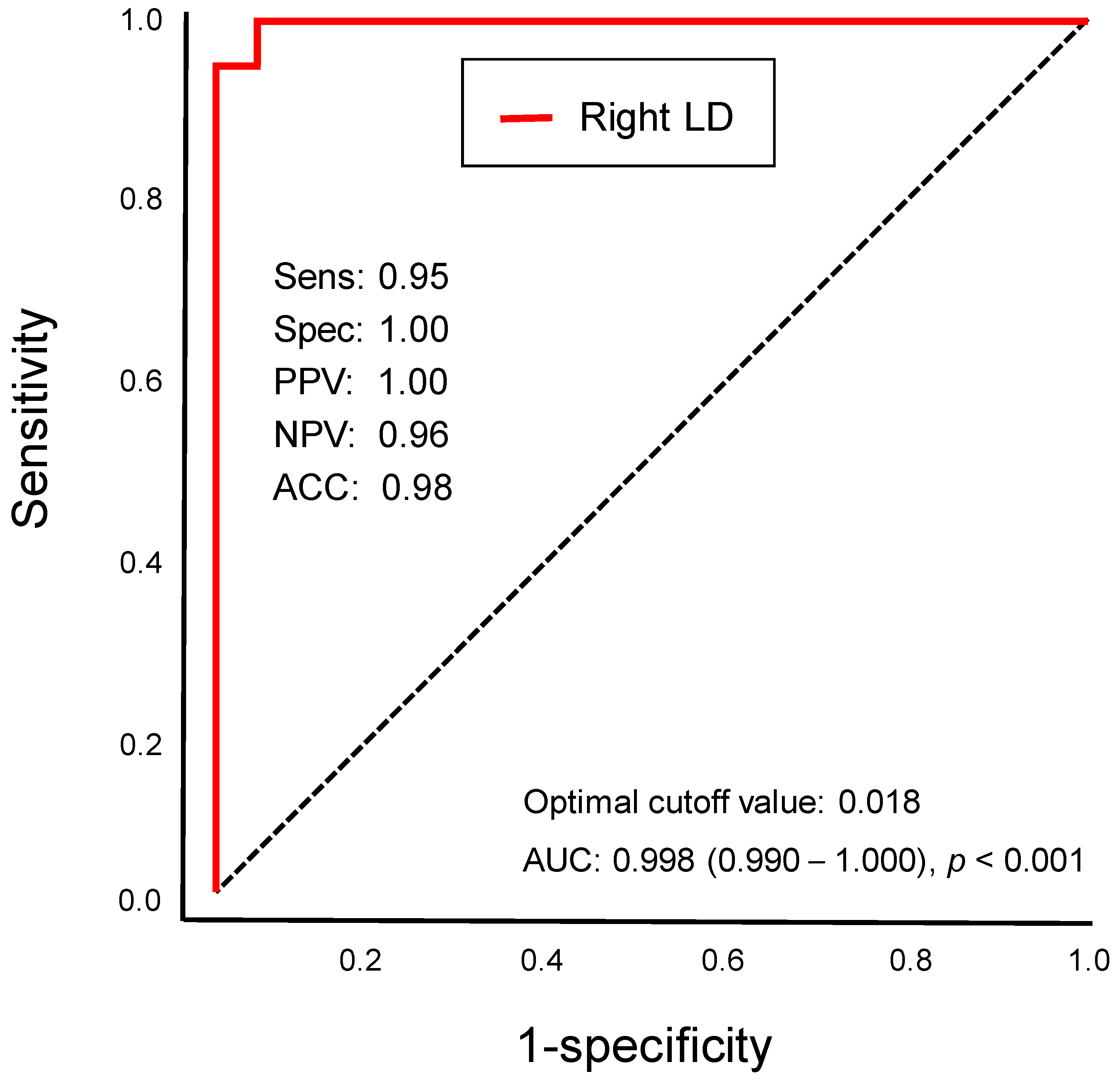
3.4. Differential Thalamic Subnuclear Volume
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, G.W.; Park, K.; Kim, Y.H.; Jeong, G.W. Increased Hippocampal-Inferior Temporal Gyrus White Matter Connectivity following Donepezil Treatment in Patients with Early Alzheimer’s Disease: A Diffusion Tensor Probabilistic Tractography Study. J. Clin. Med. 2023, 12, 967. [Google Scholar] [CrossRef]
- Bevilacqua, R.; Barbarossa, F.; Fantechi, L.; Fornarelli, D.; Paci, E.; Bolognini, S.; Giammarchi, C.; Lattanzio, F.; Paciaroni, L.; Riccardi, G.R.; et al. Radiomics and Artificial Intelligence for the Diagnosis and Monitoring of Alzheimer’s Disease: A Systematic Review of Studies in the Field. J. Clin. Med. 2023, 12, 5432. [Google Scholar] [CrossRef]
- Cammisuli, D.M.; Cipriani, G.; Giusti, E.M.; Castelnuovo, G. Effects of Reminiscence Therapy on Cognition, Depression and Quality of Life in Elderly People with Alzheimer’s Disease: A Systematic Review of Randomized Controlled Trials. J. Clin. Med. 2022, 11, 5752. [Google Scholar] [CrossRef]
- Du, Y.; Yu, J.; Liu, M.H.; Qiu, Q.; Fang, Y.; Zhao, L.; Wei, W.J.; Wang, J.H.; Lin, X.; Yan, F.; et al. The relationship between depressive symptoms and cognitive function in Alzheimer?s disease: The mediating effect of amygdala functional connectivity and radiomic features. J. Affect. Disord. 2023, 330, 101–109. [Google Scholar] [CrossRef]
- Serrano-Pozo, A.; Frosch, M.P.; Masliah, E.; Hyman, B.T. Neuropathological alterations in Alzheimer disease. Cold Spring Harb. Perspect. Med. 2011, 1, a006189. [Google Scholar] [CrossRef]
- Doroszkiewicz, J.; Kulczynska-Przybik, A.; Dulewicz, M.; Borawska, R.; Zajkowska, M.; Slowik, A.; Mroczko, B. Potential Utility of Cerebrospinal Fluid Glycoprotein Nonmetastatic Melanoma Protein B as a Neuroinflammatory Diagnostic Biomarker in Mild Cognitive Impairment and Alzheimer’s Disease. J. Clin. Med. 2023, 12, 4689. [Google Scholar] [CrossRef]
- Navarro-Martos, R.; Nieto-Escamez, F. A Proposal of Cognitive Intervention in Patients with Alzheimer’s Disease through an Assembling Game: A Pilot Study. J. Clin. Med. 2022, 11, 3907. [Google Scholar] [CrossRef]
- Knorr, U.; Simonsen, A.H.; Jensen, C.S.; Zetterberg, H.; Blennow, K.; Akhoj, M.; Forman, J.; Hasselbalch, S.G.; Kessing, L.V. Alzheimer’s disease related biomarkers in bipolar disorder—A longitudinal one-year case-control study. J. Affect. Disord. 2022, 297, 623–633. [Google Scholar] [CrossRef]
- Murakami, S.; Lacayo, P. Biological and disease hallmarks of Alzheimer’s disease defined by Alzheimer’s disease genes. Front. Aging Neurosci. 2022, 14, 996030. [Google Scholar] [CrossRef]
- Colom-Cadena, M.; Spires-Jones, T.; Zetterberg, H.; Blennow, K.; Caggiano, A.; DeKosky, S.T.; Fillit, H.; Harrison, J.E.; Schneider, L.S.; Scheltens, P.; et al. The clinical promise of biomarkers of synapse damage or loss in Alzheimer’s disease. Alzheimers Res. Ther. 2020, 12, 21. [Google Scholar] [CrossRef]
- Guo, L.; Yang, X.; Zhang, Y.; Xu, X.; Li, Y. Effect of exercise on cognitive function and synaptic plasticity in Alzheimer’s disease models: A systematic review and meta-analysis. Front. Aging Neurosci. 2022, 14, 1077732. [Google Scholar] [CrossRef]
- Barron, A.M.; Pike, C.J. Sex hormones, aging, and Alzheimer’s disease. Front. Biosci. 2012, 4, 976–997. [Google Scholar] [CrossRef]
- Horstman, A.M.; Dillon, E.L.; Urban, R.J.; Sheffield-Moore, M. The role of androgens and estrogens on healthy aging and longevity. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 1140–1152. [Google Scholar] [CrossRef]
- Subramaniapillai, S.; Almey, A.; Natasha Rajah, M.; Einstein, G. Sex and gender differences in cognitive and brain reserve: Implications for Alzheimer’s disease in women. Front. Neuroendocrinol. 2021, 60, 100879. [Google Scholar] [CrossRef]
- Vest, R.S.; Pike, C.J. Gender, sex steroid hormones, and Alzheimer’s disease. Horm. Behav. 2013, 63, 301–307. [Google Scholar] [CrossRef]
- Bianchi, V.E. Impact of Testosterone on Alzheimer’s Disease. World J. Mens Health 2022, 40, 243–256. [Google Scholar] [CrossRef]
- Bortz, J.; Klatt, K.C.; Wallace, T.C. Perspective: Estrogen and the Risk of Cognitive Decline: A Missing Choline(rgic) Link? Adv. Nutr. 2022, 13, 376–387. [Google Scholar] [CrossRef]
- Kim, G.W.; Park, K.; Jeong, G.W. Effects of Sex Hormones and Age on Brain Volume in Post-Menopausal Women. J. Sex. Med. 2018, 15, 662–670. [Google Scholar] [CrossRef]
- Kim, G.W.; Jeong, G.W. Menopause-Related Brain Activation Patterns during Visual Sexual Arousal in Menopausal Women: An Fmri Pilot Study Using Time-Course Analysis. Neuroscience 2017, 343, 449–458. [Google Scholar] [CrossRef]
- Jamshed, N.; Ozair, F.F.; Aggarwal, P.; Ekka, M. Alzheimer disease in post-menopausal women: Intervene in the critical window period. J. Midlife Health 2014, 5, 38–40. [Google Scholar] [CrossRef]
- Mosconi, L.; Berti, V.; Quinn, C.; McHugh, P.; Petrongolo, G.; Varsavsky, I.; Osorio, R.S.; Pupi, A.; Vallabhajosula, S.; Isaacson, R.S.; et al. Sex differences in Alzheimer risk: Brain imaging of endocrine vs chronologic aging. Neurology 2017, 89, 1382–1390. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Tan, L.; Wang, H.F.; Jiang, T.; Tan, M.S.; Tan, L.; Zhao, Q.F.; Li, J.Q.; Wang, J.; Yu, J.T. Meta-analysis of modifiable risk factors for Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry 2015, 86, 1299–1306. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Beydoun, H.A.; Gamaldo, A.A.; Teel, A.; Zonderman, A.B.; Wang, Y. Epidemiologic studies of modifiable factors associated with cognition and dementia: Systematic review and meta-analysis. BMC Public Health 2014, 14, 643. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef] [PubMed]
- Santos, C.Y.; Snyder, P.J.; Wu, W.C.; Zhang, M.; Echeverria, A.; Alber, J. Pathophysiologic relationship between Alzheimer’s disease, cerebrovascular disease, and cardiovascular risk: A review and synthesis. Alzheimers Dement 2017, 7, 69–87. [Google Scholar] [CrossRef]
- Sriram, S.; Mehkri, Y.; Quintin, S.; Lucke-Wold, B. Shared pathophysiology: Understanding stroke and Alzheimer’s disease. Clin. Neurol. Neurosurg. 2022, 218, 107306. [Google Scholar] [CrossRef]
- Mehkri, Y.; McDonald, B.; Sriram, S.; Reddy, R.; Kounelis-Wuillaume, S.; Roberts, J.A.; Lucke-Wold, B. Recent Treatment Strategies in Alzheimer’s Disease and Chronic Traumatic Encephalopathy. Biomed. Res. Clin. Rev. 2022, 7, 128. [Google Scholar] [CrossRef]
- Zhang, W.; Qing, Z.; Hu, Y.; Shao, M.; Lu, J.; Wang, J.; Li, M.; Zhang, X.; Nedelska, Z.; Hort, J.; et al. Thalamic Atrophy Plays a Crucial Role in the Effect of Asymptomatic Carotid Stenosis on Cognitive Impairment. Clin. Interv. Aging 2020, 15, 2083–2094. [Google Scholar] [CrossRef]
- Xiao, Y.; Wang, J.; Huang, K.; Gao, L.; Yao, S.; Alzheimer’s Disease Neuroimaging, I. Progressive structural and covariance connectivity abnormalities in patients with Alzheimer’s disease. Front. Aging Neurosci. 2022, 14, 1064667. [Google Scholar] [CrossRef]
- van de Mortel, L.A.; Thomas, R.M.; van Wingen, G.A.; Initia, A.D.N. Grey Matter Loss at Different Stages of Cognitive Decline: A Role for the Thalamus in Developing Alzheimer’s Disease. J. Alzheimers Dis. 2021, 83, 705–720. [Google Scholar] [CrossRef]
- Kim, G.W.; Kim, B.C.; Park, K.S.; Jeong, G.W. A pilot study of brain morphometry following donepezil treatment in mild cognitive impairment: Volume changes of cortical/subcortical regions and hippocampal subfields. Sci. Rep. 2020, 10, 10912. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.W.; Park, S.E.; Park, K.; Jeong, G.W. White Matter Connectivity and Gray Matter Volume Changes Following Donepezil Treatment in Patients with Mild Cognitive Impairment: A Preliminary Study Using Probabilistic Tractography. Front. Aging Neurosci. 2020, 12, 604940. [Google Scholar] [CrossRef] [PubMed]
- Dronse, J.; Ohndorf, A.; Richter, N.; Bischof, G.N.; Fassbender, R.; Behfar, Q.; Gramespacher, H.; Dillen, K.; Jacobs, H.I.L.; Kukolja, J.; et al. Serum cortisol is negatively related to hippocampal volume, brain structure, and memory performance in healthy aging and Alzheimer’s disease. Front. Aging Neurosci. 2023, 15, 1154112. [Google Scholar] [CrossRef] [PubMed]
- Chetelat, G.; Landeau, B.; Eustache, F.; Mezenge, F.; Viader, F.; de la Sayette, V.; Desgranges, B.; Baron, J.C. Using voxel-based morphometry to map the structural changes associated with rapid conversion in MCI: A longitudinal MRI study. Neuroimage 2005, 27, 934–946. [Google Scholar] [CrossRef]
- Zidan, M.; Boban, J.; Bjelana, M.; Todorovic, A.; Vujanic, T.S.; Semnic, M.; Boban, N.; Kozic, D. Thalamic volume loss as an early sign of amnestic mild cognitive impairment. J. Clin. Neurosci. 2019, 68, 168–173. [Google Scholar] [CrossRef]
- Tremblay, A.; Jobin, C.; Demers, M.; Dagenais, E.; Narayanan, S.; Araujo, D.; Douglas, A.L.; Roger, E.; Chamelian, L.; Duquette, P.; et al. Thalamic and hippocampal volume associated with memory functions in multiple sclerosis. Brain Cogn. 2018, 125, 61–68. [Google Scholar] [CrossRef]
- Pardilla-Delgado, E.; Torrico-Teave, H.; Sanchez, J.S.; Ramirez-Gomez, L.A.; Baena, A.; Bocanegra, Y.; Vila-Castelar, C.; Fox-Fuller, J.T.; Guzman-Velez, E.; Martinez, J.; et al. Associations between subregional thalamic volume and brain pathology in autosomal dominant Alzheimer’s disease. Brain. Commun. 2021, 3, fcab101. [Google Scholar] [CrossRef]
- Braak, H.; Braak, E. Alzheimer’s disease affects limbic nuclei of the thalamus. Acta Neuropathol. 1991, 81, 261–268. [Google Scholar] [CrossRef]
- Forno, G.; Saranathan, M.; Contador, J.; Guillen, N.; Falgas, N.; Tort-Merino, A.; Balasa, M.; Sanchez-Valle, R.; Hornberger, M.; Llado, A. Thalamic nuclei changes in early and late onset Alzheimer’s disease. Curr. Res. Neurobiol. 2023, 4, 100084. [Google Scholar] [CrossRef]
- Taber, K.H.; Wen, C.; Khan, A.; Hurley, R.A. The limbic thalamus. J. Neuropsychiatry Clin. Neurosci. 2004, 16, 127–132. [Google Scholar] [CrossRef]
- Bernstein, A.S.; Rapcsak, S.Z.; Hornberger, M.; Saranathan, M.; Alzheimer’s Disease Neuroimaging, I. Structural Changes in Thalamic Nuclei Across Prodromal and Clinical Alzheimer’s Disease. J. Alzheimers Dis. 2021, 82, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Low, A.; Mak, E.; Malpetti, M.; Chouliaras, L.; Nicastro, N.; Su, L.; Holland, N.; Rittman, T.; Rodriguez, P.V.; Passamonti, L.; et al. Asymmetrical atrophy of thalamic subnuclei in Alzheimer’s disease and amyloid-positive mild cognitive impairment is associated with key clinical features. Alzh. Dement-Dadm. 2019, 11, 690–699. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.W.; Farabaugh, A.H.; Vetterman, R.; Holmes, A.; Nyer, M.; Nasiriavanaki, Z.; Fava, M.; Holt, D.J. Diminished frontal pole size and functional connectivity in young adults with high suicidality. J. Affect. Disord. 2022, 310, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Lee, H.W.; Kim, B.K.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Jang, J.Y.; Park, S.Y.; Lee, H.W.; Lee, C.K.; et al. Comparison of FibroScan-Aspartate Aminotransferase (FAST) Score and Other Non-invasive Surrogates in Predicting High-Risk Non-alcoholic Steatohepatitis Criteria. Front. Med. 2022, 9, 869190. [Google Scholar] [CrossRef]
- Cleveland, H. Cleveland HearLab. Available online: https://www.clevelandheartlab.com/tests/estrogens-total-immunoassay (accessed on 20 October 2015).
- Lee, E. Clinical Research Service. Seoul, South Korea: Green Cross Reference Laboratory. 2007. Available online: http://www.gcrl.co.kr (accessed on 27 March 2018).
- Aggleton, J.P.; Pralus, A.; Nelson, A.J.; Hornberger, M. Thalamic pathology and memory loss in early Alzheimer’s disease: Moving the focus from the medial temporal lobe to Papez circuit. Brain 2016, 139, 1877–1890. [Google Scholar] [CrossRef]
- Pini, L.; Pievani, M.; Bocchetta, M.; Altomare, D.; Bosco, P.; Cavedo, E.; Galluzzi, S.; Marizzoni, M.; Frisoni, G.B. Brain atrophy in Alzheimer’s Disease and aging. Ageing Res. Rev. 2016, 30, 25–48. [Google Scholar] [CrossRef]
- Blanken, A.E.; Hurtz, S.; Zarow, C.; Biado, K.; Honarpisheh, H.; Somme, J.; Brook, J.; Tung, S.; Kraft, E.; Lo, D.; et al. Associations between hippocampal morphometry and neuropathologic markers of Alzheimer’s disease using 7 T MRI. Neuroimage Clin. 2017, 15, 56–61. [Google Scholar] [CrossRef]
- Rao, Y.L.; Ganaraja, B.; Murlimanju, B.V.; Joy, T.; Krishnamurthy, A.; Agrawal, A. Hippocampus and its involvement in Alzheimer’s disease: A review. 3 Biotech 2022, 12, 55. [Google Scholar] [CrossRef]
- Apostolova, L.G.; Zarow, C.; Biado, K.; Hurtz, S.; Boccardi, M.; Somme, J.; Honarpisheh, H.; Blanken, A.E.; Brook, J.; Tung, S.; et al. Relationship between hippocampal atrophy and neuropathology markers: A 7T MRI validation study of the EADC-ADNI Harmonized Hippocampal Segmentation Protocol. Alzheimers Dement 2015, 11, 139–150. [Google Scholar] [CrossRef]
- Frisoni, G.B.; Fox, N.C.; Jack, C.R., Jr.; Scheltens, P.; Thompson, P.M. The clinical use of structural MRI in Alzheimer disease. Nat. Rev. Neurol. 2010, 6, 67–77. [Google Scholar] [CrossRef]
- McDonald, C.R.; Gharapetian, L.; McEvoy, L.K.; Fennema-Notestine, C.; Hagler, D.J.; Holland, D.; Dale, A.M.; Initia, A.D.N. Relationship between regional atrophy rates and cognitive decline in mild cognitive impairment. Neurobiol. Aging 2012, 33, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Sarazin, M.; Chauviré, V.; Gerardin, E.; Colliot, O.; Kinkingnéhun, S.; de Souza, L.C.; Hugonot-Diener, L.; Garnero, L.; Lehéricya, S.; Chupin, M.; et al. The Amnestic Syndrome of Hippocampal type in Alzheimer’s Disease: An MRI Study. J. Alzheimers Dis. 2010, 22, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Cherubini, A.; Peran, P.; Spoletini, I.; Di Paola, M.; Di Iulio, F.; Hagberg, G.E.; Sancesario, G.; Gianni, W.; Bossu, P.; Caltagirone, C.; et al. Combined volumetry and DTI in subcortical structures of mild cognitive impairment and Alzheimer’s disease patients. J. Alzheimers Dis. 2010, 19, 1273–1282. [Google Scholar] [CrossRef] [PubMed]
- Mizumori, S.J.; Miya, D.Y.; Ward, K.E. Reversible inactivation of the lateral dorsal thalamus disrupts hippocampal place representation and impairs spatial learning. Brain Res. 1994, 644, 168–174. [Google Scholar] [CrossRef]
- van Groen, T.; Kadish, I.; Wyss, J.M. The role of the laterodorsal nucleus of the thalamus in spatial learning and memory in the rat. Behav. Brain Res. 2002, 136, 329–337. [Google Scholar] [CrossRef]
- Bezdudnaya, T.; Keller, A. Laterodorsal nucleus of the thalamus: A processor of somatosensory inputs. J. Comp. Neurol. 2008, 507, 1979–1989. [Google Scholar] [CrossRef]
- Roy, D.S.; Zhang, Y.; Aida, T.; Shen, C.; Skaggs, K.M.; Hou, Y.; Fleishman, M.; Mosto, O.; Weninger, A.; Feng, G. Anterior thalamic circuits crucial for working memory. Proc. Natl. Acad. Sci. USA 2022, 119, e2118712119. [Google Scholar] [CrossRef]
- Wolff, M.; Vann, S.D. The Cognitive Thalamus as a Gateway to Mental Representations. J. Neurosci. 2019, 39, 3–14. [Google Scholar] [CrossRef]
- Aggleton, J.P.; Nelson, A.J. Why do lesions in the rodent anterior thalamic nuclei cause such severe spatial deficits? Neurosci. Biobehav. Rev. 2015, 54, 131–144. [Google Scholar] [CrossRef]
- Shibata, H.; Naito, J. Organization of anterior cingulate and frontal cortical projections to the anterior and laterodorsal thalamic nuclei in the rat. Brain Res. 2005, 1059, 93–103. [Google Scholar] [CrossRef]
- Wilton, L.A.; Baird, A.L.; Muir, J.L.; Honey, R.C.; Aggleton, J.P. Loss of the thalamic nuclei for “head direction” impairs performance on spatial memory tasks in rats. Behav. Neurosci. 2001, 115, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Li, W.P.; Xie, Y.; Yu, T.T.; Wu, W.B.; Wang, K.; Wu, S.C.; Qing, Z.; Zhang, X.; Li, M.; Liu, R.Y.; et al. APOE & epsilon;4 allele modified the correlation between deep grey matter volume and cognitive performance in non-demented elders. Chin. J. Acad. Radio. 2020, 3, 152–161. [Google Scholar] [CrossRef]
- Dwivedi, M.; Dubey, N.; Pansari, A.J.; Bapi, R.S.; Das, M.; Guha, M.; Banerjee, R.; Pramanick, G.; Basu, J.; Ghosh, A. Effects of Meditation on Structural Changes of the Brain in Patients with Mild Cognitive Impairment or Alzheimer’s Disease Dementia. Front. Hum. Neurosci. 2021, 15, 728993. [Google Scholar] [CrossRef]
- Pedro, T.; Weiler, M.; Yasuda, C.L.; D’Abreu, A.; Damasceno, B.P.; Cendes, F.; Balthazar, M.L. Volumetric brain changes in thalamus, corpus callosum and medial temporal structures: Mild Alzheimer’s disease compared with amnestic mild cognitive impairment. Dement Geriatr. Cogn. Disord. 2012, 34, 149–155. [Google Scholar] [CrossRef] [PubMed]

| Sex Hormones | Postmenopausal Women (n = 21) | * Reference Ranges for Postmenopausal Women |
|---|---|---|
| Total estrogen (pg/mL) | 77.9 ± 42.3 | 50–170 |
| Estradiol (E2) (pg/mL) | 13.7 ± 7.4 | less than 37 |
| Estriol (E3) (pg/mL) | 2.4 ± 1.4 | - |
| Free testosterone (pg/mL) | 0.2 ± 0.2 | Women aged 20–38 y: 0.06–2.5 Women aged 40–59 y: 0.04–2.0 |
| Sex-hormone-binding globulin (SHBG, nmol/L) | 71.1 ± 19.1 | Women: 16–120 |
| Follicle-stimulating hormone (FSH, mlU/mL) | 64.0 ± 21.5 | 23–116.3 |
| Luteinizing hormone (LH, mlU/mL) | 37.1 ± 12.3 | 15.9–54.0 |
| Postmenopausal Women | Women with AD | t-Value | F-Value | p-Value | Cohen’s d | |
|---|---|---|---|---|---|---|
| Two-sample t-test | ||||||
| L Thalamus | 5.55 ± 0.55 | 4.72 ± 0.57 | 4.86 | - | <0.001 * | 1.54 |
| R Thalamus | 5.43 ± 0.55 | 4.76 ± 0.60 | 3.90 | - | <0.001 * | 1.23 |
| Multivariate analysis adjusted for age | ||||||
| L Thalamus | 5.55 ± 0.55 | 4.72 ± 0.57 | - | 0.06 | 0.807 | 0.08 |
| R Thalamus | 5.43 ± 0.55 | 4.76 ± 0.60 | - | 0.20 | 0.654 | 0.14 |
| Thalamic Nuclei | Abbrev. | Postmenopausal Women | Women with AD | F-Value | p-Value | Cohen’s d | |
|---|---|---|---|---|---|---|---|
| Anterior | L Anteroventral | AV | 0.115 ± 0.032 | 0.078 ± 0.021 | 1.2 | 0.275 | 0.35 |
| R Anteroventral | 0.124 ± 0.019 | 0.088 ± 0.022 | 3.1 | 0.086 | 0.56 | ||
| Lateral | L Laterodorsal | LD | 0.023 ± 0.009 | 0.009 ± 0.005 | 4.5 | 0.041 | 0.67 |
| R Laterodorsal | 0.028 ± 0.007 | 0.010 ± 0.005 | 12.8 | <0.001 * | 1.13 | ||
| L Laterodorsal posterior | LP | 0.091 ± 0.014 | 0.081 ± 0.021 | 0.6 | 0.429 | 0.25 | |
| R Laterodorsal posterior | 0.092 ± 0.016 | 0.082 ± 0.018 | 0.1 | 0.721 | 0.10 | ||
| Ventral | L Ventral anterior | VA | 0.320 ± 0.059 | 0.279 ± 0.030 | 0.3 | 0.591 | 0.17 |
| R Ventral anterior | 0.295 ± 0.043 | 0.246 ± 0.037 | 2.5 | 0.124 | 0.50 | ||
| L Ventral anterior magnocellular | VAmc | 0.024 ± 0.004 | 0.020 ± 0.002 | 2.2 | 0.147 | 0.47 | |
| R Ventral anterior magnocellular | 0.025 ± 0.004 | 0.020 ± 0.002 | 2.7 | 0.108 | 0.52 | ||
| L Ventral lateral anterior | VLa | 0.445 ± 0.038 | 0.438 ± 0.044 | 0.1 | 0.702 | 0.10 | |
| R Ventral lateral anterior | 0.455 ± 0.057 | 0.415 ± 0.050 | 1.2 | 0.279 | 0.35 | ||
| L Ventral lateral posterior | VLp | 0.565 ± 0.054 | 0.587 ± 0.067 | 0.0 | 0.828 | 0.00 | |
| R Ventral lateral posterior | 0.591 ± 0.071 | 0.572 ± 0.066 | 0.2 | 0.682 | 0.14 | ||
| L Ventral posterolateral | VPL | 0.583 ± 0.124 | 0.642 ± 0.077 | 0.1 | 0.707 | 0.10 | |
| R Ventral posterolateral | 0.643 ± 0.091 | 0.654 ± 0.078 | 0.2 | 0.650 | 0.14 | ||
| L Ventromedial | VM | 0.015 ± 0.003 | 0.015 ± 0.002 | 0.0 | 0.944 | 0.00 | |
| R Ventromedial | 0.017 ± 0.003 | 0.016 ± 0.002 | 0.1 | 0.739 | 0.10 | ||
| Intralaminar | L Central medial | CeM | 0.056 ± 0.016 | 0.042 ± 0.009 | 0.2 | 0.682 | 0.14 |
| R Central medial | 0.060 ± 0.011 | 0.043 ± 0.009 | 0.8 | 0.371 | 0.28 | ||
| L Central lateral | CL | 0.031 ± 0.011 | 0.024 ± 0.004 | 1.8 | 0.183 | 0.42 | |
| R Central lateral | 0.035 ± 0.010 | 0.025 ± 0.005 | 4.6 | 0.039 | 0.68 | ||
| L Paracentral | Pc | 0.003 ± 0.001 | 0.003 ± 0.000 | 0.1 | 0.779 | 0.10 | |
| R Paracentral | 0.003 ± 0.000 | 0.003 ± 0.000 | 1.6 | 0.214 | 0.40 | ||
| L Centromedian | CM | 0.170 ± 0.026 | 0.181 ± 0.028 | 1.3 | 0.258 | 0.36 | |
| R Centromedian | 0.173 ± 0.025 | 0.186 ± 0.024 | 0.0 | 0.999 | 0.00 | ||
| L Parafascicular | Pf | 0.040 ± 0.008 | 0.041 ± 0.004 | 0.0 | 0.832 | 0.00 | |
| R Parafascicular | 0.047 ± 0.008 | 0.045 ± 0.004 | 0.0 | 0.869 | 0.00 | ||
| Medial | L Paratenial | Pt | 0.005 ± 0.001 | 0.006 ± 0.001 | 0.7 | 0.422 | 0.27 |
| R Paratenial | 0.006 ± 0.001 | 0.005 ± 0.001 | 0.1 | 0.739 | 0.10 | ||
| L Reuniens | MV | 0.011 ± 0.004 | 0.006 ± 0.003 | 0.6 | 0.455 | 0.25 | |
| R Reuniens | 0.012 ± 0.003 | 0.005 ± 0.003 | 1.9 | 0.179 | 0.30 | ||
| L Mediodorsal medial magnocellular | MDm | 0.503 ± 0.102 | 0.463 ± 0.069 | 0.0 | 0.848 | 0.00 | |
| R Mediodorsal medial magnocellular | 0.478 ± 0.095 | 0.465 ± 0.061 | 0.2 | 0.671 | 0.14 | ||
| L Mediodorsal lateral parvocellular | MDl | 0.183 ± 0.045 | 0.154 ± 0.026 | 0.0 | 0.869 | 0.00 | |
| R Mediodorsal lateral parvocellular | 0.178 ± 0.041 | 0.157 ± 0.021 | 0.0 | 0.943 | 0.00 | ||
| Posterior | L Lateral geniculate | LGN | 0.190 ± 0.046 | 0.139 ± 0.034 | 1.6 | 0.219 | 0.40 |
| R Lateral geniculate | 0.202 ± 0.035 | 0.167 ± 0.035 | 1.6 | 0.215 | 0.40 | ||
| L Medial geniculate | MGN | 0.078 ± 0.018 | 0.081 ± 0.016 | 0.0 | 0.858 | 0.00 | |
| R Medial geniculate | 0.089 ± 0.014 | 0.091 ± 0.016 | 0.0 | 0.845 | 0.00 | ||
| L Limitans | L-SG | 0.016 ± 0.005 | 0.018 ± 0.004 | 0.8 | 0.382 | 0.28 | |
| R Limitans | 0.014 ± 0.004 | 0.019 ± 0.005 | 0.7 | 0.419 | 0.27 | ||
| L Pulvinar anterior | PuA | 0.143 ± 0.027 | 0.120 ± 0.017 | 0.1 | 0.760 | 0.10 | |
| R Pulvinar anterior | 0.156 ± 0.025 | 0.148 ± 0.017 | 0.9 | 0.356 | 0.30 | ||
| L Pulvinar medial | PuM | 0.728 ± 0.095 | 0.666 ± 0.103 | 0.0 | 0.985 | 0.00 | |
| R Pulvinar medial | 0.831 ± 0.128 | 0.821 ± 0.094 | 6.1 | 0.018 | 0.78 | ||
| L Pulvinar lateral | PuL | 0.129 ± 0.023 | 0.130 ± 0.026 | 3.4 | 0.072 | 0.58 | |
| R Pulvinar lateral | 0.150 ± 0.038 | 0.177 ± 0.036 | 11.7 | 0.002 | 1.08 | ||
| L Pulvinar inferior | PuI | 0.159 ± 0.024 | 0.145 ± 0.038 | 1.0 | 0.313 | 0.32 | |
| R Pulvinar inferior | 0.189 ± 0.038 | 0.187 ± 0.034 | 12.6 | 0.001 | 1.12 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, G.-W.; Park, K.; Jeong, G.-W. Early Detection of Alzheimer’s Disease in Postmenopausal Women Using Thalamic Subnuclear Volumetry. J. Clin. Med. 2023, 12, 6844. https://doi.org/10.3390/jcm12216844
Kim G-W, Park K, Jeong G-W. Early Detection of Alzheimer’s Disease in Postmenopausal Women Using Thalamic Subnuclear Volumetry. Journal of Clinical Medicine. 2023; 12(21):6844. https://doi.org/10.3390/jcm12216844
Chicago/Turabian StyleKim, Gwang-Won, Kwangsung Park, and Gwang-Woo Jeong. 2023. "Early Detection of Alzheimer’s Disease in Postmenopausal Women Using Thalamic Subnuclear Volumetry" Journal of Clinical Medicine 12, no. 21: 6844. https://doi.org/10.3390/jcm12216844
APA StyleKim, G.-W., Park, K., & Jeong, G.-W. (2023). Early Detection of Alzheimer’s Disease in Postmenopausal Women Using Thalamic Subnuclear Volumetry. Journal of Clinical Medicine, 12(21), 6844. https://doi.org/10.3390/jcm12216844






