The Use of Fissios App© as a Complement to a Face-to-Face Respiratory Physiotherapy Program versus an Attendance-Only Face-to-Face Physiotherapy Program in Patients Scheduled for Thoracic Surgical Procedures Reduces the Risk of Developing Postoperative Pulmonary Complications—A Quasi-Experimental Study
Abstract
:1. Introduction
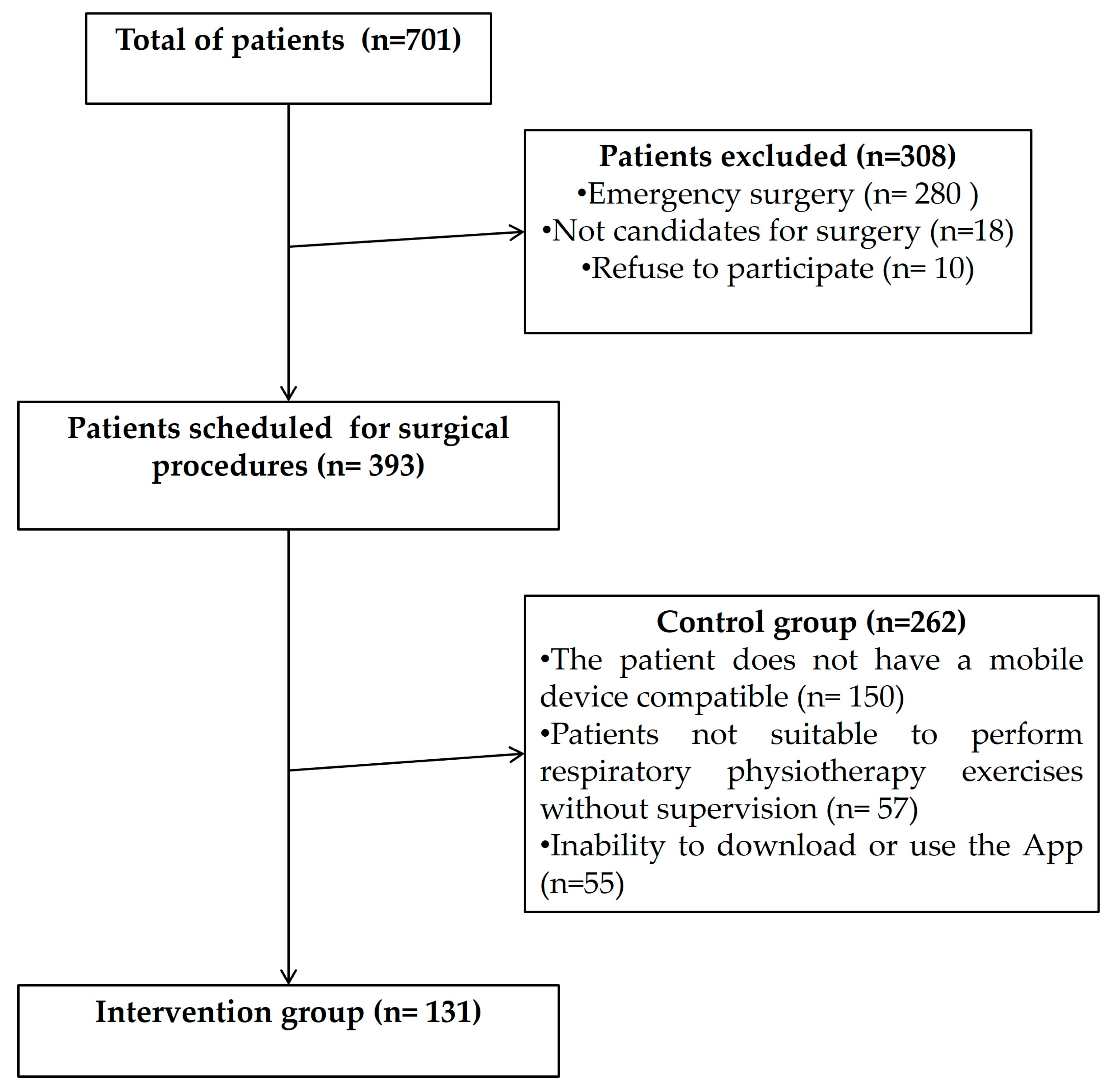
2. Materials and Methods
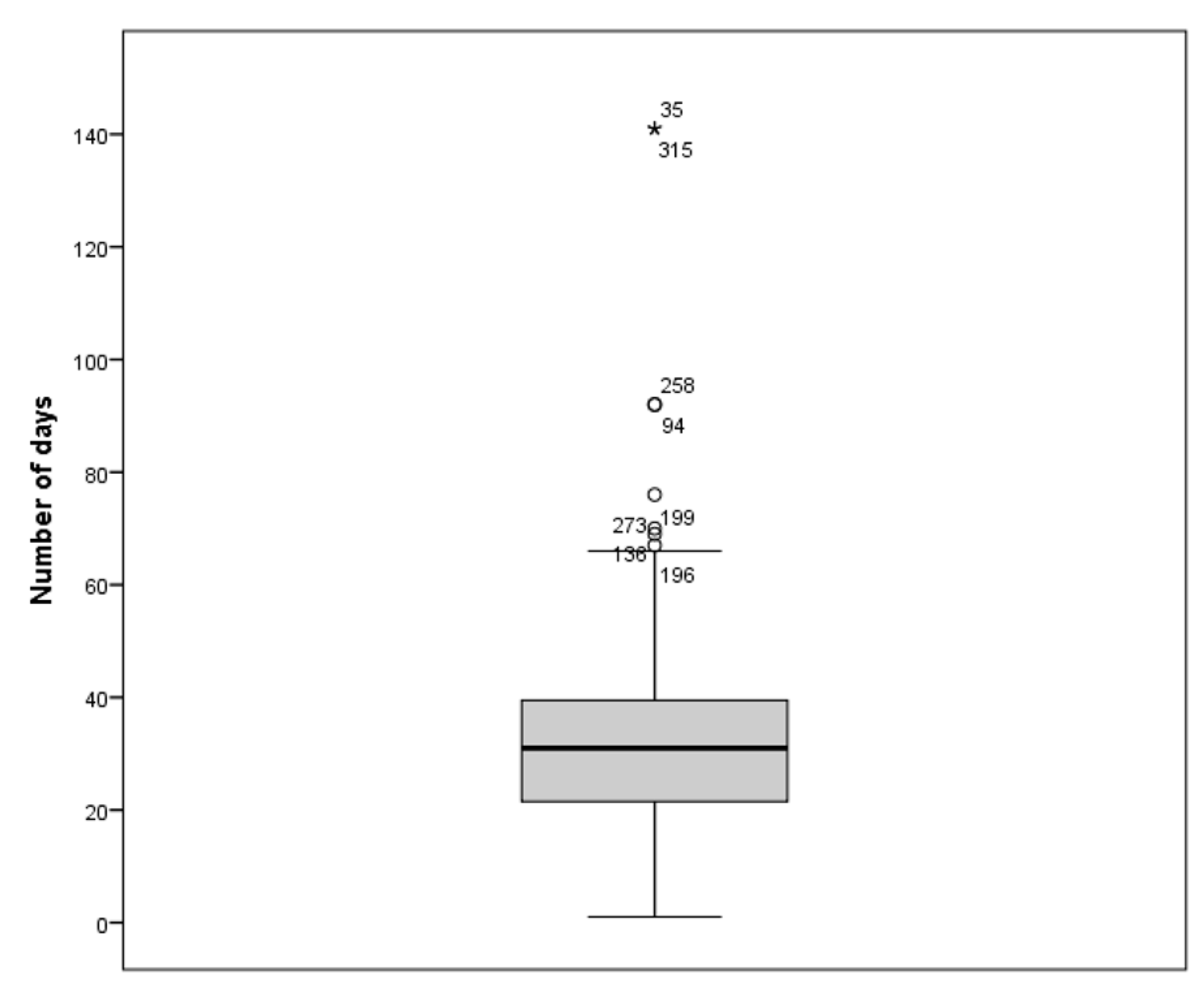
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Agostini, P.; Cieslik, H.; Rathinam, S.; Bishay, E.; Kalkat, M.S.; Rajesh, P.B.; Steyn, R.S.; Singh, S.; Naidu, B. Postoperative Pulmonary Complications Following Thoracic Surgery: Are There Any Modifiable Risk Factors? Thorax 2010, 65, 815–818. [Google Scholar] [CrossRef]
- Canet, J.; Mazo, V. Postoperative Pulmonary Complications. Minerva Anestesiol. 2010, 76, 138–143. [Google Scholar]
- Wang, S.; Li, X.; Li, Y.; Li, J.; Jiang, G.; Liu, J.; Wang, J. The Long-Term Impact of Postoperative Pulmonary Complications after Video-Assisted Thoracic Surgery Lobectomy for Lung Cancer. J. Thorac. Dis. 2017, 9, 5143–5152. [Google Scholar] [CrossRef]
- Rogers, L.J.; Bleetman, D.; Messenger, D.E.; Joshi, N.A.; Wood, L.; Rasburn, N.J.; Batchelor, T.J.P. The Impact of Enhanced Recovery after Surgery (ERAS) Protocol Compliance on Morbidity from Resection for Primary Lung Cancer. J. Thorac. Cardiovasc. Surg. 2018, 155, 1843–1852. [Google Scholar] [CrossRef]
- Sebio Garcia, R.; Yáñez Brage, M.I.; Giménez Moolhuyzen, E.; Granger, C.L.; Denehy, L. Functional and Postoperative Outcomes after Preoperative Exercise Training in Patients with Lung Cancer: A Systematic Review and Meta-Analysis. Interact. Cardiovasc. Thorac. Surg. 2016, 23, 486–497. [Google Scholar] [CrossRef] [PubMed]
- Granger, C.; Cavalheri, V. Preoperative Exercise Training for People with Non-small Cell Lung Cancer. Cochrane Database Syst. Rev. 2022, 2022, CD012020. [Google Scholar] [CrossRef]
- Ferreira, V.; Agnihotram, R.V.; Bergdahl, A.; van Rooijen, S.J.; Awasthi, R.; Carli, F.; Scheede-Bergdahl, C. Maximizing Patient Adherence to Prehabilitation: What Do the Patients Say? Support. Care Cancer 2018, 26, 2717–2723. [Google Scholar] [CrossRef]
- Rosero, I.D.; Ramírez-Vélez, R.; Lucia, A.; Martínez-Velilla, N.; Santos-Lozano, A.; Valenzuela, P.L.; Morilla, I.; Izquierdo, M. Systematic Review and Meta-Analysis of Randomized, Controlled Trials on Preoperative Physical Exercise Interventions in Patients with Non-Small-Cell Lung Cancer. Cancers 2019, 11, 944. [Google Scholar] [CrossRef] [PubMed]
- Steffens, D.; Beckenkamp, P.R.; Hancock, M.; Solomon, M.; Young, J. Preoperative Exercise Halves the Postoperative Complication Rate in Patients with Lung Cancer: A Systematic Review of the Effect of Exercise on Complications, Length of Stay and Quality of Life in Patients with Cancer. Br. J. Sports Med. 2018, 52, 344. [Google Scholar] [CrossRef] [PubMed]
- Cavalheri, V.; Granger, C. Preoperative Exercise Training for Patients with Non-small Cell Lung Cancer. Cochrane Database Syst. Rev. 2017, 2017, CD012020. [Google Scholar] [CrossRef]
- Pouwels, S.; Hageman, D.; Gommans, L.N.M.; Willigendael, E.M.; Nienhuijs, S.W.; Scheltinga, M.R.; Teijink, J.A.W. Preoperative Exercise Therapy in Surgical Care: A Scoping Review. J. Clin. Anesth. 2016, 33, 476–490. [Google Scholar] [CrossRef]
- Comacchio, G.M.; Monaci, N.; Verderi, E.; Schiavon, M.; Rea, F. Enhanced Recovery after Elective Surgery for Lung Cancer Patients: Analysis of Current Pathways and Perspectives. J. Thorac. Dis. 2019, 11, S515–S522. [Google Scholar] [CrossRef] [PubMed]
- Batchelor, T.J.P.; Rasburn, N.J.; Abdelnour-Berchtold, E.; Brunelli, A.; Cerfolio, R.J.; Gonzalez, M.; Ljungqvist, O.; Petersen, R.H.; Popescu, W.M.; Slinger, P.D.; et al. Guidelines for Enhanced Recovery after Lung Surgery: Recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2019, 55, 91–115. [Google Scholar] [CrossRef] [PubMed]
- Garutti, I.; Cabañero, A.; Vicente, R.; Sánchez, D.; Granell, M.; Fraile, C.A.; Real Navacerrada, M.; Novoa, N.; Sanchez-Pedrosa, G.; Congregado, M.; et al. Recommendations of the Society of Thoracic Surgery and the Section of Cardiothoracic and Vascular Surgery of the Spanish Society of Anesthesia, Resuscitation and Pain Therapy, for Patients Undergoing Lung Surgery Included in an Intensified Recovery Program. Rev. Esp. Anestesiol. Reanim. 2022, 69, 208–241. [Google Scholar] [CrossRef]
- Cassidy, M.R.; Rosenkranz, P.; McCabe, K.; Rosen, J.E.; McAneny, D. I COUGH: Reducing Postoperative Pulmonary Complications with a Multidisciplinary Patient Care Program. JAMA Surg. 2013, 148, 740–745. [Google Scholar] [CrossRef]
- do Nascimento Junior, P.; Módolo, N.S.P.; Andrade, S.; Guimarães, M.M.F.; Braz, L.G.; El Dib, R. Incentive Spirometry for Prevention of Postoperative Pulmonary Complications in Upper Abdominal Surgery. Cochrane Database Syst. Rev. 2014, 2014, CD006058. [Google Scholar] [CrossRef]
- Morano, M.T.; Araújo, A.S.; Nascimento, F.B.; da Silva, G.F.; Mesquita, R.; Pinto, J.S.; de Moraes Filho, M.O.; Pereira, E.D. Preoperative Pulmonary Rehabilitation versus Chest Physical Therapy in Patients Undergoing Lung Cancer Resection: A Pilot Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2013, 94, 53–58. [Google Scholar] [CrossRef]
- Cañizares Carretero, M.-Á.; García Fontán, E.-M.; Blanco Ramos, M.; Soro García, J.; Carrasco Rodríguez, R.; Peña González, E.; Cueto Ladrón De Guevara, A. Is Age a Predisposing Factor of Postoperative Complications After Lung Resection for Primary Pulmonary Neoplasms? Cir. Esp. Engl. Ed. 2017, 95, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Jean, R.A.; DeLuzio, M.R.; Kraev, A.I.; Wang, G.; Boffa, D.J.; Detterbeck, F.C.; Wang, Z.; Kim, A.W. Analyzing Risk Factors for Morbidity and Mortality after Lung Resection for Lung Cancer Using the NSQIP Database. J. Am. Coll. Surg. 2016, 222, 992–1000.e1. [Google Scholar] [CrossRef]
- Fraile Olivero, C.A.; Jarabo Sarceda, J.R.; Fernández Martín, E.; Santos Capa, P.; Arribas Manzanal, P.D.; Gómez Martínez, A.M.; Calatayud Gastardi, J.; Hernando Trancho, F. Implementation of a perioperative care App in elective thoracic surgery. Cirugía Española 2023, 101, 265–273. [Google Scholar] [CrossRef]
- Lai, Y.; Huang, J.; Yang, M.; Su, J.; Liu, J.; Che, G. Seven-Day Intensive Preoperative Rehabilitation for Elderly Patients with Lung Cancer: A Randomized Controlled Trial. J. Surg. Res. 2017, 209, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Waterland, J.L.; Ismail, H.; Amin, B.; Granger, C.L.; Denehy, L.; Riedel, B. Patient Acceptance of Prehabilitation for Major Surgery: An Exploratory Survey. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2021, 29, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Hardcastle, S.J.; Maxwell-Smith, C.; Kamarova, S.; Lamb, S.; Millar, L.; Cohen, P.A. Factors Influencing Non-Participation in an Exercise Program and Attitudes towards Physical Activity amongst Cancer Survivors. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2018, 26, 1289–1295. [Google Scholar] [CrossRef]
- Mahendran, K.; Naidu, B. The Key Questions in Rehabilitation in Thoracic Surgery. J. Thorac. Dis. 2018, 10, S924–S930. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P. Smartphone Applications for Patients’ Health and Fitness. Am. J. Med. 2016, 129, 11–19. [Google Scholar] [CrossRef]
- Fraile Olivero, C.A. Fissios App. Available online: https://fissiosapp.com/ (accessed on 1 September 2023).
| Element | Objective |
|---|---|
| Exercise | |
| Basic position (30 s) | Correct position sitting in chair |
| Nasal and mouth breathing (30 s) | Correct intake and output air during exercises |
| Abdominal–diaphragmatic ventilation (10 repetitions) | Strengthen the diaphragm, rectus abdominis, abdominal obliques, and transverse abdominis muscle |
| Lung expansion (10 repetitions) | Strengthen the diaphragm, external intercostals, trapezius, sternocleidomastoid, and scalene muscles |
| Arm exercises (10 repetitions) | Strengthen the diaphragm external intercostals, trapezius, sternocleidomastoid, and scalene muscles |
| Sigh and hug (10 repetitions) | Forced expiration and secretions mobilization |
| Incentive spirometer (10 repetitions) | Encourage long, slow, and deep breaths |
| Voluntary cough maneuver (3 repetitions) | Forced expiration and secretions mobilization |
| Effective cough (3 repetitions) | Forced expiration and secretions mobilization |
| Walking (10 min) | Early mobilization and aerobic activity |
| Medical advice | |
| Breathing exercises | Encourage performing of the breathing exercises, establishing a routine, and continuing to do usual physical activity |
| Stop smoking | Inform patients of the importance and possibility of stopping smoking before surgery |
| Oral care | Recommendation for adequate oral care and explanation of the relationship with postoperative complications |
| General points | Information to prepare for surgery, including fasting and usual medication |
| Physical exercises | Encourage putting into practice the exercises learned before surgery and performing the routine |
| Out of bed! | Explain the relationship between delaying getting out of bed and postoperative complications |
| Do you feel pain? | Inform the need to control pain and the importance of relieving it |
| Balanced and healthy food | Promote a healthy diet and prevention of microaspirations |
| Immediate postoperative period | Describe the normal postoperative period of a patient during the first 48 h in hospital |
| Variable | Intervention Group (n = 131) | Control Group (n = 262) | p-Value |
|---|---|---|---|
| Male sex (n, %) | 79 (60.3%) | 147 (56.1%) | 0.427 |
| Age, y | 62 (51–71) | 65.5 (55–73) | 0.029 |
| Smoking status (n, %) | 0.947 | ||
| Unknown | 25 (19.1%) | 51 (19.5%) | |
| Nonsmoker | 18 (13.7%) | 38 (14.5%) | |
| Former smoker | 29 (22.1%) | 63 (24%) | |
| Current smoker | 59 (45%) | 110 (42%) | |
| ASA grade (n, %) | 0.861 | ||
| I | 21 (16%) | 34 (13%) | |
| II | 73 (55.7%) | 148 (56.5%) | |
| III | 35 (26.7%) | 76 (29%) | |
| IV | 2 (1.5%) | 4 (1.5%) | |
| Lung parenchyma resection (n, %) | 115 (87.8%) | 190 (72.5%) | 0.001 |
| Surgical approach | 0.253 | ||
| VATS (n, %) | 67 (51.1%) | 118 (45%) | |
| Conventional (n, %) | 64 (48.9%) | 144 (55%) |
| Variable | Intervention Group (131 Patients) | Control Group (262 Patients) | p-Value |
|---|---|---|---|
| LOS (d) | 3 (2–5) | 4 (3–6) | <0.001 |
| PPCs (n, %) | 16 (12.2) | 63 (24) | 0.006 |
| Pneumonia (n, %) | 7 (5.3%) | 27 (10.3%) | 0.099 |
| Air leak >5 days (n, %) | 4 (3.1%) | 22 (8.4%) | 0.004 |
| Atelectasis (n, %) | 3 (2.6%) | 4 (1.5%) | 0.590 |
| 30-d mortality (n, %) | 0 (0) | 3 (1.1) | 0.219 |
| Variable | Category | n | OR | CI 95% | p-Value |
|---|---|---|---|---|---|
| Sex | Male | 167 | 2.3 | 1.3–4.2 | 0.003 |
| Female | 226 | 1 | |||
| Age | Numeric | 0.9 | 0.9–1.01 | 0.711 | |
| Surgical approach | VATS | 185 | 1 | 1.4–4.49 | <0.001 |
| Conventional | 208 | 2.5 | |||
| Lung parenchyma resection | Yes | 305 | 4.2 | 1.76–10.21 | <0.001 |
| No | 88 | 1 | |||
| Time of use of Fissios App© | No use | 262 | 1 | 0.17–0.78 | 0.009 |
| >4 weeks | 77 | 0.36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fraile Olivero, C.A.; Jarabo Sarceda, J.R.; Fernández Martín, E.; Alen Villamayor, V.; Calatayud Gastardi, J.; Gómez Martínez, A.M.; Santos, P.; Arribas Manzanal, P.D.; Cerdán Santacruz, C.; Hernando Trancho, F. The Use of Fissios App© as a Complement to a Face-to-Face Respiratory Physiotherapy Program versus an Attendance-Only Face-to-Face Physiotherapy Program in Patients Scheduled for Thoracic Surgical Procedures Reduces the Risk of Developing Postoperative Pulmonary Complications—A Quasi-Experimental Study. J. Clin. Med. 2023, 12, 6774. https://doi.org/10.3390/jcm12216774
Fraile Olivero CA, Jarabo Sarceda JR, Fernández Martín E, Alen Villamayor V, Calatayud Gastardi J, Gómez Martínez AM, Santos P, Arribas Manzanal PD, Cerdán Santacruz C, Hernando Trancho F. The Use of Fissios App© as a Complement to a Face-to-Face Respiratory Physiotherapy Program versus an Attendance-Only Face-to-Face Physiotherapy Program in Patients Scheduled for Thoracic Surgical Procedures Reduces the Risk of Developing Postoperative Pulmonary Complications—A Quasi-Experimental Study. Journal of Clinical Medicine. 2023; 12(21):6774. https://doi.org/10.3390/jcm12216774
Chicago/Turabian StyleFraile Olivero, Carlos Alfredo, José Ramón Jarabo Sarceda, Elena Fernández Martín, Verónica Alen Villamayor, Joaquín Calatayud Gastardi, Ana María Gómez Martínez, Passio Santos, Pedro Daniel Arribas Manzanal, Carlos Cerdán Santacruz, and Florentino Hernando Trancho. 2023. "The Use of Fissios App© as a Complement to a Face-to-Face Respiratory Physiotherapy Program versus an Attendance-Only Face-to-Face Physiotherapy Program in Patients Scheduled for Thoracic Surgical Procedures Reduces the Risk of Developing Postoperative Pulmonary Complications—A Quasi-Experimental Study" Journal of Clinical Medicine 12, no. 21: 6774. https://doi.org/10.3390/jcm12216774
APA StyleFraile Olivero, C. A., Jarabo Sarceda, J. R., Fernández Martín, E., Alen Villamayor, V., Calatayud Gastardi, J., Gómez Martínez, A. M., Santos, P., Arribas Manzanal, P. D., Cerdán Santacruz, C., & Hernando Trancho, F. (2023). The Use of Fissios App© as a Complement to a Face-to-Face Respiratory Physiotherapy Program versus an Attendance-Only Face-to-Face Physiotherapy Program in Patients Scheduled for Thoracic Surgical Procedures Reduces the Risk of Developing Postoperative Pulmonary Complications—A Quasi-Experimental Study. Journal of Clinical Medicine, 12(21), 6774. https://doi.org/10.3390/jcm12216774






